Abstract
Background
Inaccurate placement of an acetabular cup can cause impingement, dislocation, and accelerated wear. However, there is no universally agreed-on approach to measuring cup position using plain radiographs.
Objectives/purposes
Our goal was to evaluate the reliability and validity of measuring the orientation of acetabular components on plain anteroposterior (AP) radiographs.
Methods
We obtained plain AP radiographs and CT scans for 60 patients who underwent 60 primary total hip arthroplasties (THAs). The method devised by Lewinnek et al. was used to measure the orientation of acetabular components on plain AP radiographs, and three-dimensional (3-D) CT scans were used to measure both the radiographic anteversion angle and the inclination angle. Reliability was evaluated by analysis of the agreement between inter- and intraobserver measurements using plain AP radiographs. Measurements on 3-D CT scans were regarded as the reference standard; validity was assessed by comparing radiographic measurements with the CT scans.
Results
Inter- and intraobserver reliability for measuring component orientation on plain AP radiographs was nearly perfect with intraclass correlation coefficients of 0.896 and 0.969 for anteversion and 0.984 and 0.993 for inclination. Measurement of cup inclination angles differed between plain radiographs and CT scans, but the difference was small, and the difference, although statistically significant, probably was not clinically important (2.3° ± 1.8°, p < 0.001). There was no significant difference between the anteversion as measured on CT scan versus that measured on plain radiographs (p = 0.19).
Conclusions
Measurement of the orientation of acetabular components on plain AP radiographs is reliable and accurate compared with measurement on CT.
Level of Evidence
Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Inaccurate placement of an acetabular cup can cause impingement, dislocation, and accelerated wear after THA [3, 4, 9, 11]. Plain radiographs and CT scans have been used for measuring the orientation of acetabular components after THA. CT has been reported to be the most accurate for measuring anteversion [15, 21, 27, 29]. However, in clinical practice, plain radiographs are the most important tool for postoperative evaluation, because CT scans are obtained only for specific indications, whereas plain radiographs are obtained more routinely. The term orientation applies to both anteversion and inclination. Inclination can be easily measured on plain AP radiographs, whereas anteversion is more difficult to measure.
Many methods have been described for measuring cup anteversion from plain radiographs [1, 8, 13, 14, 23, 25, 28, 29]. The circumferential appearance of the cup opening face or wire maker is projected as an ellipse on plain radiographs. Picture Archiving and Communication System (PACS) workstations are now available in most hospitals; radiography has moved from hard-copy film to digital techniques, making it simple to draw the entire ellipse using electronic tools [20]. Therefore, Lewinnek’s method that draws the cup opening ellipse and calculates the angle using the arcsin of short versus long leg of the ellipse is more convenient for clinical practice. However, to our knowledge, only one study has attempted to demonstrate the reliability and validity of the method of Lewinnek et al. [13].
Therefore, we asked two questions: (1) What are the intraobserver reliability and interobserver reliability of the method of Lewinnek et al. for measuring cup inclination and anteversion? (2) Are inclination and anteversion measurements obtained from AP radiographs by the method of Lewinnek et al. and three-dimensional (3-D) CT measurements of the same patients similar?
Materials and Methods
We included in our study 60 patients who collectively underwent 60 primary THAs (35 men, 25 women; mean age, 47 years) between September 20 and October 20, 2011. Preoperative diagnoses were osteoarthritis (17 hips), osteonecrosis of the femoral head (35 hips), ankylosing spondylitis (four hips), and old femoral neck fracture (four hips). All arthroplasties were performed by eight experienced orthopaedic surgeons through a posterolateral approach. All implants were cementless: 18 Duraloc Option (DePuy Orthopaedics, Warsaw, IN, USA), 13 Pinnacle (DePuy), 15 Secur-Fit (Howmedica Osteonics, Mahwah, NJ, USA), seven Exceed ABT (Biomet UK, Waterton Industrial Estate, UK), and seven Reflection (Smith & Nephew, Memphis, TN, USA). The articulation was ceramic-on-ceramic in 54 hips, ceramic-on-polyethylene in four, and metal-on-polyethylene in two.
Plain AP radiographs, including bilateral hips and CT scans, were obtained between 3 days and 1 week after surgery. During radiographic examination, the patient was lying flat on the radiography table with the pelvis and legs in a neutral position. The x-ray beam was centered on the symphysis. The tube of the machine is routinely deployed perpendicular to the film (radiography table), whereas the tube–film distance can be set individually. In all cases, the tube–film distance was set to 110 cm to include both hips.
