Abstract
Improvement in treatment has led to decreased death in youth with human immunodeficiency virus (HIV) in developed countries. Despite this, youth with HIV are still at risk for increased mortality and morbidity compared with their uninfected counterparts. In developing countries, high numbers of youth die from acquired immune deficiency syndrome (AIDS)-related illnesses due to lack of access to consistent antiretroviral treatment. As a result, pediatric palliative care is a relevant topic for those providing care to youth with HIV. A systematic review was conducted to gather information regarding the status of the literature related to pediatric palliative care and medical decision-making for youth with HIV. The relevant literature published between January 2002 and June 2012 was identified through searches conducted using PubMed, CINAHL, Scopus, and PSYCInfo databases and a series of key words. Articles were reviewed by thematic analysis using the pillars of palliative care set out by the National Consensus Project. Twenty-one articles were retained after review and are summarized by theme. In general, few empirically based studies evaluating palliative care and medical decision-making in youth with HIV were identified. Articles identified focused primarily on physical aspects of care, with less attention paid to psychological, social, ethical, and cultural aspects of care. We recommend that future research focuses on broadening the evaluation of pediatric palliative care among youth with HIV by directly evaluating the psychological, social, ethical, and cultural aspects of care and investigating the needs of all involved stakeholders.
Keywords: pediatric palliative care, human immunodeficiency virus, acquired immune deficiency syndrome, advance care planning, medical decision-making
Introduction
The World Health Organization has defined palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness”.1 This approach takes place through careful assessment and subsequent treatment of physical, psychosocial and spiritual problems. Palliative care is now conceived of as “both a philosophy of care and an organized, highly structured system for delivering care”,2 a definition broadened beyond services for only those imminently dying, as modern medicine has changed diseases which were once a death sentence into complex chronic conditions. Palliative care involves a multidisciplinary team to address multifaceted areas of an individual’s functioning and can be delivered in many settings, including outpatient clinics, inpatient hospitals, hospice care at home, and specialty facilities. The National Consensus Project has defined domains of palliative care to include: the structure and process of care; physical aspects of care; psychologic aspects of care; social aspects of care; spiritual and religious aspects of care; specific cultural aspects of care; care of the imminently dying patient; and ethical and legal issues associated with providing palliative care (see Table 1).
Table 1.
Operational definitions of domains of palliative care
| Structure and process of care | Developing a plan of care with the family, including how care will be delivered, where care will be delivered, and by whom |
| Ongoing training and education for palliative care providers | |
| Physical aspects of care | Pain management |
| Other aspects of medical care provided to the patient | |
| Psychological aspects of care | Coping with associated mental health conditions as a result of the patient’s condition |
| Grief and bereavement services for the patient and family | |
| Social aspects of care | Social needs of the palliative care patient |
| Implications of the patient’s condition for their social functioning | |
| Spiritual and religious needs, including existential questions and exploration | Spiritual and religious aspects of care |
| Cultural aspects of care | Unique language, rituals, or customs of the patient’s culture |
| Practicing culturally competent palliative care provision | |
| Care of the imminently dying patient | Specific needs of the patient who may have signs and symptoms of imminent death |
| Signs are communicated to the family | |
| Plan of care specific to this timeframe is developed | |
| Ethical and legal issues | Review of regulatory and local, state, and federal laws with the goal of respecting the patient’s needs and goals for palliative care |
Note: This table is based on the domains of palliative care described by the National Consensus Project of Quality Palliative Care.2
Over the last decade, substantial improvements have been made in the treatment of pediatric human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS), such that far fewer youth are facing an early death from the disease. Nevertheless, an estimated 250,000 children under the age of 15 years died of AIDS-related causes in 2010 worldwide,3 and 11% of adolescent (10–24 years) deaths were due to HIV/AIDS and tuberculosis.4 Although progress expanding children’s access to antiretroviral therapy is being made, only one quarter of children needing treatment received it in 2010.3 Sub-Saharan Africa has a disproportionate share of the burden.3 Among youth with perinatally acquired HIV in the United States, survival rates for earlier birth cohorts (1989–1993 and 1994–1996) are lower than for those later on (1997–2001), and children with a prior AIDS-defining condition are less likely to survive to an older age.5 Similar findings for long-term outcomes in adolescents perinatally infected with HIV-1 followed since birth are reported in the French Perinatal Cohort.6 Advanced HIV puts youth at risk for experiencing possible negative medical complications that may render them unable to speak for themselves in times of medical decision-making. Thus, pediatric palliative care is relevant for youth living with HIV. However, limited research has investigated the provision of palliative care for youth with HIV. The goal of this systematic review is to fill this gap in order to outline current practices, perspectives, and effects of pediatric palliative care for youth living with HIV.
Materials and methods
We conducted a systematic review of the peer-reviewed published literature on palliative care for children/adolescents published between January 2002 and June 2012.
Eligibility criteria
Final eligibility criteria included: studies with an explicit focus on palliative care or medical decision-making; original study (quantitative or qualitative); studies including children or adolescents diagnosed with HIV; and published in English between January 1, 2002 and June 30, 2012. Papers published prior to January 2002 or after June 30, 2012, in which HIV/AIDS was not the primary illness identified, end-of-life care was not included, and the primary focus did not include youth with HIV/AIDS were excluded.
All articles generated by these searches were compiled and duplicates were eliminated. Titles and abstracts were reviewed, and if the source met the inclusion criteria, the full article was obtained and evaluated. Abstracts that did not include enough data for adequate review of the inclusion/exclusion criteria were also retained for full article review. In order to account for possible limitations in electronic databases, bibliographies of identified articles were also reviewed for articles relevant to the review that met the study inclusion/exclusion criteria. For validation purposes, the study selection criteria were applied by one author and then reviewed by another author. Information from the articles was extracted and synthesized using the domains of palliative care as an organizational framework for thematic analysis. Themes across these studies were identified and compared. A total of 21 articles were summarized in this review after the selection process was complete.
Search strategy
Four electronic databases, ie, PubMed, CINAHL, Scopus, and PSYCInfo, were used to identify relevant literature published between January 2002 and June 2012. The preliminary searches of articles with at least one palliative care-related descriptor identified relevant descriptors and key words. The search terms were then agreed on collaboratively by the authors and by consultation with experts in pediatric palliative care. A search filter was applied for publication language (English only), publication date (2002–2012) and age group (children and adolescents).
