Abstract
Background
We previously found no reduction in heterotopic ossification (HO) rates after acetabular surgery with indomethacin compared with a placebo. We subsequently abandoned routine indomethacin therapy after acetabular surgery but questioned whether the incidence had changed using a posterior approach.
Questions/purposes
We therefore determined (1) the incidence of HO after acetabular fracture surgery through a posterior approach; (2) the incidence of symptoms attributable to HO; and (3) the rate of reoperation for HO.
Methods
We retrospectively reviewed the records of all 423 patients with acetabular fractures following our clinical protocol change; of these, 120 were treated with a Kocher-Langenbeck approach and included. The presence of radiographic HO was documented a minimum of 10 weeks postoperatively using the classification of Brooker et al. Symptoms and reoperations were recorded.
Results
The overall incidence of radiographic HO was 47% (56 of 120 patients): 26% Class I–II 13% Class III, and 8% Class IV. Overall, 15% of patients developed symptoms; 3.3% underwent reoperations for excision of HO. There were no major differences between the incidence of moderate and severe HO in this study when compared with the indomethacin and placebo groups from the prior study.
Conclusions
Our incidence of moderate and severe HO has not changed since discontinuing indomethacin. These findings support our institutional decision to abandon routine indomethacin prophylaxis after acetabular surgery. We recommend improved surgical techniques to limit damage to the abductors and improved risk stratification of patients when considering treatment options for HO prophylaxis.
Levels of Evidence
Level III, retrospective comparative study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Heterotopic ossification (HO) about the hip is a known complication after operative treatment of acetabular fractures [3, 7, 9, 12, 14, 16, 17, 27]. The incidence varies greatly with reported rates of 18% to 90%, with higher rates for posterior and extensile surgical approaches [1, 3, 10, 15]. A meta-analysis of 2394 patients showed an incidence of radiographic HO of 26% after operative treatment of acetabular fractures with strong associations based on surgical approach: 24% with the extended iliofemoral approach, 12% with the Kocher-Langenbeck approach, and 1.5% with the ilioinguinal approach [10]. Excessive heterotopic bone around the hip may cause severe limitations in ROM and decreased function [9, 17]. The high incidence of radiographic HO and potential morbidity after acetabular surgery have led to the standardization of prophylactic therapies in many institutions [3, 6, 10, 11, 13, 15–18, 20, 24]. Both indomethacin and radiation therapy variably decrease the rates of severe HO after acetabular surgery to 4% to 15% [2, 3, 6, 11, 13, 15–18, 20]. Both modalities have associated complications, including risks of gastrointestinal bleeding, delayed fracture healing, radiation-associated morbidities, and the unclear cost-effectiveness of radiation therapy [1–3, 5, 6, 11, 13, 15–18, 20, 21]. Indomethacin treatment has been associated with gastric ulcers, decreased platelet function, renal toxicity, and impaired fracture healing [1, 5, 21].
Karunakar et al. conducted a prospective, randomized control study of the effects of indomethacin on reducing HO rates after acetabular surgery at our institution [13] and found no reduction in the incidence of HO with indomethacin versus placebo. Additionally, they reported poor compliance, poor tolerance, and a high incidence of gastrointestinal bleeding resulting from indomethacin in the study. For these reasons, the routine use of indomethacin therapy after acetabular surgery was abandoned at our institution. When our clinical protocol change was reviewed as a quality measure, the following questions were posed: (1) Has the incidence of HO after acetabular fracture surgery changed since we discontinued prophylactic indomethacin therapy? (2) What is the incidence of radiographic HO and symptoms attributed to HO in our patient population? (3) What is the incidence of reoperation for HO?
