Abstract
Background
Non-organ-specific autoantibodies are found in a considerable number of anti-HCV positive patients. Previous studies investigated the clinical relevance of these antibodies in patients treated with interferon monotherapy, but not combination therapies.
Methods
Anti-nuclear, anti-smooth muscle, anti-mitochondrial, anti-neutrophil-cytoplasmatic and anti-liver/kidney microsomal antibodies were determined in 78 consecutive anti-HCV positive patients by indirect immunofluorescence. The presence of these antibodies was related to demographic variables and to the outcome of antiviral combination therapy with interferon-α and ribavirin in 65 patients.
Results
In our study, positivity for autoantibodies was associated with higher alanine aminotransferase levels and higher mean values for HCV-RNA (p < 0.01). Furthermore, negativity for non-organ-specific autoantibodies was associated with a favourable treatment outcome of combination therapy with at least one negative RT-PCR for HCV-RNA during treatment (OR 4.65, 95% CI 1.31 to 16.48, p = 0.02). ANA and SMA staining patterns and titers were not correlated to treatment response. With multiple logistic regression analysis, positivity for autoantibodies and HCV genotype were independently associated with outcome of antiviral combination therapy (p = 0.02).
Conclusions
The absence of non-organ-specific autoantibodies might indicate a significantly higher chance for viral clearance in response to combination therapy for chronic hepatitis C infection. Therefore, despite of an overall higher treatment response, the addition of the immunomodulatory drug ribavirin could accentuate immunological differences that affect treatment outcome and might have been less obvious in earlier studies analysing interferon monotherapy.
Keywords: Antiviral therapy, chronic hepatitis C, interferon-α, non-organ-specific autoantibodies, ribavirin
Background
Various immunological phenomena have been described in patients being exposed to the hepatitis C virus (HCV) [1]. Organ-specific and non-organ-specific autoantibodies are found in a considerable number of patients with acute and chronic hepatitis C [2]. Especially the high percentage of non-organ-specific autoantibodies (NOSA) in chronic infection has led to further investigation of the potential biological relevance of these findings. In recent studies the prevalence of different NOSA, including anti-nuclear antibodies (ANA), anti-smooth muscle antibodies (SMA), anti-mitochondrial antibodies (AMA), anti-neutophil-cytoplasmatic antibodies (ANCA), and anti-liver/kidney micosomal antibodies (LKM) were investigated before, during and after monotherapy with interferon-α for chronic hepatitis C [3,4]. However, there is little information on NOSA prevalence in patients treated with current standard therapy, i.e. the combination of interferon-α and ribavirin. This should be investigated, as ribavirin has been demonstrated to have distinct immunomodulatory effects [5,6]. Furthermore, the former analyses of the influence of NOSA on the clearance of the hepatitis C virus upon monotherapy with interferon-α are controversial, with a few studies showing a tendency to a poorer treatment response in autoantibody-positive subjects while other investigations could not demonstrate any difference in the efficacy of therapy [3,7,8]. However, there are no studies so far that investigated the relevance of NOSA with regards to the virological and biochemical response in patients treated with interferon-α plus ribavirin. This combination therapy now represents the treatment of choice since it has been proven to be superior to interferon monotherapy in large randomised trials [9].
The aim of the present study was to determine the prevalence of NOSA in patients positive for anti-HCV antibodies and to systematically analyse the potential impact of these antibodies on the efficacy of a combined antiviral therapy with interferon-α and ribavirin in patients with chronic hepatitis C infection.
Methods
Patients and diagnosis of hepatitis C
A total of 78 patients were enrolled in the study between 1999 and the end of 2000. All patients were found to be anti-HCV positive in a second-generation enzyme-linked immunosorbent assay (Abbot Ltd., USA). Patients with a repeatable (> six months) positive viral RNA (> 600 viral copies/ml, Cobas Amplicor, Roche, Switzerland, n = 65 individuals) were considered to have chronic hepatitis C virus infection.
As the study included the measurement of autoantibodies, all subjects were thoroughly screened for autoimmune diseases during physical examination and history taking. A panel of standard laboratory parameters, including hematological, coagulation and serological parameters was taken from all subjects. In all patients mean daily alcohol intake was below 40 g. Serum assays for the hepatitis B virus surface antigen and human immunodeficiency virus were negative (all assays from Abbott Ltd., USA). The laboratory values for α1-antitrypsin, transferrin saturation and coeruloplasmin were within normal ranges in all subjects.
