Abstract
Background
Closed reduction and percutaneous pin fixation is considered standard management for displaced supracondylar fractures of the humerus in children. However, controversy exists regarding whether to use an isolated lateral entry or a crossed medial and lateral pinning technique.
Questions/purposes
We performed a meta-analysis of randomized controlled trials (RCTs) to compare (1) the risk of iatrogenic ulnar nerve injury caused by pin fixation, (2) the quality of fracture reduction in terms of the radiographic outcomes, and (3) function in terms of criteria of Flynn et al. and elbow ROM, and other surgical complications caused by pin fixation.
Methods
We searched PubMed, Embase, the Cochrane Library, and other unpublished studies without language restriction. Seven RCTs involving 521 patients were included. Two authors independently assessed the methodologic quality of the included studies with use of the Detsky score. The median Detsky quality score of the included trials was 15.7 points. Dichotomous variables were presented as risk ratios (RRs) or risk difference with 95% confidence intervals (CIs) and continuous data were measured as mean differences with 95% CI. Statistical heterogeneity between studies was formally tested with standard chi-square test and I2 statistic. For the primary objective, a funnel plot of the primary end point and Egger’s test were performed to detect publication bias.
Results
The pooled RR suggested that iatrogenic ulnar nerve injury was higher with the crossed pinning technique than with the lateral entry technique (RR, 0.30; 95% CI, 0.10–0.89). No publication bias was further detected. There were no statistical differences in radiographic outcomes, function, and other surgical complications. No significant heterogeneity was found in these pooled results.
Conclusions
We conclude that the crossed pinning fixation is more at risk for iatrogenic ulnar nerve injury than the lateral pinning technique. Therefore, we recommend the lateral pinning technique for supracondylar fractures of the humerus in children.
Level of Evidence
Level I, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Supracondylar humeral fractures are the most common elbow fractures seen in children [36, 41]. These fractures are classified according to Gartland’s criteria as nondisplaced fractures (Type I), hinged fractures with the posterior cortex intact (Type II), and completely displaced fractures (Type III) [15].
Percutaneous pinning of supracondylar humerus fractures in children is an effective way to maintain an anatomic reduction after closed reduction of a displaced fracture and was first described by Casiano in 1960 [7]. Since that time, closed reduction and percutaneous pin fixation has evolved as the standard treatment for displaced supracondylar fractures in children [41]. Two basic techniques of pin configuration exist: a lateral entry pin technique and a medial and lateral (crossed) pin technique. Previous studies have shown that increased biomechanical stability is probably the advantage of medial and lateral entry pin fixation, although iatrogenic ulnar nerve injury may result from placement of the medial pin [27, 31, 34, 43, 53, 56, 60]. Conversely, lateral-only pins have been used in an attempt to avoid ulnar nerve injury, although the construct may be less stable biomechanically [8, 17, 26, 31, 34, 46]. Therefore, controversy persists regarding whether to use an isolated lateral entry or a crossed medial and lateral pinning technique for displaced supracondylar fractures of the humerus in children [23, 30, 42, 44, 45].
Although several meta-analyses or systematic reviews of lateral entry versus crossed medial and lateral entry pinning for supracondylar fractures of the humerus have been reported [3, 5, 29, 38, 52, 57], the conclusions drawn are based largely on results from nonrandomized controlled trials (nRCTs), which increases the likelihood that bias has affected those analyses. Randomized controlled trials (RCTs) are considered to be the most reliable form of scientific evidence in the hierarchy of evidence because they reduce spurious inferences of causality and bias. Numerous RCTs have been published on this topic [2, 16, 35, 54, 55], which provides the opportunity for us to perform a meta-analysis of RCTs comparing lateral entry pin fixation with crossed medial and lateral entry pin fixation of displaced supracondylar fractures of the humerus in children.
In this meta-analysis, we sought to determine which technique (lateral or crossed medial and lateral pinning) is associated with (1) a higher risk of iatrogenic ulnar nerve injury caused by pin fixation, (2) a better quality of fracture reduction in terms of the radiographic outcomes, and (3) better functional outcomes in terms of criteria of Flynn et al. and elbow ROM, and fewer other surgical complications caused by pin fixation.
Search Strategy and Criteria
We searched PubMed (1966 to August 2012), Embase (1974 to August 2012), and the Cochrane Library (Issue 8 of 12, August 2012). The following key words were used for the searches: supracondylar fracture, humerus or humeral, pin or Kirschner wire, and children or pediatric. The electronic databases were supplemented by searching for gray literature including unpublished trials or trials in progress up to August 2012. Specifically, we searched Google, ClinicalTrials.gov, World Health Organization International Clinical Trials Registry Platform, International Standard Randomised Controlled Trial Number Register, and the National Research Register Archive. No restriction for language was applied.
RCTs have been regarded as superior to nRCTs because of the biases that can arise in nRCTs and the diverging results of nRCTs relative to RCTs. Therefore, only RCTs or quasi-RCTs comparing lateral entry pin with crossed entry pin fixation methods for supracondylar fractures of the humerus were considered for inclusion. Quasi-RCTs were defined as those in which randomization is inadequately concealed (ie, patients are allocated according to known characteristics such as date of birth, hospital chart number, or day of presentation).
We systematically reviewed RCTs according to the following criteria: (1) a target population of children between 1 and 12 years of age; (2) displaced supracondylar fractures of the humerus, including Gartland Types II and III; (3) RCTs involving comparison of lateral entry versus medial and lateral entry pin fixation; and (4) although patients included should be treated using closed reduction, a few with open reduction in RCTs also were included.
Two investigators (PZ, JW) independently reviewed all titles, abstracts, ongoing trials, and the full text of articles that potentially were eligible based on abstract review. Reviewers were not blinded to authors, journal, or source of financial support. Any disagreements were resolved by discussion between two authors (PZ, JW) and, when necessary, further discussion with another independent investigator (JGZ).
