Abstract
Background/Aim
The role of substance P and the neurokinin-1 receptor (NK-1R) in the transition from inflammation to dysplasia in inflammatory bowel disease is not clear.
Methods
Colitis-associated dysplasia was induced in Sprague-Dawley rats by intracolonic, then systemic, administration of trinitrobenzene sulfonic acid. One group of animals received the NK-1R antagonist SR140333; the rest received vehicle. Colons were removed and analyzed for damage and expression of NK-1R downstream components.
Results
The NK-1R antagonist-treated animals had significantly reduced macroscopic and microscopic damage and decreased incidence of inflammatory bowel disease. Twice as many of these animals had a normal diagnosis in any region of the colon. A decrease in proliferation index, Cox-2 expression, and active Erk1/2 was found compared with the vehicle-treated group. In Caco-2 cells, Erk1/2 was activated by substance P and prostaglandin E2.
Conclusion
A selective NK-1R antagonist may delay the development of further colonic damage, offering a potential treatment for patients with long-standing colitis.
Keywords: Animal model, antagonist, colitis, dysplasia, neurokinin
Crohn’s disease and ulcerative colitis are inflammatory bowel diseases (IBD) with unidentified causes. Although the exact etiologies are poorly understood, there is evidence that they involve interactions of the immune system, the environment, and genetic susceptibility (1).
One of the potential consequences of long-standing ulcerative colitis is cancer (2). Each year, more than 140,000 Americans are diagnosed with colorectal cancer, and more than 55,000 die from this disease, accounting for ~15% of all deaths in IBD patients (3, 4). However, the underlying mechanisms in ulcerative colitis-associated dysplasia are poorly understood.
Substance P (SP) is a neuropeptide that is associated with the regulation of biological processes such as nociception, smooth muscle contraction, exocrine and endocrine gland secretion, and connective tissue proliferation (5). The endogenous receptor for SP is the neurokinin-1 receptor (NK-1R). SP and NK-1R have been implicated in the pathophysiology of intestinal inflammation (6). A pro-inflammatory role for SP and NK-1R has been shown in acute colitis, resulting in histologic inflammation, neutrophil accumulation, and an increase in inflammatory mediators (7–9). NK-1R has been found to be increased during chronic inflammatory processes including IBD (6, 10), and the involvement of both SP and NK-1R have been demonstrated in an animal model of chronic inflammation (11). By stimulating NK-1R, SP triggers a number of responses that are important for tumor growth (12). The binding of SP to NK-1R causes activation of mitogen-activated protein kinases (MAPKs) and Erk1 and Erk2 (Erk1/2), by transactivation of the epidermal growth factor receptor (EGFR) via a metalloproteinase-dependent pathway (13). The Erk1/2 MAPK pathways control cell proliferation and other activities essential for tumorigenesis. The proliferative effects and anti-apoptotic signals may result in aberrant growth and neoplasia formation, since chronic intestinal inflammatory diseases are associated with a high incidence of cancer (14).
Investigation of the underlying events occurring in colitis-associated dysplasia is complicated by the fact that there are a limited number of animal models available to study the transition of inflammation to dysplasia. Investigators have attempted to develop colitis-associated colon carcinogenesis models, but each model involves the administration of a carcinogen, such as dimethylhydrazine or azoxymethane, before the induction of colitis (15, 16). Although useful, these models do not truly mimic the chronic inflammation that transitions into colorectal cancer. Perhaps more relevant are studies investigating the use of the pro-inflammatory agent dextran sulfate sodium, but, again, this is given in combination with a carcinogen (17, 18). A well-established rat model of chronic colitis was recently modified to develop an animal model that can be used to investigate ulcerative colitis-associated dysplasia (19). This model more closely mimics the human condition, with a transition from chronic inflammation to dysplasia and carcinoma, a scenario similar to that seen in humans who have progression of ulcerative colitis to cancer. Its characteristics of long-term chronic inflammation, in which the involvement of SP and NK-1R have been demonstrated, now allow the unique opportunity to study the NK-1R signaling pathways.
The aim of this study was to investigate the role of NK-1R in the novel model of colitis-associated dysplasia (19), with supporting in vitro analyses, and to explore the potential therapeutic use of a selective NK-1R antagonist. It was hypothesized that the degree of inflammation and dysplasia would correlate with the expression of NK-1R and its downstream components and that this effect could be altered by administration of an NK-1R antagonist.
Materials and Methods
Cell culture and cell proliferation assay
Caco-2 cells were obtained from American Type Culture Collection (Manassas, VA, USA), and maintained in DMEM-10% fetal calf serum at 37°C and 5% CO2. For cell proliferation assays, cells were plated in 96-well plates (1,000 cells/well) in DMEM-0.1% fetal calf serum in the presence or absence of SP (10 nM), prostaglandin E2 (PGE2; 2 µM), or EGF (1 ng/ml). The number of relative viable cells was measured after 4 days of culture in CellTiterGlo reagent (Promega, Madisson, WI, USA). SP and PGE2 were obtained from Sigma (St. Louis, MO, USA), EGF from Peprotech (Rocky Hill, NJ, USA) and Erlotinib (Tarceva) from Fisher Scientific (Pittsburgh, PA, USA).
Animals
Male Sprague-Dawley rats weighing 200–220 g at the start of the initial treatment were maintained in restricted-access rooms with controlled temperature (23°C) and a 12-h light-dark cycle. Standard laboratory chow and drinking water were provided ad libitum. Rats were weighed weekly for weight loss analysis and drug administration. Animal protocols were approved by the Institutional Animal Care and Use Committee at Ponce School of Medicine and were performed in accordance with the principles described in the ‘Guide for the Care and Use of Laboratory Animals’ (publication No. DHHS (NIH) 86–23).
Induction and reactivation of the colitis and development of dysplasia
To induce chronic colitis, trinitrobenzene sulfonic acid (TNBS; 0.5 ml of 60 mg/ml; Sigma Aldrich; St. Louis, MO, USA) in 50% ethanol was introduced rectally into the colon with a rubber catheter, approximately 8 cm proximal to the anus. This was followed by intravenous reactivation 6 weeks later (20). Briefly, the rats were lightly anesthetized with ether, and TNBS (5 mg/kg in 0.9% saline) was administered intravenously via a tail vein every 24 hours for 3 consecutive days (20). Dysplasia was developed by continuing the administration of TNBS (5 mg/kg) twice a week intravenously for 10 weeks (19). The rats were weighed weekly until they were euthanized at 10 weeks with an overdose of pentobarbital (~1.5 ml of 65 mg/kg for rats >500 g).