Furthermore, all patients were evaluated according to the revised scoring system for the diagnosis of autoimmune hepatitis. Using this algorithm, none of the patients investigated in our study displayed a score of more than 10 points, excluding autoimmune hepatitis as the underlying liver disease with a high sensitivity and specificity in our patients [10].
Liver Histology
All subjects who were found positive for HCV-RNA underwent percutaneous liver biopsy and histological parameters were classified according to the score system of Batts and Ludwig [11]. The necro-inflammatory activity in the obtained specimen was graded from 0 (no activity) to 4 (severe activity) by a pathologist blinded to the study design (J.L.).
Antiviral combination therapy
Overall, 48 patients with chronic hepatitis C infection were treated with 3 million units interferon-α 2a (20 subjects) or 2b (28 subjects) three times a week and 1000 or 1200 mg ribavirin daily depending on body weight.
HCV-RNA was tested after 4, 12, 24 and 48 weeks during therapy and 4, 12 and 24 weeks after completion of therapy. Overall, there were 17 sustained responders (35.4%) and 4 relapsers (8.3%), while 27 subjects showed no virological response (56.3%). In anticipation of a small number of patients in our single-centre study, we initially decided that any negative RT-PCR during treatment or thereafter should be considered as a positive treatment response for the purpose of this particular investigation. After completion of patients' enrolment all analyses were re-calculated with stratification of patients according to the current standard criteria for treatment response [9].
The study protocol was approved by the local ethic committee in accordance to the Declaration of Helsinki.
Autoantibody determination
ANA, AMA, SMA, ANCA and LKM antibodies were searched for by indirect immunofluorescence (IFL) on Hep-2 cells, cryostat sections of rat liver, kidney, stomach, and human granulocytes, respectively. The initial dilution was 1:20 following standard protocols [12,13]. Positive reactions were titrated by double dilution to the end point. Serum reactivity at a dilution of at least 1:40 was considered as a positive result for all autoantibodies in this study. ANA and SMA staining patterns were identified according to published protocols [12,13]. Antibody assays were performed prior to and during antiviral treatment.
Data collection and statistical analysis
Continuous variables were compared by using the unpaired Student's t test with Welsh correction in case of unequal variances. Univariate analysis of dichotomous variables in contingency tables was performed with Fisher's exact test. Multivariate analysis was done by logistic regression analysis with treatment outcome as dependent variable and presence of autoantibodies, HCV genotype and HCV-RNA concentrations as covariates. Univariate and regression analyses were performed with STATA 7.0 software (College Station, TX,, USA), employing a package of commands (Genassoc) written by D. Clayton and available from http://www-gene.cimr.cam.ac.uk/.
Results
Demographic analysis
Table 1 summarises the autoantibody prevalence in our study patients. Overall, 36 patients had at least one NOSA (ANA, AMA, ANCA, or SMA) at a titer higher than 1:40 as determined by IFL. SMA was the most frequent autoantibody (32.0%) followed by ANA in 19.2% of the subjects. AMA and ANCA were detected in only a small number of cases at low titers (n = 2 and n = 4, respectively) and no anti-M2 antibodies were found in the AMA-positive sera. Furthermore, in the two patients who were tested positive for AMA, values for IgM and bilirubin were within the normal range and the liver biopsies revealed no signs of primary biliary cirrhosis. LKM antibodies were not detectable in our patients. For further analysis the patients were divided in two groups, as shown in table 2. The first group comprised the subjects without NOSA; the second group represented autoantibody-positive patients.
Table 1.
Prevalence of non-organ specific autoantibodies in anti-HCV positive patients (n = 78).
| Autoantibody (Titer ≥ 1:40 by IFL) | n (%) |
| ANA | 15 (19.2) |
| SMA | 25 (32.0) |
| AMA | 2 (2.6) |
| ANCA | 4 (5.2) |
| LKM | 0 (0) |
| Any autoantibody | 36 (46.2) |
| ANA and/or SMA | 33 (42.3) |
All serum autoantibodies were determined by indirect immunofluorescence (IFL). A serum dilution of at least 1:40 was considered as a positive result. ANA, anti-nuclear antibodies; SMA, anti-smooth muscle anibodies; AMA, anti-mitochondrial antibodies, ANCA, anti-neutophil-cytoplasmatic antibodies; LKM, anti liver/kidney microsomal antibodies
Table 2.