For each included study, two authors (PZ, JW) independently extracted data using a piloted data extraction form. Disagreement was resolved by consensus or a third author (JGZ). All relevant information regarding baseline characteristics of the patient population, sample size, inclusion and exclusion criteria, intervention, followup time, and various data of radiographic or clinical outcomes were abstracted from each eligible trial. The baseline characteristics of the enrolled patients included the average age, sex, neurovascular status, types of fracture, types of displacement, and time of injury. When necessary, we contacted the investigators of original studies for additional information.
We initially identified 881 titles, abstracts, and ongoing trials (Fig. 1). According to the inclusion and exclusion criteria, seven RCTs involving 521 patients were included in this meta-analysis with individual sample sizes ranging from 40 to 160 patients (Appendix 1) [2, 14, 16, 28, 35, 54, 55]. Of these 521 patients, 256 were randomly assigned to the lateral entry group and 265 were assigned to the medial and lateral entry group. Three trials [16, 28, 55] included patients with Gartland Type III fractures and four [2, 14, 35, 54] included patients with Gartland Types II and III fractures. Two-pin (two lateral pins or crossed pins) fixation was used initially in all trials. Of the seven studies, three justified unstable reduction using a third pin [16, 54, 55]. A miniopen technique of medial pinning was used in three studies [28, 35, 55]. Six of the trials described the time of injury [2, 14, 16, 28, 35, 55] and one trial [54] was unclear (Table 1).
Fig. 1.
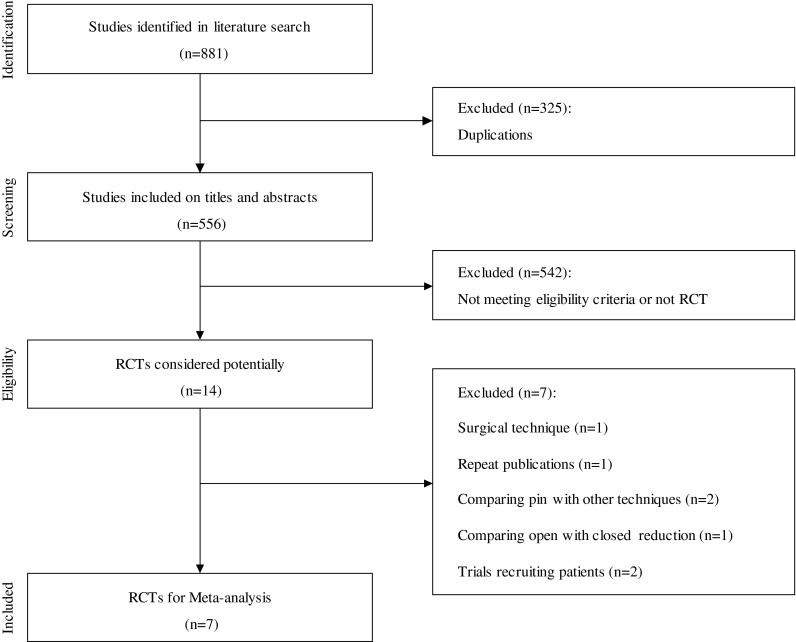
This flow chart summarizes our study selection process, the exclusion steps, and the resulting studies that were left for analysis. RCT = randomized controlled trial.
Table 1.
Characteristics of included studies
| Study | Time of injury | Fracture type | Miniopen technique* | Patients | Patients with a third pin | Iatrogenic ulnar nerve injury | |||
|---|---|---|---|---|---|---|---|---|---|
| LG | CG | LG | CG | LG | CG | ||||
| Foead et al. [14] | Within 72 hours | Gartland II and III | No | 27 | 28 | 0 | 0 | 2 | 5 |
| Kocher et al. [28] | Within 48 hours | Gartland III | Yes | 28 | 24 | 0 | 0 | 0 | 0 |
| Tripuraneni et al. [54] | N/A | Gartland II and III | No | 20 | 20 | 8 | 5 | 0 | 1 |
| Vaidya [55] | Within 96 hours | Gartland III | Yes | 29 | 31 | N/A | N/A | 0 | 3 |
| Gaston et al. [16] | Within 24 hours | Gartland III | No | 47 | 57 | 5 | 8 | 0 | 2 |
| Anwar et al. [2] | Within 72 hours | Gartland II and III | No | 25 | 25 | 0 | 0 | 0 | 1 |
| Maity et al. [35] | Within 72 hours | Gartland II and III | Yes | 80 | 80 | 0 | 0 | 0 | 0 |
| Totals | 256 | 265 | ≥ 13 | ≥ 13 | 2 | 12 | |||
* Was this performed for medial pinning; LG = lateral group; CG = crossed group; N/A = not available.
Two authors (JGZ and JW) independently assessed the methodologic quality of the included studies with use of the Detsky score [10] (maximum, 21 points). Disagreements were resolved by discussion to achieve consensus. The Detsky score has been used to determine the quality of published orthopaedic RCTs and has shown good consistency and reliability [4]. This scale evaluates randomization, description of outcome measures, inclusion and exclusion criteria, description of therapy, and statistics. A quality score greater than 75% is considered to indicate high quality; greater than 50% and less than 75%, moderate quality; and less than 50%, low quality. Low-quality RCTs were excluded to ensure the power of this meta-analysis.
The Detsky quality index scores [10] (maximum, 21 points) for the included trials ranged from 13 to 19 points (median, 15.7 points). We found no studies to be of low quality. Five trials [2, 14, 28, 35, 55] reported adequate generation of the allocation sequence and two of them [28, 35] reported allocation concealment. There were no major differences in five trials [16, 28, 35, 54, 55] regarding baseline characteristics, and one [14] only described the similar interval from injury to admission and surgery. It was not clear whether outcome assessors were blinded to the procedure in all trials [2, 14, 16, 28, 35, 54, 55]. Loss to followup rate was considered to be acceptable in all trials (within 20%). Four trials [16, 28, 35, 54] performed intention-to-treat analysis (Table 2).