We used a spiral CT scanner (Aquilion 64-slice CT scanner; Toshiba, Tokyo, Japan). Scans were acquired at a pixel size of 0.782, at 140 mAs and 120 kV, including scans of the two anterosuperior iliac spines and the proximal femur. All images were digitally acquired using the PACS (Rogan-Delft View Pro-X, Version 3.2.0.12, Veenendaal, The Netherlands). The volume data were stored to an optical disk in DICOM (Digital Imaging and Communications in Medicine) format for later 3-D analysis. The protocol was approved by our institution’s ethics committee, and written informed consent was obtained from each patient.
Definitions
According to Murray’s definition [19], anteversion and inclination have been defined as radiographic, operative, and anatomic. The angles measured on a plain AP radiographs by the method of Lewinnek et al. are radiographic anteversion and inclination.
The selection of the coronal plane affects the values of the angles too. There are two coronal planes for measuring cup orientation, one is the anterior pelvic plane (APP) [18] defined by two anterosuperior iliac spines and the pubic tubercles and the other is the radiographic coronal plane (functional coronal plane). Postoperatively plain radiographs are taken on the radiographic coronal plane. Only when there is zero pelvic tilt are the APP and the radiographic coronal plane parallel. Pelvic posterior tilt increased the inclination and anteversion of the cup on the coronal plane and pelvic anterior tilt decreased the measurements on that plane. One degree of tilt changed anteversion by an average of 0.8° [16].
In this study, for consistency with Lewinnek’s method, the radiographic definition and radiographic coronal plane were used when measuring cup inclination and anteversion with the CT method.
Measurement of Cup Orientation on Plain Radiographs
We used the method devised by Lewinnek et al. [13] to calculate anteversion and measure inclination on plain AP radiographs (Fig. 1). Anteversion is arcsin (short axis/long axis), and inclination is the angle between the line on which the long axis of the ellipse is located and the interteardrop line. With the PACS program, the ellipse of the acetabular cup’s opening rim can be drawn; the short axis and long axis can be determined as well. The lengths of the short axis and the long axis are measured first, and then anteversion is calculated using the equation. Inclination can be directly measured on a plain radiograph with the PACS program.
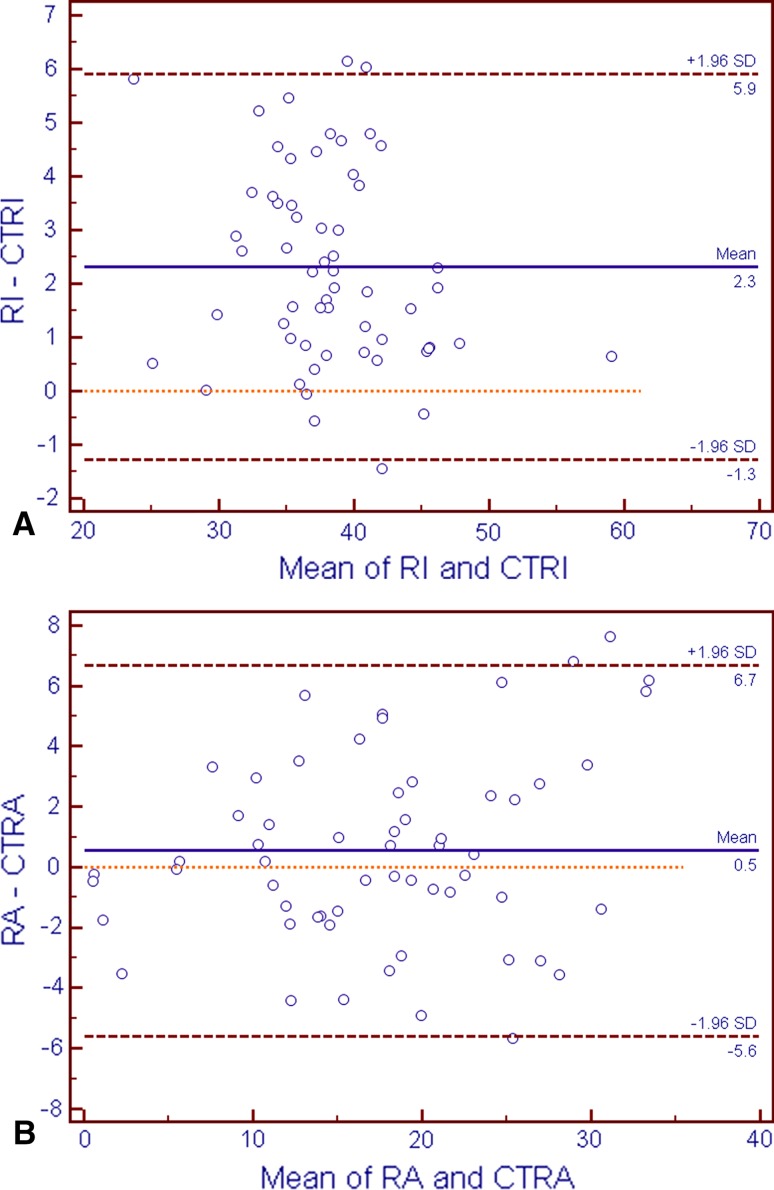
Fig. 1A–B.
