Abstract
Posttraumatic stress disorder (PTSD) has been estimated to affect up to 18% of returning Operation Iraqi Freedom (OIF) veterans. Soldiers need to maintain constant vigilance to deal with unpredictable threats, and an unprecedented number of soldiers are surviving serious wounds. These risk factors are significant for development of PTSD; therefore, early and efficient intervention options must be identified and presented in a form acceptable to military personnel. This case report presents the results of treatment utilizing virtual reality exposure (VRE) therapy (virtual Iraq) to treat an OIF veteran with PTSD. Following brief VRE treatment, the veteran demonstrated improvement in PTSD symptoms as indicated by clinically and statistically significant changes in scores on the Clinician Administered PTSD Scale (CAPS; Blake et al., 1990) and the PTSD Symptom Scale Self-Report (PSS-SR; Foa, Riggs, Dancu, & Rothbaum, 1993). These results indicate preliminary promise for this treatment.
Posttraumatic stress disorder (PTSD) has been estimated to affect up to 18% of returning Operation Iraqi Freedom (OIF) veterans (Hoge et al., 2004). Due to the nature of this conflict, the war in Iraq presents unique and chronic stressors, including civilian threats such as guerilla warfare and terrorist actions (Hoge et al., 2004). Soldiers and Marines need to maintain constant vigilance to deal with unpredictable threats like roadside bombs, and to discern safe civilians from potential combatants (Litz, 2005). Additionally, an unprecedented number are now surviving serious wounds (Bilmes, 2007). Ninety-two percent of soldiers and Marines serving in Iraq reported being attacked or ambushed, 86% reported knowing someone who was seriously injured or killed, 70% reported seeing dead or seriously injured Americans, and 53% reported handling or uncovering human remains (Hoge et al., 2004). The above risk factors are significant for development of PTSD (Schnurr, Lunney, & Sengupta, 2004). Because this is a disorder which, once manifested, often results in a chronic course, early and efficient intervention options must be identified. Presenting treatment in a brief form that is acceptable to military personnel is also a priority, as concern about the stigma of treatment remains an issue which prevents soldiers from seeking the help they may require (e.g., Hoge et al., 2004).
Reviews of research and empirical evidence have found cognitive behavior therapy, including exposure therapy, to be a most effective treatment for PTSD (e.g., Bradley, Greene, Russ, Dutra, & Westen, 2005; Van Etten & Taylor, 1998). According to the emotional processing model proposed by Foa and Kozak (1986), the fear structure must be activated and modified to allow for the processes of habituation and extinction of fear to occur, which results in the feared stimuli no longer eliciting anxiety. A specific form of exposure therapy, virtual reality exposure (VRE) therapy, is a human–computer interaction medium in which patients can be immersed in a virtual environment which gives the user a sense of presence, and is proposed to effectively elicit the fear structure and aid the emotional processing of fears (Rothbaum et al., 1995). The virtual reality simulation allows for precise delivery and control of trauma-relevant exposure stimuli in a safe environment. Case reports and controlled studies of VRE have demonstrated reduction in fear of flying, heights, claustrophobia, and spiders (Rothbaum, 2006), as well as some success in treating combat veterans of the Vietnam era utilizing a virtual Vietnam environment (Rothbaum et al., 1999, Rothbaum, Hodges, Ready, Graap, & Alarcon, 2001).
A controlled study is currently underway to evaluate the effectiveness of VRE using a virtual Iraq for OIF veterans with combat-related PTSD. The current generation of military personnel may be familiar with simulation technology used primarily for training purposes by the military, and may be comfortable with participation in a virtual reality treatment approach as an alternative to traditional talk therapy. The virtual Iraq environment allows for the simultaneous delivery of trigger stimuli including visual, audio, and olfactory events to create an immersive and multimodal experience for the participant (Rizzo, Rothbaum, & Graap, 2007). The current case study documents the treatment response of the first OIF veteran at our site to receive treatment using the virtual Iraq environment.