Anti-HCV positive patients with and without serum autoantibodies (ANA, SMA, ANCA, AMA) – comparison of demographic variables, clinical, and biochemical parameters.
| Autoantibody-negative (n = 42) | p**** | Autoantibody-positive (n = 36) | |
| Gender (m/f) | 16/26 | 0.81 | 15/21 |
| Age (yrs)* | 46.1 ± 12.6 | 0.25 | 42.9 ± 12.2 |
| HCV genotype | |||
| Genotype 1 and 4 | 24 | 0.57 | 22 |
| Genotypes 2 and 3/ not detected | 18 | 14 | |
| HCV-RNA (copies/ml)* | 4.1 × 105 ± 5.5 × 105 | 0.007 | 9.1 × 105 ± 9.6 × 105 |
| ALT (U/l)* | 27.4 ± 25.0 | 0.006 | 47.5 ± 36.3 |
| AST (U/l)* | 21.5 ± 26.9 | 0.11 | 33.2 ± 35.9 |
| Albumin (g/l)* | 46.0 ± 8.3 | 0.16 | 43.8 ± 4.8 |
| IgG (g/l)* | 13.9 ± 3.1 | 0.08 | 15.4 ± 4.0 |
| IgM (g/l)* | 2.1 ± 0.9 | 0.69 | 2.2 ± 2.0 |
| IgA (g/l)* | 1.4 ± 0.8 | 0.23 | 1.8 ± 1.7 |
| IgG to CMV (pos / neg)*** | 22 / 11 | 0.44 | 17 / 14 |
| IgG to EBV (pos / neg)*** | 28 / 5 | 0.99 | 28 / 4 |
| Histological score** | 1.4 ± 0.8 | 0.62 | 1.5 ± 0.6 |
| Interferon-α treatment [n (%)] | 27 (64%) | 0.64 | 21 (58%) |
*Mean ± SD, **Necro-inflammatory activity in liver biopsy were graded from 0 (no activity) to 4 (severe activitiy), ***IgG antibodies to cytomegaly virus and Ebstein-Barr virus were determined by ELISA, ****p-values were calculated by Fisher's exact test or Student's t test where appropriate
Table 2 demonstrates that there were no differences between the groups regarding age, HCV genotype distribution, AST, albumin and IgG to cytomegaly virus, or Ebstein-Barr virus. Of note, there were also no significant differences between autoantibody-positive and autoantibody-negative subjects with regards to levels of total IgG, IgM, and IgA. The necro-inflammatory activity upon histological examination of the liver biopsies also did not reveal a significant difference between the groups. In contrast, ALT values and the concentrations of HCV-RNA were significantly higher in autoantibody-positive patients compared to autoantibody-negative subjects (p = 0.006 and p = 0.007, respectively).
Association between NOSA and efficacy of antiviral therapy
Figures 1 and 2 illustrate the potential interactions between NOSA and response to antiviral treatment. Overall, 78 patients with positive anti-HCV were included in the study. In 65 subjects (83.3%) HCV-RNA was detectable for more than six months, indicating a chronic viral infection. In 13 patients (16.7%) no viral replication was found upon repeated testing by RT-PCR, suggesting spontaneous viral clearance. Figure 1 illustrates that in 3 of these 13 patients at least one NOSA could be detected, while no autoantibodies were found in the majority (n = 10) of these patients (OR 3.44, 95% CI 0.87 to 13.65, p = 0.07).
Figure 1.