Patients and Methods
We performed a retrospective chart review of 423 consecutive patients treated for acetabular fractures at our institution (Level I regional trauma center) since we discontinued the routine use of indomethacin as prophylactic therapy. Patients were identified through our trauma registry from January 1, 2006, through December 31, 2011. A total of 281 patients (282 fractures) were treated operatively with 202 patients (203 fractures, one patient with bilateral acetabular fractures) treated with the Kocher-Langenbeck approach. Only patients treated through a posterior Kocher-Langenbeck approach were included to ensure more accurate comparison to the historical control from the prior study conducted at our institution [13]. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Inclusion criteria were (1) 18 years of age or older at the time of injury; (2) presence of an acetabular fracture treated operatively through a Kocher-Langenbeck approach; and (3) presence of at least one postoperative radiograph and followup clinic visit at 10 to 20 weeks. A total of 81 patients were excluded for the following reasons: 48 patients potentially eligible for inclusion were lost to followup; two patients were excluded for treatment with radiation therapy as HO prophylaxis after acetabular surgery (one patient received radiation after completion of operative fixation of their acetabular fracture during a second operation [interrupted index procedure as a result of intraoperative medical complication] and a second patient received radiation therapy for unclear reasons [not clearly documented in records]); four patients were excluded for acute failure and conversion to THA within 3 months; four patients were excluded for combined fixation and THA; one patient was excluded for periprosthetic fracture around a THA socket; 13 patients (14 fractures, one patient with bilateral acetabular fractures) were excluded for documented head injury (eg, open or closed with hemorrhage, traumatic brain injury, or diffuse axonal injury); seven patients were excluded for reoperation for acute (within 4 weeks) deep infection or hematoma; one patient was excluded for acute reoperation (immediately postoperatively) for hardware misplacement; and one patient was excluded for postoperative indomethacin use for pain control. After the exclusions were applied, there were 120 included patients (120 fractures).
We had no standard followup protocol and variability in the timing of postoperative followup visits necessitated a wide-range assessment of radiographs and clinical symptoms. We documented symptoms attributable to the presence of radiographic HO at the last clinic followup and reoperation for excision of HO. Chief subjective complaints at the last followup were pain, stiffness, and limp; the most common clinical finding was loss of active and passive hip ROM. Radiographic HO is usually seen with maximum formation by 12 weeks postoperatively [6, 13, 15–20, 24], and last clinic followup averaged 10 months postoperatively for patients with moderate HO (Brooker Class III) and 7 months postoperatively for patients with severe HO (Brooker Class IV).
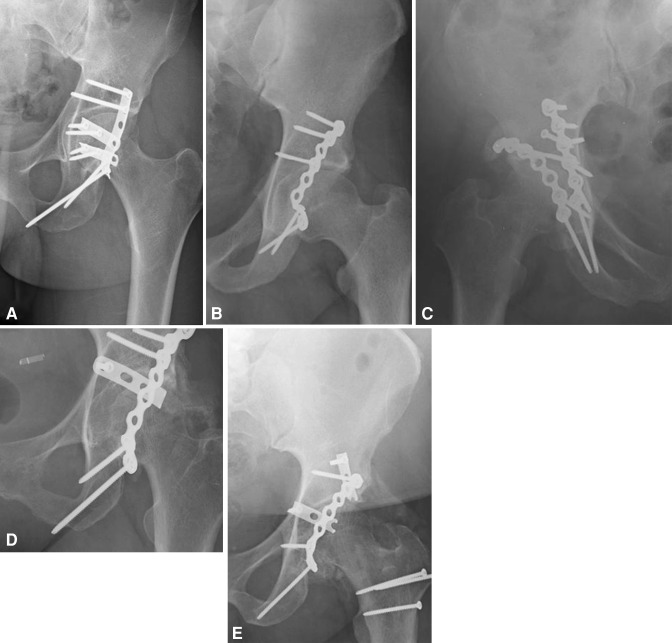
Standard plain film radiographs were taken during the postoperative period; AP, iliac oblique, and obturator oblique views were reviewed according to Moed and Smith [19]. One of us (SMG) classified the presence of HO as documented on radiographs at 10 to 20 weeks postoperatively according to the classification of Brooker et al. [4]. Class 0 indicated no HO, Class I described islands of bone within the soft tissues about the hip, Class II described bone spurs from the pelvis or proximal end of the femur with at least a 1-cm gap, Class III described bone spurs from the pelvis or proximal end of the femur with a gap less than 1 cm, and Class IV described apparent bony ankylosis of the hip [4, 13] (Fig. 1). Patients were classified into four categories for all analyses: no HO (Brooker Class 0), mild HO (Brooker Classes I and II), moderate HO (Brooker Class III), and severe HO (Brooker Class IV). We used the combined data for Classes III and IV for comparison to the data from our previous study as the historical control.
