Abstract
Background
In a previous study, we described two subtypes of high dislocation of the hip depending on the presence (C1) or absence (C2) of a false acetabulum, yet we have already presented the concise followup of total hip arthroplasty (THA) in these patients as a group at a minimum of 15 years.
Questions/purposes
In this retrospective study, we investigated differences in the results of THA in the C1 and C2 subtypes of high dislocation such as (1) survivorship of the reconstructions; (2) Merle d’Aubigné-Postel clinical scores; (3) leg lengthening and femoral shortening; and (4) site of reattachment and union rate of the greater trochanter.
Methods
We included 49 hips of the C1 subtype and 30 hips of the C2 subtype operated on from 1976 to 1994. We evaluated survivorship (using reoperation for any reason as the end point) and performed chart and radiographic reviews.
Results
The 15-year survival was 84% (± 10% [95% CI]) for the C1 subtype and 60% (± 17% [95% CI]) for the C2 subtype (p = 0.001). Cox regression analysis, after adjustment for confounding factors, showed also statistically significantly worse survivorship in the C2 subtype (p = 0.021) and, after adjustment for possible predictive factors, found a statistically significant relationship of high dislocation subtype (p = 0.018) and trochanteric union (p = 0.005) with survival of THAs. Pain, function, and mobility scores improved from preoperative to last followup in C1 and C2 groups but they did not differ between C1 and C2 hips. C2 hips were lengthened more (p < 0.001) despite greater amounts of femoral shortening (p = 0.006). Site of reattachment and the risk of greater trochanter nonunion were not different between the groups.
Conclusions
We found important differences in fundamental parameters after THA in the high-dislocation subtypes, including the risk of revision, which was higher in patients whose hips did not have a false acetabulum. These findings indicate that while reporting THA results in patients with high dislocation, mixing results of the two subtypes may lead to statistical bias.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
We have recognized two subtypes of high dislocation of the hip on the basis of the presence (C1 hips) or absence of a false acetabulum (C2 hips) [10]. Xu et al. [21] found that the presence or absence of false acetabulum in high dislocated hips is associated with different loading patterns and that this could influence the development and shape of the proximal femur.
We have previously reported, in a concise followup study, a group of 67 female patients with high dislocation (84 hips) who underwent total hip arthroplasty (THA) comparing cemented with hybrid and cementless reconstructions, without separating C1 and C2 hips [8]. However, we are concerned that there may be differences in the long-term clinical and radiographic results of THA between the two subtypes of high hip dislocation. If there were such differences, then mixing results of the C1 and C2 subtypes could lead to statistical bias.
In this report, we sought to compare (1) survivorship of the reconstructions; (2) Merle d’Aubigné-Postel clinical scores; (3) leg lengthening and femoral shortening; and (4) site of reattachment and union rate of the greater trochanter between patients having THA for C1 and C2 high hip dislocations.
Patients and Methods
This study was approved by the institutional board of our hospital. In our previous studies, we have reported the clinical and radiographic results in a series of 84 THAs performed during the period 1976 to 1994 by a single surgeon (GH) in 67 female patients with high dislocation of both subtypes (C1: Fig. 1; C2: Fig. 2) [8, 9].
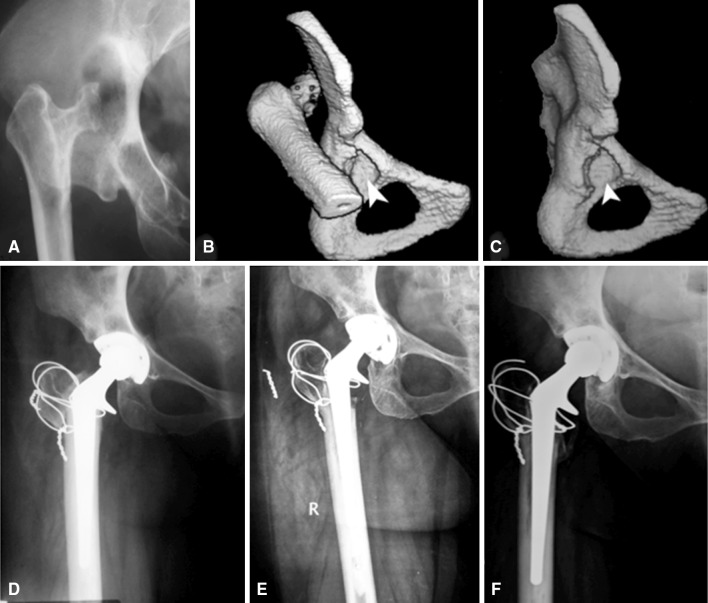
Fig. 1A–E.
