Abstract
Background
A future increase in total joint arthroplasties in patients with diabetes seems likely considering the prevalence of osteoarthritis and diabetes mellitus are increasing. However, the rates of arthroplasty in the population of patients with diabetes are unclear.
Questions/purposes
We sought to determine whether lower extremity arthroplasties in a veteran population with diabetes is different from a similar population without diabetes. The following specific questions were asked: (1) Is the rate of TKA in veterans with diabetes higher than in those without diabetes? (2) Is the rate of THA in veterans with diabetes higher than in those without diabetes? (3) Are arthroplasty revision rates greater in veterans with diabetes than in veterans without diabetes?
Methods
The US Department of Veterans Affairs Health administrative data from fiscal year 2000 was used to identify persons with primary or secondary TKA or THA. The rate of surgeries among a diabetic population was compared with that among a nondiabetic population.
Results
The diabetic cohort received total joint arthroplasties at a higher rate than the nondiabetic cohort at all ages younger than 66 years, with a range of odd ratios from 1.3 to 3.4. In answer to our specific questions, (1) the rate of TKA (95% CI, 2.1–3.7), (2) the rate of THA (95% CI, 1.0–2.6), and (3) the rates of arthroplasty revision (95% CI, 0.9–5.8 TKA and 0.7–6.8 THA) were higher in veterans with diabetes. Furthermore, those with diabetes in the youngest age group studied received total joint arthroplasties and revision surgeries at approximately double the rates of those without diabetes.
Conclusions
If these findings hold true for the population as a whole, they imply that clinicians in the United States may see a sharp increase in younger diabetic candidates for joint arthroplasty.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Joint arthroplasty is a common treatment for end-stage joint disease to restore mobility and reduce pain. Diabetes contributes to poor orthopaedic surgical outcomes including increased pain and stiffness, decreased joint function, decreased ROM, nonhomebound discharge status, and reduction of implant survivorship requiring subsequent revision surgery [3, 4, 9, 24, 28]. A patient’s glycemic control has additional effects on surgical outcome. Patients with uncontrolled diabetes undergoing arthroplasty are reported to have higher postsurgical complications and costs compared with patients with controlled diabetes undergoing arthroplasty [23].
Because national trends indicate that the prevalence of diabetes mellitus is increasing rapidly [25], the number of patients with diabetes and with osteoarthritis seeking an arthroplasty also can be expected to increase. However, whether this comorbid condition contributes to an increase in the number of arthroplasties performed is unknown. A recent study indicated that obesity, another comorbid condition that is increasing in prevalence in the United States, cannot be the only cause of increased rates of TKA [21].
To obtain a better estimation of the rates of lower extremity total joint arthroplasties among patients with diabetes nationwide, an observational retrospective study was performed using the US Department of Veterans Affairs Health Administration (VHA) administrative data. The following questions were asked: (1) Is the rate of TKA in veterans with diabetes higher than in those without diabetes? (2) Is the rate of THA in veterans with diabetes higher than in those without diabetes? (3) Are arthroplasty revision rates greater in veterans with diabetes than in veterans without diabetes?
Patients and Methods
The study design was observational and retrospective, in compliance with the Helsinki Declaration, and conducted with the approval of the Colorado Multiple Institutional Review Board and the VHA Research Committee. All data were examined without protected health information. The review boards determined this protocol qualified for exempt status.
Because the goal was to identify the rates of operations in a large population with a broad age range, data were obtained from the VHA administrative database (Austin Center, TX, USA). Persons who had at least one visit at any VHA medical center during the VA fiscal year 2000 (October 1999 to September 2000) were counted once in the study. The criterion to identify VHA patients with diabetes was either (1) prescribed antidiabetic medication or (2) a record of two outpatient visits and/or inpatient stays within 24 months of diagnosis for diabetes. This criterion was defined as the best (ie, high sensitivity and high specificity) for identifying patients with diabetes [25]. Data for TKAs and THAs for primary and revision operations in these two cohorts were obtained using the following International Classification of Diseases, 9th Revision, Clinical Modification codes: 81.54 (primary TKA), 81.55 (revision TKA), 81.51 (primary THA), and 81.53 (revision THA).