(A) Sequence for drawing the elliptical appearance of the acetabular cup rim. First determine the two apexes of the cup, which is also the direction of the long axis. Then draw four random points on the cup opening rim, which is not obscured by the femoral head; the ellipse will be automatically completed. (B) Measuring the distance of the short and long axes of the ellipse (red lines) and inclination angle. Anteversion = arcsin (short axis/long axis); inclination is the angle between the line on which the long axis of the ellipse is located and the interteardrop line.
Measurement of Cup Orientation on Three-dimensional CT
We used the Materialise Interactive Medical Image Control System (MIMICS, Version 10.01, Leuven, Belgium) to reconstruct the pelvis and prosthesis after inputting the volumetric CT data. Using the radiographic plane of the CT table as the coronal plane, we corrected malpositioning, including rotation and abduction/adduction of the pelvis, during CT scanning but maintained flexion/extension position relative to the CT table so that the coronal planes used for both CT and plain radiographs were the same coronal plane (the radiographic coronal plane). Then the pelvic images were resliced so that on the new and standardized coronal plane, radiographic inclination was the angle between the line connecting the two points of the cup edge and the line connecting the two teardrops. According to Murray’s definition [19], radiographic anteversion is the angle between the axis of the cup and its projection on the coronal plane, and it can be measured on an oblique plane that is perpendicular to the coronal plane and the cup opening plane simultaneously. We used the MIMICS software to reconstruct the prosthesis and then drew the cup opening plane using three points on the cup rim. Then we drew a line perpendicular to the cup opening plane; the line is not the exact axis of the cup but is parallel to it in space. When we rotated the cup projection, the opening plane and the coronal plane became two lines on the computer screen, meaning that the screen was then the oblique plane that we wanted. Then by further rotating the projection, we made the coronal plane horizontal to the screen. The angle between the axis and the horizontal line represents radiographic anteversion. Using the screen software e-Ruler (MyCnKnow, Inc, www.mycnknow.com), we measured the angle of inversion on the computer screen (Fig. 2).
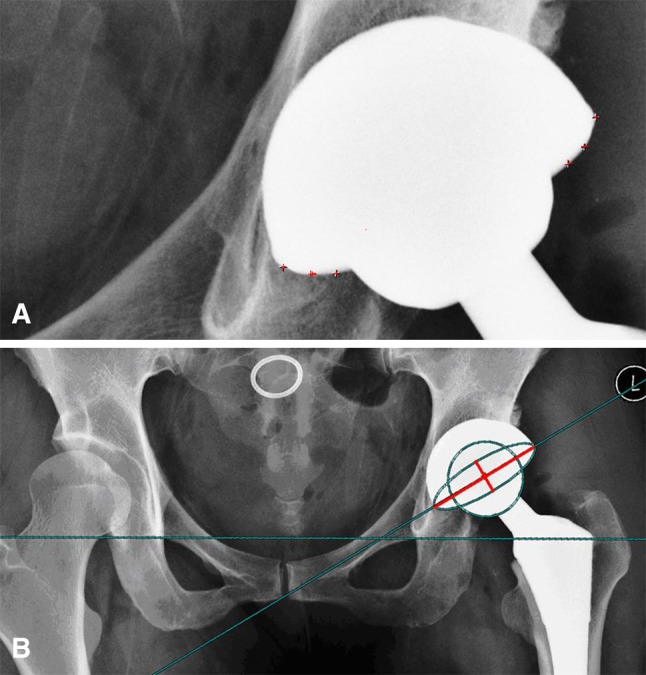
Fig. 2A–C.
(A) Measurement of radiographic inclination on the CT coronal plane. (B) Measurement of radiographic anteversion on 3-D CT. The cup opening plane (COP) and the coronal plane (two lines coming together) are both perpendicular to the screen. Here, for the purposes of illustration, the coronal plane (the dotted line) is not quite parallel to the horizontal line; otherwise, it would not be visible. The screen here is the plane on which radiographic anteversion (the angle between the axis and the horizontal line) should be measured using screen-measuring software. (C) For the convenience of measurement, we have shown only the prosthesis and lines here by making the bony pelvis invisible.