Images illustrate the case of a patient with a C1 subtype high dislocation. (A) A preoperative radiograph shows the height of the dislocation was 4 cm. (B–C) Three-dimensional CT shows the hip (B) with and (C) without the femoral head (the stars depict the false and arrowhead the true acetabulum). (D) A postoperative radiograph taken after a hybrid-type THA shows the femur was shortened 3 cm, whereas the limb was lengthened 1 cm. (E) Twenty years after surgery, the patient remains free of symptoms.
Fig. 2A–F.
Images illustrate the case of a patient with a C2 subtype high dislocation. (A) A preoperative radiograph shows the height of the dislocation was 7 cm. Three-dimensional CT shows the hip (B) with and (C) without the femoral head. (D) A postoperative radiograph taken after a hybrid-type THA shows the femur was shortened 1 cm, whereas the limb was lengthened 6 cm. (E) Fourteen years after surgery, exchange of the liner only was required as a result of progressive wear. (F) Five years after liner exchange and 19 years after the original operation, the patient is free of symptoms.
For the purpose of this study, we excluded three patients (three hips) as a result of postoperative infection and two patients (two hips) who died 6 and 7 years after the operation, before completion of the minimum followup of 15 years. Therefore, 79 hips in 62 patients, 49 of the C1 subtype and 30 of the C2 subtype, remained for evaluation. The minimum followup for patients that retained the original implants was 15 years (mean, 21 years; range, 15–33 years).
Eight patients had bilateral high dislocation of the C1 subtype (one of them operated on only one hip) and six had bilateral high dislocation of the C2 subtype. Four more patients had high dislocation of the C1 subtype in one hip and of the C2 subtype in the contralateral hip. The diagnosis of the opposite hip in 44 unilateral hips is shown (Table 1).
Table 1.
Diagnosis of the opposite hip in patients with a high-dislocated hip
| Type of high dislocation | Number of hips | ||
|---|---|---|---|
| Low dislocation | Dysplasia | Normal | |
| C1 (n = 30) | 4 | 12 | 14 |
| C2 (n = 14) | 7 | 4 | 3 |
The mean patient age was 49 years (range, 23–73 years) for the C1 subtype and 48 years (range, 23–68 years) for the C2 subtype. The height of the dislocation was measured on the preoperative AP radiograph according to the method of Crowe et al. [5] as the vertical distance between the teardrop and the head-neck junction. The average height was 4.8 cm (range, 3–9 cm) in the C1 subtype and 6.9 cm (range, 2–10 cm) in the C2 subtype. The Charnley low-friction technique [4] was used in 39 hips of the C1 subtype and 21 hips of the C2 subtype. The hybrid technique (insertion of the acetabular component without cement and of the femoral component with cement) was used in nine hips of the C1 subtype and nine hips of the C2 subtype. One arthroplasty in a C1 hip was performed with cementless acetabular and femoral components. All operations were performed after osteotomy of the greater trochanter, proximal femoral shortening at the level of the femoral neck (Fig. 3) and placing the acetabular component at the level of true acetabulum [7].
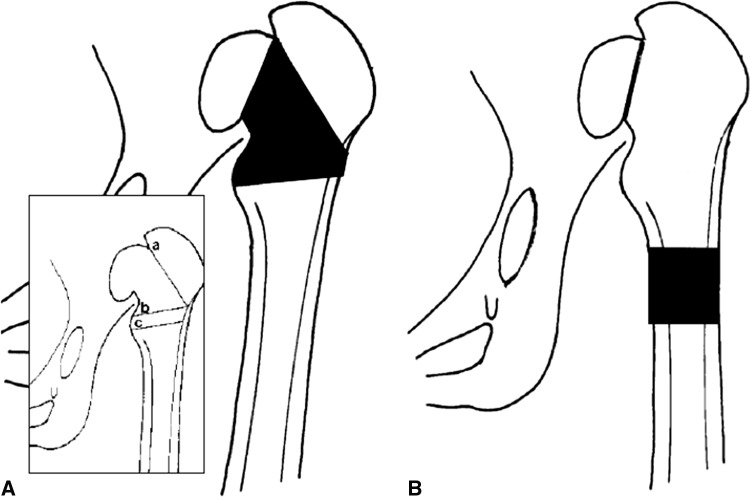
Fig. 3A–B.