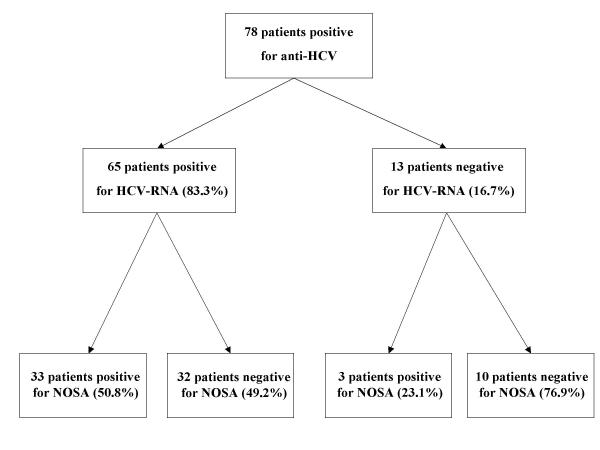
Overall, 78 anti-HCV positive patients were screened for HCV-RNA. IN 65 patients (83.3%) HCV-RNA was detected. In 13 patients (16.7%) no HCV-RNA was found upon repeated testing, suggesting viral clearance in these patients. There is a trend towards a higher rate of viral clearance in patients without NOSA compared to patients with NOSA (p = 0.07, Fisher's exact test). NOSA, non-organ-specific autoantibodies.
Figure 2.
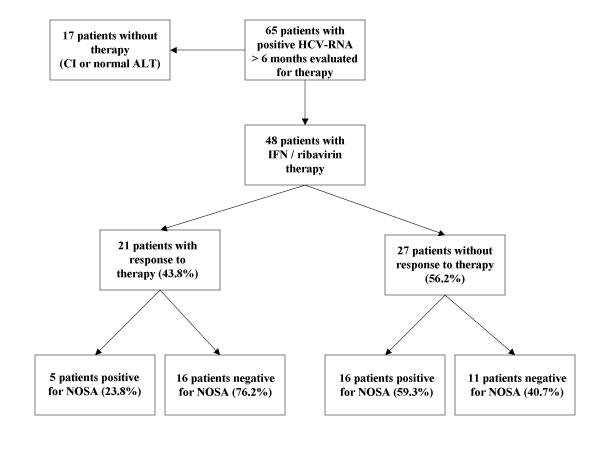
65 patients with viral persistence for more than six months antiviral therapy was considered. Seventeen patients were excluded from antiviral therapy due to contraindications, i.e. repeatable normal ALT values, severe psychiatric disorders, or persistent drug abuse. Forty-eight patients were treated with interferon-α and ribavirin for at least six months. Overall, 21 patients (48.3%) had at least one negative RT-PCR for HCV-RNA, while 27 patients (56.2%) did not show a virological response. Among the patients who responded to the therapy 76.2% had no detectable NOSA, while 23.8% were positive for NOSA. Absence of NOSA was statistically associated with a favourable treatment response (OR 4.65, 95% CI 1.31 to 16.48, Fisher's exact test) in univariate and multivariate analysis. ALT, alanine aminotranferase; NOSA, non-organ-specific autoantibodies; RT-PCR, reverse transcriptase polymerase chain reaction; OR, odds ratio; CI, contraindications.
In 48 of 65 patients with measurable viral replication a combination therapy with interferon-α and ribavirin adjusted to body weight was initiated. Twenty-seven patients had no detectable antibodies before or during treatment, whereas in 21 cases at least one NOSA was detected. HCV genotype distributions were similar between groups. Overall, 21 of the 48 treated patients showed a virological response to treatment with a repeatable negative RT-PCR during or after completion of the therapy. Figure 2 depicts that 16 of these 21 patients (76.2%) had no detectable autoantibodies during the course of the study, whereas only 5 patients (23.8%) were positive for any NOSA. This favourable treatment response in autoantibody-negative individuals was significant in univariate analysis (OR 4.65, 95% CI 1.31 to 16.48, p = 0.019). We additionally calculated a regression analysis to control for known predictive factors related to the outcome of antiviral treatment. In this multivariate analysis, positivity for autoantibodies (OR 7.4, CI 1.3 – 39.5, p = 0.02) and HCV genotype (OR 6.1, CI 1.0 – 36.2, p = 0.048) were both independently associated with the outcome of antiviral therapy.
Titers and staining patterns of ANA and SMA in relation to antiviral therapy
Table 3 displays the prevalence, titers and staining patterns of ANA and SMA in patients with a response or non-response to treatment with interferon-α and ribavirin. Of these two autoantibodies, SMA were detectable at significantly higher frequencies in non-responders compared to patients with a sustained response to antiviral therapy (OR 4.8, CI 1.4 – 20.2, p = 0.03). In contrast, the titers of ANA and SMA did not differ between the groups. ANA showed a speckled pattern in all cases, whereas only one patient had SMA without a vessel wall staining pattern.