Assessment of Reliability and Validity
Reliability was defined as the agreement of measurements on plain radiographs, and validity was defined as proximity to measurements on CT. For assessing the intraobserver reliability of the radiographic method, one examiner (ML) measured all hips three times, with a 2-week interval between measurements, on randomly ordered radiographs without knowing the previous results. For the assessment of interobserver reliability, the other two examiners (HD, JZ) measured all hips by the same radiographic method independently. For the assessment of the validity of radiographic measurement, we used the average of radiographic measurements as the final result to compare with the average of CT measurements. The intraclass correlation coefficient (ICC) and the 95% confidence interval were calculated for inter- and intraobserver reliability. We used the one-way random-effects intraclass correlation model and absolute agreement to calculate the ICC. An ICC value of 1 means perfect reliability, and a value of 0 means the opposite. ICC values of 0.00 to 0.20 represented slight reliability, 0.21 to 0.40 represented fair reliability, 0.41 to 0.60 represented moderate reliability, 0.61 to 0.80 represented substantial reliability, and > 0.81 represented almost perfect reliability [12]. To determine the validity of the radiographic method compared with CT measurements, we used the paired t-test with statistical significance set at p < 0.05. Bland and Altman plots were used to show the discrepancies. We also calculated the means and SDs of radiographic anteversion and radiographic inclination measured on plain AP radiographs and 3-D CT, respectively.
Results
Inter- and intraobserver reliability was nearly perfect for anteversion (Table 1) as well as for inclination (Table 2) on plain radiographs. The ICCs for these measurements ranged from 0.896 (95% confidence interval [CI], 0.846–0.933) for the interobserver reliability of anteversion to 0.993 (95% CI, 0.989–0.996) for the intraobserver reliability of inclination.
Table 1.
Inter- and intraobserver reliability for anteversion measured on plain anteroposterior radiographs
| Type of reliability | ICC | 95% CI for ICC |
|---|---|---|
| Intraobserver | 0.969 | 0.948–0.981 |
| Interobserver | 0.896 | 0.846–0.933 |
ICC = intraclass correlation coefficient; CI = confidence interval.
Table 2.
Inter- and intraobserver reliability for inclination measured on plain anteroposterior radiographs
| Type of reliability | ICC | 95% CI for ICC |
|---|---|---|
| Intraobserver | 0.993 | 0.989–0.996 |
| Interobserver | 0.984 | 0.975–0.990 |
ICC = intraclass correlation coefficient; CI = confidence interval.
Validity of measurements on plain radiographs generally was excellent using 3-D CT scan as the reference standard. In terms of inclination, we observed a small but statistically significant difference between plain films and CT scans (2.3°, 1.8° SD, p < 0.001). There was no significant difference between the anteversion as measured on CT scan versus that measured on plain radiographs (0.6°, 3.1° SD, p = 0.19; Table 3).
Table 3.
Validity of radiographic measurements compared with CT measurements for anteversion and inclination using a paired t-test
| Dimension | Difference | |||
|---|---|---|---|---|
| Mean | SD | 95% CI | p value | |
| Radiographic anteversion | 0.55 | 3.14 | –0.27 to 1.36 | 0.186 |
| Radiographic inclination | 2.32 | 1.83 | 1.84 to 2.80 | <0.001 |
CI = confidence interval.
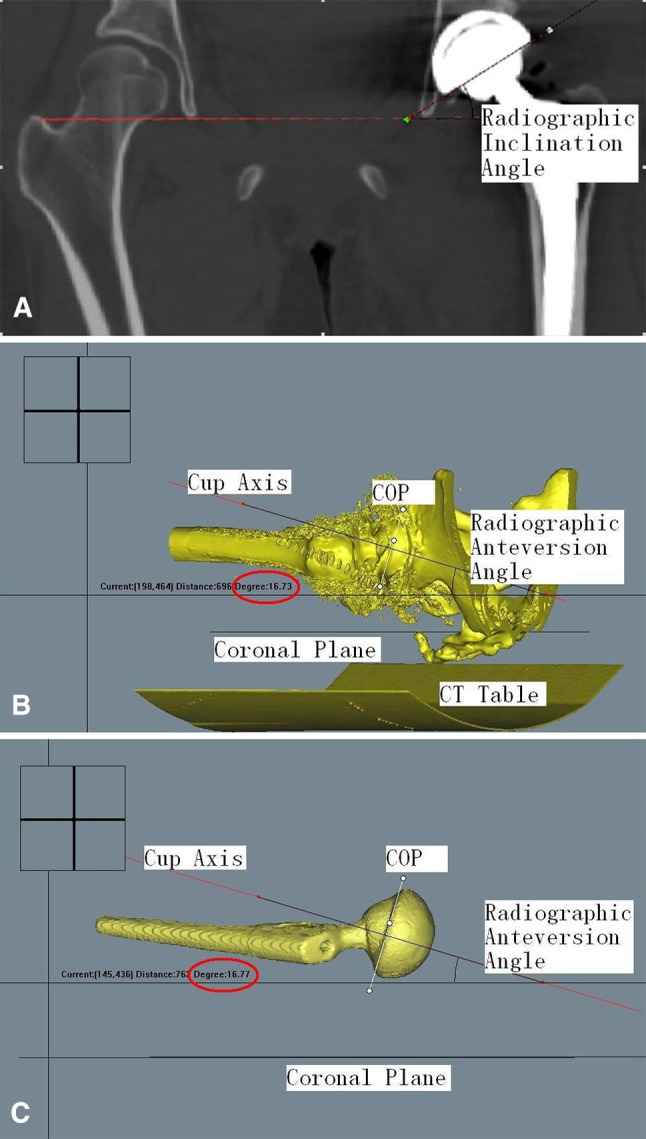
Bland-Altman plots showed that the means of the measurements were spread evenly and randomly for inclination and anteversion, indicating no systematical error (Fig. 3).