The following search terms were used: “HIV and palliative care and adolescence”, “AIDS and palliative care and adolescence”, “HIV and end of life care and adolescence”, “AIDS and end of life care and adolescence”, “HIV and terminal care and adolescence”, “AIDS and terminal care and adolescence”, “HIV and palliative care and pediatrics”, “AIDS and palliative care and pediatrics”, “HIV and end of life care and pediatrics”, “AIDS and end of life care and pediatrics”, “HIV and terminal care and pediatrics”, “AIDS and terminal care and pediatrics”, “HIV and adolescence and medical decision making”, “AIDS and adolescence and medical decision making”, “adolescence and medical decision making”, and “pediatrics and medical decision making”.
Phase 1
A data collection tool created for this study that included, if available, authors, date of publication, article objectives, methods, design, setting, participants, intervention, results, conclusion, and palliative care domain(s), was used to import information from retrieved references.
Phase 2
One of two independent reviewers cross-checked abstracts for the eligibility criteria stated above, and disagreements were discussed and resolved by author consensus.
Phase 3
For the remaining list, full articles were reviewed in depth by the first reviewer to make final decisions about inclusion based on a priori eligibility criteria. A second reviewer further examined all articles excluded in this phase to reduce the possibility of exclusion error.
Phase 4
The reference lists of all included articles were screened further for relevant publications. Articles with relevant titles were reviewed following the outlined process. Articles published by one of the authors were independently reviewed by alternative authors to prevent bias.
Data extraction and assessment of study quality
Full articles were reviewed for systematic coding of the following study characteristics: study design, setting, country/region of origin, sample, evidence level, and National Consensus Project domains of palliative care.
Data synthesis
identified articles were synthesized using thematic analysis. This type of analysis was chosen to allow for integration of the varied types of data identified in the review.7,8 The domains of palliative care discussed above were selected a priori as the thematic framework to provide structure and organization for this review. For each article identified in the search, we extracted all findings that referred to the domains of palliative care. Findings were then summarized across studies into broader themes for each domain.
Results
Twenty-one articles were retained for review (see Figure 1). A summary of these articles can be found in Table 2. Eight were conducted in the United States, seven in Africa, and the remaining four did not specify their location because they were reviews, editorials, or policy articles. The ages of the participants ranged from birth to 28 years. Fifteen articles included original data, five were editorial, policy, or review articles, and one described the design and methods of a randomized controlled trial that was enrolling participants at the time of publication. Of the 14 articles that included original data, 13 were prospective, 11 were quantitative designs, and one included mixed-methods methodology. Only one randomized controlled trial was identified, but without blinding and on a small sample (38 youth with HIV). The majority of original data studies were cross-sectional designs or retrospective data reviews, using qualitative or quantitative methodologies.
Figure 1.
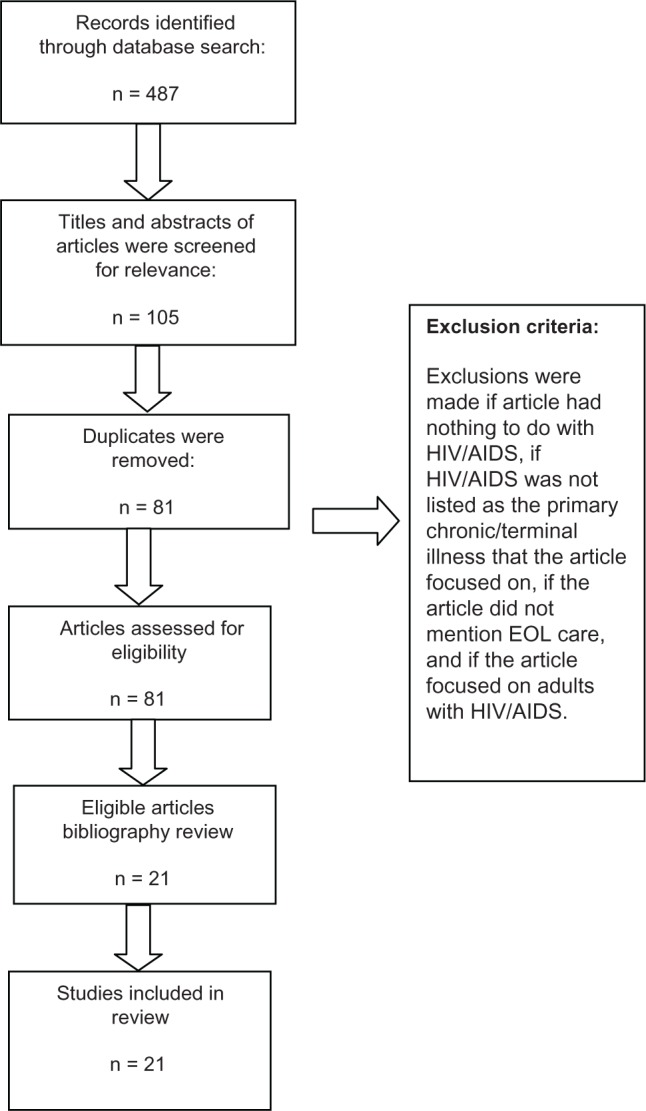
Process used for selection of papers included in this review.
Abbreviations: AIDS, acquired immune deficiency syndrome; EOL, end-of-life; HIV, human immunodeficiency virus.
Table 2.