Fig. 1A–E.
Brooker classification for HO about the hip [4]. (A) Brooker Class 0, no HO. (B) Brooker Class I, islands of bone within the soft tissues about the hip. (C) Brooker Class II, bone spurs from the pelvis or proximal end of the femur with at least a 1-cm gap. (D) Brooker Class III, bone spurs from the pelvis or proximal end of the femur with a gap less than 1 cm. (E) Brooker Class IV, apparent bony ankylosis of the hip.
Categorical variables were compared with those in our previous study [13] using Pearson chi-square tests and continuous variables were compared using independent sample t-tests or one-way analysis of variance. The Brooker classes were separated into four categories for all analyses: none (Class 0), mild (Classes I and II), moderate (Class III), and severe (Class IV). The data were analyzed using Stata® 12 (StataCorp LP, College Station, TX, USA) software.
Results
We found no major differences between the combined incidence of moderate and severe HO (Brooker Classes III and IV) in this study when compared with the same incidences for both the indomethacin and placebo treatment groups from the prior study (historical control). The combined incidence for Brooker Class III and IV in the current study was 21% (25 of 120 patients). No differences were found when this was compared with the indomethacin treatment group (incidence of Brooker Class III–IV HO was 15% [nine of 59 patients], p = 0.36) and with the placebo treatment group (incidence of Brooker Class III–IV HO was 19% [12 of 62 patients], p = 0.72) from the prior study (Table 1). The overall incidence of radiographic HO was 47% (56 of 120 patients); 31 of 120 patients (26%) had mild HO (Brooker Class I–II); 15 of 120 (13%) patients had moderate HO (Brooker Class III); and 10 of 120 (8%) patients had severe HO (Brooker Class IV).
Table 1.
Incidence of severe heterotopic ossification, including data reported in randomized trials and historic data
| Author | Moderate or severe radiographic HO (Brooker III and IV) | ||
|---|---|---|---|
| No prophylaxis or placebo | Indomethacin | Radiation | |
| Current study | 21% (25/120) | ||
| Karunakar et al. [13] | 19% (12/62) | 15% (9/59) | |
| Letournel and Judet* [14] | 11% (31/281) | ||
| Matta and Siebenrock† [15] | 5% (1/21) | 9% (3/32) | |
| Burd et al. [6] | 11% (8/72) | 4% (3/78) | |
* Letournel used Kocher-Langenbeck, no prophylaxis; †only includes patients treated through a posterior or extensile approach; HO = heterotopic ossification. Table provided by and modified with permission from SLACK Incorporated: Karunakar MA. Acetabular fractures: heterotopic ossification. In: Archdeacon MT, Anglen JO, Ostrum RF, Hersocovici D Jr. Prevention and Management of Common Fracture Complications. Thorofare, NJ, USA: Slack Inc; 2012:179–188.
Symptoms were reported in the medical records as pain, limp, and stiffness/decreased ROM. Of those with mild radiographic HO (Brooker Class I–II), no patients had any hip-related symptoms at last clinical followup. Of patients with moderate radiographic HO (Brooker Class III), eight of 15 patients (53%) had hip-related symptoms at last followup, which averaged 10 months postoperatively for this group. The chief subjective complaints at last followup were pain (five of eight patients), stiffness (five of eight patients), and limp (three of eight patients); the most common clinical finding was loss of active and passive hip ROM (loss of internal rotation [IR] documented in six of eight patients with average IR of 3.3°). All patients (10 of 10 patients) with severe HO (Brooker Class IV) were symptomatic at last clinic followup, which averaged 7 months postoperatively for this group. The chief subjective complaints at last followup for this group were pain (five of 10 patients), stiffness (10 of 10 patients), and limp (five of five patients); the most common clinical finding was loss of active and passive hip ROM (loss of IR documented in six of 10 patients with average IR of 3.3°) (Table 2).