Drug treatment
One group of animals was treated with the NK-1R antagonist (SR140333; kind gift of Sanofi-Synthelabo Recherche, Paris, France). Each rat received an intraperitoneal dose of 1 mg/kg SR140333 dissolved in saline twice a week. The other group was treated with saline.
Measurement of macroscopic damage
The colon was analyzed macroscopically using the criteria of Appleyard and Wallace (20). Four variables were examined: the presence of diarrhea (0 or 1 for absence or presence), adhesions between the colon and other organs (0, 1, or 2 for none, minor, or major, respectively), the thickness of each colon segment (in millimeters), and the degree of ulceration (0 for no damage; with increasing scores up to 10, depending on the extent of ulceration). These variables were added to give a total macroscopic damage score.
Sample collection
The colon length was measured in centimeters and cut into equal thirds representing the proximal, mid, and distal portions. These segments were cut longitudinally; one half was weighed and stored at −80°C for molecular analysis, and the other half was fixed in 10% buffered formalin for histological analysis. The Swiss-roll technique was used to evaluate each colon segment microscopically, allowing the entire length of the intestine to be seen at once. Briefly, the tissue was rolled into a small piece using forceps and then fixed and placed in a cassette for the remainder of the histological analysis (19).
Microscopic assessment
The tissues were scored microscopically for damage by a blinded observer as previously described (19). Criteria included loss of mucosal architecture (0–3: absent, mild, to severe), cellular infiltration (0, none; 1, in muscularis mucosae; 2, in lamina propria/villi; 3, in serosa), muscle thickening (0, muscle < 1/2 of mucosal thickness; 1, muscle = 1/2 to 3/4 of mucosal thickness; 2, muscle = mucosal thickness; 3 = all muscle), goblet cell depletion (0, absent; 1, present), and crypt abscess formation (0, absent; 1, present). The score of each variable was added to give a total microscopic damage score (maximum of 11).
Pathologic evaluation
Colonic sections (2–4 µm), stained with hematoxylin and eosin, were analyzed for dysplasia by a blinded pathologist. Scoring for dysplasia was based on previously published criteria (19, 21). Briefly, tissue sections were classified as either negative for dysplasia or positive for dysplasia or carcinoma. The tissues classified as negative for dysplasia adhered to one of the following two descriptions: normal (small basally located nuclei and normal architecture) or active colitis (cryptitis, glandular invasion by neutrophils, crypt abscesses, microabscesses). A classification of positive dysplasia was characterized by low-grade dysplasia, which included hyperchromasia, loss of mucin, increased nuclear/cytoplasmic ratio, nuclear elongation and stratification, irregular nuclear outline, and increased number of normal mitosis. The criteria for high-grade dysplasia included the characteristics of low-grade dysplasia plus mucosal architectural distortion including fusion of glands (cribiform pattern) and presence of vesicular polygonal nuclei. For a diagnosis of carcinoma, the characteristics of high-grade dysplasia were included in addition to presence of atypical mitosis and/or of single tumor cells within the lamina propria (19).
Immunohistochemistry
Formalin-fixed 4-µm tissue sections were deparaffinized with xylene, 2 changes, 10 minutes each, and then hydrated through descending grades of ethanol to deionized water. After antigen retrieval in an Emerson 1100W microwave with the appropriate buffer (0.01 M citrate buffer, pH 6.0, high to boiling, and then 20 minutes on power level 5; or 1 mM EDTA high to boiling and then 10 minutes on power level 4), slides were cooled at room temperature for 20 minutes, rinsed with deionized water, and placed in TBS-Tween for 5 minutes. Slides were immunostained on the Dako Autostainer Plus (Dako, Carpinteria, CA, USA). Endogenous peroxidase was blocked with 3% aqueous hydrogen peroxide. After slides were washed with phosphate-buffered saline for 5 minutes, they were blocked with normal serum for 20 minutes, followed by incubation with the primary antibody. The following antibodies were used: pEGFR-pY1068, pSrc-pY416 (Cell Signaling Technology, Boston, MA, USA) and NK-1R (Santa Cruz Biotechnology, Santa Cruz, CA, USA), with working solutions of 1:400 (overnight), 1:50 (overnight), and 1:50 (60 minutes) respectively. Endogenous avidin-biotin activity was blocked using the Avidin/Biotin Blocking kit and Vector Elite Mouse or Rabbit IgG-HRP for detection (Vector Laboratories, Burlingame, CA, USA). In addition, Cox 2 (Cayman Chemical, Ann Arbor, MI, USA), pErk ½ (Cell Signaling Technology, Boston, MA, USA), and Ki-67 (BD Pharmigen, San Jose, CA, USA) were used at working solutions of 1:200 (overnight), 1:100 (overnight), and 1:400 (30 minutes). EnVision+Rabbit-IgG HRP polymer detection (Dako Corporation, Carpinteria, CA, USA) were used for Cox-2 and pErk ½, and Mouse to Mouse polymer detection (Chemicon, Billerica, MA, USA) for Ki67.
All samples were lightly counterstained with Mayer's hematoxylin for 30 seconds, dehydrated through graded alcohol, cleared with xylene, and mounted with resinous mounting medium. The stain was semiquantitatively examined by two independent pathologists using the Allred 8-unit system (22) using the combination of a proportion score from 0 to 5, with an intensity score on a scale from 0 to 3 (none, weak, moderate, strong). A total score of 2–3 was considered low, a score of 4–5 was considered intermediate, and a score of 6–8 was considered high (22).
Western and immunoblot analysis
Proteins were extracted using lysis buffer (50 mM Tris-HCl, pH 7.5, 150 mM NaCl, 1 mM EDTA, 1 mM EGTA, 25 mM NaF, 5 mM Na4P2O7, 1% Triton X-100, 1 mM Na3VO4, 20 mM p-nitrophenyl phosphate, 2 mg/ml leupeptin, 2 mg/ml aprotinin, and 1 mM phenylmethylsulfonyl fluoride). Equal amounts (30 µg) of protein were fractionated in 12% SDS gel and transferred to a PVDF membrane. Membranes were blocked with 5% non-fat dry milk in TBST and incubated with one of the following primary antibodies: Erk1/2, p-Erk1/2, Akt, p-Akt, Src, or pSrc-pY416 (Cell Signaling catalog nos. 9102, 4376, 9272, 9271, 2109, and 2113, respectively). Membranes were washed with TBST and incubated with horseradish peroxidase-labeled secondary antibodies. The bands were detected using ECL-Plus reagent kit (GE Amersham, Piscataway, NJ, USA; #RPN2132). Western blot bands were quantified by densitometry using ImageQuant 5.2 Software (Typhoon 9410; GE Amersham, Piscataway, NJ, USA), and p-Erk1/2, p-Akt, and pSrc-pY416 bands were normalized for the corresponding total kinase. Caco-2 cells were lysed in lysis buffer. Cell lysate supernatants (10 µg protein/each) were analyzed by immunoblotting as described previously (23).