Diagrams illustrate the alternatives of femoral shortening: (A) shortening by segmental dissection of bone at the level of femoral neck and (B) shortening by resection of bone from the femoral diaphysis.
We used the Merle d’Aubigné-Postel scoring system for pain, function, and motion, as modified by Charnley [4], for clinical rating. Survival analyses were performed according to the Kaplan-Meier method [12] with revision for any reason as the end point.
Furthermore, the following parameters were investigated: (1) leg lengthening (leg length was measured as the distance between the superior iliac spine and the lower end of medial malleolus in a patient lying on a supine position) and presence of Trendelenburg sign; (2) placement (height) of the cup in relation to the teardrop; (3) extent of femoral shortening needed during the operation, estimated by subtraction of leg lengthening from the height of the dislocation and by adding or subtracting the height of the cup placement, because in all hips special CDH stems with short necks (Charnley CDH stems, C.F. Thucrey, Leeds, UK; Harris CDH stems, Zimmer, Warsaw, IN, USA; and Opti-Fix, Smith and Nephew, Richards Inc, Memphis, TN, USA) were used; and (4) position of reattachment and rate of union of the osteotomized greater trochanter. We recognized four categories of trochanteric reattachment relative to its original bed: (1) at the original bed; (2) distal, the trochanter having contact with the distal part of the original bed; (3) at the lateral femoral cortex; and (4) proximal to the original bed [7]. The trochanter was considered radiographically healed based on trabecular continuity between the trochanteric fragment and the femur. Fibrous union was defined as a persistent radiolucent gap of less than 15 mm, and nonunion was defined as gaps larger than that [3]. Complications such as postoperative nerve palsies and dislocation were also recorded.
Statistical Analysis
With revision for any reason as the end point, Kaplan-Meier survival data were used to construct the survival probabilities [12]. In each survivorship analysis, the probability of survival was reported at the time when high numbers of hips remained at risk (minimum, 17 hips). The log-rank test was used to compare time-to-failure curves between the two groups.
Cox regression analysis was used to assess the time to failure between C1 and C2 subtype hips adjusted for confounding factors. For the identification of confounding factors among patients’ age, type of reconstruction (cemented, hybrid and cementless technique), contralateral hip diagnosis, leg lengthening, femoral shortening, and trochanteric reattachment and union, we used the independent sample t-test for the quantitative variables and Fisher’s exact test for the qualitative variables. Cox regression analysis was also used to identify the possible predicting variables of the time to failure using the Enter and Wald method.
Comparison of clinical results according to the Merle d’Aubigné-Postel scoring system as modified by Charnley between the groups was performed using paired and independent samples t-test.
All tests were two-sided with 95% significance level. We performed all statistical tests using SPSS® 20 statistical software (SPSS Inc, Chicago, IL, USA). Probability values < 0.05 were considered significant.