Table 2.
Incidence of heterotopic ossification
| HO class/outcome | Incidence |
|---|---|
| No HO | 53% (64/120 patients) |
| Radiographic HO | 47% (56/120 patients) |
| Mild radiographic HO (Brooker I–II) | 26% (31/120 patients) |
| Moderate radiographic HO (Brooker III) | 13% (15/120 patients) |
| Severe radiographic HO (Brooker IV) | 8% (10/120 patients) |
| Hip-related symptoms resulting from HO | 53% (8/15 patients) with moderate HO (Brooker III), 100% (10/10 patients) with severe HO (Brooker IV), 15% (18/120 patients) overall |
| Reoperation for HO excision | 22% (4/18 patients) with symptomatic moderate or severe HO (Brooker III and IV), 3.3% (4/120 patients) overall |
HO = heterotopic ossification.
Four of 120 patients (3.3%) underwent reoperation for excision of HO at a mean of 9 months postoperatively (range, 5–13 months); one of these patients had moderate HO (Brooker Class III), and three patients had severe HO (Brooker Class IV). This gives an overall incidence of symptomatic moderate or severe HO (Brooker Class III and IV) of 15% (18 of 120 patients).
Discussion
We previously examined the effect of indomethacin on reducing HO rates after acetabular surgery through a posterior approach and found no reduction by indomethacin versus a placebo [13]. The routine use of indomethacin therapy after acetabular surgery was subsequently abandoned at our institution. The current study was designed to evaluate changes in clinical outcomes after our protocol change and to either support or call into question the changes made in our treatment algorithm. The development of symptomatic HO remains an important clinical problem. When reviewed as a quality measure, we asked whether the incidence of HO after acetabular surgery had changed, what is the incidence of radiographic HO and symptoms resulting from HO, and what is the rate of reoperation for symptoms resulting from major HO since abandoning indomethacin prophylaxis.
We recognize major limitations of our study. First, we had a relatively low number of patients, particularly those with major symptoms and reoperations and the study would be underpowered to determine factors related to major symptoms or reoperations. Our exclusion criteria were designed to control for some confounding variables. Risk factors for HO after acetabular surgery have been identified and include traumatic brain injury, fracture pattern and severity, being male, high Injury Severity Score, associated thoracic and abdominal trauma, and a delay in fracture fixation [9–12, 14, 23, 27]. We serve a patient population that is often critically injured and prone to complications; therefore, severe injuries and complications that may be confounding factors must be eliminated from consideration when possible. Therefore, a substantial number of patients were eliminated from the study on that basis. The largest factor responsible, however, for the relatively low number of patients in the study was loss to followup (24% of all potentially eligible patients), a factor over which we had no control. The aim of this study was to compare results with those from the prior study done here, and the numbers of eligible patients were nearly identical [13] (120 eligible patients versus 121 eligible patients in the previous study). Second was the inability to further classify the nature of clinical symptoms that occurred in the 18 patients in whom symptoms resulting from HO were noted. Symptoms were attributed to HO when directly specified by the treating clinician in the clinic note. The descriptions generally included only mention of pain and decreased ROM as a subjective complaint, and infrequently actual ranges were given. Because this was a retrospective chart review, better characterization and quantification of these symptoms was not possible. These data would be useful in more accurately analyzing what symptoms are the result of the presence of HO, grading of symptom severity, and correlation to the radiographic severity of HO present. Additionally, two patients in the moderate and severe HO groups with major symptoms who had planned and scheduled surgical excision of HO who were lost to followup before the procedure. It is not possible to know if these patients had their procedure elsewhere