Summary of key points in papers included in review
| Study | Objective/s | Method | Participants | Location | Conclusion | Pillar(s) of palliative care |
|---|---|---|---|---|---|---|
| De Baets et al10 | To strengthen the position of health care works of district hospitals by summarizing rationale for pediatric HIV care and treatment, identifying gaps in knowledge, and identifying needs for palliative care (pain relief and emotional support) | Position paper | Pediatric patients with HIV, aged 0–14 years | Sub-Saharan Africa | Recommendations: Provide critical (non-ART) interventions for HIV-infected children, even if ART not available Provide emotional support, pain relief, and palliative care for children with terminal AIDS Provide psychosocial support for caregivers and health care providers who care for HIV-infected children at the end of life Provide care at the district hospital level Stop limiting pediatric HIV care to tertiary hospitals where access is limited by poverty and/or lack of transportation |
Physical Psychological Imminently dying |
| Collins and Harding9 | To measure the multidimensional palliative care needs of patients in Muheza, Tanzania | Prospective chart review | Mean age 35.4 ± 13.7 years, receiving care at a hospital clinic | Tanzania | Even in the presence of ART, palliative care continues to be an important part of HIV programs Need to provide specialist pediatric palliative care skills in the HIV context | Physical Psychological Spiritual/religious Imminently dying |
| No authors listed11 | Editorial report examining the findings of the human rights report “Needless Pain: Failure to Provide Palliative Care for Children in Kenya” | Position paper | Children with cancer, HIV/AIDS, or sickle cell anemia | Kenya | Access to oral morphine should be improved immediately and a plan of action on how to scale up palliative care should be implemented Legal obligations to ensure the child’s right to the highest attainable standard of health are not being adhered to in Kenya | Physical Imminently dying Ethical/legal |
| Lavy15 | Baseline study to determine the prevalence of symptoms in children referred for palliative care in Malawi | Retrospective chart review, and prospective, observational survey | Children (n = 95; 4 months to 16 years) referred to a pediatric palliative care team 77% were diagnosed with HIV/AIDS, 17% with cancer, and 6% other illness | Malawi | Children with HIV presented with a larger variety of symptoms, reflecting the need to address a wide range of problems Palliative care focusing on pain did not seem to be important in this sample, but pain was not assessed in a structured way Health care needs to include relief of symptoms that are causing distress, and be holistic, addressing the associated physical, emotional, and social problems |
Physical Imminently dying Ethical/legal |
| Onuoha et al23 | To examine the mental health of children whose parents have died of AIDS in Uganda and South Africa | Prospective, observational | Children aged 0–17 years who have lost at least one parent to AIDS (n = 373), orphaned for other reasons (n = 287), or not orphaned (n = 290) | Uganda and South Africa | AIDS-orphaned children had highest negative mental health state because of higher rates of double parental loss Natural mentorship was palliative against negative mental health | Physical Imminently dying Ethical/legal |
| Richter et al13 | To describe ways to develop simple, low-cost, and context-relevant interventions to improve hospital care for children living with HIV/AIDS and poverty | Qualitative interview | Children hospitalized with HIV/AIDS (no participant demographics included) | South Africa | Data from the evaluation phase have not been published at the time of this review | Physical Social |
| Malloy et al12 | To showcase the activities of ELNEC-PPC trainers and demonstrate their commitment to improving palliative care at their institutions and at local, state, national, and international levels | Position paper | Description of nurse training programs for end-of-life care | US | ELNEC-PCC helps nurses by extending palliative care principles across settings to improve care; achieve quality of life at end of life; finding meaning, communication, and decision-making; pain and symptom management; providing bereavement and supporting nurses | Other education/training of nurses to provide pediatric palliative care |
| Chenneville et al27 | To evaluate the relationship among decisional capacity, developmental stage, intellectual ability and social-emotional functioning in children with and without HIV | Prospective, observational | Children (aged 7–17 years) with HIV (n = 25) and without HIV (n = 25) Convenience sample recruited from two infectious diseases outpatient clinics and from local family health clinics Sample included 60% ethnic minorities |
US | No significant differences were observed when comparing the decisional capacity of those with HIV versus those without HIV Developmental level was significantly related to decisional capacity, which is consistent with typically developing population research Results support children living with HIV having the capacity to participate meaningfully in their health care decisions despite intellectual and adaptive functioning deficits |
Psychological Social Cultural Ethical/legal |
| Allen and Sorensen Marshall30 | To provide an overview of palliative care provision for children with HIV/AIDS | Position paper | Focused on children with HIV/AIDS needing palliative care No specific sample measured | N/A | Provided review of HIV, HIV in children, and global perspective of HIV/AIDS Highlighted family concerns, including disclosure of diagnosis, physical needs and pain management, adherence with medication, transition from childhood to adulthood, financial concerns, and spiritual concerns Discussed vulnerability amongst children, future challenges, and implications for clinical practice Discussed need for more research on palliative care and HIV/AIDS |
Structure/processes Physical Psychological Social Spiritual/religious Cultural Imminently dying Ethical/legal |
| Kovacs et al31 | To define family-centered care, trends in care giving, and barriers to family-centered care To reintroduce family into the focus of care at end of life |
Position paper | Families dealing with end-of-life care | N/A | Review of history of palliative and HIV care Defined palliative care-related terms Trends in care giving reviewed Recommended advocates for family-centered care at the end of life for those with HIV Highlighted barriers to family-centered care at end of life Discussion of supporting caregivers included Summarized implications for social work practice |
Psychological Social Spiritual/religious Cultural Imminently dying |
| Blake et al28 | To identify ways to improve adolescent understanding of informed assent by exploring adolescent comprehension of research topics | Qualitative focus groups | 33 healthy adolescents (aged 15–17 years) in a community-based organization | US | Teens had the most difficulty with the concept of a placebo and randomization in the general research topic They also had difficulty understanding how a vaccine works and that it is preventative and not a treatment Regarding a HIV vaccine trial, teens had difficulty understanding/showed misunderstanding regarding the idea that an HIV antibody test might provide a false positive result for people who receive the HIV vaccine Teens indicated they wanted to be informed about adverse effects, procedures involved in the clinical trial, and if the research was novel or had been performed before |
Ethical/legal |
| Harding et al16 | To measure clinical outcomes when initiated on ART while in care at specialist pediatric hospice facility | Retrospective chart review | 37 children (mean age 5.5 years) who began ART during a six-month review period in 2006 | South Africa | Children initiated on ART in hospices/palliative care hospitals showed significant improvement in clinical outcomes Most were still alive and had a good virologic response ART thought to be an excellent palliative therapy, over and above just treating illness presentation |
Physical |
| Summers et al25 | To detail a recent case involving adolescent clinical care including ethical and legal issues faced by the patient’s physician | Case study | A 15 year-old girl who has been under the care of the same pediatrician since 5 years of age | US | Case analysis from perspective of related confidentiality and legal issues (emancipation, mature minor doctrine, and type of medical care the minor is seeking per state) Discussed what information should be provided to the patient regarding her rights and limits to her confidentiality financial issues of confidential care discussed (ie, potential for involuntary disclosure due to billing practices) Also reviewed cognitive development as a factor in determining the rights of adolescents and how to communicate with this age group |