Table 2.
Methodologic quality of included studies
| Study | Adequate randomization | Conceal allocation | Blinded assessor | Similar baseline | ITT analysis | Loss to followup | Detsky scores* |
|---|---|---|---|---|---|---|---|
| Foead et al. [14] | Yes | N/A | N/A | N/A | No | 16.7% | 15 |
| Kocher et al. [28] | Yes | Yes | N/A | Yes | Yes | 0% | 19 |
| Tripuraneni et al. [54] | Partial† | N/A | N/A | Yes | Yes | 0% | 14 |
| Vaidya [55] | Yes | N/A | N/A | Yes | No | 9.1% | 14 |
| Gaston et al. [16] | Partial† | N/A | N/A | Yes | Yes | 13.2% | 15 |
| Anwar et al. [2] | Yes | N/A | N/A | N/A | No | 0% | 13 |
| Maity et al. [35] | Yes | Yes | N/A | Yes | Yes | 18.8% | 18 |
* Detsky score is designed to evaluate the quality of a randomized clinical trial (maximum score 21); †quasirandomized controlled trials were considered as partial randomization (ie, patients are allocated according to known characteristics such as date of birth, hospital chart number, or day of presentation); ITT = intention-to-treat; N/A = not available.
The primary objective of our study was to identify the relative risk of iatrogenic ulnar nerve injury between lateral entry and crossed entry pin fixation. Secondary objectives were to assess several outcomes such as radiographic outcomes (Baumann angle, carrying angle, humerocapitellar angle, change in Baumann angle, loss of carrying angle, change in humerocapitellar angle, and loss of reduction), function (ROM, criteria described by Flynn et al. [13], loss of elbow flexion and extension, and return to function), and other surgical complications (infection, reoperation, and compartment syndrome). Loss of reduction also was determined on the basis of the change in the Baumann angle according to the criteria reported by Skaggs et al. [49]: no displacement was defined as a change in the Baumann angle less than 6°; mild displacement as a change of 6° to 12°; and major displacement as a change greater than 12°. Moreover, the functional results were graded according to the criteria of Flynn et al. that weres based on the carrying angle and elbow motion [13].
Dichotomous variables were presented as risk ratios (RRs) or risk difference with 95% confidence intervals (CIs) and continuous data were measured as mean differences with 95% CI. To establish inconsistency in the study results, statistical heterogeneity between studies was formally tested with the standard chi-square test [25]. We also determined the I2 statistic (I² = 100% × [Q − df]/Q, where Q is the chi-square statistic and df is its degrees of freedom), which yields values between 0% and 100% with higher values denoting a greater degree of heterogeneity (0% ≤ I2 < 25%, no heterogeneity; 25% ≤ I2 < 50%, moderate heterogeneity; 50% ≤ I2 < 75%, large heterogeneity; and 75% ≤ I2 < 100%, extreme heterogeneity). If neither clinical nor statistical heterogeneity was found, we pooled results using a fixed-effect model with the significance level set at p = 0.05. The Review Manager (RevMan, Copenhagen, Denmark, The Nordic Cochrane Centre) software program was used for graphic representation of the pooled data.
If possible, studies were categorized into different subgroup analyses according to the number of pins (two pins versus three pins), time of injury (within 12 hours versus more than 12 hours), operative method (miniopen versus nonopen for medial pinning), and fracture type (Gartland Type II versus Gartland Type III). We performed meta-regression analysis if the included studies were no fewer than 10 because the small number of studies is prone to misleading false-positive results [24].
For the primary objective, publication bias was assessed through the construction of a funnel plot for the primary end point. Egger’s test, as described by Egger et al. [12], also was performed to detect publication bias (p < 0.05 indicating statistical significance) using Stata/SE12.0 (Stata Corporation, College Station, TX, USA).
Results
Iatrogenic ulnar nerve injury occurred more commonly in patients treated with crossed medial and lateral pins than in patients with isolated lateral pins (RR, 0.30; 95% CI, 0.10–0.89; p = 0.03) (Fig. 2). The test for heterogeneity showed that no important heterogeneity existed in these meta-analysis pooled results (I2 = 0%). All included RCTs reported on the end point of iatrogenic ulnar nerve injury; it occurred in 12 (4.5%) of 265 patients with medial and lateral entry pins and in two (0.78%) of 256 patients with isolated lateral entry pins. Other subgroup assessments according to the number of pins, time of injury, fracture type, and miniopen technique of crossed pinning were not performed because of the existence of heterogeneity and the small number of studies. A funnel plot of iatrogenic ulnar nerve injury was performed to evaluate publication bias (Fig. 3). No publication bias was detected by Egger’s test (t = −1.60; p > |t| = 0.208; 95% CI, 1.83–0.61). Meta-regression analysis was not performed because of the small number of included studies. Four studies reported the recovery from iatrogenic ulnar nerve injury [2, 14, 16, 54]. Ten of 11 patients with iatrogenic ulnar nerve injury recovered completely after surgery. One patient had incomplete resolution of ulnar nerve symptoms with limited 3-month clinic followup [16].
Fig. 2.