or if they declined reoperation. Inclusion of these patients in the reoperation cohort would influence our data. Third, the use of nonindomethacin NSAIDs, specifically aspirin and ibuprofen, in the postoperative period could have confounded the findings and we did not control for these agents in our analysis. Indomethacin, aspirin, and ibuprofen all decrease heterotopic bone formation in both animal and human studies [1, 8, 21, 22, 26]. Pagnani et al. demonstrated high-dose aspirin reduced the incidence of severe (Brooker Class III–IV) HO in a study of 83 male patients after THA [22]. Ibuprofen reportedly reduced HO in both human and rat studies [8, 26]. Because ours was a retrospective chart review, we could not rule out the use of prescribed or over-the-counter NSAID medications because our documentation did not accurately reflect the medication profiles. One patient was discharged from the hospital with prescribed indomethacin for pain control and was excluded on this basis. Two patients in the study group were discharged on low-dose aspirin for cardiac prophylaxis but were not excluded because of the low-dose regimen. Use of ibuprofen for pain control in the postoperative period was not considered as exclusion criteria for our study because of an inability to verify compliance and dosing. Nineteen patients in our study were prescribed ibuprofen at discharge, but actual use could not be verified as a result of lack of recordkeeping. Despite these obvious limitations, our findings seem to support our decision to abandon indomethacin prophylaxis with outcomes similar to the previous index study [13] in a nearly identical study population size.
We found no major differences between the combined incidence of moderate and severe HO (Brooker Classes III and IV) in this study (21%) when compared with the incidence of moderate to severe HO (Brooker Classes III and IV) for both the indomethacin (15%) and placebo (19%) treatment groups from the prior study [13]. Letournel and Judet [14] reported an 11% incidence of severe HO after acetabular surgery through a Kocher-Langenbeck approach without any prophylaxis. This is similar to the 9% to 15% reported for patients receiving indomethacin in randomized clinical trials [10, 14, 18] as well as the 19% to 21% reported in the prior [13] and current studies at our institution. In the absence of adjunctive prophylaxis, surgical techniques have been developed to decrease the formation of HO, including débridement of the gluteus minimus and the digastric slide trochanteric osteotomy. Débridement of devitalized gluteus minimus muscle at the time of surgery reportedly reduces the development of severe HO after acetabular surgery through a posterior or extensile approach. Rath et al. [24] reported a 10% incidence of severe HO after débridement of devitalized gluteus minimus after acetabular surgery through a posterior approach, and this compared favorably with other series using chemoprophylaxis. Trochanteric osteotomy has historically been associated with increased HO, likely related to the elevation and subsequent injury to the abductor muscles [9, 11, 12, 14]. Siebenrock et al. [25] proposed a modified osteotomy, the trochanteric slide, which they asserted minimizes abductor injury, resulting in a lower rate of HO. Most authors suggest surgical techniques to minimize injury to the abductor muscle may reduce the risk of formation of heterotopic bone [9, 13, 15, 24]. Gluteus minimus débridement was done in all patients in this study, and digastric slide trochanteric osteotomy was used in all patients who required osteotomy. However, these techniques did not seem to show any reduction in HO formation in our study population, suggesting our technique may be causing more abductor injury than expected and refinement is needed. Single-dose radiation therapy reduces the incidence and severity of HO after acetabular surgery [2, 3, 6, 20]; however, as a result of its high cost and potentially associated morbidity, it has been used only sporadically in our institution. Radiation therapy was used for HO prophylaxis for only two high-risk patients during our study period, and they were excluded from the study. This may be considered in the future for high-risk patients.