Statistical analysis
Values are presented as means ± SEM, where ‘n’ represents one tissue from one animal used for a single replicate of an experiment. Statistical analyses were performed using GraphPad Instat V3.0 and GraphPad Prism V3.0 (GraphPad Software, San Diego, CA, USA). In all cases, groups were analyzed using the Student’s unpaired t-test. P < 0.05 was considered to represent a significant difference.
Results
SR140333 treatment significantly decreased parameters of colonic damage
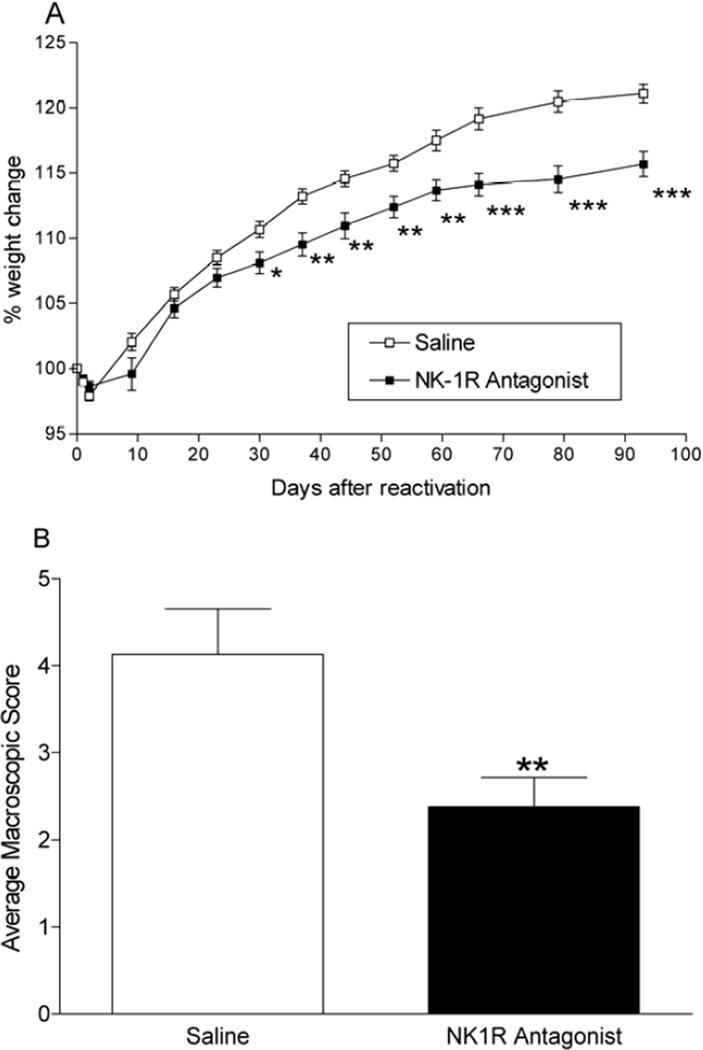
During the study (10 weeks), all animals gained weight compared with their original starting weight, apart from the first 3 days of treatment (Figure 1A). As mentioned in a prior study, this was most likely due to a combination of the intravenous administration of TNBS and stress from the procedure until acclimatization (19). The NK-1R antagonist-treated group gained less weight than the vehicle-treated group throughout the study (Figure 1A), probably due to the purported role of SP in appetite regulation and metabolism, in addition to its recognized effects in gastric motility and digestion (24).
Figure 1.
(A). Effect of an NK-1R antagonist on weight change in an animal model of colitis-associated dysplasia (*P < 0.05; **P < 0.01; ***P < 0.001 versus vehicle-treated animals). Results are means ± SE; n = 22 per group. (B). Effect of an NK-1R antagonist on macroscopic damage score in an animal model of colitis-associated dysplasia. The average macroscopic score (including the presence of adhesions, thickness of the tissue, presence or absence of diarrhea, and grade of ulceration) was significantly decreased by administration of the antagonist (**P < 0.01). Results are means ± SE; n = 22 per group.
Treatment with the NK-1R antagonist significantly decreased the total macroscopic damage score compared with the vehicle-treated group (p < 0.01; Figure 1B). As reported previously (19), these animals have shortened colons compared to colons from normal rats; however, the average length of the colon in the vehicle-treated animals (10.35 ± 0.34 cm), although shorter, was not significantly affected by the NK-1R antagonist treatment (10.52 ± 0.39 cm).
The colon was examined microscopically for loss of mucosal architecture, cellular infiltration, muscle thickening, crypt abscess formation, and goblet cell depletion (Table I). The total microscopic damage in all regions of the colon was lower in the NK-1R antagonist-treated animals than in vehicle-treated animals. This decrease reached significance in both the proximal and mid-colon (p < 0.01).
Table I.
Average of Microscopic Variables
| Loss of Mucosal Architecture |
Cell Infiltration |
Muscle Thickness |
Goblet Cell Depletion |
Crypt Abscess Formation |
Total Microscopic Score |
|
|---|---|---|---|---|---|---|
| Proximal | ||||||
| Saline | 1.68 ± 0.15 | 3.00 ± 0.00 | 2.45 ± 0.13 | 1.00 ± 0.00 | 0.14 ± 0.07 | 8.05 ± 0.15 |
| NK-1R Antagonist | 1.43 ± 0.11 | 3.00 ± 0.00 | 1.64 ± 0.15 *** | 0.95 ± 0.04 | 0.27 ± 0.10 | 7.33 ± 0.20 ** |
| Mid | ||||||
| Saline | 1.50 ± 0.11 | 2.95 ± 0.04 | 2.33 ± 0.17 | 1.00 ± 0.00 | 0.23 ± 0.09 | 8.19 ± 0.26 |
| NK-1R Antagonist | 1.23 ± 0.10 | 3.00 ± 0.00 | 2.05 ± 0.19 | 0.95 ± 0.04 | 0.09 ± 0.06 | 7.10 ± 0.26 ** |
| Distal | ||||||
| Saline | 1.40 ± 0.11 | 3.00 ± 0.00 | 2.82 ± 0.08 * | 1.00 ± 0.00 | 0.23 ± 0.09 | 8.59 ± 0.17 |
| NK-1R Antagonist | 1.81 ± 0.15 * | 2.95 ± 0.04 | 2.38 ± 0.15 * | 1.00 ± 0.00 | 0.32 ± 0.10 | 8.14 ± 0.25 |
Values are means ± SE; n = 21.
p < 0.05,
p < 0.01,
p <0.001, versus vehicle-treated animals within the same colonic region.