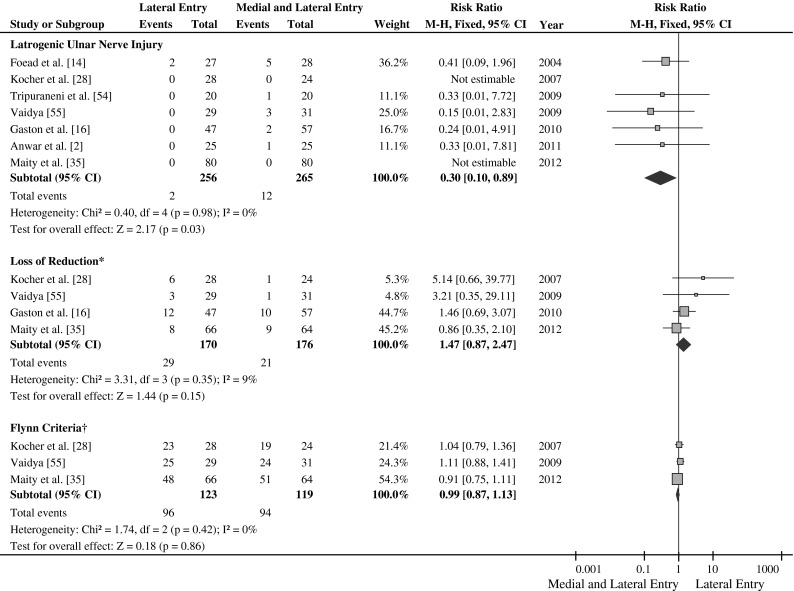
Comparisons of iatrogenic ulnar nerve injury, loss of reduction, and Flynn criteria between lateral entry and crossed entry pin fixation are shown. The size of each square is proportional to the weight of the study. *Mild or major displacement (change in the Baumann angle > 6°) based on the criteria of Skaggs et al. [49]; †excellent grading of Flynn criteria [13]; M-H = Mantel-Haenszel; Fixed = fixed effect; Z = p value of weighted test for overall effect; df = degrees of freedom; I2 = test statistic; CI = confidence interval.
Fig. 3.
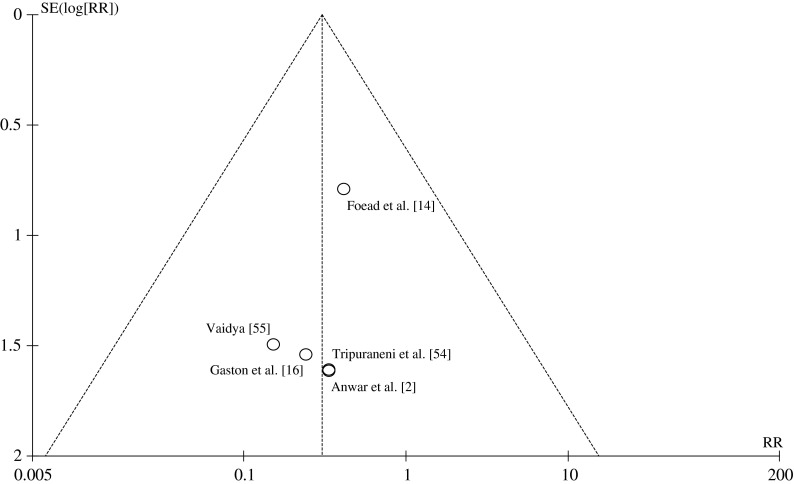
This is a funnel plot of iatrogenic ulnar nerve injury to assess publication bias. SE = standard error; RR = risk ratio.
The meta-analysis identified no significant differences between the two surgical techniques compared in terms of carrying angle, loss of carrying angle, Baumann angle, change in Baumann angle, humerocapitellar angle, change in humerocapitellar angle, or loss of reduction based on the criteria of Skaggs et al. [49] (Fig. 2). No statistical heterogeneity was found in these meta-analysis pooled results (Table 3).
Table 3.
Summary of the meta-analysis
| Analysis item | Studies | Patients | Heterogeneity | Statistical method | Effect estimate | p value | |
|---|---|---|---|---|---|---|---|
| I2 | p | ||||||
| Radiographic outcomes | |||||||
| Carrying angle | 2 | 182 | 0% | 0.95 | MD (IV, fixed, 95% CI) | 0.08 (−0.73 to 0.90) | 0.85 |
| Loss of carrying angle | 4 | 295 | 0% | 0.98 | MD (IV, fixed, 95% CI) | 0.11 (−0.52 to 0.74) | 0.73 |
| Baumann angle | 3 | 222 | 0% | 0.76 | MD (IV, fixed, 95% CI) | −0.97 (−2.19 to 0.25) | 0.12 |
| Change in Baumann angle | 5 | 347 | 0% | 0.89 | MD (IV, fixed, 95% CI) | −0.03 (−0.62 to 0.57) | 0.93 |
| Humerocapitellar angle | 2 | 92 | 0% | 0.46 | MD (IV, fixed, 95% CI) | −1.69 (−3.89 to 0.52) | 0.13 |
| Change in humerocapitellar angle | 2 | 112 | 0% | 0.96 | MD (IV, fixed, 95% CI) | −0.25 (−2.20 to 1.70) | 0.80 |
| Loss of reduction* | 4 | 346 | 9% | 0.35 | RR (M-H, fixed, 95% CI) | 1.47 (0.87 to 2.47) | 0.15 |
| Functional outcomes | |||||||
| Criteria of Flynn et al.† | 3 | 242 | 0% | 0.42 | RR (M-H, fixed, 95% CI) | 0.99 (0.87 to 1.13) | 0.86 |
| Full return to function | 2 | 112 | 0% | 0.48 | RR (M-H, fixed, 95% CI) | 1.00 (0.92 to 1.09) | 0.96 |
| Loss of elbow flexion | 2 | 105 | 0% | 0.35 | MD (IV, fixed, 95% CI) | 0.31 (−1.34 to 1.95) | 0.71 |
| Loss of elbow extension | 2 | 105 | 0% | 0.91 | MD (IV, fixed, 95% CI) | 0.33 (−1.38 to 2.03) | 0.71 |
| Complications | |||||||
| Iatrogenic ulnar nerve injury | 7 | 521 | 0% | 0.98 | RR (M-H, fixed, 95% CI) | 0.30 (0.10 to 0.89) | 0.03 |
| Reoperation | 3 | 216 | 0% | 0.83 | RR (M-H, fixed, 95% CI) | 0.19 (0.02 to 1.52) | 0.12 |
| Pin tract infection | 3 | 242 | 0% | 0.48 | RR (M-H, fixed, 95% CI) | 1.01 (0.26 to 3.93) | 0.99 |
| Superficial infection | 3 | 152 | 0% | 0.76 | RR (M-H, fixed, 95% CI) | 0.42 (0.07 to 2.72) | 0.36 |
| Compartment syndrome | 3 | 209 | 0% | 1.00 | RD (M-H, fixed, 95% CI) | 0.00 (−0.03 to 0.03) | 1.00 |
* Mild or major displacement (change in the Baumann angle > 6°) based on the criteria of Skaggs et al. [49]; †excellent grading of criteria of Flynn et al. [13]; MD = mean difference; RR = risk ratio; RD = risk difference; IV = inverse variance; M-H = Mantel-Haenszel; fixed = fixed effect; CI = confidence interval.