Although the overall incidence of radiographic HO in our current study was 47% with a combined incidence of moderate and severe HO of 21%, only 18 of 120 patients (15%) developed symptoms we attributed to HO. Symptoms were reported in the medical records as pain, limp, and stiffness/decreased ROM. The only quantifiable symptoms documented in the medical records were loss of active and passive hip ROM. However, because normal ROM of the unaffected contralateral sides was not documented for each patient, it was very difficult to accurately calculate motion loss retrospectively.
Our reoperation rate for symptomatic HO was low overall (3.3%), and reoperation only occurred in patients with moderate and severe radiographic HO. However, within the combined moderate and severe subgroups, the reoperation rate was relatively high at 22%. Patients with symptomatic moderate or severe HO not undergoing reoperation were not recalled for the purposes of this study to evaluate why treatment was not sought or if they underwent treatment elsewhere.
Since discontinuing indomethacin prophylaxis after acetabular surgery, our incidence of moderate and severe radiographic and symptomatic HO has not changed despite the standardized use of surgical techniques designed to minimize the risks of developing HO. Our findings support our institutional protocol change to discontinue routine indomethacin prophylaxis after acetabular surgery for low-risk patients. An ideal prophylactic regimen for HO would show a large reduction in the incidence of severe HO, have ease of use with a high compliance rate, and be cost-effective with a minimal risk of side effects or complications. Based on current evidence, neither indomethacin nor radiation meets all of these criteria. We would, however, recommend improved surgical techniques to limit damage to the abductors and improved risk stratification of patients when considering treatment options for HO prophylaxis for higher risk patients after acetabular fracture surgery.
Acknowledgments
We thank Elizabeth Cotton, MS, for her contributions to this project.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Carolinas Medical Center, Charlotte, NC, USA.
References
- 1.Altman RD, Latta LL, Keer R, Renfree K, Hornicek FJ, Banovac K. Effect of nonsteroidal antiinflammatory drugs on fracture healing: a laboratory study in rats. J Orthop Trauma. 1995;9:392–400. doi: 10.1097/00005131-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Blokhuis TJ, Frölke JP. Is radiation superior to indomethacin to prevent heterotopic ossification in acetabular fractures? A systematic review. Clin Orthop Relat Res. 2009;467:526–530. doi: 10.1007/s11999-008-0532-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosse MJ, Poka A, Reinert CM, Ellwanger F, Slawson R, McDevitt ER. Heterotopic ossification as a complication of acetabular fracture. Prophylaxis with low-dose irradiation. J Bone Joint Surg Am. 1988;70:1231–1237. [PubMed] [Google Scholar]
- 4.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 5.Burd TA, Hughes MS, Anglen JO. Heterotopic ossification prophylaxis with indomethacin increases the risk of long-bone nonunion. J Bone Joint Surg Br. 2003;85:700–705. [PubMed] [Google Scholar]
- 6.Burd TA, Lowry KJ, Anglen JO. Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am. 2001;83:1783–1788. doi: 10.2106/00004623-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Daum WJ, Scarborough MT, Gordon W, Uchida T. Heterotopic ossification and other perioperative complications of acetabular fractures. J Orthop Trauma. 1992;6:427–432. doi: 10.1097/00005131-199212000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Elmstedt E, Lindholm TS, Nillson OS, Tornkvist H. Effect of ibuprofen on heterotopic ossification after hip replacement. Acta Orthop Scand. 1985;56:25–27. doi: 10.3109/17453678508992973. [DOI] [PubMed] [Google Scholar]