METHOD
Participant
The veteran is a 29-year-old middle-class married Caucasian male combat engineer serving with the Georgia Army National Guard following 10 years of active duty service. He had recently spent a year-long tour in Iraq, and entered treatment approximately 6 months after his return. He is college-educated, has been employed full-time since his return, and has had no prior treatment. He reported ongoing intrusive recollections of military trauma that interfered with functioning at home and work, along with avoidance behaviors including difficulty driving. He reported experiencing poor concentration, mood irritability and angry outbursts, sleep disturbance with “cold sweats,” strong startle response, inability to relax, and hypervigilance. He endorsed weekend use of alcohol, which did not meet criteria according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV ; American Psychiatric Association [APA], 1994) for abuse.
Procedure
A preliminary telephone screening and interview was conducted during which the participant was informed about study details. Informed consent was obtained during the pretreatment evaluation conducted at Emory University by an independent assessor who also conducted the posttreatment assessment. A current PTSD diagnosis as determined by the Clinician Administered PTSD Scale (CAPS; Blake et al., 1990) was required for study inclusion. Identification of the index trauma to be addressed in treatment occurred at this time. The Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) was conducted to rule out the presence of exclusion criteria (current substance dependence, psychosis, mania, active suicidal ideation). The participant was asked to complete a battery of self-report scales including the Deployment Resilience and Recovery Inventory (DRRI; King, King, & Vogt, 2003), the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), the State-Trait Anxiety Inventory (STAI-S; Spielberger, 1983), the PTSD Symptom Scale Self-Report (PSS-SR; Foa, Riggs, Dancu, & Rothbaum, 1993), Quality of Life Inventory (QOLI; Frisch, 1993), Childhood Trauma Questionnaire (CTQ; Bernstein, Ahluvlia, Pogge, & Handelsman, 1997), and Clinical Global Impression (CGI; 1976), and was scheduled to return for the initial treatment session.
Apparatus
During the VRE sessions, the participant wore an eMagin Z800 head-mounted display (HMD; eMagin Corp., Bellevue, WA) that included separate display screens for each eye, integrated head-tracking, and stereo earphones. The participant was presented with a computer-generated view of a Virtual Iraq environment that changed in a natural way with head and body motion. The Virtual Iraq software and environment models (Rizzo et al., 2007) were constructed with design input from OIF veterans. A handheld controller allowed the participant to move forward within the environment at his own pace. In the virtual environment, the participant could drive a Humvee down a desert highway either alone or in a convoy or navigate through “Iraq-like” city scenes. Trigger stimulus options included sounds of weapons fire, explosions, incoming mortars, helicopter flyovers, vehicle noise, wind, human voices, and radio, and visual stimuli such as night vision, wounded civilians and combatants, and wrecked vehicles. Olfactory stimuli delivered via a scent palette in an airtight chamber filled with compressed air included such scents as burning rubber, diesel fuel, weapons fire, and spices. Tactile stimuli (i.e., vibration) were delivered through a raised floor platform with a subwoofer attached driven by an audio amplifier. The therapist used an interface panel to deliver and control trigger stimulus presentations via a separate standard PC that is network-linked to the PC that runs the simulation. While the HMD occludes real-world stimuli, the therapist communicated with the participant via a head-mounted microphone and earphones.
Treatment
Treatment was delivered in four, 90-minute individual sessions conducted once weekly over 4 weeks. Session 1 was devoted to information gathering and elaboration of the index trauma, explaining treatment rationale, education around common reactions to trauma, and teaching a brief breathing relaxation method. The index trauma had been previously identified during the pretreatment assessment, and was defined as the trauma memory which was selected by the participant as being most intrusive and/or distressing. During session 1, specific details of the index trauma event were elicited, including location, time of day, weather, significant events (ambush, explosion, medevac), and other stimuli such as particular sounds (AK-47 gunfire) and smells (diesel fuel, cordite), which were components of the memory. This elaboration served to inform the therapist around appropriate cues to be introduced during VRE sessions. The participant was informed that the identified memory would be the focus of the treatment, and that he would be asked to repeatedly recount it. This was explained in the context of education about imaginal exposure therapy as a vehicle to confront feared memories in a safe and controlled environment to facilitate extinction of fear and processing of the memory. Concerns regarding the treatment were addressed at this time. At the completion of this session, the participant indicated on the 0–8 Likert scale of the Expectancy of Therapeutic Outcome questionnaire (Foa et al., 1991) that he felt the treatment was logical (7), would be successful in reducing trauma-related symptoms (7), would be successful in reducing other personal problems (7), and he would be confident in recommending this treatment to a friend with similar problems (7).