Table 3.
Titers and staining patterns of ANA and SMA in responders and non-responders to antiviral combination therapy.
| Responder (n = 21) | Non-responder (n = 27) | p* | |
| ANA [n (%)] | 2 (9.5) | 5 (18.5) | 0.44 |
| ANA titer [median (range)] | 1:80 (1:80 – 1:160) | 1:80 (1:40 – 1:320) | |
| Speckled staining pattern [n (%)] | 2 (100) | 5 (100) | |
| SMA [n (%)] | 3 (14.3) | 12 (44.4) | 0.03 |
| SMA titer [median (range)] | 1:40 (1:40–1:80) | 1:40 (1:40 – 1:160) | |
| Vessel wall staining pattern [n (%)] | 3 (100) | 11 (91.7) |
*p-values were calculated with Fisher's exact test
Discussion
The nucleoside analogue ribavirin has been demonstrated to increase the efficacy of antiviral treatment for hepatitis C when used in combination with interferon-α [9]. As the role of the balance between Th1- and Th2-associated cytokines has been shown to be of primary importance in antiviral therapy [14], the superiority of the current standard treatment might be partly attributed to the immunomodulatory properties of ribavirin [5,6,15]. The aim of our study was to assess whether such properties of ribavirin could unmask clinical differences with relation to the presence of autoantibodies in patients with hepatitis C. Therefore, we first determined the prevalence of NOSA in a cohort of 78 anti-HCV positive patients. In our study, a total of 46.2% of subjects had at least one NOSA, with ANA and SMA showing the highest prevalence rates (19.2% and 32.0%, respectively). The prevalence of NOSA in our patients is comparable to previous studies [2,16], which demonstrated these antibodies to be present at similar frequencies. AMA and ANCA have been rarely found in patients with hepatitis C [17,18], which was confirmed in our cohort of patients. In contrast to other investigations [16,19], LKM antibodies were not detected in our patients, most likely due to the sample size and the cut-off for positivity of immunofluorescence (reactivity at serum dilution ≥ 1: 40) in our study. The analysis of ANA and SMA subspecificities revealed that the vast majority of these autoantibodies in our study subjects were ANA with a speckled pattern and SMA with a vessel wall staining pattern, which is in line with earlier findings [7,16,20]. In these former studies positivity for NOSA was associated with distinct clinical and laboratory variables. Cassani et al. [7] found an association between NOSA (mostly ANA and SMA) and female gender, AST and AST values as well as with necro-inflammatory activity in liver biopsies. The correlation between ALT and the presence of NOSA could be reproduced in our series, but there was no association between the presence of NOSA and either gender or grade of portal necro-inflammation in liver specimens. The latter differences are likely due to the different sizes of the study populations, as other smaller studies could also not confirm a close relationship between NOSA and gender or liver histology [16,21]. Interestingly, despite a considerable overlap between groups, the association of ALT values with positive NOSA seems to be reproducible throughout different studies [7,22].
The clinically most important finding of our study is the different efficacy of antiviral therapy with ribavirin and interferon-α in patients without NOSA as compared to subjects tested positive for NOSA. Absence of NOSA prior to and during the combination therapy was associated with a highly favourable treatment response with an odds ratio of 4.65 (95% CI 1.31 – 16.48). This association held true after adjustments for HCV genotypes and HCV-RNA levels in logistic regression analysis. Since we focused on immunological parameters in a small cohort of patients, a positive treatment response was initially defined as any negative HCV-RNA throughout the course of the study. However, there was no subject with a viral breakthrough and only four patients relapsed after completion of the therapy (two with NOSA, two without NOSA). The re-analysis with inclusion of the latter patients does support our major conclusions (OR 6.46, 95% CI 1.54 – 27.19).
These results differ from other studies that could not find an association between presence of NOSA and efficacy of antiviral therapy [8,23]. However, the former studies employed interferon monotherapy, whereas combination therapy (interferon-α plus ribavirin) was used in our patients only. Furthermore, in two studies [3,7], including the one with the highest number of patients (n = 144) [7], a trend towards a poorer response to therapy in patients with autoantibodies was already noted. In both studies this trend just failed the 95%-level of statistical significance.