Physical Psychological Social Ethical/legal |
| Amery et al14 | To evaluate children’s palliative care services in a resource-poor Sub-Saharan African setting | Retrospective chart review, prospective survey, qualitative interview | Respondents from a hospice and hospital setting Included all children using hospice services (n = 11), their legal guardians (n = 12), and all hospice and hospital staff on the ward (n = 10) |
Uganda | Study suggests child-focused palliative care services can be effectively and affordably provided in Sub-Saharan Africa Results suggest more effective than a combined program with adults Key elements: recruitment of children, provision of free and effective prescriptions for medications, provision of nutritional support, play and learning facilities, and effective systems for child protection Services seem affordable Staff need support and ongoing training |
Physical Psychological Social Cultural |
| Henley et al26 | To evaluate terminal care among hospitalized children who died of HIV/AIDS | Retrospective chart review | All patients (n = 165) who died from HIV/AIDS-related causes between February 1998 and June 2000 in a children’s hospital Mean age was 10 months |
South Africa | Despite clinical uncertainty, doctors made tough end-of-life decisions that included DNR orders and comfort care plans The lower rate of comfort care plans suggested doctors had difficulty making the transition from curative to palliative care Improving terminal care requires a shift in goals from prolonging life to palliation |
Physical Imminently dying |
| Lyon et al24 | To examine the frequency of DNR orders and hospice enrolment in children/adolescents living with AIDS and followed in PACTG for any association with racial disparities or enhanced quality of life, particularly psychologic adjustment | Prospective, observational | 726 children with AIDS (mean age 12.9 years) across 89 US hospitals | US | Children who died of AIDS rarely had DNR/hospice enrolment National guidelines recommend that quality palliative care be integrated routinely with HIV care Further research is needed to explore barriers to palliative care and advance care planning in this population |
Physical Psychological Cultural Imminently dying Ethical/legal |
| Lyon et al19 | To develop, adapt, and ensure feasibility, acceptability, and safety of the FACE advance care planning intervention | Randomized controlled trial | Adolescents aged 14–21 years with HIV/AIDS and surrogates/family members older than 20 years attending two hospital-based outpatient clinics in Washington, DC, and Memphis, TN from 2006 to 2008 | US | Existing advance care planning models can be adapted for age, disease, and culture Adolescents with HIV/AIDS were satisfied with an advance care planning approach that facilitated discussion about their end-of-life wishes with their families Families acknowledged a life-threatening condition and were willing to initiate end-of-life conversations when their adolescents were medically stable |
Psychological Cultural |
| Lyon et al21 | To test the effectiveness of a model of family/adolescent-centered advance care planning for adolescents living with HIV and their families for increasing congruence and quality of communication while decreasing decisional conflict | Randomized controlled trial | Adolescents aged 14–21 years with HIV/AIDS and surrogates/families over the age of 20 years attending two hospital-based outpatient clinics in Washington, DC, and Memphis, TN from 2006 to 2008 | US | Family-centered advance care planning by trained facilitators increased congruence in adolescent/surrogate preferences for end-of-life care, decreased decisional conflict, and enhanced communication quality Families acknowledged a life-threatening condition and were willing to initiate end-of-life conversations when their adolescents were medically stable |
Psychological Ethical/legal |
| Wiener et al17 | To explore whether adolescents and young adults living with a life-limiting illness find it acceptable and helpful to have a planning document to share their wishes and thoughts regarding end-of-life care If so, to learn about specific concerns adolescents and young adults feel are important to include in such a document | Qualitative interviews | Outpatient adolescents enrolled on NCI protocols, and aged 16–28 years with a diagnosis of either cancer or HIV | US | An advance care planning document may be appropriate and helpful for adolescents and young adults living with a serious illness Future research should further validate the preferences identified by participants and explore whether an age-appropriate document can improve communication with family and staff in end-of-life care |
Psychological Ethical/legal |
| Lindsey et al25 | To investigate the experiences of and impact on young girls and older women caring for family members living with HIV/AIDS and other chronic and terminal illnesses at home in three districts of Botswana | Qualitative interviews | 70 interviews with primary caregivers (n = 35) of people living with HIV/AIDS and other terminally or chronically ill family members at home Key informants, such as CHBC volunteers, family welfare educators, nurses, social workers, and members of nongovernmental organizations involved in CHBC, were included Data were collected from personnel at the Ministry of Health and researchers and consultants involved in issues related to CHBC |
Botswana | The burden of care for terminally and chronically ill family members on older women and younger girls is profound They must assume multiple and often overwhelming roles Poverty exacerbates these problems These caregivers feel isolated, lack necessary knowledge, and require effective and easily accessible psychosocial support In addition, the stigma of HIV/AIDS prevents adequate flow of information and care provision for these needy families Traditional medicine and spiritual healing played important roles in many of the families interviewed; however, the costs of this service could be crippling |
Psychological Social Spiritual/religious Ethical/legal |
| Dallas et al22 | To describe a clinical trial with the aim of evaluating the long-term efficacy of the FACE intervention with regard to congruence in end-of-life treatment between adolescents with HIV/AIDS and their family, decisional conflict about end-of-life decisions, quality of communication about care, and quality of life | Methods paper | No participants described Descriptive of methods only |
US | Trial enrolling participants at the time this review was written Offers description of a novel methodology compared with commonly implemented practices using a structured, theoretically grounded, and targeted intervention to facilitate advanced care planning Proposed/described clinical trial addresses many limitations of previous intervention work dealing with end-of-life care |
Physical Psychological Social Spiritual/religious Ethical/legal |
Abbreviations: AIDS, acquired immune deficiency syndrome; ART, antiretroviral therapy; DNR, do-not-resuscitate; HIV, human immunodeficiency virus; N/A, not applicable; ELNEC-PPC, End-of-Life Nursing Education Consortium for Pediatric Palliative Care; PACTG, Pediatric AIDS Clinical Trials Group; FACE, Family Adolescent-Centered; CHBC, community home-based care; NCI, National Cancer Institute.
Structure and process of care: planning of care, interdisciplinary teams, education, and training
Several articles addressed gaps in the structure and process of care for pediatric HIV patients in Sub-Saharan Africa. Interdisciplinary assessment and consultation with the family about the plan of care were reported to be limited or lacking.9 Pediatric HIV care was often limited to tertiary hospitals where access was restricted by poverty and lack of transportation.10 In Tanzania, Collins and Harding9 conducted a census of presenting problems for all patients with HIV (N = 741), of whom 82 were under the age of 18 years. Of 434 patients using antiretroviral therapy, 53% had palliative care needs.
Although it has been advocated that training health care professionals should overcome misconceptions about palliative care,11 few education and training articles were identified by this review. One education and training article identified was a discussion by Malloy et al12 of the ten-module curriculum, “End-of-Life Nursing Education Consortium for Pediatric Palliative Care”, published in the United States. This curriculum details training of nurses to provide pediatric palliative care in the United States and internationally.