To address the concern that patients with diabetes may be more frequent users of outpatient care, rates for arthroplasties in the VHA were determined using a denominator for patients with diabetes and patients without diabetes based on the total numbers of veterans with at least one visit during that fiscal year. Any record in the outpatient file (eg, a physician visit or having laboratory work or blood drawn) qualified to count the patient in the respective denominator.
For all analyses, both cohorts were stratified by age into three groups: 46 to 55 years, 56 to 65 years, and older than 65 years. The numbers of patients in each age group of the diabetic cohort were: 46 to 55 years, 34,949; 56 to 65 years, 70,156; and 66 years and older, 342,933. The numbers of patients in each age group of the nondiabetic cohort were: 46 to 55 years, 800,660; 56 to 65 years, 603,918; and 66+ years, 1,614,757.
The chi-square test was performed to analyze the association between arthroplasty and diabetes status. Odd ratios and 95% CIs were calculated to quantify risk for surgery according to diabetes status [2]. Surgical types (primary TKA, revision TKA, primary THA, and revision THA) were tested individually. Statistical significance was set at a probability less than 0.05.
Results
In the hip and the knee, the frequency of arthroplasty among patients in the VHA in fiscal year 2000 was higher in the diabetic cohort.
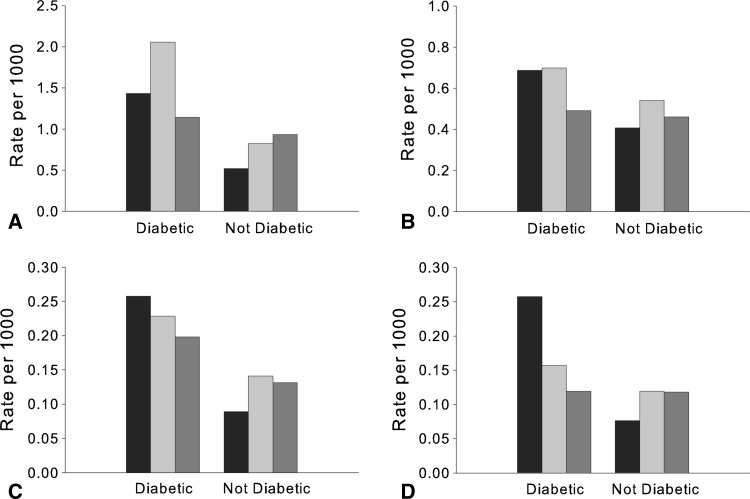
Regarding whether the rate of having a TKA is greater with diabetes, the data showed a significant increase in primary TKAs for all three age groups tested: 46 to 55, 56 to 65, and 66+ years. The proportion of the diabetes cohort receiving primary TKAs resulted in a calculated increased risk for TKA from a low of 1.2 for patients 66+ years to a high of 2.8 for patients 46 to 55 years (Table 1). An unexpected finding was that although arthroplasty rates increased with age in the nondiabetic groups, the rates for the diabetic groups were highest in the younger age groups. The highest rate of operations was for primary TKA in a younger diabetic group—more than two per 1000 for patients 56 to 65 years (Fig. 1A).
Table 1.
Rates of primary and revision TKAs
| Age group (years) |
Rates of diabetic cohort having surgery | Rates of nondiabetic cohort having surgery | Odds ratio | 95% CI of odds ratio | p value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary TKA | Revision TKA | Primary TKA | Revision TKA | Primary TKA | Revision TKA | Primary TKA | Revision TKA | Primary TKA | Revision TKA | |
| 46–55 | 0.14 | 0.03 | 0.05 | 0.01 | 2.8 | 2.9 | 2.1–3.7 | 1.5–5.8 | < 0.0001 | 0.004 |
| 56–65 | 0.21 | 0.02 | 0.08 | 0.01 | 2.5 | 1.6 | 2.1–3.0 | 0.9–2.8 | < 0.0001 | NS |
| 66+ | 0.11 | 0.02 | 0.09 | 0.01 | 1.2 | 1.5 | 1.1–1.4 | 1.1–1.2 | 0.0004 | 0.0037 |
Total number of patients in the diabetic cohort age groups were 34,949 (46–55 years), 70,156 (56–65 years), and 342,933 (66+ years); total number of patients in the nondiabetic cohorts were 800,660 (46–55 years), 603,918 (56–65 years), and 1,614,757 (66+ years); NS = not significant (p > 0.05).