Why should the addition of ribavirin to antiviral therapy make a difference? In view of our data and published results [7,16,19,20,22] the presence of autoantibodies can be interpreted as a marker for a non-specific activation of mononuclear cells in response to infection with the hepatitis C virus. This might be associated with an attenuation of the specific immune response and consecutive failure to clear the virus in a number of patients. This hypothesis is supported by our finding that patients with NOSA have a higher viral load compared to subjects without autoantibodies. As ribavirin has distinct immunomodulatory properties, the addition of this agent to the therapy might modulate the balance between a specific antiviral and a non-specific immune response in selected patients. Therefore, despite the overall benefits of ribavirin, the addition of this immunomodulatory drug to the therapy could unmask individual differences in the immune balance (Th1 versus Th2) with regards to antiviral treatment, which were not obvious in studies investigating interferon monotherapy only. In accordance to these findings, a recent study could demonstrate that the addition of ribavirin to interferon monotherapy does not modify the thyroid autoantibody pattern but increases the risk to develop hypothyroidism, which was significantly associated with long-term remission [24]. It is important to note that safe and efficacious therapy is still lacking for patients with hepatitis C and (auto)immune abnormalities and that it is mandatory to be aware of the potentially life-threatening autoimmune reaction in patients with chronic hepatitis C and positive NOSA during interferon therapy. Therefore, further studies with larger numbers of patients are needed to confirm the clinical relevance of our findings.
Our observations are related to the immunopathological discrimination between chronic hepatitis C, autoimmune hepatitis, and the "hepatitis C-autoimmune-overlap syndrome". In our study, we employed the revised scoring system for the diagnosis of autoimmune hepatitis in order to exclude a predominant autoimmune liver disease with sufficient specificity and sensitivity [10,25]. Furthermore, only one of our patients had low titer SMA without vessel wall staining pattern and none had ANA with homogeneous staining pattern or LKM antibodies, which are closely correlated to autoimmune hepatitis [26]. Nevertheless, there are clinical presentations with mixed or atypical features because exclusive viral and autoimmune disorders only represent the two ends of the diagnostic spectrum [27]. Therefore, in the light of our and previous studies, NOSA might be determined in order to further stratify patients with chronic hepatitis C and (auto)immune abnormalities.
Conclusions
In this study, we were able to demonstrate a negative relationship between the efficacy of a combined antiviral treatment with interferon-α plus ribavirin for chronic hepatitis C and the presence of non-organ-specific autoantibodies in univariate and multivariate analyses. However, studies in a larger number of patients should be performed before generalising our findings with regards to treatment decisions. Furthermore, future studies should include the measurement of peripheral immune parameters, i.e. cytokines and monocyte activation markers, as well as genetic studies in order to elucidate the pathophysiological association between the presence of autoantibodies and a reduced efficacy of combined antiviral treatment with interferon-α and ribavirin.
Competing interests
None declared.
Authors' contributions
HEW planned the study, wrote the study protocol, took care of study patients, and performed the analysis of the data. CS coordinated and performed the autoantibody detection. AG and CGD took care of the study patients. CG participated in the study desgin and coordination. JL was responsible for the analysis of the liver histologies. SM participated in the design and coordination of the study. FL planned the study, supervised the autoantibody detection, and performed the final analysis of the study. All authors contributed to the writing of the manuscript and approved the final version.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
This work was supported by grants from the Ministry of Science and Research (MSWF) of North-Rhine-Westphalia, the Federal Ministry of Education and Research (BMBF Network of Excellence for Viral Hepatitis Hep-Net), and Aachen University (START grants).
Contributor Information
Hermann E Wasmuth, Email: hwasmuth@ukaachen.de.
Christian Stolte, Email: C.Stolte@web.de.
Andreas Geier, Email: ageier@ukaachen.de.
Christoph G Dietrich, Email: christoph.dietrich@post.rwth-aachen.de.
Carsten Gartung, Email: cgartung@ukaachen.de.
Johann Lorenzen, Email: lorenzen@pat.rwth-aachen.de.
Siegfried Matern, Email: smatern@ukaachen.de.
Frank Lammert, Email: flammert@ukaachen.de.