Fig. 3A–B.
Bland-Altman plots showed that the means of the measurements were spread evenly and randomly for inclination (RI) (A) and anteversion (B). CTRI = CT measurements of radiographic inclination; CTRA = CT measurements of radiographic anteversion.
The mean radiographic values (measured on plain AP radiographs) were 17.9° (SD, 8.7°) for anteversion and 39.4° (SD, 5.5°) for inclination. The mean CT values were 17.4° (SD, 7.9°) for anteversion and 37.0° (SD, 5.9°) for inclination. There were no hips with retroversion according to CT measurements.
Discussion
Acetabular component orientation is one of the most important factors determining the long-term outcomes of THA [3, 4, 9, 11]. CT has been reported to be the most accurate method for measuring cup orientation. However, because plain radiography has the benefit of ease in obtaining and interpretation, ubiquity, low radiation exposure, and low cost, it is the most widely used method for postoperative evaluation after THA [5, 8, 13, 14, 28, 29]. A so-called safe zone for cup orientation was proposed with anteversion of 15° ± 10° and inclination of 40° ± 10° based on the method of Lewinnek et al. [13]. Therefore, we sought to (1) determine the intraobserver and interobserver reliability of this method for measurements of inclination and anteversion; and (2) compare measurements by the method of Lewinnek et al. on AP radiographs and those obtained from 3-D CT.
Our study had several limitations. First, there is no gold standard for validation of radiographic or CT-based values in vivo. Because previous studies have shown that acetabular component orientation can be measured accurately by CT methods [15, 21, 26, 30], we used 3-D CT measurements as the reference standard. Although the software MIMICS is not widely used in clinical practice, the principle of our 3-D CT method is similar to those reported in the literature. The main difference is the method of determining cup opening plane and cup axis. Because little metal artifacts were encountered, finding the cup edge is not difficult in this study. Second, we used symphysis-centered radiographs to calculate anteversion. The center of the x-ray beam has been reported to affect the measurement of radiographic anteversion [7]. Because of divergence of the x-rays, centering over the hip versus centering over the pubic symphysis can theoretically lead to different anteversion angles. However, there is no simple general correction factor available. Ackland et al. [1] and Pradhan [23] suggested making a general correction by adding 5° for all symphysis-centered radiographs, but they presented no evidence to support that proposal. Goergen and Resnick [7] found a difference of 3.5° for radiographic anteversion between these two different x-ray centers. Widmer [28] calculated this difference to be 4° to 5° depending on inclination. In this study, using symphysis-centered radiographs, we did not perform any correction, but when we compared those measurements with measurements made on CT, we found the mean difference to be only 0.6° (SD, 3.1°). Therefore, we believe it is unnecessary to correct anteversion when using the PACS program for measuring cup anteversion on a symphysis-centered radiograph. Finally, retroversion cannot be determined from anteversion on an AP radiograph. In this study, there were no hips with retroversion according to CT measurements.
Two main factors affect the reliability of the method devised by Lewinnek et al.: one is drawing the ellipse, and the other is determining the two teardrops. As more and more hard-on-hard articulations are used in modern THA, the femoral head may more often obscure part of the cup rim so drawing the entire ellipse on a radiograph becomes difficult. Because PACS workstations are now available in most hospitals, radiography has moved from hard-copy film to digital techniques and electronic tools can be used reliably for the evaluation of hip arthroplasty [22], making it simple to draw the entire ellipse using electronic tools [20]. The interteardrop line affects the measurement of radiographic inclination. We found both inter- and intraobserver measurements of radiographic inclination are highly consistent. Therefore, determining the location of the teardrops is not a big problem in measuring inclination. With nearly perfect agreement on inter- and intraobserver measurements, we answered our first question that measurements of both acetabular component anteversion and inclination on plain AP radiographs are reliable. Our findings are similar to those of previous studies [6, 8, 20] (Table 4).