Fig. 1A–D.
The bar graphs illustrate the rates of surgeries in a cohort with diabetes compared with a cohort without diabetes during the VA’s fiscal year 2000. Rates per 1000 patients for (A) primary TKA, (B) primary THA (C) revision knee arthroplasty, and (D) revision hip arthroplasty by cohort and by age group are shown.  = patients 46–55 years old;
= patients 46–55 years old;  = patients 56–65 years old;
= patients 56–65 years old;  = patients 66+ years old.
= patients 66+ years old.
Regarding whether the rate of having a THA is greater with diabetes, the data showed a significant increase in primary THAs for patients 46 to 55 years old (Table 2). No significant differences in the frequencies of primary THAs between cohorts were detected in the 56 to 65 and the 66+ year age groups. Although arthroplasty rates increased with age in the nondiabetic groups, the rates for the diabetic groups were highest in the younger age groups (Fig. 1B).
Table 2.
Rates of primary and revision THAs
| Age group (years) | Rates of diabetic cohort having surgery | Rates of nondiabetic cohort having surgery | Odds ratio | 95% CI of odds ratio | p value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary THA | Revision THA | Primary THA | Revision THA | Primary THA | Revision THA | Primary THA | Revision THA | Primary THA | Revision THA | |
| 46–55 | 0.07 | 0.03 | 0.04 | 0.01 | 1.7 | 3.4 | 1.1–2.6 | 1.7–6.8 | 0.0173 | 0.0009 |
| 56–65 | 0.07 | 0.02 | 0.05 | 0.01 | 1.3 | 1.3 | 1.0–1.7 | 0.7–2.5 | NS | NS |
| 66+ | 0.05 | 0.01 | 0.05 | 0.01 | 1.1 | 1.0 | 0.9–1.3 | 0.7–1.4 | NS | NS |
Total number of patients in the diabetic cohort age groups were 34,949 (46–55 years), 70,156 (56–65 years), and 342,933 (66+ years); total number of patients in the nondiabetic cohorts were 800,660 (46–55 years), 603,918 (56–65 years), and 1,614,757 (66+ years); = not significant (p > 0.05).
Regarding whether arthroplasty revision rates are greater in patients with diabetes, the data showed significant increases in revision TKA for patients 46 to 55 years old and 66+ years (Table 1), and for revision THA for patients 46 to 55 years old (Table 2). Odds ratios for these specific revisions were 2.9, 1.5, and 3.4, respectively. In the diabetic cohort, higher rates were found in the younger groups (Fig. 1C–D).
Discussion
Using a diabetic and an analogous nondiabetic cohort of VHA patients, we found that the cohort with diabetes has higher rates of arthroplasty and that these arthroplasties are being performed at a younger age than in the nondiabetic cohort. This finding contrasts with diabetic risks for other medical complications (eg, heart disease and stroke, hypertension, nervous system damage, and severe periodontitis), which typically are found to increase with age [7]. Others have reported on the higher risk for perisurgical and postsurgical complications associated with diabetes mellitus [3, 9, 16, 23, 33]. However, to our knowledge, our study is the first to report specifically the rates of primary and revision knee and hip arthroplasties in a diabetic population.