References
- Manns MP, Rambusch EG. Autoimmunity and extrahepatic manifestations in hepatitis C virus infection. J Hepatol. 1999;31 Suppl 1:39–42. doi: 10.1016/S0168-8278(99)80372-9. [DOI] [PubMed] [Google Scholar]
- Zauli D, Cassani F, Bianchi FB. Auto-antibodies in hepatitis C. Biomed Pharmacother. 1999;53:234–241. doi: 10.1016/S0753-3322(99)80094-8. [DOI] [PubMed] [Google Scholar]
- Lopes EP, Silva AE, Sette Junior H, Guimaraes RX, Ferraz ML. Autoantibodies before, during and after administration of recombinant interferon-alpha for chronic viral hepatitis. Rev Inst Med Trop Sao Paulo. 1995;37:455–460. doi: 10.1590/s0036-46651995000500012. [DOI] [PubMed] [Google Scholar]
- Bayraktar Y, Bayraktar M, Gurakar A, Hassanein TI, Van Thiel DH. A comparison of the prevalence of autoantibodies in individuals with chronic hepatitis C and those with autoimmune hepatitis: the role of interferon in the development of autoimmune diseases. Hepatogastroenterology. 1997;44:417–425. [PubMed] [Google Scholar]
- Fang SH, Hwang LH, Chen DS, Chiang BL. Ribavirin enhancement of hepatitis C virus core antigen-specific type 1 T helper cell response correlates with the increased IL-12 level. J Hepatol. 2000;33:791–798. doi: 10.1016/S0168-8278(00)80312-8. [DOI] [PubMed] [Google Scholar]
- Tam RC, Pai B, Bard J, Lim C, Averett DR, Phan UT, Milovanovic T. Ribavirin polarizes human T cell responses towards a Type 1 cytokine profile. J Hepatol. 1999;30:376–382. doi: 10.1016/S0168-8278(99)80093-2. [DOI] [PubMed] [Google Scholar]
- Cassani F, Cataleta M, Valentini P, Muratori P, Giostra F, Francesconi R, Muratori L, Lenzi M, Bianchi G, Zauli D, Bianchi FB. Serum autoantibodies in chronic hepatitis C: comparison with autoimmune hepatitis and impact on the disease profile. Hepatology. 1997;26:561–566. doi: 10.1002/hep.510260305. [DOI] [PubMed] [Google Scholar]
- Noda K, Enomoto N, Arai K, Masuda E, Yamada Y, Suzuki K, Tanaka M, Yoshihara H. Induction of antinuclear antibody after interferon therapy in patients with type-C chronic hepatitis: its relation to the efficacy of therapy. Scand J Gastroenterol. 1996;31:716–722. doi: 10.3109/00365529609009156. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C 2002 (June 10-12, 2002) Gastroenterology. 2002;123:2082–2099. doi: 10.1053/gast.2002.1232082. [DOI] [PubMed] [Google Scholar]
- Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ, Donaldson PT, Eddleston AL, Fainboim L, Heathcote J, Homberg JC, Hoofnagle JH, Kakumu S, Krawitt EL, Mackay IR, MacSween RN, Maddrey WC, Manns MP, McFarlane IG, Meyer zum Buschenfelde KH, Zeniya M, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/S0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- Batts KP, Ludwig J. Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol. 1995;19:1409–1417. doi: 10.1097/00000478-199512000-00007. [DOI] [PubMed] [Google Scholar]
- Bottazzo GF, Florin-Christensen A, Fairfax A, Swana G, Doniach D, Groeschel-Stewart U. Classification of smooth muscle autoantibodies detected by immunofluorescence. J Clin Pathol. 1976;29:403–410. doi: 10.1136/jcp.29.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassani F, Bianchi FB, Lenzi M, Volta U, Pisi E. Immunomorphological characterisation of antinuclear antibodies in chronic liver disease. J Clin Pathol. 1985;38:801–805. doi: 10.1136/jcp.38.7.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazzolla G, Tortorella C, Fiore G, Fanelli M, Pisconti A, Antonaci S. Interleukin-12 p40/p70 ratio and in vivo responsiveness to IFN-alpha treatment in chronic hepatitis C. J Interferon Cytokine Res. 2001;21:453–461. doi: 10.1089/10799900152434303. [DOI] [PubMed] [Google Scholar]