Results
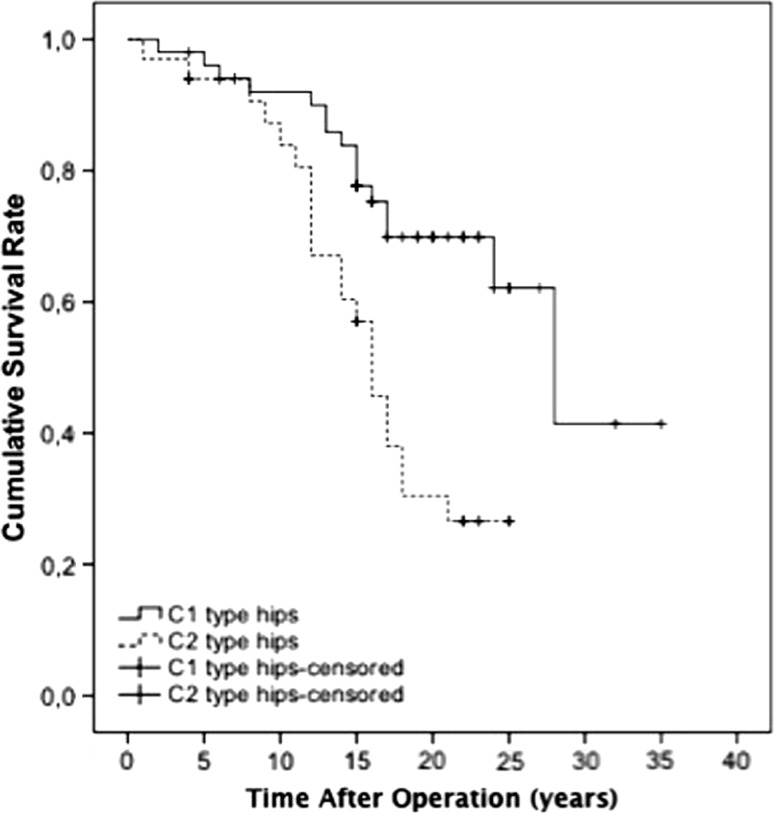
Hips that had a pseudoacetabulum (C1 hips) were less likely to be revised than those that did not (C2 hips). The Kaplan-Meier survivorship at 15 years, with reoperation for any reason as the end point, was 84% (± 10% [95% CI]) for the C1 subtype when 38 hips were at risk and 60% (± 17% [95% CI]) for the C2 subtype when 17 hips were at risk (p = 0.001) (Fig. 4). Sixteen hips (33%) of the C1 subtype and 21 hips (70%) of the C2 subtype were revised during the followup period. Cox regression analysis, after adjustment for confounding factors (leg lengthening and femoral shortening, see subsequently), showed also significantly worse survivorship in the C2 subtype (p = 0.021) (Table 2). Cox regression analysis, after adjustment for possible predictive factors, showed a statistically significant relationship of high dislocation subtype (p = 0.018) and trochanteric union (p = 0.005) with survival of THAs (Table 3). Cup placement was excluded from the analysis because none of the cups was placed higher than 3.5 cm, which is considered high placement. Patient’s age, type of reconstruction, contralateral hip diagnosis, leg lengthening, femoral shortening, and trochanteric reattachment were not predictive for the survival of THAs.
Fig. 4.
The Kaplan-Meier survivorship at 15 years with reoperation for any reason as the end point was 84% (± 10% [95% CI]) for the C1 subtype when 38 hips were at risk and 60% (± 17% [95% CI]) for the C2 subtype when 17 hips were at risk (p = 0.001).
Table 2.
Cox analysis for possible confounding factors
| Enter method | Reference category | RR (95% CI) | p value |
|---|---|---|---|
| Subtype of high dislocation | C1 | 3.094 (1.182–8.095) | 0.021 |
| Leg lenghtening | – | 0.966 (0.716–1.304) | 0.822 |
| Femoral shortening | – | 0.979 (0.744–1.287) | 0.878 |
RR = relative risk; CI = confidence interval.
Table 3.
Cox analysis for possible predictive factors
| Enter method | Reference category | RR (95% CI) | p value |
|---|---|---|---|
| Subtype of high dislocation | C1 | 3.788 (1.258–11.405) | 0.018 |
| Age of patient | – | 0.992 (0.960–1.024) | 0.602 |
| Type of reconstruction | Low friction arthroplasty | 1.493 (0.662–3.364) | 0.334 |
| Diagnosis of the contralateral hip | 0.202 | ||
| Dysplasia | Neutral | 0.822 (0.261–2.593) | 0.738 |
| Low dislocation | 0.837 (0.265–2.644) | 0.761 | |
| High dislocation | 0.364 (0.130–1.022) | 0.055 | |
| Leg lenghtening | – | 1.041 (0.726–1.493) | 0.827 |
| Femoral shortening | – | 1.044 (0.767–1.421) | 0.784 |
| Trochanteric reattachment | Optimal | 0.892 (0.335–2.372) | 0.818 |
| Trochanteric union | Bony | 3.192 (1.412–7.220) | 0.005 |
| Wald’s method | Reference category | RR (95% CI) | p value |
|---|---|---|---|
| Subtype of high dislocation | C1 | 3.021 (1.529–5.968) | 0.001 |
| Trochanteric reattachment | Optimal | 2.217 (1.077–4.561) | 0.031 |
RR = relative risk; CI = confidence interval.