A limitation of these data is that the percentages of Type 1 versus Type 2 diabetes in each cohort are unavailable. The prevalence of diabetes in the VHA population had been 19.6% during the year relevant to this study [25]. No data are available specifying prevalence or incidence between Types 1 and 2 diabetes in veterans. However, in active duty US military, the incidence rate of Type 1 diabetes in 2000 was only 3.7 per 100,000 (fewer than 6% of all diabetes diagnoses) [12]. As our study includes only the VHA population, it may differ from the general population for various reasons. For example, the data available from this study point to higher rates and risk of primary TKAs in the population using the VA healthcare system, in which the incidence of diabetes is increasing approximately 2% each year [25] and could signal greater effects in coming years. The VHA patient population is predominantly male compared with the general US population. In addition, the VHA patient population is underrepresented in Hispanics, Native Americans, and Asian/Pacific Islanders [34], groups reported to have a higher prevalence of diagnosed diabetes [7]. Thus, the findings of our study may underestimate prevalence in the general US population. Another limitation is the absence of data for the prevalence of early arthritis not requiring arthroplasty. However, the Centers for Disease Control and Prevention does report the prevalence of arthritis in the United States and territories is higher for adults with diabetes, 52% compared with 29% for those without diabetes [5]. Our study does not include persons with undiagnosed diabetes or persons not healthy enough for surgery who might otherwise opt for arthroplasty. Thus, the potential full effect of diabetes on articular joints may be greater than illustrated in our study. In addition, the revision rates are overall population rates and do not represent the actual number of people who have had primary arthroplasties as that is not possible to determine from our data set. Therefore our data cannot be used to project the precise number of patients who may require revision surgery in the future. Finally, additional data on other comorbidities were not collected from these cohorts. Potential confounding effects may arise from conditions known to be associated with diabetes such as obesity, chronic kidney disease, and heart disease.
We are unable to identify potential biological mechanisms for increased arthroplasty in patients at younger ages with diabetes from the data collected. Candidate mechanisms include hyperglycemia leading to joint tissue changes, particularly in collagen [27], and obesity leading to (1) increased mechanical load to the joint [31]; and/or (2) nonbiomechanical factors such as metabolism from increased fat [8, 14, 20, 22]. Obesity is a risk factor for diabetes [1, 15, 17, 19, 30] and osteoarthritis [8, 13, 20, 22, 26], and both factors are increasing rapidly in the US population [6, 10]. Unfortunately, data that might further explore these potential hypotheses are unavailable in our data set (BMI, HbA1c, adipokine biomarkers). The finding that arthroplasty rate increases with diabetes is consistent with a study of a much smaller population (arthroplasty performed at one hospital with only 69 subjects in the diabetes group) in which increased risk for primary arthroplasty was the result of diabetes and independent of age and BMI [32]. However, differences between joints could not be assessed because data were combined for the knee and hip [32].
With primary hip arthroplasty, the increase in diabetes was not as dramatic as with the knee and was detected only in the youngest age group. Whether this is related to fewer primary hip than knee surgeries in the general population [18] or to a biological mechanism related to diabetes cannot be determined by our study.
For revision arthroplasty, there were greater rates in our diabetic cohort in the youngest (knee and hip) and oldest (knee) age groups. The multicenter NAKAR study found that worse outcomes for revision TKA, as measured by the SF-36, WOMAC, and Lower-Extremity Activity Scale (LEAS) instruments, were associated with a higher number of comorbidities which included diabetes [11]. A recent study examining hip revisions also found an increased risk for revision with diabetes [29]. Two studies of TKAs showed rates of implant nonsurvivorship were higher in the short-term but not significantly higher in the long-term (> 7 years) [24, 28]. Higher arthroplasty rates add to increasing healthcare costs. A total joint arthroplasty is an expensive procedure with costs ranging from USD 20,000 to USD 35,000; and revision arthroplasty at more than USD 47,000 [3, 4]. However, when these procedures are performed on patients with diabetes, costs increase USD 1000 per hospital admission, likely owing to greater nursing care, monitoring and testing, and glucose management [3]. Furthermore, patients with diabetes undergoing an arthroplasty are more often than the general population to be discharged to another care facility rather than their home [3, 16].
That arthroplasty rates are higher in patients with diabetes and more weighted toward younger patients could have important clinical implications such as a potential increase in revision surgeries in subsequent years. We found that patients younger than 66 years with diabetes in the VHA receive total joint arthroplasties at a higher rate than those without diabetes. Furthermore, patients with diabetes in the youngest age group studied (46–55 years) are receiving arthroplasties at approximately double the rate of patients without diabetes. Although the mechanisms for this doubling are not entirely clear, if these findings hold true for the population at large, clinicians will see a sharp increase in younger diabetic candidates for joint arthroplasties. Therefore it would be important to elucidate the underlying mechanisms related to diabetes that cause revisions and, more importantly, to reduce the number of primary surgeries for patients with diabetes.
Acknowledgments
We thank Miriam Maney MA for helpful discussions regarding this study.