During the VRE sessions, the participant was exposed to the desert convoy virtual environment, which matched his index trauma experience. The trauma involved an attack on his convoy, which resulted in significant physical injury to two soldiers. Average time spent in the VR apparatus was approximately 50 minutes per session (25 minutes for each of two detailed recountings of the trauma memory). During the first VRE session, simply being in the Humvee and feeling the vibration, and moving ahead along the road lined with telephone poles, triggered the identified trauma. Subjective units of distress (SUDS) ratings ranging from 0–100 were elicited from the patient every 5 minutes during exposure. The initial recounting of the memory lacked cohesion, and the patient was confused about details, including who was driving the vehicle at critical points, and the order in which events occurred. During the processing that occurred with the therapist after each exposure, he reported that he had recalled scenarios within the memory that he had forgotten until the session. For example, a powerful scene that he recalled while recounting the memory in the VR apparatus involved seeing himself in a mirror immediately after the traumatic event, still holding his weapon in hand, covered with dirt and blood, and questioning the reality of what had just occurred. Processing involved discussion of such reactions and events identified by him and/or the therapist as being significant to facilitate integration and emotional processing of the experience. Homework was not assigned between sessions.
Sessions 3 and 4 consisted of repetition of the traumatic memory with gradual addition of cues. Cues included, for example, helicopter flyover at the point in the memory when the medevac arrived, and background radio communication. More intense cues such as explosions and gunfire were introduced by the therapist as sessions progressed; in this way the therapy experience was customized to meet the individual needs of the participant via systematic real-time delivery and control of trigger stimuli in the environment (Rizzo et al., 2007). Expression of affect by the participant remained relatively strong over the course of treatment sessions, and it was notable that the valence shifted over repetitions from horror, grief, and guilt to include feelings of admiration and pride around the resourcefulness and bravery of fellow soldiers, and acceptance around actions taken in time of war. The recounted story evolved into a flowing and cohesive narrative over time, with access to new details such as names of individuals and roads, and specific times of day. Anxiety reduction was indicated within sessions by decreased level of apparent distress and in reported SUDS ratings (see Table 1). The SUDS ratings did not consistently indicate substantial decreases within sessions; however, according to Van Minnen and Foa (2006), within-session habituation may not be a necessary condition for successful treatment of PTSD. It is important to note also that the intensity of the presented stimuli increased across sessions, and SUDS ratings likely reflected these additions and changes. Full assessments were conducted at pretreatment and posttreatment, and brief self-report measures were completed prior to each VRE session. The participant received $25 for completing the pretreatment and posttreatment assessments.
Table 1.
Subjective Units of Distress (SUDS) Ratings (1–100) Across Virtual Reality Exposure Sessions
| Session number |
Recounting of trauma memory |
BL | Minutes in session | ||||
|---|---|---|---|---|---|---|---|
| 5 min | 10 min | 15 min | 20 min | 25 min | |||
| 2 | 1 | 80 | 100 | 100 | 85 | 95 | 65 |
| 2 | 90 | 100 | 70 | 90 | 70 | 65 | |
| 3 | 1 | 75 | 98 | 700 | 90 | 80 | 60 |
| 2 | 70 | 90 | 90 | 90 | 60 | 60 | |
| 4 | 1 | 80 | 90 | 80 | 75 | 70 | 60 |
| 2 | 85 | 80 | 80 | 75 | 65 | 60 | |
Note. BL = Baseline, wearing head-mounted display. SUDS ratings: 0 = absence of anxiety, 100 = highest subjective level of anxiety.