- 9.Ghalambor N, Matta JM, Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture. An analysis of risk factors. Clin Orthop Relat Res. 1994;305:96–105. doi: 10.1097/00003086-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Giannoudis PV, Grotz MRW, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 11.Johnson EE, Kay RM, Dorey FJ. Heterotopic ossification prophylaxis following operative treatment of acetabular fracture. Clin Orthop Relat Res. 1994;305:88–95. [PubMed] [Google Scholar]
- 12.Kaempffe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5:439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Karunakar MA, Sen A, Bosse MJ, Sims SH, Goulet JA, Kellam JF. Indomethacin as prophylaxis for heterotopic ossification after the operative treatment of fractures of the acetabulum. J Bone Joint Surg Br. 2006;88:1613–1617. doi: 10.1302/0301-620X.88B12.18151. [DOI] [PubMed] [Google Scholar]
- 14.Letournel E, Judet R. Fractures of the Acetabulum. 2. Berlin, Germany: Springer-Verlag; 1993. [Google Scholar]
- 15.Matta JM, Siebenrock KA. Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? A prospective randomised study. J Bone Joint Surg Br. 1997;79:959–963. doi: 10.1302/0301-620X.79B6.6889. [DOI] [PubMed] [Google Scholar]
- 16.McLaren AC. Prophylaxis with indomethacin for heterotopic bone. After open reduction of fractures of the acetabulum. J Bone Joint Surg Am. 1990;72:245–247. [PubMed] [Google Scholar]
- 17.Moed BR, Karges DE. Prophylactic indomethacin for the prevention of heterotopic ossification after acetabular fracture surgery in high-risk patients. J Orthop Trauma. 1994;8:34–39. doi: 10.1097/00005131-199402000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Moed BR, Maxey JW. The effect of indomethacin on heterotopic ossification following acetabular fracture surgery. J Orthop Trauma. 1993;7:33–38. doi: 10.1097/00005131-199302000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Moed BR, Smith ST. Three-view radiographic assessment of heterotopic ossification after acetabular fracture surgery. J Orthop Trauma. 1996;10:93–98. doi: 10.1097/00005131-199602000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Moore KD, Goss K, Anglen JO. Indomethacin versus radiation therapy for prophylaxis against heterotopic ossification in acetabular fractures: a randomized, prospective study. J Bone Joint Surg Br. 1998;80:259–263. doi: 10.1302/0301-620X.80B2.8157. [DOI] [PubMed] [Google Scholar]
- 21.Nilsson OS, Bauer HCF, Brosjo O, Tornkvist H. Influence of indomethacin on induced heterotopic bone formation in rats: importance of length of treatment and of age. Clin Orthop Relat Res. 1986;207:239–245. [PubMed] [Google Scholar]
- 22.Pagnani MJ, Pellicci PM, Salvati EA. Effect of aspirin on heterotopic ossification after total hip arthroplasty in men who have osteoarthritis. J Bone Joint Surg Am. 1991;73:924–929. [PubMed] [Google Scholar]
- 23.Pape HC, Lehmann U, van GM, Gansslen A, von GS, Krettek C. Heterotopic ossifications in patients after severe blunt trauma with and without head trauma: incidence and patterns of distribution. J Orthop Trauma. 2001;15:229–237. doi: 10.1097/00005131-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Rath EM, Russell GV, Jr, Washington WJ, Routt ML., Jr Gluteus minimus necrotic muscle debridement diminishes heterotopic ossification after acetabular fracture fixation. Injury. 2002;33:751–756. doi: 10.1016/S0020-1383(01)00194-2. [DOI] [PubMed] [Google Scholar]
- 25.Siebenrock KA, Gautier E, Ziran BH, Ganz R. Trochanteric flip osteotomy for cranial extension and muscle protection in acetabular fracture fixation using a Kocher-Langenbeck approach. J Orthop Trauma. 2006;20:S52–S56. doi: 10.1097/01.bot.0000177103.99488.fe. [DOI] [PubMed] [Google Scholar]
- 26.Tornkvist H, Nilsson OS, Bauer FCH, Lindholm TS. Experimentally induced heterotopic ossification in rats influenced by anti-inflammatory drugs. Scand J Rheumatol. 1983;12:177–180. doi: 10.3109/03009748309102907. [DOI] [PubMed] [Google Scholar]
- 27.Webb LX, Bosse MJ, Mayo KA, Lange RH, Miller ME, Swiontkowski MF. Results in patients with craniocerebral trauma and an operatively managed acetabular fracture. J Orthop Trauma. 1990;4:376–382. [PubMed] [Google Scholar]