Footnotes
One of the authors certifies that she (KBK) received salary support (less than USD 10,000) for this study in part by a Pilot and Feasibility Grant from the University of Colorado Denver Diabetes and Endocrinology Research Center (NIDDK P30DK57516). All authors of this study are employed by the Department of Veterans Affairs. One of the authors (KBK) has received funding from Cerapedics, Inc, (Lakewood, CO, USA) for unrelated scientific consulting work (less than USD 10,000).
The contents of this paper do not represent the views of the Department of Veterans Affairs or the United States Government.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Colorado School of Medicine, Aurora, CO, USA; the VA Eastern Colorado Health Care System, Denver, CO, USA; and the VA Medical Center East Orange, NJ, USA.
References
- 1.Abdullah A, Stoelwinder J, Shortreed S, Wolfe R, Stevenson C, Walls H, de Courten M, Peeters A. The duration of obesity and the risk of type 2 diabetes. Public Health Nutr. 2011;14:119–126. doi: 10.1017/S1368980010001813. [DOI] [PubMed] [Google Scholar]
- 2.Bland JM, Altman DG. Statistics notes: the odds ratio. BMJ. 2000;320:1468. doi: 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolognesi MP, Marchant MH, Jr, Viens NA, Cook C, Pietrobon R, Vail TP. The impact of diabetes on perioperative patient outcomes after total hip and total knee arthroplasty in the United States. J Arthroplasty. 2008;23(6 suppl 1):92–98. doi: 10.1016/j.arth.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:570–576. doi: 10.2106/JBJS.D.02121. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Arthritis as a potential barrier to physical activity among adults with diabetes—United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep. 2008;57:486–489. [PubMed]
- 6.Centers for Disease Control and Prevention (CDC). Estimated county-level prevalence of diabetes and obesity—United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:1259–1263. [PubMed]
- 7.Centers for Disease Control and Prevention (CDC). National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. Available at: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed October 15, 2012
- 8.Dahaghin S, Bierma-Zeinstra SM, Koes BW, Hazes JM, Pols HA. Do metabolic factors add to the effect of overweight on hand osteoarthritis? The Rotterdam study. Ann Rheum Dis. 2007;66:916–920. doi: 10.1136/ard.2005.045724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher DA, Dierckman B, Watts MR, Davis K. Looks good but feels bad: factors that contribute to poor results after total knee arthroplasty. J Arthroplasty. 2007;22(6 suppl 2):39–42. doi: 10.1016/j.arth.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 11.Ghomrawi HM, Kane RL, Eberly LE, Bershadsky B, Saleh KJ, North American Knee Arthroplasty Revision (NAKAR) Study Group Patterns of functional improvement after revision knee arthroplasty. J Bone Joint Surg Am. 2009;91:2838–2845. doi: 10.2106/JBJS.H.00782. [DOI] [PubMed] [Google Scholar]
- 12.Greenburg D, Haverkos HW, Vigersky R. Diabetes mellitus, active component, U.S. Armed forces, 1997–2007. Medical Surveillance Monthly Reports. 2009;16:7–9. Available at: http://www.afhsc.mil/viewMSMR?file=2009/v16_n02.pdf#Page=07. Accessed April 17, 2013.