RESULTS
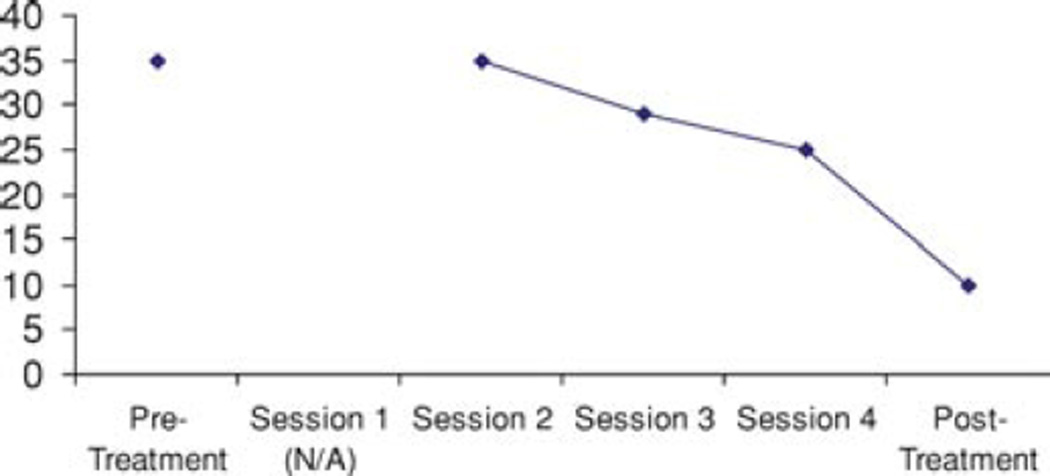
Results from pretreatment to posttreatment on individual measures can be found in Table 2. The CAPS score decreased by 56%, from a total score (106) in the extreme range of >80 to a total score (47) in the moderate/threshold range of 40 to 59. The PSS-SR score decreased from a total of 35 to 10 (See Figure 1). Jacobson’s Reliable Change Index (Jacobson & Truax, 1991) was employed to evaluate treatment change on these two major outcome measures. For the CAPS (test-retest reliability = .63 and SD = 33.39 in the original CAPS PTSD sample), calculated standard error of the difference between the two administrations is 28.72; reliable change is indicated by the CAPS total decrease of 59 points from pre- to posttreatment (p < .05). For the PSS-SR (test-retest reliability = .74 and SD & equals; 10.24 in a PTSD sample), calculated standard error of the difference between the two administrations is 7.38; reliable change is indicated by the PSS-SR decrease of 25 points (p < .01). These results indicate observed changes to be both clinically and statistically significant.
Table 2.
Pre- to Posttreatment Assessment Scores
| Measure | Pretreatment | Posttreatment |
|---|---|---|
| CAPS Total | 106 | 47 |
| CAPS Reexperiencing | 33 | 16 |
| CAPS Avoidance | 39 | 11 |
| CAPS Hyperarousal | 34 | 20 |
| PSS-SR | 35 | 10 |
| BDI | 13 | 11 |
| STAI-S | 53 | 39 |
| CGI Severity | 4 | 2 |
| CGI Improve | N/A | 1 |
| CGI Self-rating | 3 | 2 |
Note. Decrease in score indicates improvement. CAPS = Clinician-Administered PTSD Scale; PSS-SR = PTSD Symptom Scale-Self Report; BDI = Beck Depression Inventory; STAI-S = State-Trait Anxiety Inventory–State; CGI = Clinical Global Impressions.
Figure 1.
PTSD Symptom Scale-Self Report (PSS-SR) scores across sessions.