Richter et al13 conducted an observational qualitative study of the palliative care needs of children with HIV in KwaZulu-Natal, South Africa. Using videotapes of hospitalized children with HIV/AIDS, they documented routine health care practices, caregiver visits, and challenges to the children’s care. Initial findings indicated that children suffered from separation anxiety because caregivers were not allowed to stay with them, and the children were often in pain. Hospital protocols decreased parental contact with children and may have disempowered parents with regard to care of their child. Health professionals appeared to be suffering from burnout. At the time of this review, the authors reportedly were developing an intervention using community-based participatory research to improve nursing and caregiver skills in this resource-poor province.
Amery et al14 conducted a mixed quantitative and qualitative evaluation of a children’s palliative care service in a resource-poor Sub-Saharan African setting (Uganda). Through retrospective review of patient medical records and semistructured interviews with children, parents, and staff on the palliative care service, data were collected and analyzed by systematic coding and categorization. This revealed a large increase in the number of children referred to the program after implementation of the formal palliative care program, with an average cost of $75 per child. Pain and symptom control were both rated as strengths of the program, as was addressing hunger and poverty by provision of food packs. Staff who completed the questionnaire reported difficulty caring for children and families in the program, and one third described a need for further training in pediatric palliative care. Overall, this study suggested that child-focused palliative care services can be effectively and affordably implemented in resource-poor settings. The study results also suggested that a pediatric-focused program may be more effective than a combined program with adults, which included the key elements of free and effective prescriptions, provision of nutritional support, and ongoing staff training and support.
Physical aspects of care
Pain management
Three studies suggested that pain management for children with HIV/AIDS in Sub-Saharan Africa is problematic. The belief that morphine is dangerous for children persists in some countries.11 In a review of palliative care in Sub-Saharan Africa, De Baets et al10 identified a need for access to pediatric HIV/AIDS care and antiretroviral therapy, treatment of chronic severe pain in children with low CD4 counts, and an absence of analgesia use in approximately half of children with terminal AIDS. Only one country (Uganda) provided palliative home-based care, including free morphine. Of 250 district hospitals in Sub-Saharan Africa, only seven stock morphine for pain relief.10 As a consequence, the call was made for education and training of medical staff, particularly in Kenya, where children with HIV/AIDS, cancer, or sickle cell anemia reportedly die “in uncontrollable agony”.11
In a paper reported from Malawi,15 of 95 children referred for palliative care, the most commonly reported symptom was pain (27%). However, of the 77% with HIV/AIDS (mean age three years) the most common symptom was wasting (90%), followed by cough, diarrhea, and mouth sores. These symptoms were not assessed in a structured way, but by presenting complaint.
Medical care and antiretroviral therapy
Only one study focused on medical care. In a chart review aimed at measuring clinical outcomes for youth initiating antiretroviral therapy while under care at a specialist pediatric palliative care service in South Africa, Harding et al16 described medical outcomes for 37 children (54% female, mean age 5.5 years). Primary evaluation measures included change in weight, CD4 count, viral load, and mortality. Primary presentations at the time of referral to the program included tuberculosis, encephalopathy, wasting, lymphocytic interstitial pneumonitis, and cor pulmonale. Of 37 children followed over a six-month period, six died before follow-up assessment. The causes of four of those deaths were unknown, while the remaining two were related to respiratory illness. At six months, weight increased significantly, CD4 counts doubled, and the CD4 percentages increased significantly, while viral load decreased significantly for youth in the program. Therefore, even with advanced disease, children initiated on antiretroviral therapy showed significant clinical improvement and most were still alive with good virologic response. Further, use of antiretroviral therapy was suggested as an excellent palliative therapy above and beyond treating illness presentation.
Psychologic and psychiatric aspects of care
The psychologic and psychiatric aspects of palliative care were reported in seven studies. Three quantitative studies demonstrated that advance care planning for youth with HIV is acceptable to patients, parents, and professionals. Wiener et al17 sought to determine whether young adults living with HIV or cancer would find it acceptable and helpful to have a planning document to share their wishes regarding end-of-life care with their families or caregivers. The survey was completed by 20 participants enrolled in research protocols at the National Cancer Institute. Ninety-five percent of the participants indicated that an advance care planning document like “Five Wishes”18 would be helpful and 90% indicated that it would be helpful to others.
Lyon et al19 did a two-group, randomized controlled trial in two urban hospital-based outpatient clinics in the United States with the primary goal of measuring the efficacy of a model of FAmilyCEntered (FACE) advance care planning for youth (14–21 years) living with HIV. This three-session intervention with youth, family, and surrogate decision-makers aged at least 21 years used an adapted adult model.20 The results of this pilot study with 38 youth/surrogate dyads indicated that this intervention increased congruence in adolescent/surrogate treatment preferences for end-of-life care, decreased decisional conflict, and enhanced the quality of communication. In a quantitative evaluation of the FACE protocol, 21 92% of 76 families were satisfied overall with the intervention and 93% attended all study sessions.
Dallas et al22 recently published a paper describing the design and methods of a FACE intervention study that built upon prior pilot results from Lyon et al.19 The first aim of this study is to evaluate the long-term efficacy of the FACE intervention with regard to congruence in end-of-life treatment preferences between adolescents with HIV/AIDS and their family, decisional conflict about end-of-life decisions, quality of communication about end-of-life care, and quality of life. The second aim is to evaluate the possible mediating and moderating effects of spiritual struggle, threat appraisal, and adherence with antiretroviral medication on the relationship between the FACE intervention and quality of life, hospitalization, and use of dialysis. To examine the effect of the FACE intervention on study outcomes over an 18-month period, a blinded, dyadic, two-arm, randomized, controlled clinical trial with a time-matched control will be used. At the time of this review, the FACE trial was still open to enrollment at four pediatric/adolescent hospitals across the United States, and the results are not yet available.
Two studies focused on the psychologic needs of children with HIV/AIDS and AIDS orphans. Among the Malawian children who had HIV/AIDS,15 40% had lost their mother or had a mother who was ill. No resources were available to support the emotional or social problems associated with being an orphan. Onuoha et al23 specifically examined the mental health of orphaned children who had lost at least one parent to AIDS in Uganda and South Africa. They found that AIDS-orphaned children showed the highest negative and lowest positive mental health factors. Children in a mentoring relationship with an adult demonstrated better mental health. They concluded that natural mentorship was a palliative care against negative mental health symptoms.
Finally, Lyon et al24 conducted a cross-sectional analysis of 726 children with AIDS aged from birth to 20 years in the Pediatric AIDS Clinical Trials Group 219C database. Their mean age was 12.8 years. Psychologic status (eg, anxiety/depression, hyperactivity, and peer conflict) was similar for those with or without a do-not-resuscitate order or hospice care, despite poorer quality of life.