SR140333 treatment-ameliorated inflammation
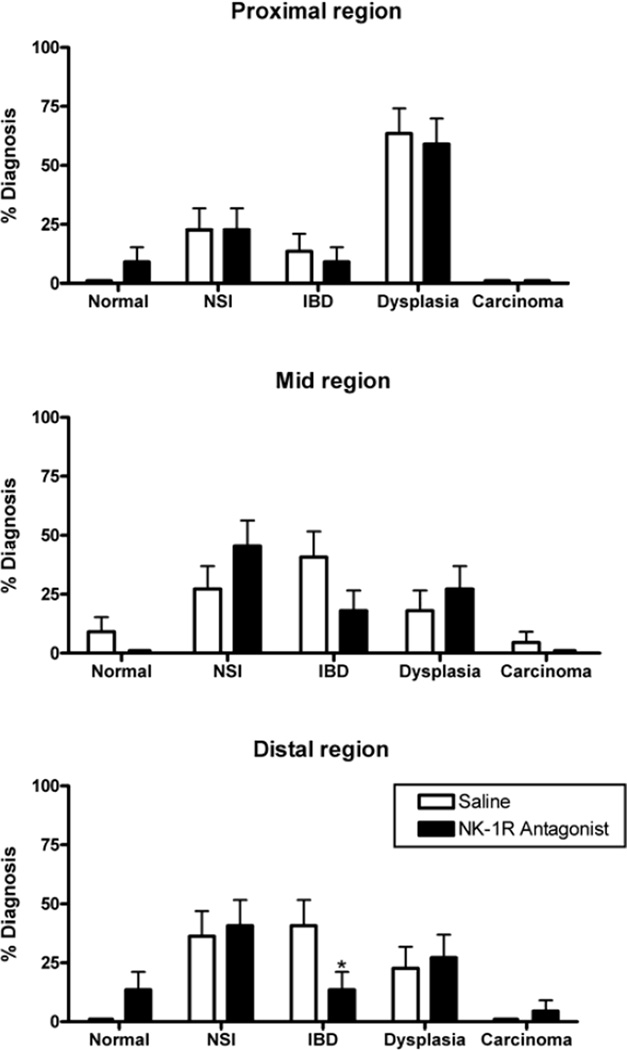
Pathological analysis was carried out by a blinded pathologist to identify normal, inflamed (IBD and non-specific inflammation), dysplasic, and carcinomic regions. Analysis revealed that 77% of the vehicle-treated animals had dysplasia in any region of the colon and 4.5% had carcinoma. In the NK-1R antagonist-treated group, 72% of the animals had dysplasia in some area of the colon, with twice as many animals having a completely normal diagnosis (18% versus 9% in the vehicle-treated group).
When the occurrence of dysplasia was compared within each of the different regions of the colon, no significant differences between the two treatment groups were found; however, those animals treated with the NK-1R antagonist had decreased incidence of IBD (Figure 2). This was most notable in the mid and distal regions of the colon (9%, 19%, and 14% in the proximal, mid, and distal regions versus 14%, 41%, and 41%, respectively, in vehicle-treated controls), reaching significance in distal colon (Figure 2). This, combined with the increase in the number of animals diagnosed as being normal, confirms previous studies that demonstrated an important role of NK-1R in inflammation (11).
Figure 2.
Effect of an NK-1R antagonist on pathological analysis in an animal model of colitis-associated dysplasia. The percentage of animals with the most severe diagnosis found in each region of the colon is shown (*p < 0.05 versus vehicle-treated animals; n = 22 per group). NSI, non-specific inflammation; IBD, inflammatory bowel disease.
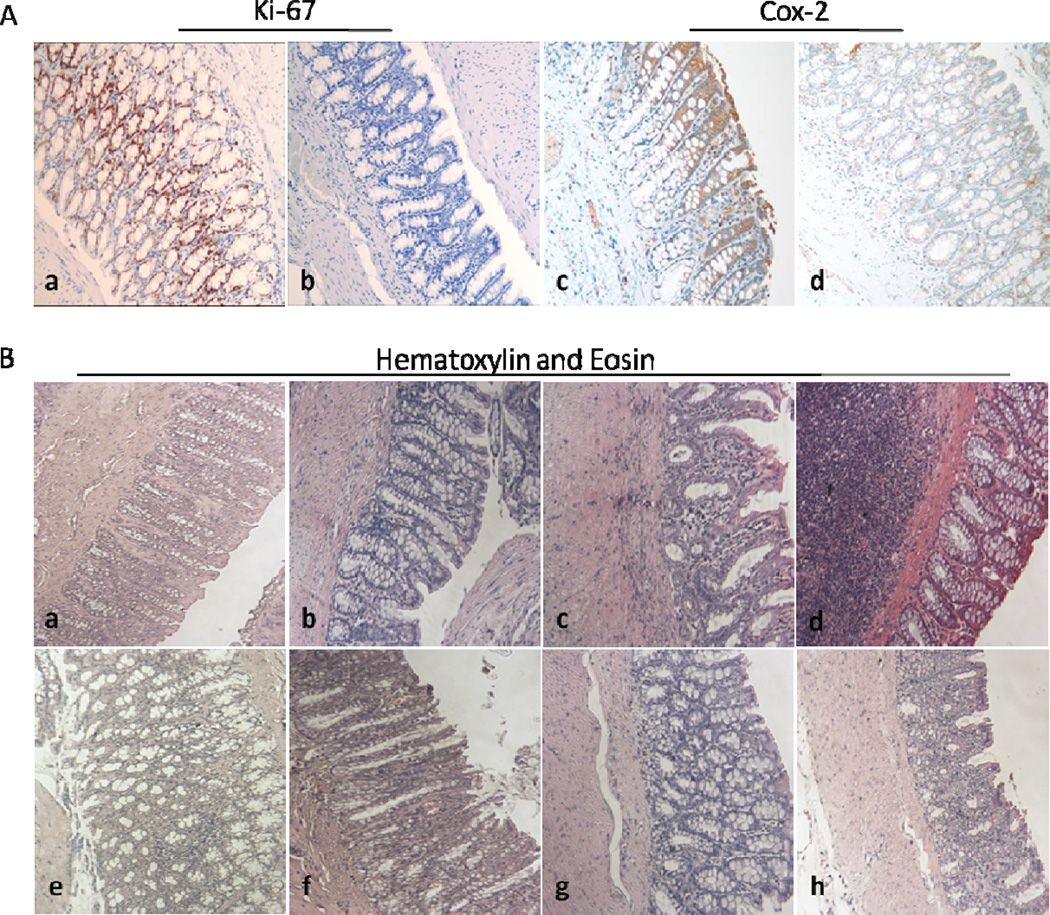
NK-1R antagonist decreased cell proliferation and Cox-2 expression
The proliferation of colon cells was examined using Ki67, a cellular marker for proliferation. Rats treated with the antagonist showed decreased expression of the Ki67 protein compared with that shown in the vehicle-treated group (Figure 3A, 4.30±1.24 vs. 7.67±0.52; p < 0.05; n = 9–10). Animals treated with the NK-1R antagonist showed decreased expression of Cox-2 compared with that shown in the vehicle-treated group (Figure 3A, 3.27±0.29 vs. 5.13±0.61; p < 0.01; n = 16). Although staining showed decreased expression of NK-1R and pSrc-pY416 in the NK-1R antagonist-treated group, this did not reach significance. Staining for EGFR and Erk1/2 activation showed no significant difference between the two treatment groups.