- Fang SH, Lai MY, Hwang LH, Yang PM, Chen PJ, Chiang BL, Chen DS. Ribavirin enhances interferon-gamma levels in patients with chronic hepatitis C treated with interferon-alpha. J Biomed Sci. 2001;8:484–491. doi: 10.1159/000046170. [DOI] [PubMed] [Google Scholar]
- Lenzi M, Bellentani S, Saccoccio G, Muratori P, Masutti F, Muratori L, Cassani F, Bianchi FB, Tiribelli C. Prevalence of non-organ-specific autoantibodies and chronic liver disease in the general population: a nested case-control study of the Dionysos cohort. Gut. 1999;45:435–441. doi: 10.1136/gut.45.3.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimbert S, Johanet C, Bendjaballah F, Homberg JC, Poupon R, Beaugrand M. Antimitochondrial antibodies in patients with chronic hepatitis C. Liver. 1996;16:161–165. doi: 10.1111/j.1600-0676.1996.tb00722.x. [DOI] [PubMed] [Google Scholar]
- Dalekos GN, Tsianos EV. Anti-neutrophil antibodies in chronic viral hepatitis. J Hepatol. 1994;20:561. doi: 10.1016/s0168-8278(05)80508-2. [DOI] [PubMed] [Google Scholar]
- Dalekos GN, Makri E, Loges S, Obermayer-Straub P, Zachou K, Tsikrikas T, Schmidt E, Papadamou G, Manns MP. Increased incidence of anti-LKM autoantibodies in a consecutive cohort of hepatitis C patients from central Greece. Eur J Gastroenterol Hepatol. 2002;14:35–42. doi: 10.1097/00042737-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Vella FS, Orlando P, Attanasi F, Simone B, Mundo A, Lopalco P, Schiraldi O, Antonaci S. [Autoantibodies in chronic hepatitis C. Markers of autoimmunity or non-specific events?] Recenti Prog Med. 2001;92:107–112. [PubMed] [Google Scholar]
- Peng YC, Hsieh SC, Yang DY, Tung CF, Hu WH, Huang WN, Chen GH. Expression and clinical significance of antinuclear antibody in hepatitis C virus infection. J Clin Gastroenterol. 2001;33:402–406. doi: 10.1097/00004836-200111000-00012. [DOI] [PubMed] [Google Scholar]
- Muratori P, Muratori L, Stroffolini T, Pappas G, Terlizzi P, Ferrari R, Loffreda S, Cassani F, Rapicetta M, Guadagnino V, Bianchi FB, Lenzi M. Prevalence of non-organ specific autoantibodies in HCV-infected subjects in the general population. Clin Exp Immunol. 2003;131:118–121. doi: 10.1046/j.1365-2249.2003.02030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada M, Kang KB, Kinugasa A, Shintani S, Sawada K, Nishigami T, Shimoyama T. Does the presence of serum autoantibodies influence the responsiveness to interferon-alpha 2a treatment in chronic hepatitis C? Intern Med. 1997;36:248–254. doi: 10.2169/internalmedicine.36.248. [DOI] [PubMed] [Google Scholar]
- Carella C, Mazziotti G, Morisco F, Rotondi M, Cioffi M, Tuccillo C, Sorvillo F, Caporaso N, Amato G. The addition of ribavirin to interferon-alpha therapy in patients with hepatitis C virus-related chronic hepatitis does not modify the thyroid autoantibody pattern but increases the risk of developing hypothyroidism. Eur J Endocrinol. 2002;146:743–749. doi: 10.1530/eje.0.1460743. [DOI] [PubMed] [Google Scholar]
- McFarlane IG. Autoimmune hepatitis: diagnostic criteria, subclassifications, and clinical features. Clin Liver Dis. 2002;6:317–333. doi: 10.1016/s1089-3261(02)00019-3. [DOI] [PubMed] [Google Scholar]
- Strassburg CP, Manns MP. Autoantibodies and autoantigens in autoimmune hepatitis. Semin Liver Dis. 2002;22:339–352. doi: 10.1055/s-2002-35704. [DOI] [PubMed] [Google Scholar]
- Heathcote J. Variant syndromes of autoimmune hepatitis. Clin Liver Dis. 2002;6:381–396. doi: 10.1016/s1089-3261(02)00031-4. [DOI] [PubMed] [Google Scholar]