We also identified no differences in functional outcomes and other complications between patients treated with crossed medial and lateral pins and those treated with isolated lateral pins as identified by the criteria of Flynn et al. (Fig. 2), return to function, loss of elbow flexion and extension, pin tract infection, superficial infection, reoperation, or compartment syndrome (Table 3). No statistical heterogeneity (I2 = 0%) was found in these meta-analysis pooled results.
Discussion
Recently a questionnaire described by Lee et al. showed general orthopaedic surgeons tended to prefer the lateral pinning technique to the crossed pinning technique [30]. However, no statistically significant difference was found between pediatric orthopaedic surgeons and hand surgeons in the choice between lateral and crossed pinning techniques [30]. Several RCTs have been published on this topic [2, 16, 35, 54, 55], which provides the opportunity to perform a meta-analysis to help resolve this controversy. We therefore performed a meta-analysis of the available RCTs comparing lateral entry pin fixation with medial and lateral entry pin fixation of displaced supracondylar fractures of the humerus in children to determine whether one technique is safer in terms of ulnar nerve injuries or results in better radiographic or functional outcomes.
Some possible limitations to this meta-analysis should be acknowledged. First, the most prevalent methodologic shortcomings appeared to be the small size of populations and inappropriate design of RCTs. A Detsky quality score less than 50% is considered to indicate low quality in this meta-analysis. However, we found no studies to be of low quality. Second, although no publication bias was found using a funnel plot and Egger’s test, the small number of included RCTs weakens the power of those tests. Third, inconsistent interventions exist in included studies. Several factors such as surgical technique, fracture type, number of pins, and time of injury may modify comparing the results between the interventions [17, 18, 20, 32, 51] . Direct observation of the medial epicondyle can ensure the pin is not placed in the ulnar nerve groove [58]. Previous studies have shown the miniopen technique of crossed entry pin associated with a low incidence of ulnar nerve injury [18, 20, 32]. Whether a third pin should be added to be more stable is controversial [19, 46], but it may lead simultaneously to the increased risk of nerve injury [51, 58]. Different results have been affected by the time from injury to surgery [11, 21, 22, 33, 45, 47]. In our meta-analysis, the time from injury to surgery of the included trials was inconsistent. It is difficult to take into account the above various confounders.
Iatrogenic ulnar nerve injury is one of the most important issues regarding pin configuration of supracondylar humeral fractures. The pooled result of iatrogenic ulnar nerve injury in the current study is in agreement with previous reviews [1, 3, 5, 38, 40, 52]. Babal et al. [3] performed a meta-analysis which was derived almost exclusively from retrospective studies and concluded that the medial pin carried the greater overall risk of nerve injury as compared with a lateral-pin-only construct, and that the ulnar nerve was at risk of injury in patients who had medial pins. In a systematic review, Brauer et al. [5] reported the probability of iatrogenic nerve injury was 1.84 times higher with medial and lateral pins than with a lateral entry pin alone. In this meta-analysis of prospective RCTs, we observed a large difference in the incidence of iatrogenic ulnar nerve injury between the two methods of fixation. Although we attempted to perform the subgroup analysis according to the previously mentioned factors, the existence of heterogeneity and the small number of studies make it difficult. Although iatrogenic ulnar nerve injury does not necessarily result from direct penetration of the ulnar nerve, it can be caused by stretch over the medial pin, tethering in the cubital tunnel, or anterior fixation over the medial epicondyle [58]. Neural recovery, regardless of which nerve is injured, generally occurs after 2 to 2.5 months of observation, but it may take up to 6 months [6]. Our study also showed the majority of patients with ulnar nerve injuries recovered completely during followup.
For loss of reduction and deformity, inconsistent results were reported in previous studies [5, 9, 37, 39, 48, 50, 59]. Skaggs et al. [50] retrospectively reviewed the results of reduction and pin fixation of 345 extension-type supracondylar fractures in children and found there was no difference regarding maintenance of fracture reduction between the crossed pins and the lateral pins. Omid et al. [40] considered that lateral entry pins could be as stable as crossed pinning in biomechanical and clinical studies if they are well spaced at the fracture line. A systematic review performed by Brauer et al. [5] showed that deformity occurred in 3.4% of the patients treated with medial and lateral entry pins and in 5.9% of patients treated with lateral entry pins, therefore concluding that medial and lateral pin entry provides a more stable configuration and the probability of deformity or loss of reduction is 0.58 times lower than with isolated lateral pin entry. Our meta-analysis included RCTs showing there are no differences in radiographic outcomes between the two methods.