Merle d’Aubigné-Postel scores for pain, function, and mobility improved from those obtained before surgery to those obtained at last followup in C1 and C2 hips; however, no significant differences were observed between postoperative scores of C1 and C2 hips (Table 4).
Table 4.
Comparison of clinical results according to the Merle d’Aubigné-Postel scoring system as modified by Charnley
| Subtype of high dislocation | Preoperative | Postoperative | ||||
|---|---|---|---|---|---|---|
| Pain | Function | Motion | Pain | Function | Motion | |
| C1 | 3 (1–6) | 3 (1–4) | 3 (0–5) | 5 (3–6)* | 5 (2–6)* | 4 (2–6)* |
| C2 | 3 (1–5) | 2 (1–3) | 5 (3–6) | 5 (5–6)* | 5 (4–5)* | 5 (4–6) |
| p value | 0.232 | 0.121 | 0.006 | 0.859 | 0.163 | 0.470 |
All variables are presented as median (minimum-maximum value); * p < 0.001 versus preoperative scores.
Leg lengthening was more in hips without a pseudoacetabulum despite the fact that these patients, on average, were treated with larger femoral shortening. The average leg lengthening for the C1 and C2 subtypes was 2.6 cm (range, 0–6 cm) and 4.2 cm (range, 2–6 cm), respectively (p < 0.001). The average femoral shortening in C1 and C2 hips was 1.7 cm (range, 0–5 cm) and 2.7 cm (range, 0–7 cm), respectively (p = 0.006).
There was no difference detected in the risk of greater trochanter nonunion between C1 and C2 hips. Bony union was observed in 35 (71.4%) C1 hips and 25 (83.3%) C2 hips (p = 0.233), fibrous union in 14 (28.6%) C1 hips and four (13.3%) C2 type hips, and nonunion in one (3.3%) C2 hip. The greater trochanter was reattached to its original bed in 19 C1 hips and 3 C2 hips, was advanced distally having contact with the distal part of the original bed in four C1 hips and five C2 hips, was reattached to the lateral femoral cortex in 12 C1 hips and 11 C2 hips, and was reattached proximally in 14 C1 hips and 11 C2 hips. There was no difference between C1 and C2 hips in terms of persistence of the Trendelenburg sign postoperatively (Table 5). The acetabular component was placed at the level of the teardrop in 26 (53%) C1 hips and 21 (70%) C2 hips, 1 cm higher to the teardrop in 17 C1 hips and seven C2 hips, 2 cm higher in two C1 hips and one C2 hip, and 3 cm higher in one C1 hip. The cup was placed 1 cm lower to the teardrop in three C1 hips and one C2 hip.
Table 5.
Persistence of the Trendelenburg sign postoperatively
| Subtype of high dislocation | Number of hips | ||||
|---|---|---|---|---|---|
| Preoperative | Postoperative* | ||||
| Positive (%) | Negative | Positive (%) | Less pronounced (%) | Negative (%) | |
| C1 | 49 (100) | – | – | 18 (37) | 31 (63) |
| C2 | 30 (100) | – | 1 (3)† | 13 (43) | 16 (53) |
* p = 0.560 for comparision using chi square test for persistence of the Trendelenburg sign for C1 and C2 type hips; †the number of postoperative positive hips is one, a value that cannot be analysed with chi square test and was excluded from the analysis.
Other Complications
There were two postoperative neurologic complications: one in the peroneal nerve in a patient with a C1 hip and one in the femoral nerve in a patient with a C2 hip. In both patients, there was full recovery within 6 months. Postoperative dislocation occurred in three C2 hips: 20 days and 17 years after hybrid THA and 9 years after low-friction arthroplasty.
Discussion
We have previously described two subtypes of high dislocation of the hip, depending on the presence (C1) or absence (C2) of a false acetabulum [10], and we have reported on the results of THA for high dislocation in this group of patients without separating C1 and C2 hips [8]. In this study, we determined whether the results of THA differ between the two aforementioned subtypes of high dislocation.