DISCUSSION
Short-term virtual reality exposure treatment of PTSD in an OIF veteran resulted in a substantial drop in the patient’s self-reported PTSD symptoms. This participant reported feeling comfortable with the technology utilized in this form of treatment and found the treatment to be logical and credible. Although the participant still met CAPS criteria for a PTSD diagnosis at posttreatment, he anecdotally reported experiencing improvement in functioning in many areas of his life as a result of treatment, including increased ability to concentrate at work, increased communication with spouse, decreased anhedonia, and decreased avoidance of friends and fellow soldiers. He also discussed feeling that he no longer needed to “keep thinking about” the identified trauma. The limitations of an uncontrolled case report are obvious; nevertheless, this outcome provides preliminary promise for the use of virtual reality exposure therapy with OIF veterans with PTSD.
Acknowledgments
This study was supported by NIMH Grant #R01-MH070880 awarded to Dr. Rothbaum. Thanks to Jarrell Pair, USC Institute for Creative Technologies, for his contribution to the creation of the Virtual Iraq environment.
Footnotes
Disclosure Statement: Dr. Rothbaum is a consultant to and owns equity in Virtually Better, Inc., which creates virtual environments; however, Virtually Better did not create the Virtual Iraq environment tested in this study. The terms of this arrangement have been reviewed and approved by Emory University and Georgia Institute of Technology in accordance with their conflict of interest policies.
Contributor Information
Maryrose Gerardi, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Barbara Olasov Rothbaum, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Kerry Ressler, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Mary Heekin, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA.
Albert Rizzo, Institute for Creative Technologies, University of Southern California, Marina del Ray, CA.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.) Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bilmes L. Soldiers returning from Iraq and Afghanistan: The long-term costs of providing veterans medical care and disability benefits. Paper presented at the Allied Social Sciences Meetings; Chicago, IL. 2007. Jan, [Google Scholar]
- Blake DD, Weathers F, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;13:187–188. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Guy W, editor. Clinical Global Impressions. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: U.S. Department of Health, Education and Welfare; 1976. (DHEW Publication No. [ADM], 76–338.). [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Frisch MB. The Quality of Life Inventory: A cognitive-behavioral tool for complete problem assessment, treatment planning, and outcome evaluation. Behavior Therapist. 1993;16:42–44. [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Jacobson MS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Vogt DS. Manual for the Deployment Risk and Resilience Inventory (DRRI): A collection of measures for studying deployment-related experiences of military veterans. Boston: National Center for PTSD; 2003. [Google Scholar]
- Litz BT. A brief primer on the mental health impact of the wars in Afghanistan and Iraq: A National Center for PTSD fact sheet. Boston: National Center for PTSD; 2005. [Google Scholar]
- Rizzo AA, Rothbaum BO, Graap K. Virtual reality applications for combat-related posttraumatic stress disorder. In: Figley CR, Nash WP, editors. Combat stress injury: Theory, research and management. New York: Routledge; 2007. pp. 183–204. [Google Scholar]
- Rothbaum BO, editor. Pathological anxiety: Emotional processing in etiology and treatment. New York: Guilford Press; 2006. [Google Scholar]
- Rothbaum BO, Hodges L, Alarcon R, Ready D, Shahar F, Graap K, et al. Virtual reality exposure therapy for PTSD Vietnam Veterans: A case study. Journal of Traumatic Stress. 1999;12:263–271. doi: 10.1023/A:1024772308758. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Hodges LF, Kooper R, Opdyke D, Williford JS, North M. Effectiveness of computer-generated (virtual reality) graded exposure in the treatment of acrophobia. American Journal of Psychiatry. 1995;152:626–628. doi: 10.1176/ajp.152.4.626. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Hodges LF, Ready D, Graap K, Alarcon RD. Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62:617–622. doi: 10.4088/jcp.v62n0808. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:85–95. doi: 10.1023/B:JOTS.0000022614.21794.f4. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini Inter-national Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Van Etten ML, Taylor S. Comparative efficacy of treatments of posttraumatic stress disorder: An empirical review. Journal of the American Medical Association. 1998;268:633–638. [Google Scholar]
- Van Minnen A, Foa EB. The effect of imaginal exposure length on outcome of treatment for PTSD. Journal of Traumatic Stress. 2006;19:427–438. doi: 10.1002/jts.20146. [DOI] [PubMed] [Google Scholar]