We also reviewed several postoperative functional outcomes and other surgical complications in this meta-analysis. End points we studied included the criteria of Flynn et al. [13], loss of elbow flexion and extension, and return to function. Pin tract infection, superficial infection, reoperation, and compartment syndrome also were compared. Previous systematic reviews were aimed mainly at iatrogenic nerve injury, deformity, or loss of reduction [3, 5, 29, 38, 52]. Few meta-analyses or systematic reviews compared the postoperative functional outcomes. Woratanarat et al. [57] performed a meta-analysis to compare the criteria of Flynn et al. for the two pin fixation techniques, but there were insufficient RCTs to pool data until September 2007. The current meta-analysis included three studies which reported the criteria of Flynn et al. Further, no major differences were found concerning the outcomes between the lateral entry pin and crossed entry pin in our meta-analysis.
Based on our meta-analysis of prospective RCTs, we conclude crossed medial and lateral pinning results in a higher risk of iatrogenic ulnar nerve injury than the lateral pinning technique for displaced supracondylar fractures of the humerus in children. Lateral entry pin fixation was not found to be different from medial and lateral entry pin fixation in terms of radiographic outcomes, function, and other surgical complications. Therefore, we recommend the lateral pinning technique for supracondylar fractures of the humerus in children.
Acknowledgments
We thank the professional staff of Tianjin Medical Information Center and Tianjin Medical Library for providing assistance. We also thank the patients and clinical researchers who were involved in the publications mentioned in our article.
Appendix 1. Detailed characteristics of included studies
| Variable | Foead et al. [14] | Kocher et al. [28] | Tripuraneni et al. [54] | Vaidya [55] | Gaston et al. [16] | Anwar et al. [2] | Maity et al. [35] |
|---|---|---|---|---|---|---|---|
| Year | 2004 | 2007 | 2009 | 2009 | 2010 | 2011 | 2012 |
| Design type | RCT | RCT | Quasi-RCT | RCT | Quasi-RCT | RCT | RCT |
| Populations | |||||||
| Number | |||||||
| Lateral group | 27 | 28 | 20 | 29 | 47 | 25 | 80 |
| Crossed group | 28 | 24 | 20 | 31 | 57 | 25 | 80 |
| Age (years) | 5.78 | 7.02 | |||||
| Lateral group | 6.1 | 4.3 | 5.8 | 5.7 | 6.12 | ||
| Crossed group | 5.7 | 5.5 | 6.2 | 6.2 | 6.24 | ||
| Male: female | Unclear | Unclear | 33:17 | ||||
| Lateral group | 10:18 | 21:8 | 22:25 | 51:29 | |||
| Crossed group | 13:11 | 17:14 | 31:26 | 48:32 | |||
| Gartland type | II and III | III | II and III | III | III | II and III | II and III |
| Inclusion criteria | Closed extension fracture; within 72 hours of injury | Closed extension fracture; within 48 hours of injury | No restriction for open, multiple and compound fracture (total 3 patients) | Closed fracture; within 96 hours of injury | Closed extension fracture; within 24 hours of injury | Closed fracture; within 72 hours of injury | Closed extension fracture; within 72 hours of injury |
| Exclusion criteria | Multiple fracture; compound fracture; previous fracture | Multiple fracture; compound fracture; previous fracture; open reduction | Revision fixation cases | Multiple fracture; compound fracture; previous fracture; open reduction | Inadequate perioperative radiographs | Neurovascular complications; open reduction and internal fixation | Multiple fracture; compound fracture; previous fracture; open reduction |
| Interventions | |||||||
| Lateral group | Closed reduction and two lateral pins | Closed reduction and two lateral pins | Closed reduction and two lateral pins; 8 patients with a third pin | Closed reduction and two or three lateral pins | Closed reduction and two lateral pins; 5 patients with a third pin; 3 open reductions | Closed reduction and two lateral pins | Closed reduction and two lateral pins |
| Crossed group | Closed reduction and two crossed pins | Closed reduction and two crossed pins | Closed reduction and two crossed pins; 5 patients with a third pin; one open reduction | Closed reduction with one medial and one or two lateral pins | Closed reduction and two crossed pins; 8 patients with a third pin; 5 open reduction | Closed reduction and two crossed pins | Closed reduction and two crossed pins |
| Outcomes | |||||||
| Radiographic outcomes | Change in carrying angle, Baumann angle, and medial epicondylar epiphyseal angle | Baumann, carrying and humerocapitellar angle; change in Baumann and Humerocapitellar angle; loss of reduction | Baumann angle, Humerotrochlear angle | Change in carrying angle, change in Baumann and Humerocapitellar angle; loss of reduction | Humerocapitellar angle; change in Baumann and Humerocapitellar angle; loss of reduction | Change in Baumann angle; loss of carrying angle; loss of metaphyseal diaphyseal angle | Baumann and carrying angle; change in Baumann angle; loss of carrying angle; loss of reduction |
| Functional outcomes | Loss of extension and flexion | Range of motion; Flynn criteria; return to function | Range of motion | Range of motion; Flynn criteria; return to function | Flynn criteria; loss of extension and flexion | Range of motion; Flynn criteria | |
| Complications | Iatrogenic nerve injury; infection; vascular injury; compartment syndrome | Iatrogenic nerve injury; infection; reoperation | Iatrogenic nerve injury; infection | Iatrogenic nerve injury; infection; reoperation | Iatrogenic nerve injury; reoperation; compartment syndrome | Iatrogenic nerve injury; compartment syndrome | Iatrogenic nerve injury; infection |
| Followup | 8.9 months | 3 months | 6 months | Unclear | 6 months | 3 months | |
| Lateral group | 65.1 days | ||||||
| Crossed group | 54.6 days | ||||||
Quasi-RCTs were defined as those in which randomization is inadequately concealed (ie, patients are allocated according to known characteristics such as date of birth, hospital chart number, or day of presentation); RCT = randomized controlled trial.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This work was performed at Department of Orthopaedic Surgery, Tianjin Hospital, Tianjin, China.