Limitations of the study are the retrospective nature of the investigation, the relatively small number of hips, and the use of different types of reconstruction. However, to our knowledge, no previous study has reported differences in results of THA in the two hip subtypes.
In our study, we investigated the potential differences in THA in the two high dislocation subtypes. Survivorship was lower in hips without a pseudoacetabulum (p = 0.001). Although there are no other studies in the literature comparing results of THA in high dislocation subtypes, this outcome seems reasonable, because C2 type hips have more affected morphology compared with C1 type hips that may result in a higher rate of failure [13, 21]. Cox regression analysis, after adjustment for confounding factors, also showed statistically significantly worse survivorship in the C2 subtype (p = 0.021) and, after adjustment for possible predictive factors, we found a statistically significant relationship of high dislocation subtype (p = 0.018) and trochanteric union (p = 0.005) with survival of THAs.
Differences regarding the latest clinical rating of pain, function, and motion were not statistically significant between C1 and C2 hips, although survivorship was significantly different between the two subtypes. Exact positioning of the cup at the level of the true acetabulum was obtained in 26 (53%) C1 hips and 21 (70%) C2 hips, probably because soft tissues were tighter in C1 hips than in C2 hips. However, none of the cups was placed higher than 3.5 cm, which is considered high placement [11, 17, 20]. To our knowledge, no previous study has compared these subtypes, and so it will be important that future studies replicate this finding to see whether it generalizes well to other study settings and approaches.
Femoral shortening during THA for high dislocation is necessary for the reduction of the components and avoidance of neurovascular complications. The extent of shortening is decided during surgery on the basis of the height of the dislocation and tightness of the soft tissues. We have performed this shortening by progressive resection of bone from the femoral neck [13, 22]. Other reported approaches to shortening are by subtrochanteric, diaphyseal, or distal osteotomy [2, 6, 14–16, 18, 19]. Nonetheless, shortening at the level of the femoral neck averaged in our study 1.7 cm in the C1 subtype and 2.7 cm in the C2 subtype and was easily and safely performed in contrast to the complicated technique of more distal osteotomies resembling an artificial fracture and usually requiring additional osteosynthesis.
Trochanteric nonunion has been considered as a major problem, with reported rates, even in routine arthroplasties, of up to 17% [1]. However, in this series, nonunion of the osteotomized greater trochanter was seen in one C2 hip. The patients with the 14 C1 hips and four C2 with fibrous union were asymptomatic. All three postoperative dislocations occurred in C2 hips in which the greater trochanter was united.
In this study, we found important differences in the results of THA in the C1 and C2 subtypes of high dislocation, most importantly in survival rate of the reconstructions. These findings indicate that when reporting results of THA in patients with high dislocations, mixing results of the two subtypes may lead to statistical bias. It is therefore important that these subtypes be stratified in analyses that deal with the survivorship of THAs for high hip dislocations.
Acknowledgments
We thank Antonios Galanos MSc, for his contribution to the statistical analysis and Professor S. M. Vratsanos for his kind suggestions regarding the writing style throughout the course of this work.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the National and Kapodistrian University of Athens, KAT Hospital, Athens, Greece.