Spiritual, religious, and existential aspects of care
The domain of spiritual, religious, or existential aspect of palliative care was not studied as the primary aim in any of the papers reviewed. This gap is consistent with that identified in the review by De Baets et al.10 Nevertheless, Collins and Harding9 conducted a prospective census of presenting problems for all patients with HIV during a one-month period (n = 731; n = 82 under the age of 16 years) in Tanzania. They found a need for spiritual support (19%) and social support (24%), with 51.7% of patients having palliative care needs. Further, only 18 (2%) of patients in the study had received advance care planning.
Cultural aspects of care
Lindsey et al25 conducted an exploratory study in Botswana to understand better the impact of caring for family members living with HIV/AIDS on young girls and older women. The study population was a convenience sample of 35 primary caregivers and terminally or chronically ill family members. Qualitative interviews were conducted, and the results suggested that younger girls often missed school because of their responsibilities as caregivers and were also sexually and physically abused. The results show that the burden of care for terminally and chronically ill family members is profound for both older and younger women in Botswana. The authors concluded that effective and affordable community home-based care is critical in impoverished settings.
Care of the imminently dying patient
Three of the articles discussed earlier focused on treatment of pain for the imminently dying patient.10,11,15 Otherwise, only two studies evaluated terminal care in children who died of HIV/AIDS. Henley26 studied a children’s hospital in Cape Town, South Africa, where 165 patients died of HIV-related causes. The primary outcome measures included documentation of do-not-resuscitate orders and comfort care plans, intensity of diagnostic and therapeutic interventions in the last 24 hours of life, and presence of pain and distress in the last 48 hours of life. Medical chart abstraction and a structured questionnaire were used to collect data. The results indicated that 84% of participants had do-not-resuscitate orders, but that almost two thirds of these had no record indicating whether the do-not-resuscitate order had been discussed with the parents or caregiver. Comfort care plans were identified in 44% of the participants’ medical records. Pain and distress was documented in 55% of cases.
Similarly, Lyon et al24 examined the frequency of do-not-resuscitate orders and hospice enrolment for the 41 children participating in the Pediatric AIDS Clinical Trials Group 219C study who had died in 2000–2005, and found that 20% had a do-not-resuscitate order or had received hospice care. Quality of life scores were significantly lower for those participants with do-not-resuscitate orders/hospice enrolment. No racial differences in prevalence of do-not-resuscitate orders or hospice enrolment were detected among the sample. Children who died of AIDS rarely had a do-not-resuscitate order or hospice care, while parent’s perception of their child’s health as poor was associated with having a do-not-resuscitate order/hospice care.
Ethical and legal aspects of care
Data on the ethical and legal aspects of care were available for five studies. One editorial, discussed earlier, focused on legal barriers to providing pain management required by patients living with HIV/AIDS in Kenya due to cultural beliefs about the appropriateness of morphine treatment in children.11
Another assessed the question of discrimination in Uganda and South Africa, where Onuoha et al23 found that double-orphaned children were more likely to suffer social discrimination, be victims of child abuse, and receive significantly less social support than single-orphaned children. Double-orphaned children received the least love and comfort when they felt bad, the least financial support, and the least assistance with things they could not do. Recommendations were made for “natural mentors”, ie, extended family members, to be part of a palliative care team and alleviate the effects of double parental loss and potentially prevent negative mental health outcomes.
Three studies conducted in the United States assessed ethical and legal aspects of decisional capacity, as related to intellectual ability, understanding informed assent, and confidentiality for minors. Chenneville et al27 assessed the relationship among youth decisional capacity, developmental stage, intellectual ability, and social-emotional functioning in a sample of youth with and without HIV. The study groups did not differ significantly with regard to level of decisional capacity. Youth developmental level was found to relate significantly to decisional capacity, which was consistent with typically developing population research. These results support the idea that youth living with HIV have the decisional capacity to participate meaningfully in their health care, despite possible deficits in intellectual and/or adaptive skills.
Blake et al28 identified ways to improve adolescent understanding of informed assent by assessing adolescent comprehension of research topics. These authors conducted eight focus groups (n = 33) with youth aged 15–17 years for understanding of several research topics through qualitative review of the focus group content discussed. Topics included general research concepts, general vaccine trial concepts, and concepts unique to HIV vaccine trials. Teens had the most difficulty with the concept of “placebo” and “randomization”, and also demonstrated difficulty with comprehension of how a vaccine works and the concept that a vaccine is preventative in nature. The authors also reported confusion in this age group about the possibility of a false positive result after receiving an HIV vaccine. In general, youth indicated a desire to be informed about adverse effects and the procedures of clinical trials in which they may participate.
In a single case study in New York City involving the medical care of a 15-year-old minor who disclosed possible HIV exposure to her health care provider, Summers et al29 described the ethical, legal, and developmental issues that ensued. This case study included discussion of patient confidentiality and legal issues related to emancipation of minors, the mature minor doctrine, and state-specific issues related to insurance/billing practices and the type of medical care sought. These authors highlighted cognitive functioning as a factor in determining adolescent capacity and rights. This case study also examined the role of the practitioner in supporting adolescent decision-making and appropriate health care and systemic barriers to working effectively with adolescents in the medical environment.
General reviews of the literature
Two articles reviewed the literature regarding palliative care for youth with HIV, one by Allen and Sorensen Marshall30 and the other by Kovacs et al.31 Both presented a broad review of the pillars of palliative care and included a review of standards of care, as well as suggestions for appropriate clinical care.
Discussion
Status of literature
This systematic review of the literature regarding pediatric palliative care for youth with HIV identified 21 papers involving youth with HIV and topics of palliative care and/or medical decision-making. Our review revealed that while most studies were completed in the United States, a substantial number were completed in Sub-Saharan Africa. Most studies involved qualitative or retrospective methods and were descriptive in nature. Only one study evaluated an intervention to improve well-being in this population.24 Several articles evaluated a single pediatric palliative care program internationally. These findings reflect the relative novelty of this type of service provision in general, and particularly in low-income countries.
Overall, the evidence is insufficient to make definite conclusions about palliative care for HIV-infected youth. One randomized controlled trial has been conducted, but was limited to advance care planning. The remaining studies are descriptive or use qualitative approaches without evaluating outcomes. No unifying theme emerged on the role of pediatric palliative care among youth living with HIV. As such, the reported findings should be regarded as preliminary data.