References
- 1.Abzug JM, Herman MJ. Management of supracondylar humerus fractures in children: current concepts. J Am Acad Orthop Surg. 2012;20:69–77. doi: 10.5435/JAAOS-20-02-069. [DOI] [PubMed] [Google Scholar]
- 2.Anwar W, Rahman N, Iqbal MJ, Khan MA. Comparison of the two methods of percutaneous K-wire fixation in displaced supracondylar fracture of humerus in children. J Postgrad Med Inst. 2011;25:356–361. [Google Scholar]
- 3.Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30:253–263. doi: 10.1097/BPO.0b013e3181d213a6. [DOI] [PubMed] [Google Scholar]
- 4.Bhandari M, Richards RR, Sprague S, Schemitsch EH. The quality of reporting of randomized trials in the Journal of Bone and Joint Surgery from 1988 through 2000. J Bone Joint Surg Am. 2002;84:388–396. doi: 10.1302/0301-620X.84B7.12532. [DOI] [PubMed] [Google Scholar]
- 5.Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27:181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 6.Brown IC, Zinar DM. Traumatic and iatrogenic neurological complications after supracondylar humerus fractures in children. J Pediatr Orthop. 1995;15:440–443. doi: 10.1097/01241398-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Casiano E. Reduction and fixation by pinning “banderillero” style-fractures of the humerus at the elbow in children. Mil Med. 1960;125:262–264. [PubMed] [Google Scholar]
- 8.Davis RT, Gorczyca JT, Pugh K. Supracondylar humerus fractures in children: comparison of operative treatment methods. Clin Orthop Relat Res. 2000;376:49–55. doi: 10.1097/00003086-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 9.de las Heras J, Duran D, de la Cerda J, Romanillos O, Martinez-Miranda J, Rodriguez-Merchan EC. Supracondylar fractures of the humerus in children. Clin Orthop Relat Res. 2005;432:57–64. [DOI] [PubMed]
- 10.Detsky AS, Naylor CD, O’Rourke K, McGeer AJ, L’Abbe KA. Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol. 1992;45:255–265. doi: 10.1016/0895-4356(92)90085-2. [DOI] [PubMed] [Google Scholar]
- 11.Donnelly M, Green C, Kelly IP. An inconvenient truth: treatment of displaced paediatric supracondylar humeral fractures. Surgeon. 2012;10:143–147. doi: 10.1016/j.surge.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children: sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;56:263–272. [PubMed] [Google Scholar]
- 14.Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong). 2004;12:76–82. doi: 10.1177/230949900401200114. [DOI] [PubMed] [Google Scholar]
- 15.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109:145–154. [PubMed] [Google Scholar]
- 16.Gaston RG, Cates TB, Devito D, Schmitz M, Schrader T, Busch M, Fabregas J, Rosenberg E, Blanco J. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010;30:799–806. doi: 10.1097/BPO.0b013e3181f73d59. [DOI] [PubMed] [Google Scholar]
- 17.Gordon JE, Patton CM, Luhmann SJ, Bassett GS, Schoenecker PL. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J Pediatr Orthop. 2001;21:313–318. [PubMed] [Google Scholar]
- 18.Gosens T, Bongers KJ. Neurovascular complications and functional outcome in displaced supracondylar fractures of the humerus in children. Injury. 2003;34:267–273. doi: 10.1016/S0020-1383(02)00312-1. [DOI] [PubMed] [Google Scholar]
- 19.Gottschalk HP, Sagoo D, Glaser D, Doan J, Edmonds EW, Schlechter J. Biomechanical analysis of pin placement for pediatric supracondylar humerus fractures: does starting point, pin size, and number matter? J Pediatr Orthop. 2012;32:445–451. doi: 10.1097/BPO.0b013e318257d1cd. [DOI] [PubMed] [Google Scholar]
- 20.Green DW, Widmann RF, Frank JS, Gardner MJ. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Orthop Trauma. 2005;19:158–163. doi: 10.1097/00005131-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop. 2004;24:245–248. doi: 10.1097/01241398-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Han QL, Wang YH, Liu F. Comparison of complications and results of early versus delayed surgery for Gartland type III supracondylar humeral fractures in pediatric patients. Orthop Surg. 2011;3:242–246. doi: 10.1111/j.1757-7861.2011.00153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasler CC. Supracondylar fractures of the humerus in children. Eur J Trauma. 2001;27:1–15. [Google Scholar]
- 24.Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23:1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kallio PE, Foster BK, Paterson DC. Difficult supracondylar elbow fractures in children: analysis of percutaneous pinning technique. J Pediatr Orthop. 1992;12:11–15. [PubMed] [Google Scholar]
- 27.Kim WY, Chandru R, Bonshahi A, Paton RW. Displaced supracondylar humeral fractures in children: results of a national survey of paediatric orthopaedic consultants. Injury. 2003;34:274–277. doi: 10.1016/S0020-1383(02)00321-2. [DOI] [PubMed] [Google Scholar]
- 28.Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, Hedequist D, Karlin L, Kim YJ, Murray MM, Millis MB, Emans JB, Dichtel L, Matheney T, Lee BM. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children: a randomized clinical trial. J Bone Joint Surg Am. 2007;89:706–712. doi: 10.2106/JBJS.F.00379. [DOI] [PubMed] [Google Scholar]
- 29.Lee KM, Chung CY, Gwon DK, Sung KH, Kim TW, Choi IH, Cho TJ, Yoo WJ, Park MS. Medial and lateral crossed pinning versus lateral pinning for supracondylar fractures of the humerus in children: decision analysis. J Pediatr Orthop. 2012;32:131–138. doi: 10.1097/BPO.0b013e3182471931. [DOI] [PubMed] [Google Scholar]