Figure 3.
Representative immunohistochemistry and hematoxylin and eosin staining for NK-1R antagonist-treated and untreated animals (×200). (A). Immunohistochemical analyses of Ki67 and Cox-2 was used to compare expression levels in NK-1R antagonist-treated group versus vehicle-treated group. (a) Ki67 expression in vehicle-treated, (b) Ki67 expression in antagonist-treated, (c) Cox-2 expression in vehicle-treated, and (d) Cox-2 expression in antagonist-treated. (B). Hematoxylin and eosin staining of (a) non-specific inflammation in vehicle-treated, (b) normal diagnosis in antagonist-treated, (c) IBD diagnosis in vehicle-treated, (d) IBD diagnosis in antagonist-treated, (e) low-grade dysplasia diagnosis in vehicle-treated, (f) low-grade dysplasia diagnosis in antagonist-treated, (g) high-grade dysplasia diagnosis in vehicle-treated, and (h) high-grade dysplasia diagnosis in antagonist-treated animals.
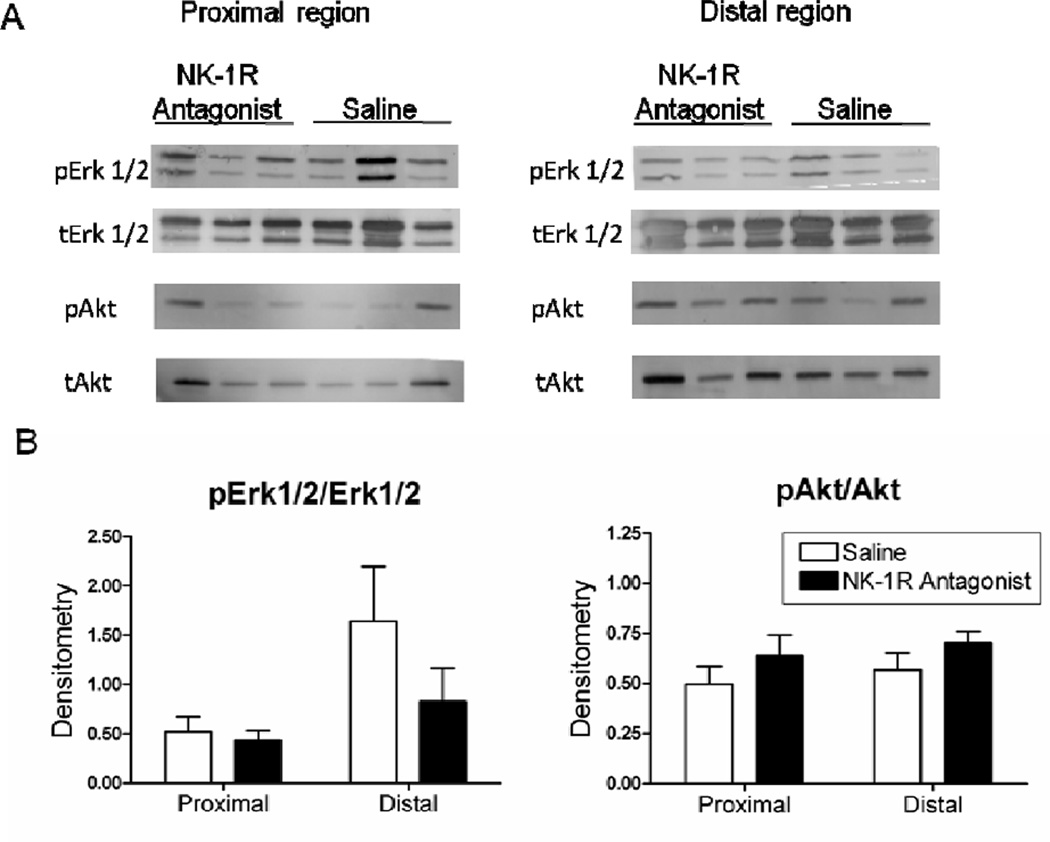
Erk1/2 pathway was down-regulated by blockade of NK-1R
Erk1/2 and Src were used as markers for MAPK kinase pathway activation, and Akt was used as a marker for anti-apoptosis pathway activation using Western blot analysis. Animals treated with the NK-1R antagonist showed a small decrease in the ratio p-Erk1/2/Erk1/2 and pSrc-pY416/Src versus that shown in the vehicle-treated group in both proximal and distal regions (Figure 4, and data not shown). In contrast, the ratio of p-Akt/Akt was unchanged in animals treated with the NK-1R antagonist compared with the vehicle-treated group (Figure 4).
Figure 4.
Effect of the NK-1R antagonist in an animal model of colitis-associated dysplasia on MAPK kinase components. (A). Tissues from proximal and distal region of rats treated with the NK-1R antagonist or with saline were ground, and equal amounts of protein (30 µg) were fractionated by SDS-12% PAGE before analysis by Western blot. Antibodies against pErk1/2, Erk1/2, pAkt, and Akt were used. Representative samples from 3 independent rats per group are shown. (B). Densitometry was performed with ImageQuant 5.2 software (Typhoon 9410) (n = 8–9± SEM).