Based on this review, palliative care provision in youth with HIV appears to focus on amelioration of pain symptoms and managing physical care of patients near end of life. Internationally, palliative care has been shown to be affordable and useful to families of youth with HIV. Most articles reported youth with HIV in a palliative care program to benefit physically. The review identified limited literature on psychologic functioning, social functioning, and ethical/legal issues. The lack of focus on these areas of palliative care may also reflect the novelty of this field within the area of pediatric HIV care, whereby the recent focus has been on reducing experience of pain and the physical discomforts of dying. Further, a majority of the published literature focused on end-of-life or near death issues, and relatively little addressed advance care planning among patients who have HIV but are not near the end of life. Antiretroviral treatment was identified as an important part of the physical care of patients with HIV in palliative care programs in Sub-Saharan Africa.
Culturally, several areas appeared to impact provision of pediatric palliative care for youth with HIV, including community norms regarding the use of pain medication11 and the role of women in caring for those dying from HIV-related causes.25 Further, this review revealed evidence that existing advance care planning models can be adapted for age, disease, and culture.19 Lindsey et al25 also highlighted that issues surrounding spiritual well-being and the role it plays in palliative care are important for adolescents and their families.
Ongoing training and support for staff is important for pediatric palliative care programs, not only for adolescent care but also for staff effectiveness. As Amery et al14 reported, staff attitudes towards adolescents receiving palliative care is particularly important. Staff members reported finding it difficult to treat children with life-threatening illnesses and were concerned about service accessibility and abandonment of children. There is a need for multidisciplinary palliative care from trained staff to ensure effective care for children with HIV, especially in Sub-Saharan Africa.9 Finally, the review suggested improvements are needed for advance care planning that are appropriate and helpful for adolescents, and should also encourage effective communication with clinic and palliative care staff.17,24
Few studies directly evaluated the ethical and legal issues in palliative care. Chenneville et al27 reported no differences between youth with HIV and their noninfected counterparts with regard to medical decision-making skills. This is important to document, given the historically reported cognitive deficits found in adults with HIV. A case study reported by Summers et al29 reviewed key ethical and legal issues for consideration in the context of clinical care of youth with HIV, but did not specifically address palliative care outside the context of medical decision-making.
Gaps in the literature
A dearth of literature was observed regarding psychological, social, and ethical issues in palliative care. Most papers focused on physical aspects of palliative care or on general review of a pediatric palliative care program. Further, there was a paucity of relevant interventional research in this area. Few articles focused on implementation or evaluation of education and training in pediatric palliative care involving youth. More work focusing on the psychologic aspects of pediatric palliative care among HIV-infected youth is needed. Further, studies evidencing intervention or training models are also needed to address palliative care specific to youth with HIV.
Within the domain of care of imminently dying youth with HIV, most studies did not indicate whether or not signs and symptoms of impending death were recognized and communicated to patients and families. Further, no studies evaluated family perception of whether or not care was appropriate for this phase of advanced disease.
Very few of the studies reviewed actually published original data. Those including original data were limited by their cross-sectional or observational design. Only one randomized controlled trial was identified in the literature that included published data, while another study presented the design and methods for a randomized trial, but analysis of the data had not been completed at the time of publication of this review. This could be due to the fact that data from randomized controlled trials is often insufficient to address all aspects of palliative care and may be unethical or difficult to conduct.32
Limitations
A core challenge to our systematic review was there was no consistent agreement internationally on the domains of palliative care. Care was taken to decrease the impact of this limitation by reviewing the citation lists of identified articles and searching a breadth of databases using the identified key words. Due to high variability in the types of published literature, we were unable to evaluate the merits of the research objectively. In light of the minimal literature that exists in this topical area, we decided a priori to include all studies identified in our search regardless of their methodology or design. Further, a thematic narrative approach was used to synthesize the findings, due to the observed variability of the published literature and limitations of the quantitative results.
Finally, the results of our review are not necessarily applicable to populations or care settings other than those addressed by the included studies. Several studies included a wide age range, and were not exclusive to youth. Our search yielded only research from the United States and Africa and did not include other regions. We do not know if approaches used in the United States or in Africa are applicable to other cultures or in other social contexts.
Conclusion
Pediatric palliative care of youth with HIV is a burgeoning area of investigation and warrants further research attention. There have been few empirically based studies evaluating palliative care and medical decision-making in youth with HIV. What was available tended to focus on physical aspects of care with less attention toward psychological, social, ethical, and cultural aspects of care. Future research should focus on broadening the evaluation of pediatric palliative care among youth with HIV by directly evaluating the psychological, social, ethical, and cultural aspects of care, while investigating the needs of all stakeholders, patients, families, and health care providers.