- 30.Lee S, Park MS, Chung CY, Kwon DG, Sung KH, Kim TW, Choi IH, Cho TJ, Yoo WJ, Lee KM. Consensus and different perspectives on treatment of supracondylar fractures of the humerus in children. Clin Orthop Surg. 2012;4:91–97. doi: 10.4055/cios.2012.4.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22:440–443. [PubMed] [Google Scholar]
- 32.Li YA, Lee PC, Chia WT, Lin HJ, Chiu FY, Chen TH, Feng CK. Prospective analysis of a new minimally invasive technique for paediatric Gartland type III supracondylar fracture of the humerus. Injury. 2009;40:1302–1307. doi: 10.1016/j.injury.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 33.Loizou CL, Simillis C, Hutchinson JR. A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury. 2009;40:245–248. doi: 10.1016/j.injury.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 34.Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop. 1998;18:43–45. [PubMed] [Google Scholar]
- 35.Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. 2012;7:6. doi: 10.1186/1749-799X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCarthy SM, Ogden JA. Radiology of postnatal skeletal development: V. Distal humerus. Skeletal Radiol. 1982;7:239–249. doi: 10.1007/BF00361979. [DOI] [PubMed] [Google Scholar]
- 37.Mostafavi HR, Spero C. Crossed pin fixation of displaced supracondylar humerus fractures in children. Clin Orthop Relat Res. 2000;376:56–61. doi: 10.1097/00003086-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop. 2012;32(suppl 2):S143–S152. doi: 10.1097/BPO.0b013e318255b17b. [DOI] [PubMed] [Google Scholar]
- 39.Nacht JL, Ecker ML, Chung SM, Lotke PA, Das M. Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop Relat Res. 1983;177:203–209. [PubMed] [Google Scholar]
- 40.Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121–1132. doi: 10.2106/JBJS.G.01354. [DOI] [PubMed] [Google Scholar]
- 41.Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Paradis G, Lavallee P, Gagnon N, Lemire L. Supracondylar fractures of the humerus in children: technique and results of crossed percutaneous K-wire fixation. Clin Orthop Relat Res. 1993;297:231–237. [PubMed] [Google Scholar]
- 43.Rasool MN. Ulnar nerve injury after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1998;18:686–690. doi: 10.1097/00004694-199809000-00027. [DOI] [PubMed] [Google Scholar]
- 44.Reising K, Schmal H, Kohr M, Kuminack K, Sudkamp NP, Strohm PC. Surgical treatment of supracondylar humerus fractures in children. Acta Chir Orthop Traumatol Cech. 2011;78:519–523. [PubMed] [Google Scholar]
- 45.Reynolds RA, Jackson H. Concept of treatment in supracondylar humeral fractures. Injury. 2005;36(suppl 1):A51–A56. doi: 10.1016/j.injury.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 46.Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am. 2007;89:713–717. doi: 10.2106/JBJS.F.00076. [DOI] [PubMed] [Google Scholar]
- 47.Sibinski M, Sharma H, Bennet GC. Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg Br. 2006;88:380–381. doi: 10.2106/JBJS.C.01518. [DOI] [PubMed] [Google Scholar]
- 48.Sibinski M, Sharma H, Sherlock DA. Lateral versus crossed wire fixation for displaced extension supracondylar humeral fractures in children. Injury. 2006;37:961–965. doi: 10.1016/j.injury.2006.02.054. [DOI] [PubMed] [Google Scholar]
- 49.Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86:702–707. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 50.Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children: the consequences of pin placement. J Bone Joint Surg Am. 2001;83:735–740. [PubMed] [Google Scholar]
- 51.Skaggs DL, Kay RM, Tolo VT. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J Pediatr Orthop. 2002;22:697; author reply 697–698. [DOI] [PubMed]
- 52.Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop. 2010;30:430–436. doi: 10.1097/BPO.0b013e3181e00c0d. [DOI] [PubMed] [Google Scholar]
- 53.Topping RE, Blanco JS, Davis TJ. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J Pediatr Orthop. 1995;15:435–439. doi: 10.1097/01241398-199507000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Tripuraneni KR, Bosch PP, Schwend RM, Yaste JJ. Prospective, surgeon-randomized evaluation of crossed pins versus lateral pins for unstable supracondylar humerus fractures in children. J Pediatr Orthop B. 2009;18:93–98. doi: 10.1097/BPB.0b013e32832989ff. [DOI] [PubMed] [Google Scholar]
- 55.Vaidya SM. Percutaneous fixation of displaced supracondylar fracture in children comparing lateral with medial and lateral pin. A thesis submitted to university of Seychelles American institute of medicine. 2009. Available at: http://www.mch-orth.com/pdf/Thesis%20by%20Dr.Sudeep%20Vaidya.pdf. Accessed April 17, 2013.
- 56.Wang X, Feng C, Wan S, Bian Z, Zhang J, Song M, Shao J, Yang X. Biomechanical analysis of pinning configurations for a supracondylar humerus fracture with coronal medial obliquity. J Pediatr Orthop B. 2012;21:495–498. doi: 10.1097/BPB.0b013e328355d01f. [DOI] [PubMed] [Google Scholar]
- 57.Woratanarat P, Angsanuntsukh C, Rattanasiri S, Attia J, Woratanarat T, Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26:48–53. [DOI] [PubMed]
- 58.Yen YM, Kocher MS. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children: surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):20–30. doi: 10.2106/JBJS.G.01337. [DOI] [PubMed] [Google Scholar]
- 59.Zamzam MM, Bakarman KA. Treatment of displaced supracondylar humeral fractures among children: crossed versus lateral pinning. Injury. 2009;40:625–630. doi: 10.1016/j.injury.2008.10.029. [DOI] [PubMed] [Google Scholar]
- 60.Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76:253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]