References
- 1.Amstutz HC, Yao J. Trochanteric non-union. In: Amstutz HC, editor. Hip Arthroplasty. New York, NY, USA: Churchill Livingstone; 1991. p. 457. [Google Scholar]
- 2.Bernasek TL, Haidukewych GJ, Gustke KA, Hill O, Levering M. Total hip arthroplasty requiring subtrochanteric osteotomy for developmental hip dysplasia: 5- to 14-year results. J Arthroplasty. 2007;22:145–150. doi: 10.1016/j.arth.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 3.Browne AO, Sheehan JM. Trochanteric osteotomy in Charnley low-friction arthroplasty of the hip. Clin Orthop Relat Res. 1986;211:128–133. [PubMed] [Google Scholar]
- 4.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 5.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 6.Eskelinen A, Helenius I, Remes V, Ylinen P, Tallroth K, Paavilainen T. Cementless total hip arthroplasty in patients with high congenital hip dislocation. J Bone Joint Surg Am. 2006;88:80–91. doi: 10.2106/JBJS.E.00037. [DOI] [PubMed] [Google Scholar]
- 7.Hartofilakidis G, Babis GC, Georgiades G, Kourlaba G. Trochanteric osteotomy in total hip replacement for congenital hip disease. J Bone Joint Surg Br. 2011;93:601–607. doi: 10.2106/JBJS.J.00875. [DOI] [PubMed] [Google Scholar]
- 8.Hartofilakidis G, Karachalios T, Georgiades G, Kourlaba G. Total hip arthroplasty in patients with high dislocation: a concise follow-up, at a minimum of fifteen years, of previous reports. J Bone Joint Surg Am. 2011;93:1614–1618. doi: 10.2106/JBJS.J.00875. [DOI] [PubMed] [Google Scholar]
- 9.Hartofilakidis G, Stamos K, Karachalios T. Treatment of high dislocation of the hip in adults with total hip arthroplasty. Operative technique and long-term clinical results. J Bone Joint Surg Am. 1998;80:510–517. doi: 10.2106/00004623-199804000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Hartofilakidis G, Yiannakopoulos CK, Babis GC. The morphologic variations of low and high hip dislocation. Clin Orthop Relat Res. 2008;466:820–824. doi: 10.1007/s11999-008-0131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001;388:135–142. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 13.Karachalios T, Hartofilakidis G. Congenital hip disease in adults: terminology, classification, pre-operative planning and management. J Bone Joint Surg Br. 2010;92:914–921. doi: 10.1302/0301-620X.92B7.24114. [DOI] [PubMed] [Google Scholar]
- 14.Koulouvaris P, Stafylas K, Sculco T, Xenakis T. Distal femoral shortening in total hip arthroplasty for complex primary hip reconstruction. A new surgical technique. J Arthroplasty. 2008;23:992–998. doi: 10.1016/j.arth.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Krych AJ, Howard JL, Trousdale RT, Cabanela ME, Berry DJ. Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia. J Bone Joint Surg Am. 2009;91:2213–2221. doi: 10.2106/JBJS.H.01024. [DOI] [PubMed] [Google Scholar]
- 16.Macheras GA, Kateros K, Koutsostathis SD, Tsakotos G, Galanakos S, Papadakis SA. The Trabecular Metal Monoblock acetabular component in patients with high congenital hip dislocation: a prospective study. J Bone Joint Surg Br. 2010;92:624–628. doi: 10.1302/0301-620X.92B5.23256. [DOI] [PubMed] [Google Scholar]
- 17.Morag G, Zalzal P, Liberman B, Safir O, Flint M, Gross AE. Outcome of revision hip arthroplasty in patients with a previous total hip replacement for developmental dysplasia of the hip. J Bone Joint Surg Br. 2005;87:1068–1072. doi: 10.1302/0301-620X.87B8.15949. [DOI] [PubMed] [Google Scholar]
- 18.Nagoya S, Kaya M, Sasaki M, Tateda K, Kosukegawa I, Yamashita T. Cementless total hip replacement with subtrochanteric femoral shortening for severe developmental dysplasia of the hip. J Bone Joint Surg Br. 2009;91:1142–1147. doi: 10.1302/0301-620X.91B9.21736. [DOI] [PubMed] [Google Scholar]
- 19.Reikeraas O, Lereim P, Gabor I, Gunderson R, Bjerkreim I. Femoral shortening in total arthroplasty for completely dislocated hips: 3–7 year results in 25 cases. Acta Orthop Scand. 1996;67:33–36. doi: 10.3109/17453679608995605. [DOI] [PubMed] [Google Scholar]
- 20.Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J Bone Joint Surg Am. 1991;73:587–592. [PubMed] [Google Scholar]
- 21.Xu H, Zhou Y, Liu Q, Tang Q, Yin J. Femoral morphologic differences in subtypes of high developmental dislocation of the hip. Clin Orthop Relat Res. 2010;468:3371–3376. doi: 10.1007/s11999-010-1386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao X, Zhu ZA, Xie YZ, Yu B, Yu DG. Total hip replacement for high dislocated hips without femoral shortening osteotomy. J Bone Joint Surg Br. 2011;93:1189–1193. doi: 10.1302/0301-620X.93B9.25914. [DOI] [PubMed] [Google Scholar]