- 13.Griffin TM, Guilak F. Why is obesity associated with osteoarthritis? Insights from mouse models of obesity. Biorheology. 2008;45:387–398. [PMC free article] [PubMed] [Google Scholar]
- 14.Hart DJ, Doyle DV, Spector TD. Association between metabolic factors and knee osteoarthritis in women: the Chingford study. J Rheumatol. 1995;22:1118–1123. [PubMed] [Google Scholar]
- 15.Hu G, Lindstrom J, Valle TT, Eriksson JG, Jousilahti P, Silventoinen K, Qiao Q, Tuomilehto J. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch Intern Med. 2004;164:892–896. doi: 10.1001/archinte.164.8.892. [DOI] [PubMed] [Google Scholar]
- 16.Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005;435:232–238. doi: 10.1097/01.blo.0000156479.97488.a2. [DOI] [PubMed] [Google Scholar]
- 17.Kodama S, Horikawa C, Fujihara K, Heianza Y, Hirasawa R, Yachi Y, Sugawara A, Tanaka S, Shimano H, Iida KT, Saito K, Sone H. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: a meta-analysis. Am J Epidemiol. 2012;176:959–969. doi: 10.1093/aje/kws172. [DOI] [PubMed] [Google Scholar]
- 18.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 19.Li S, Zhao JH, Luan J, Langenberg C, Luben RN, Khaw KT, Wareham NJ, Loos RJ. Genetic predisposition to obesity leads to increased risk of type 2 diabetes. Diabetologia. 2011;54:776–782. doi: 10.1007/s00125-011-2044-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engström G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Ann Rheum Dis. 2009;68:490–496. doi: 10.1136/ard.2008.089748. [DOI] [PubMed] [Google Scholar]
- 21.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lübbeke A, Duc S, Garavaglia G, Finckh A, Hoffmeyer P. BMI and severity of clinical and radiographic signs of hip osteoarthritis. Obesity (Silver Spring). 2009;17:1414–1419. doi: 10.1038/oby.2008.663. [DOI] [PubMed] [Google Scholar]
- 23.Marchant MH, Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009;91:1621–1629. doi: 10.2106/JBJS.H.00116. [DOI] [PubMed] [Google Scholar]
- 24.Meding JB, Reddleman K, Keating ME, Klay A, Ritter MA, Faris PM, Berend ME. Total knee replacement in patients with diabetes mellitus. Clin Orthop Relat Res. 2003;416:208–216. doi: 10.1097/01.blo.0000093002.90435.56. [DOI] [PubMed] [Google Scholar]
- 25.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10–B21. doi: 10.2337/diacare.27.suppl_2.B10. [DOI] [PubMed] [Google Scholar]
- 26.Mooney RA, Sampson ER, Lerea J, Rosier RN, Zuscik MJ. High-fat diet accelerates progression of osteoarthritis after meniscal/ligamentous injury. Arthritis Res Ther. 2011;13:R198. doi: 10.1186/ar3529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oren TW, Botolin S, Williams A, Bucknell A, King KB. Arthroplasty in veterans: analysis of cartilage, bone, serum, and synovial fluid reveals differences and similarities in osteoarthritis with and without comorbid diabetes. J Rehabil Res Dev. 2011;48:1195–1210. doi: 10.1682/JRRD.2010.09.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papagelopoulos PJ, Idusuyi OB, Wallrichs SL, Morrey BF. Long term outcome and survivorship analysis of primary total knee arthroplasty in patients with diabetes mellitus. Clin Orthop Relat Res. 1996;330:124–132. doi: 10.1097/00003086-199609000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Pedersen AB, Mehnert F, Johnsen SP, Sorensen HT. Risk of revision of a total hip replacement in patients with diabetes mellitus: a population-based follow up study. J Bone Joint Surg Br. 2010;92:929–934. doi: 10.2106/JBJS.I.00882. [DOI] [PubMed] [Google Scholar]
- 30.Perry IJ, Wannamethee SG, Walker MK, Thomson AG, Whincup PH, Shaper AG. Prospective study of risk factors for development of non-insulin dependent diabetes in middle aged British men. BMJ. 1995;310:560–564. doi: 10.1136/bmj.310.6979.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Recnik G, Kralj-Iglic V, Iglic A, Antolic V, Kramberger S, Rigler I, Pompe B, Vengust R. The role of obesity, biomechanical constitution of the pelvis and contact joint stress in progression of hip osteoarthritis. Osteoarthritis Cartilage. 2009;17:879–882. doi: 10.1016/j.joca.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Schett G, Kleyer A, Perricone C, Sahinbegovic E, Iagnocco A, Zwerina J, Lorenzini R, Aschenbrenner F, Berenbaum F, D’Agostino MA, Willeit J, Kiechl S. Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohort study. Diabetes Care. 2013;36:403–409. doi: 10.2337/dc12-0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.SooHoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371. doi: 10.1007/s11999-010-1354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Veterans Affairs. 2001 National Survey of Veterans. Final Report. Available at: http:www.va.gov/VETDATA/docs/SurveysAndStudies/NSV_Final_Report.doc. Accessed October 15, 2012.