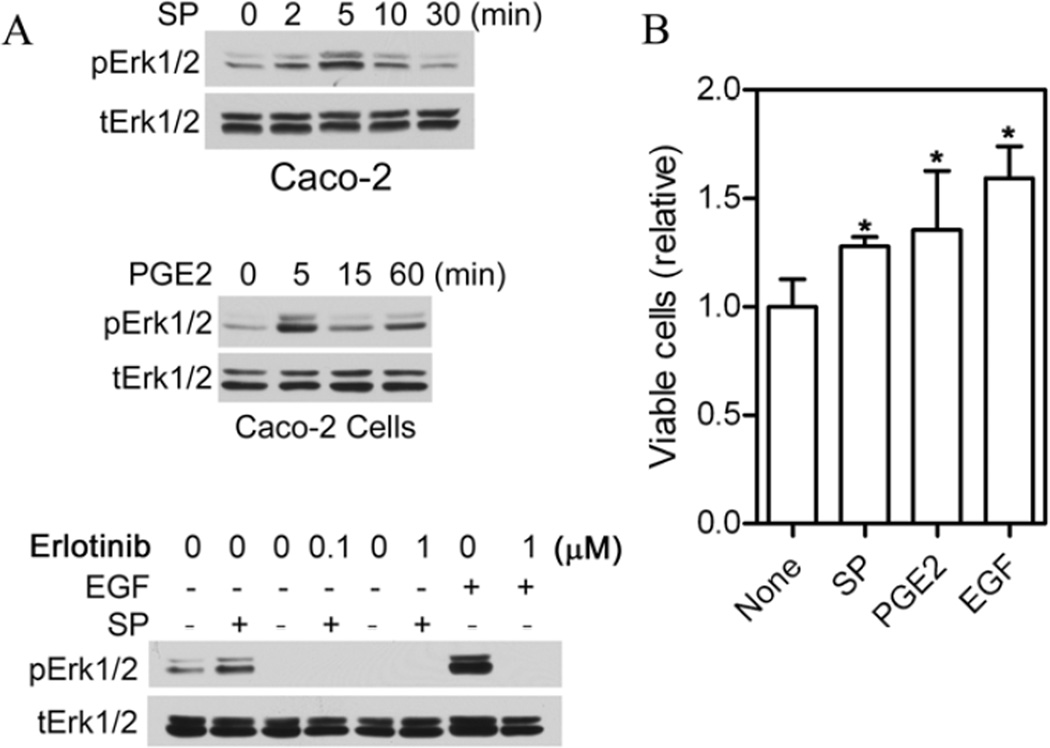
SP, PGE2, and EGF activated Erk1/2 and stimulated proliferation of Caco-2 cells
To further analyze the effects of the NK-1R ligand SP and the Cox-2 product PGE2 on Erk1/2 activation and proliferation of colon epithelial cells, Caco-2 cells were treated with SP and PGE2 and Erk1/2 and cell proliferation were determined. As shown in Figure 5, both SP and PGE2 induced Erk1/2 activation in Caco-2 cells, which peaked at 5 min. SP-stimulated Erk1/2 activation was blocked by the EGFR tyrosine kinase inhibitor erlotinib. Incubation of cells with SP, PGE2, and EGF also resulted in significantly increased cell numbers in the cell proliferation assay (p = 0.046, 0.0098, and <0.0001 respectively; Figure 5B).
Figure 5.
SP, PGE2, and EGF activate Erk1/2 and stimulate proliferation of Caco-2 cells. (A). Near confluent Caco-2 cells were serum-starved overnight, pre-treated with or without erlotinib (30 min at the indicated concentrations), and stimulated with SP (100 nM), PGE2 (5 µM), or EGF (5 ng/ml) or mock-treated for the indicated times or for 5 min (bottom panel). (B). Caco-2 cell proliferation assayed as described in Materials and Methods; *p<0.05 vs none).
Discussion
It is well known that patients with long-standing IBD run an increased risk of developing colorectal cancer. In these patients, colorectal cancer is responsible for 15% of all deaths (25). Many factors contribute to increasing the risk of this cancer, such as the duration of disease, the anatomic extent of disease, age at onset, disease activity, family history of colon cancer, and primary sclerosing cholangitis (26). Inflammation appears to be a common denominator among these factors, suggesting a potential role in carcinogenesis. Many possible pathways have been suggested and described in the literature.
The role of NK-1R in IBD has been studied in both in vitro and in vivo models (6, 11). SP and NK-1R appear to be up-regulated in dextran sulfate sodium and TNBS models during acute and chronic colitis (6–10). In the dextran sulfate sodium model, peripheral blood levels of SP were increased during acute colitis (27). Other studies that used this model have shown that administration of an NK-1R antagonist decreased colonic inflammation, as demonstrated by decreased disease activity index, mucosal myeloperoxidase activity, and colonic tissue damage score (10). During the acute phase of TNBS-induced colitis, NK-1R-deficient mice showed less histologic inflammation (28). Despite this evidence, the role of this receptor during long-standing colitis is still unknown. SP-NK-1R has been found to have an important function in the pathophysiology of the disease. It has been demonstrated in both human IBD and in this animal model, that NK-1R is expressed in dysplasia (29). Up-regulation of NK-1R protein expression correlated with a diagnosis of IBD, dysplasia, and colorectal cancer, with significantly higher up-regulation in those tissues with a diagnosis of dysplasia (30). In the present study, the results showed a significant decrease in both macroscopic and microscopic damage scores in animals treated with the NK-1R antagonist. Interestingly, IBD and nonspecific inflammation were found in both groups, treated and untreated, but only the NK-1R antagonist group showed a significant decrease in the IBD diagnosis. This suggests a possible use of the NK-1R antagonist as a treatment for patients with long-standing ulcerative colitis.
NK-1R and its ligand can cause the activation of MAPKs by transactivation of the EGFR via a metalloproteinase-dependent pathway, mediating many cellular functions, such as cell proliferation, cell-cycle arrest, terminal differentiation, and apoptosis. Because of that activation, it was hypothesized that NK-1R and EGFR-signaling pathways play critical roles in the development of colitis-associated dysplasia. In this study, no significant decrease in overall dysplasia was found. A concentration of 1 mg/kg, administered intraperitoneally two times per week was used, based on the beneficial effects that other investigators had found in treating colonic hypersensitivity (31). More recently, a higher dose (10 mg/kg per day, orally) has been shown to offer protection against the development of acute IBD in rats (9). It is possible that future studies using a higher dose of the antagonist would confirm the trend towards a decrease in the transition of inflammation to dysplasia observed in our animals.