Table 4.
Reported inter- and intraobserver reliability for anteversion measured on plain radiographs
| Study | Method for measuring anteversion | ICC for intraobserver reliability | ICC for interobserver reliability |
|---|---|---|---|
| Hassan et al. [8] | Hassan’s method from AP radiographs | 0.97–0.99 | |
| Ghelman et al. [6] | Woo’s method from cross-table lateral radiographs | 0.9990–0.9992 | 0.9686 |
| Nho et al. [20] | Lewinneck’s method from AP radiographs | 0.938 | 0.943 |
| Current study | Lewinneck’s method from AP radiographs | 0.969 | 0.896 |
ICC = intraclass correlation coefficient.
Concerning the validity of radiographic methods for measuring cup orientation, we believe there are two main reasons for different conclusions of previous studies [6, 8, 17, 20]: (1) the definition of cup orientation and (2) the selection of the coronal plane. First, cup orientation has been defined as radiographic, operative, and anatomic [19]. Different methods for measuring anteversion are based on those different definitions of cup orientation. For example, on the transectional plane on CT, anteversion is anatomic, but when it is calculated from plain AP radiographs using the method of Lewinnek et al., it is radiographic. These two angles have different values, so it is inappropriate to compare them directly. Therefore, for comparing measurements of one method with those of another, the prerequisite is that the angles are based on the same definition. Second, the selection of the coronal plane affects the values of the angles too [16]. Some reports [15, 18, 21, 27, 30] on the use of the CT method to measure cup orientation have used the APP, which is defined by two anterosuperior iliac spines and pubic tubercles as the coronal plane. Although pelvic position in the method of Lewinnek et al. was standardized to the APP in the original study [13], postoperatively it is difficult to make the APP parallel to the radiographic coronal plane because of fixed deformity of the spine or contralateral hip. One study [2] has shown that the APP varies individually and postoperatively the pelvic tilt angle is not neutral when the subject is in the supine position. Malik et al. [16] reported that pelvic posterior tilt increased the inclination and anteversion of the cup on the coronal plane and that pelvic anterior tilt decreased the measurements on that plane. One degree of tilt changed anteversion by an average of 0.8°. Thus, to allow comparison of measurements made by the radiographic method with those made by the CT method, the same coronal plane should be qualified first; otherwise, each method will produce different results. For example, in hips with ankylosing spondylitis and severe pelvic posterior tilt, if the APP is used as the coronal plane to measure cup orientation, then the hips may appear to be in retroversion, but if the functional coronal plane (radiographic coronal plane) is used, the hips will be optimally anteverted (Fig. 4). In the method of Lewinnek et al., the radiographic coronal plane is used as a reference. Thus, when comparing measurements on radiographs with those on CT, we should use the same radiographic coronal plane.
Fig. 4A–B.
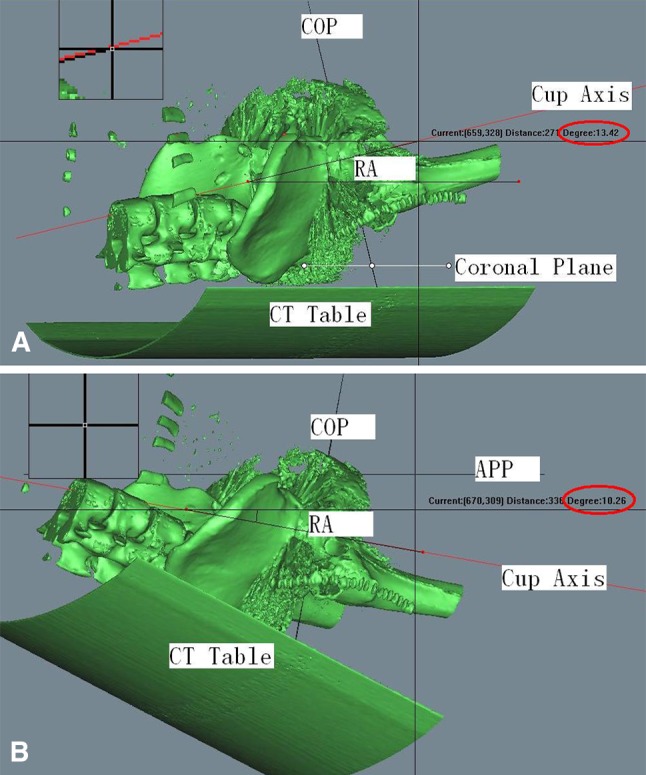
(A) Hip with ankylosing spondylitis and severe pelvic posterior tilt. Radiographic orientation, measured using the functional coronal plane, was in 13.4° of anteversion. (B) Hip with ankylosing spondylitis and severe pelvic posterior tilt. Radiographic orientation, measured using the APP as the coronal plane, was in 10.2° of retroversion. RA = radiographic anteversion; COP = cup opening plane.