Acknowledgments
This paper is published on behalf of the FACE Adolescent Palliative Care Consortium. The authors acknowledge Nancy Hutton’s contribution to the design of this review.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization WHO definition of palliative care Available from: http://www.who.int/cancer/palliative/definition/en/Accessed May 14, 2013
- 2.National Consensus Project of Quality Palliative Care Clinical practice guidelines for quality palliative care Available from: http://www.nationalconsensusproject.org/guideline.pdfAccessed January 26, 2012
- 3.World Health Organization, Joint United Nations Programme on HIV/AIDS, United Nations Children’s Fund Epidemic update and health center progress towards universal access: progress report 2011. Global HIV/AIDS Response 2011Available from: http://www.afro.who.int/en/clusters-a-programmes/dpc/acquired-immune-deficiency-syndrome/features/3439-global-hivaids-response-progress-report-2011.htmlAccessed May 26, 2013
- 4.World Health Organization Adolescent health epidemiology Available from: http://www.who.int/entity/maternal_child_adolescent/epidemiology/adolescence/en/Accessed May 26, 2013
- 5.McConnell MS, Byers RH, Frederick T, et al. Trends in antiretroviral therapy use and survival rates for a large cohort of HIV-infected children and adolescents in the United States, 1989–2001. J Acquir Immune Defic Syndr. 2005;38(4):488–494. doi: 10.1097/01.qai.0000134744.72079.cc. [DOI] [PubMed] [Google Scholar]
- 6.Dollfus C, Le Chenadec J, Faye A, et al. Long-term outcomes in adolescents perinatally infected with HIV-1 and followed up since birth in the French perinatal cohort (EPF/ANRS CO10) Clin Infect Dis. 2010;51(2):214–224. doi: 10.1086/653674. [DOI] [PubMed] [Google Scholar]
- 7.Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesizing qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy. 2005;10(1):45–53. doi: 10.1177/135581960501000110. [DOI] [PubMed] [Google Scholar]
- 8.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins K, Harding R. Improving HIV management in sub-Saharan Africa: how much palliative care is needed? AIDS Care. 2007;19(10):1304–1306. doi: 10.1080/09540120701402863. [DOI] [PubMed] [Google Scholar]
- 10.De Baets AJ, Bulterys M, Abrams EJ, Kankassa C, Pazvakavambwa IE. Care and treatment of HIV-infected children in Africa: issues and challenges at the district hospital level. Pediatr Infect Dis J. 2007;26(2):163–173. doi: 10.1097/01.inf.0000253040.82669.22. [DOI] [PubMed] [Google Scholar]
- 11.Providing paediatric palliative care in Kenya. Lancet. 2010;376(9744):846. doi: 10.1016/S0140-6736(10)61394-3. [No authors listed] [DOI] [PubMed] [Google Scholar]
- 12.Malloy P, Sumner E, Virani R, Ferrell B. End-of-life nursing education consortium for pediatric palliative care (ELNEC-PPC) MCN Am J Matern Child Nurs. 2007;32(5):298–302. doi: 10.1097/01.NMC.0000288000.87629.de. [DOI] [PubMed] [Google Scholar]
- 13.Richter L, Chandan U, Rochat T. Improving hospital care for young children in the context of HIV/AIDS and poverty. J Child Health Care. 2009;13(3):198–211. doi: 10.1177/1367493509336680. [DOI] [PubMed] [Google Scholar]
- 14.Amery JM, Rose CJ, Holmes J, Nguyen J, Byarugaba C. The beginnings of children’s palliative care in Africa: evaluation of a children’s palliative care service in Africa. J Palliat Med. 2009;12(11):1015–1021. doi: 10.1089/jpm.2009.0125. [DOI] [PubMed] [Google Scholar]
- 15.Lavy V. Presenting symptoms and signs in children referred for palliative care in Malawi. Palliat Med. 2007;21(4):333–339. doi: 10.1177/0269216307077689. [DOI] [PubMed] [Google Scholar]
- 16.Harding R, Brits H, Penfold S. Paediatric antiretroviral therapy outcomes under HIV hospice care in South Africa. Int J Palliat Nurs. 2009;15(3):142–145. doi: 10.12968/ijpn.2009.15.3.41093. [DOI] [PubMed] [Google Scholar]
- 17.Wiener L, Ballard E, Brennan T, Battles H, Martinez P, Pao M. How I wish to be remembered: the use of an advance care planning document in adolescent and young adult populations. J Palliat Med. 2008;11(10):1309–1313. doi: 10.1089/jpm.2008.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aging with Dignity Five wishes Available from: http://www.agingwithdignity.org/five-wishes.phpAccessed May 26, 2013
- 19.Lyon ME, Garvie PA, Briggs L, He J, McCarter R, D’Angelo LJ. Development, feasibility, and acceptability of the Family/Adolescent-centered (FACE) advance care planning intervention for adolescents with HIV. J Palliat Med. 2009;12(4):363–372. doi: 10.1089/jpm.2008.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Briggs L, Hammes BJ, Disease specific advance care planning (DSACP) Next Steps Facilitator Certification: A communication skills training program [manual] La Crosse, WI: Gundersen Medical Foundation Inc; 2008. 2010. [Google Scholar]
- 21.Lyon ME, Garvie PA, McCarter R, Briggs L, He J, D’Angelo LJ. Who will speak for me? Improving end-of-life decision-making for adolescents with HIV and their families. Pediatrics. 2009;123(2):e199–e206. doi: 10.1542/peds.2008-2379. [DOI] [PubMed] [Google Scholar]
- 22.Dallas RH, Wilkins ML, Wang J, Garcia A, Lyon ME. Longitudinal pediatric palliative care: quality of life and spiritual struggle (FACE): design and methods. Contemp Clin Trials. 2012;33(5):1033–1043. doi: 10.1016/j.cct.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Onuoha FN, Munakata T, Serumaga-Zake PA, Nyonyintono RM, Bogere SM. Negative mental health factors in children orphaned by AIDS: natural mentoring as a palliative care. AIDS Behav. 2009;13(5):980–988. doi: 10.1007/s10461-008-9459-0. [DOI] [PubMed] [Google Scholar]
- 24.Lyon ME, Williams PL, Woods ER, et al. Do-not-resuscitate orders and/or hospice care, psychological health, and quality of life among children/adolescents with acquired immune deficiency syndrome. J Palliat Med. 2008;11(3):459–469. doi: 10.1089/jpm.2007.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindsey E, Hirschfeld M, Tlou S. Home-based care in Botswana: experiences of older women and young girls. Health Care Women Int. 2003;24(6):486–501. doi: 10.1080/07399330390199384. [DOI] [PubMed] [Google Scholar]
- 26.Henley LD. End of life care in HIV-infected children who died in hospital. Dev World Bioeth. 2002;2(1):38–54. doi: 10.1111/1471-8847.00034. [DOI] [PubMed] [Google Scholar]
- 27.Chenneville T, Sibille K, Lujan-Zilbermann J, Rodriguez C, Brown M, Emmanuel P. Medical decisional capacity among children with HIV. AIDS Care. 2010;22(11):1359–1366. doi: 10.1080/09540121003758499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blake DR, Lemay CA, Kearney MH, Mazor KM. Adolescents’ understanding of research concepts: a focus group study. Arch Pediatr Adolesc Med. 2011;165(6):533–539. doi: 10.1001/archpediatrics.2011.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Summers D, Alpert I, Rousseau-Pierre T, et al. An exploration of the ethical, legal and developmental issues in the care of an adolescent patient. Mt Sinai J Med. 2006;73(3):592–595. [PubMed] [Google Scholar]
- 30.Allen D, Sorensen Marshall E. Children with HIV/AIDS: a vulnerable population with unique needs for palliative care. J Hosp Palliat Nurs. 2008;10(6):359–367. [Google Scholar]
- 31.Kovacs PJ, Bellin MH, Fauri DP. Family-centered care: a resource for social work in end-of-life and palliative care. J Soc Work End Life Palliat Care. 2006;2(1):13–27. doi: 10.1300/J457v02n01_03. [DOI] [PubMed] [Google Scholar]
- 32.Wee B, Hadley G, Derry S. How useful are systematic reviews for informing palliative care practice? Survey of 25 Cochrane systematic reviews. BMC Palliat Care. 2008;7:13. doi: 10.1186/1472-684X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]