The study presented here also demonstrates the possible role of Cox-2 in the development of dysplasia in this animal model. Animals with a higher incidence of dysplasia showed a greater expression of Cox-2 in the colon, which corroborates a similar increase in expression that we recently demonstrated in patients with dysplasia (30). Among the subset of animals analyzed for Cox-2 expression, 38% of animals treated with the NK-1R antagonist had dysplasia compared with 56% of animals treated with the vehicle. This finding correlates with studies that have indicated the existence of crosstalk between Cox-2 and EGFR contributing to the process of carcinogenesis via angiogenesis, apoptosis, cell proliferation, and invasiveness (31). At the same time, vehicle-treated animals showed increased expression of the Ki67 protein, a protein that is active in all phases of the cell cycle. These increases in Cox-2 and the Ki67 protein were significantly reduced by the administration of the NK-1R antagonist.
Previous studies have shown a role for the SP-NK-1R-EGFR pathway in inflammation (6, 32). Here, it was also demonstrated that a novel NK-1R antagonist ameliorated the inflammation. In vitro, cells stimulated with SP showed increased Erk1/2 activation; however, this activation was blocked by an EGFR inhibitor, suggesting crosstalk between SP and EGFR. Since the EGFR pathway is involved in proliferation mediated by SP (33), the possible role of the SP-NK-1R-EGFR pathway in the transition of inflammation to dysplasia was further analyzed. The expression of the downstream components of EGFR, including Erk1/2, Akt, and pSrc-pY416, was measured. Among these components, it was found that Erk1/2 activation was decreased in animals treated with the NK-1R antagonist. Other groups studying colonic inflammation, using a different NK-1R antagonist or a tumor necrosis factor-α-converting enzyme, have shown decreases in both Akt and Erk1/2 activation in human colonocytes (6, 32).
In conclusion, this study demonstrated that an NK-1R antagonist may be an effective treatment for long-standing colitis in that it ameliorates the damage that characterizes the disease. Further studies are needed to ascertain whether it may be possible to reduce the occurrence of dysplasia in a given target population by administering the drug at a higher concentration.
Acknowledgements
The authors thank Drs. Richard J. Noel and Pedro Santiago for molecular advice in this study and the technical assistance of Alcira Benitez Barros, Sandra Livingston, Edelmarie Rivera, and Genovés Rosario Soto. We also thank Rasa G. Hamilton for editorial assistance.
This work was supported by the National Institutes of Health (F31 GM078951 to B.P., U56 CA126379 to A.A.I. and C.B.A., and U56CA118809 to Z.C., Y.R. and J.W.).
Footnotes
Preliminary data from this study were previously presented at the Annual Meeting of the American Gastroenterological Association (Chicago, 2009).
References
- 1.Baumgart DC. What’s new in inflammatory bowel disease in 2008? World J Gastroenterol. 2008;14:329–330. doi: 10.3748/wjg.14.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elson CO, Balfour-Sartor R, Tennyson GS, Riddell RH. Experimental models of inflammatory bowel disease. Gastroenterology. 1995;109:1344–1367. doi: 10.1016/0016-5085(95)90599-5. 1995. [DOI] [PubMed] [Google Scholar]
- 3.Greenstein AJ. Cancer in inflammatory bowel disease. Mt Sinai J Med. 2000;67:227–240. [PubMed] [Google Scholar]
- 4.Munkholm P. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:1–5. doi: 10.1046/j.1365-2036.18.s2.2.x. [DOI] [PubMed] [Google Scholar]
- 5.Pernow B. Substance P. Pharmacol Rev. 1983;35:85–141. [PubMed] [Google Scholar]
- 6.Koon HW, Zhao D, Na X, Moyers MP, Pothoulakis C. Metalloproteinases and transforming growth factor-α mediate substance P-induced mitogen-activated protein kinase activation and proliferation in human colonocytes. J Biol Chem. 2004;279:45519–45527. doi: 10.1074/jbc.M408523200. [DOI] [PubMed] [Google Scholar]
- 7.Catagliuolo I, Keates AC, Qiu B, Kelly CP, Nikulasson S, Leeman SE, Pothoulakis C. Increased substance P responses in dorsal root ganglia and intestinal macrophages during Clostridium difficile toxin A enteritis in rats. Proc Natl Acad Sci USA. 1997;94:4788–4793. doi: 10.1073/pnas.94.9.4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Sebastiano P, Grossi L, Di Mola D, Angelucci D, Friess H, Marzio L, Innocenti P, Büchler MW. SR140333, a substance P receptor antagonist, influences morphological and motor changes in rat experimental colitis. Dig Dis Sci. 1999;44:439–444. doi: 10.1023/a:1026639509036. [DOI] [PubMed] [Google Scholar]
- 9.Ursino MG, Vasina V, De Ponti F. Protection from DNBS-induced colitis by the tachykinin NK(1) receptor antagonist SR140333 in rats. Eur J Pharmacol. 2009;603:133–137. doi: 10.1016/j.ejphar.2008.11.064. [DOI] [PubMed] [Google Scholar]
- 10.Stucchi AF, Shofer S, Leeman S, Materne O, Beer E, McClung J, Shebani K, Moore F, O'Brien M, Becker JM. NK-1 antagonist reduces colonic inflammation and oxidative stress in dextran sulfate-induced colitis in rats. Am J Physiol Gastrointest Liver Physiol. 2000;279:G1298–G1306. doi: 10.1152/ajpgi.2000.279.6.G1298. [DOI] [PubMed] [Google Scholar]
- 11.Appleyard CB, Morales M, Santiago C. Chronic inflammation alters the contribution of neurokinin receptor subtypes to epithelial function in rat colon. Dig Dis Sci. 2008;53:220–228. doi: 10.1007/s10620-007-9847-8. [DOI] [PubMed] [Google Scholar]
- 12.Palma C, Nardelli F, Manzini S, Maggi CA. Substance P activates responses correlated with tumour growth in human glioma cell lines bearing tachykinin NK1 receptors. Br J Cancer. 1999;79:236–243. doi: 10.1038/sj.bjc.6690039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castagliuolo I, Valenick L, Liu J, Pothoulakis C. Epidermal growth factor receptor transactivation mediates substance P-induced mitogenic response in U-373 MG cells. J Biol Chem. 2000;34:26545–26550. doi: 10.1074/jbc.M003990200. [DOI] [PubMed] [Google Scholar]