There are a few studies on the accuracy of measuring anteversion on plain radiographs in the literature [6, 8, 17, 20]. Some used the same radiographic definition and radiographic coronal plane to compare measurements on plain radiographs with those on CT, whereas others did not (Table 5). Hassan et al. [8] compared measurements on plain radiographs with true measurements and found that plain radiographs produced accurate measurements of cup anteversion. Ghelman et al. [6] reported that CT outperforms cross-table lateral radiographs for determination of acetabular cup version after THA using the same definition and radiographic coronal plane. However, Marx et al. [17] used the radiographic definition and APP-referenced coronal plane and concluded that plain radiological methods were inaccurate for measuring cup anteversion compared with the CT method. Nho et al. [20] compared radiographic anteversion calculated from plain radiographs with anatomic anteversion measured on the CT transectional plane and concluded that methods of Lewinnek et al., Hassan et al., Liaw et al., and Woo et al. were accurate, whereas methods of Widmer and Ackland et al. were not. To our knowledge, this study is the first one using the same radiographic definition and radiographic coronal plane to assess the validity of the method of Lewinnek et al. compared with CT. We believe it was the selection of the coronal plane that made different conclusions between our study and the previous study [17].
Table 5.
Reported validity of plain radiographs measurements compared with CT measurements for anteversion
| Study | Method for measuring anteversion | Definition of anteversion measured on CT | Referenced coronal plane of CT | Mean error ± SD |
|---|---|---|---|---|
| Ghelman et al. [6] | Woo’s method from cross-table lateral radiographs | Radiographic anteversion | Radiographic coronal plane | 8.7° (range, −10.7° to 25°) |
| Hassan et al. [8] | Hassan’s method from AP radiographs | Not known (true measurements in vitro) | Not known (true measurements in vitro) | −2.5° (range, −0.8° to −3.4°) |
| Marx et al. [17] | AP radiographs for all: | Radiographic anteversion for all | APP for all | |
| McLaren’s method | −14.5° ± 10.5° | |||
| Ackland’s method | −14.3° ± 10.3° | |||
| Pradhan’s method | −14.5° ± 10.2° | |||
| Widmer’s method | −6.4° ± 10.8° | |||
| Hassan’s method | −14.4° ± 10.2° | |||
| Nho et al. [20] | AP radiographs | Anatomic anteversion | Radiographic coronal plane | Not known |
| Current study | Lewinneck’s method from AP radiographs | Radiographic anteversion | Radiographic coronal plane | 0.55° ± 3.14° |
Acetabular inclination angle can be directly and simply measured on AP radiographs, and its value is less affected by pelvic tilt. Previous studies have shown that inclination can be determined reliably on conventional radiographs compared with CT methods. Kalteis et al. [10] reported a mean difference of 0.54° ± 2.94° for operative inclination calculated from plain radiographic measurements compared with CT measurements. Steppacher et al. [24] reported the mean accuracy for radiographs measuring inclination in clinical series was 1.7° ± 1.7°. Our result with 2.3° ± 1.8° is similar to the previous studies. Considering the broad range of 40° ± 10° safe zone for inclination angle suggested by Lewinnek et al., we believe that the accuracy for measuring inclination angle on plain radiographs is acceptable for clinical use.
Our study found excellent reproducibility of the method of Lewinnek; in terms of validity, measurements made using plain radiographs were in good accord with those made on CT scans. We found no significant differences in measurements of anteversion; in terms of inclination, the difference we observed, although statistically significant, is probably clinically insignificant. Considering the advantages of plain radiography, including low cost, low radiation level, and convenience for clinical followup and assessment of prosthesis position, we believe the error is within a clinically acceptable range. Therefore, in measuring acetabular component orientation, plain AP radiographs provide reproducible and accurate data compared with CT. Radiographic divergence has little effect on the measurement of component orientation on plain radiographs using the PACS program. We recommended when comparing measurements of cup orientation on plain radiographs with those on CT, the same radiographic coronal plane should be used.
