We previously reported that patients undergoing interhospital transfer for primary PCI in the United States rarely met national guidelines-based recommendations of door-to-balloon times of 90 minutes or less using data from 1999 to 2002 in the National Registry of Myocardial Infarction (NRMI).(1) The median “total” door-to-balloon times – i.e., the time from arrival at the first hospital to initial balloon inflation at the PCI hospital – in these patients was 180 minutes and only 4.2% had times less than 90 minutes. Since the publication of this report, there have been widespread efforts to improve timely access to primary PCI through the establishment of regionalized networks of hospitals for STEMI.(2, 3) However, more contemporary data on total door-to-balloon times in patients undergoing interhospital transfer for primary PCI have yet to be reported.
We used 2005 and 2006 data from the American College of Cardiology's National Cardiovascular Data Registry's (NCDR) CathPCI Registry™. Details of hospitals and data collection methods employed by the NCDR have been previously described.(4) We included all catheterization laboratory visits of STEMI patients undergoing primary PCI after interhospital transfer (n=22,019). To narrow our study population further, we excluded catheterization laboratory visits by patients: (1) who presented to the hospital more than 12 hours after symptom onset (n = 2993) or with uncertain time of symptom onset (n = 453); (2) who received any fibrinolytic therapy prior to arrival in the cardiac catheterization laboratory (n=2,622); (3) with unknown or invalid date/time of reference for hospital arrival or PCI (n=852); (4) with door-to-balloon times that exceeded 12 hours (n=1,677); and with any combination of the above exclusions (n=6874). This restricted our study population to 15,145 catheterization laboratory visits in 15,049 patients at 491 hospitals.
Our primary end point was “total” door-to-balloon time, which was defined as the time of arrival at the first hospital to the time of initial balloon inflation at the PCI hospital. We also evaluated: (1) door-to-door time (time of arrival at the initial hospital to time of arrival at the PCI hospital) and (2) PCI hospital door-to-balloon time (time of arrival at the PCI hospital to time of the first balloon inflation at the PCI hospital). Univariable analyses were used to report characteristics of the study population and the distribution of these endpoints.
The mean age of the study population was 60.5 years old, 29.0% were women, 88.3% were white, and 20.8% had diabetes mellitus. In addition, 31.6% of patients arrived at the first hospital on weekdays between 8AM and 4PM, 14.6% presented more than 6 hours after symptom onset, and 10.6% were in cardiogenic shock. The median time from arrival in the initial hospital to the first balloon inflation time at the PCI hospital (i.e. total door-to-balloon time) was 152 minutes (interquartile range, 116–211). Total door–to-balloon time was less than 2 hours in 27.7% of patients, between 2 and 4 hours in 53.9% of patients, and greater than or equal to 4 hours in 18.4% of patients (Figure 1). Only 8.6% of patients had total door-to-balloon times less than 90 minutes. The median door-to-door and PCI hospital door-to-balloon times were 109 and 38 minutes, respectively.
Figure 1.
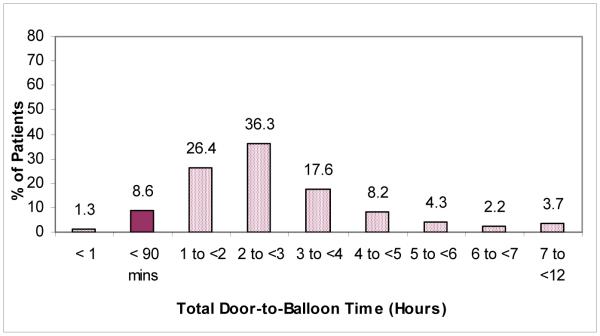
Distribution of “total” door-to-balloon times in patients undergoing transfer for primary PCI. Total balloon time refers to the time from arrival at the first hospital to first balloon inflation at the PCI hospital. The proportion of patients with total door-to-balloon times under 90 minutes is highlighted by the darkened bar.
The use of primary PCI in patients with STEMI is rising in the United States.(5) However, there continue to be concerns about its effectiveness in patients undergoing interhospital transfer given the potential risks of delays in time-to-reperfusion. Although we previously reported that such delays are common, these results used data collected prior to the publication of the Danish Multicenter Randomized Study on Thrombolytic Therapy Versus Acute Coronary Angioplasty in Acute Myocardial Infarction-2 (DANAMI-2) trial.(6) This landmark study – which found that interhospital transfer for primary PCI is both feasible and efficacious within the controlled setting of a clinical trial – has prompted local and national efforts in the United States to improve timely access to primary PCI by establishing regionalized networks of hospitals for STEMI.
In this context, the current analysis adds important new information to the literature. Our findings suggest shorter total door-to-balloon times in transfer patients during the intervening few years (i.e., 152 versus 180 minutes). However, we also found that many patients still have marked delays in total door-to-balloon times and that few reach the benchmark established by national guidelines. When compared with the previous analysis, total door-to-balloon times were shorter because of more rapid door-to-door times (109 versus 120 minutes) and PCI hospital door-to-balloon times (38 versus 53 minutes). Of course, any direct comparisons between the current and previous analyses should be done with caution due to the involvement of different hospitals and types of patients between registries. The current analysis, for example, included more non-urban hospitals as well as patients with cardiogenic shock. Finally, it is important to note that these hospitals participated voluntarily in the CathPCI Registry™, a national quality improvement registry. These hospitals therefore may present a “best”-case scenario for transfer patients.
Acknowledgments
Funding Source: Supported in part by a grant from the National Heart, Lung, and Blood Institute, grant #R01HL072575, Bethesda, MD.
Footnotes
Conflict of Interest Disclosure: Dr. Rumsfeld is Chief Science Officer for the NCDR. Dr. Krumholz has research contracts with ACC.
References
- 1.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. NRMI Investigators. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111:761–767. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 2.Henry TD, Atkins JM, Cunningham MS, et al. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers. J Am Coll Cardiol. 2006;47:1339–1345. doi: 10.1016/j.jacc.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of Systems of Care for ST-Elevation Myocardial Infarction Patients: Executive Summary. Circulation. 2007;116:217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 4.Anderson HV, Shaw RE, Brindis RG, et al. A contemporary overview of percutaneous coronary interventions: The American College of Cardiology - National Cardiovascular Data Registry (ACC-NCDR) J Am Coll Cardiol. 2002;39:1096–1103. doi: 10.1016/s0735-1097(02)01733-3. [DOI] [PubMed] [Google Scholar]
- 5.Nallamothu BK, Blaney ME, Morris SM, et al. Acute Reperfusion Therapy in ST-Elevation Myocardial Infarction from 1994–2003. Am J Med. 2007;120:693–699. doi: 10.1016/j.amjmed.2007.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersen HR, Nielsen TT, Rasmussen D, et al. A Comparison of Coronary Angioplasty with Fibrinolytic Therapy in Acute Myocardial Infarction. N Engl J Med. 2003;349:733–742. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]