- 14.Solomon MJ, Schnitzler M. Cancer and inflammatory bowel disease: bias, epidemiology, surveillance, and treatment. World J Surg. 1998;22:352–358. doi: 10.1007/s002689900396. [DOI] [PubMed] [Google Scholar]
- 15.Wang J-G, Wang D-F, Lv B-J, Si J-M. A novel mouse model for colitis-associated colon carcinogenesis induced by 1,2-dimethylhydrazine and dextran sulfate sodium. World J Gastroenterol. 2004;10:2958–2962. doi: 10.3748/wjg.v10.i20.2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohno H, Suzuki R, Sugie S, Tanaka T. Suppression of colitis-related mouse colon carcinogenesis by a COX-2 inhibitor and PPAR ligands. BMC Cancer. 2005;5:46. doi: 10.1186/1471-2407-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper HS, Murthy S, Kido K, Yoshitake H, Flanigan A. Dysplasia and cancer in the dextran sulfate sodium mouse colitis model. Relevance to colitis-associated neoplasia in the human: a study of histopathology, β-catenin and p53 expression and the role of inflammation. Carcinogenesis. 2000;21:757–768. doi: 10.1093/carcin/21.4.757. [DOI] [PubMed] [Google Scholar]
- 18.Clapper ML, Cooper HS, Chang WC. Dextran sulfate sodium-induced colitis-associated neoplasia: a promising model for the development of chemopreventive interventions. Acta Pharmacol Sin. 2007;28:1450–1459. doi: 10.1111/j.1745-7254.2007.00695.x. [DOI] [PubMed] [Google Scholar]
- 19.Santiago C, Pagán B, Isidro AA, Appleyard CB. Prolonged chronic inflammation progresses to dysplasia in a novel rat model of colitis-associated colon cancer. Cancer Res. 2007;67:10766–10773. doi: 10.1158/0008-5472.CAN-07-1418. [DOI] [PubMed] [Google Scholar]
- 20.Appleyard CB, Wallace JL. Reactivation of hapten-induced colitis and its prevention by anti-inflammatory drugs. Am J Physiol Gastrointest Liver Physiol. 1995;269:G119–G125. doi: 10.1152/ajpgi.1995.269.1.G119. [DOI] [PubMed] [Google Scholar]
- 21.Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Lantz PE, Listrom MB, Rilke FO. Gastrointestinal Pathology, an Atlas and Text. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999. Inflammatory bowel disease; pp. 631–716. [Google Scholar]
- 22.Allred DC, Clark GM, Elledge R, Fuqua SA, Brown RW, Chamness GC, Osborne CK, McGuire WL. Association of p53 protein expression with tumor cell proliferation rate and clinical outcome in node-negative breast cancer. J Natl Cancer Inst. 1993;85:200–206. doi: 10.1093/jnci/85.3.200. [DOI] [PubMed] [Google Scholar]
- 23.Meng S, Chen Z, Munoz-Antonia T, Wu J. Participation of both Gab1 and Gab2 in the activation of the ERK/MAPK pathway by epidermal growth factor. Biochem J. 2005;391:143–151. doi: 10.1042/BJ20050229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karagiannides I, Torres D, Tseng Y-H, Bowe C, Carvalho E, Espinoza D, Pothoulakis C, Kokkotou E. Substance P as a novel anti-obesity target. Gastroenterology. 2008;134:747–755. doi: 10.1053/j.gastro.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Itzkowitz S, Harpaz N. Diagnosis and management of dysplasia in patients with inflammatory bowel disease. Gastroenterology. 2004;126:1634–1648. doi: 10.1053/j.gastro.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 26.Herszenyi L, Miheller P, Tulassay Z. Carcinogenesis in inflammatory bowel disease. Dig Dis. 2007;25:267–269. doi: 10.1159/000103898. [DOI] [PubMed] [Google Scholar]
- 27.Castagliuolo I, Morteau O, Keates AC, Valenick L, Wang CC, Zacks J, Lu B, Gerard NP, Pothoulakis C. Protective effects of neurokinin-1 receptor during colitis in mice: role of the epidermal growth factor receptor. Br J Pharmacol. 2002;136:271–279. doi: 10.1038/sj.bjp.0704697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Niess JH, Mönnikes H, Dignass AU, Klapp BF, Arck PC. Review on the influence of stress on immune mediators, neuropeptides and hormones with relevance for inflammatory bowel disease. Digestion. 2002;65:131–140. doi: 10.1159/000064933. [DOI] [PubMed] [Google Scholar]
- 29.Rosso M, Robles-Frías MJ, Coveñas R, Salinas-Martín MV, Muñoz M. The NK-1 receptor is expressed in human primary gastric and colon adenocarcinomas and is involved in the antitumor action of L-733,060 and the mitogenic action of substance P on human gastrointestinal cancer cell lines. Tumour Biol. 2008;29:245–254. doi: 10.1159/000152942. [DOI] [PubMed] [Google Scholar]
- 30.Isidro RA, Cruz ML, Rodríguez VA, Isidro AA, Arroyo A, Baez A, Appleyard CB. Neurokinin-1 receptor (NK-1R), phosphorylated epidermal growth factor receptor (pEGFR) and cyclooxygenase-2 (Cox-2) are up-regulated in patients with colonic dysplasia. Gastroenterology. 2010;138(5 suppl 1):S286–S287. [Google Scholar]
- 31.Schwetz I, Bradesi S, McRoberts JA, Sablad M, Miller JC, Zhou H, Ohning G, Mayer EA. Delayed stress-induced colonic hypersensitivity in male Wistar rats: role of neurokinin-1 and corticotropin-releasing factor-1 receptors. Am J Physiol Gastrointest Liver Physiol. 2004;286:G683–G691. doi: 10.1152/ajpgi.00358.2003. [DOI] [PubMed] [Google Scholar]
- 32.Koon HW, Zhao D, Zhan Y, Rhee SH, Moyer MP, Pothoulakis C. Substance P stimulates cyclooxygenase-2 and prostaglandin E2 expression through JAK-STAT activation in human colonic epithelial cells. J Immunol. 2006;176:5050–5059. doi: 10.4049/jimmunol.176.8.5050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koon HW, Zhao D, Zhan Y, Moyer MP, Pothoulakis C. Substance P mediates antiapoptotic responses in human colonocytes by Akt activation. Proc Natl Acad Sci USA. 2007;104:2013–2018. doi: 10.1073/pnas.0610664104. [DOI] [PMC free article] [PubMed] [Google Scholar]