Acknowledgments
Medical editor, Katharine O’Moore-Klopf ELS (East Setauket, NY, USA), provided professional English-language editing of this article.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup: measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 2.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 3.Barrack RL, Lavernia C, Ries M, Thornberry R, Tozakoglou E. Virtual reality computer animation of the effect of component position and design on stability after total hip arthroplasty. Orthop Clin North Am. 2001;32:569–579. doi: 10.1016/S0030-5898(05)70227-3. [DOI] [PubMed] [Google Scholar]
- 4.Del Schutte H, Jr, Lipman AJ, Bannar SM, Livermore JT, Ilstrup D, Morrey BF. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13:621–626. doi: 10.1016/S0883-5403(98)80003-X. [DOI] [PubMed] [Google Scholar]
- 5.DiGioia AM, 3rd, Jaramaz B, Plakseychuk AY, Moody JE, Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 6.Ghelman B, Kepler CK, Lyman S. Della Valle AG. CT outperforms radiography for determination of acetabular cup version after THA. Clin Orthop Relat Res. 2009;467:2362–2370. doi: 10.1007/s11999-009-0774-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goergen TG, Resnick D. Evaluation of acetabular anteversion following total hip arthroplasty: necessity of proper centering. Br J Radiol. 1975;48:259–260. doi: 10.1259/0007-1285-48-568-259. [DOI] [PubMed] [Google Scholar]
- 8.Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D. Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty. 1995;10:369–372. doi: 10.1016/S0883-5403(05)80187-1. [DOI] [PubMed] [Google Scholar]
- 9.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip prosthesis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 10.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;5:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 12.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 13.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 14.Liaw CK, Hou SM, Yang RS, Wu TY, Fuh CS. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res. 2006;451:134–139. doi: 10.1097/01.blo.0000223988.41776.fa. [DOI] [PubMed] [Google Scholar]
- 15.Lin F, Lim D, Wixson RL, Milos S, Hendrix RW, Makhsous M. Validation of a computer navigation system and a CT method for determination of the orientation of implanted acetabular cup in total hip arthroplasty: a cadaver study. Clin Biomech (Bristol, Avon). 2008;23:1004–1011. doi: 10.1016/j.clinbiomech.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Malik A, Wan Z, Jaramaz B, Bowman G, Dorr LD. A validation model for measurement of acetabular component position. J Arthroplasty. 2010;25:812–819. doi: 10.1016/j.arth.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 17.Marx A, von Knoch M, Pförtner J, Wiese M, Saxler G. Misinterpretation of cup anteversion in total hip arthroplasty using planar radiography. Arch Orthop Trauma Surg. 2006;126:487–492. doi: 10.1007/s00402-006-0163-0. [DOI] [PubMed] [Google Scholar]
- 18.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 19.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 20.Nho JH, Lee YK, Kim HJ, Ha YC, Suh YS, Koo KH. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012;94:32–36. doi: 10.1302/0301-620X.94B1.27621. [DOI] [PubMed] [Google Scholar]
- 21.Olivecrona H, Weidenhielm L, Olivecrona L, Beckman MO, Stark A, Noz ME, Maguire GQ, Jr, Zeleznik MP, Svensson L, Jonson T. A new CT method for measuring cup orientation after total hip arthroplasty: a study of 10 patients. Acta Orthop Scand. 2004;75:252–260. doi: 10.1080/00016470410001169. [DOI] [PubMed] [Google Scholar]
- 22.Patel SR, Toms AP, Rehman JM, Wimhurst J. A reliability study of measurement tools available on standard picture archiving and communication system workstations for the evaluation of hip radiographs following arthroplasty. J Bone Joint Surg Am. 2011;93:1712–1719. doi: 10.2106/JBJS.J.00709. [DOI] [PubMed] [Google Scholar]
- 23.Pradhan R. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs. J Bone Joint Surg Br. 1999;81:431–435. doi: 10.1302/0301-620X.81B3.9067. [DOI] [PubMed] [Google Scholar]
- 24.Steppacher SD, Tannast M, Zheng G, Zhang X, Kowal J, Anderson SE, Siebenrock KA, Murphy SB. Validation of a new method for determination of cup orientation in THA. J Orthop Res. 2009;27:1583–1588. doi: 10.1002/jor.20929. [DOI] [PubMed] [Google Scholar]
- 25.Visser JD, Konings JG. A new method for measuring angles after total hip arthroplasty: a study of the acetabular cup and femoral component. J Bone Joint Surg Br. 1981;63:556–559. doi: 10.1302/0301-620X.63B4.7298684. [DOI] [PubMed] [Google Scholar]
- 26.Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wassilew GI, Perka C, Koenig C, Janz V, Asbach P, Hasart O. 3D CT analysis of combined cup and stem anteversion in cases of cup navigation in hip arthroplasty. Orthopedics. 2010;33(Suppl):48–51. doi: 10.3928/01477447-20100510-53. [DOI] [PubMed] [Google Scholar]
- 28.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 29.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 30.Ybinger T, Kumpan W, Hoffart HE, Muschalik B, Bullmann W, Zweymüller K. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements. J Arthroplasty. 2007;22:812–817. doi: 10.1016/j.arth.2006.10.001. [DOI] [PubMed] [Google Scholar]