Abstract
Background:
There are limited data about Iyengar Yoga and EMG biofeedback in knee OA, although the efficacy of EMG biofeedback in the rehabilitation of patients with quadriceps muscle weakness secondary to immobilization, contracture, and joint surgery has been well established.
Materials and Methods:
Thirty subjects who have fulfilled inclusion and exclusion criteria were selected and divided into two groups (Group A and B). Both the groups were treated with EMG biofeedback, knee muscle strengthening exercises, and TENS. Group A received additionally Iyengar Yoga for 8 weeks. Both groups were evaluated by Visual Analog Scale and Modified WOMAC–Western Ontario McMaster Universities Scale.
Results:
Patients in both groups experienced significant reduction in pain and improvement in functional ability. In VAS scale Group A showed reduction of 56.83% (P = 0.001) when compared with Group B 38.15% (P ≤ 0.001). In modified WOMAC Scale, Group A showed reduction of 59.21% (P = 0.001) when compared with Group B 34.08% (P = 0.001).
Conclusion:
Adding Iyengar Yoga along with conventional therapy provides better results in chronic unilateral knee osteoarthritis in terms of pain and functional disability.
Keywords: Chronic knee osteoarthritis, EMG biofeedback, Iyengar Yoga, TENS
INTRODUCTION
Osteoarthritis (OA) is the most common form of arthritis characterized pathologically by both focal loss of articular cartilage and marginal and central new bone formation.[1] Although biomechanical and biochemical processes occur mainly on the articular cartilage, the entire joint, including subchondral bone, synovial membrane, joint capsule, and ligaments, are affected in OA.[2] Cytokines (IL-1 and TNF-b) activate enzymes causing proteolytic digestion of cartilage and tissue growth factor and insulin growth factor causes cartilage synthesis. When catabolism exceeds cartilage synthesis, OA develops.[3] After few years, the reparative process exhausted and this leaves cartilage degradation unopposed leading to progressive OA, which results into inflammation, pain, and structural damage leading to loss of function.[4]
OA disease causes pain, swelling, and loss of motion of the joint due to the bones under the cartilage rubbing together.[5] Endogenous factors such as age, sex, hereditary, post-menopausal changes, exogenous factors such as macro trauma, lifestyle factors such as (alcohol, tobacco), obesity,[6] or overweight, repetitive joint surgery leads to OA.
Pharmacological drugs such as non-opioid analgesics, opioid and topical analgesics, NSAID, hyaluronic acid injections, and intra-articular steroid injections are given in the initial stages. Surgical procedures such as Cartilage Repair Techniques, Osteotomy, and TKA can also performed in later stages.[7] Various interventions such as Acupuncture, LASER, TENS, Ultrasound, Hydrotherapy, and Manual therapy techniques can be applied for acute and chronic stages and Braces and orthosis are prescribed for the supportive purposes.[8]
Yoga is one intervention which has off late been considered as a treatment for OA. Of the various schools of Yoga, Iyengar Yoga is a form of Hatha Yoga created by BKS Iyengar and stresses strength, balance, breathing, and the alignment of the body. It allows the use of various assistive devices such as chairs or blocks to aid balance and straps to facilitate stretching. It can be performed by anyone at any age and level of fitness. Because the body can be supported and balanced by these techniques, beginners can achieve many postures that would otherwise be literally, out of reach.[9]
Another intervention which is frequently used in the treatment of OA is EMG biofeedback. EMG biofeedback is generally used to provide muscle re-education and to regain muscle strength in cases of muscle weakness.[10] A patient's compliance to the exercise program can be improved by addition of EMG biofeedback to the rehabilitation programs.[11] EMG biofeedback assisted exercise programs are suggested as they increase compliance with exercise and motivation of patients.[12]
Though individual effects of different treatment modalities are discussed in various studies, there is lack of evidence in understanding the combined effect of Iyengar Yoga with physiotherapy methods. Thus the purpose of the study is to find out if there is any additional effect of Iyengar Yoga when combined with conventional physiotherapy for Chronic Unilateral Knee OA.
MATERIALS AND METHODS
Design and sample
Thirty (n = 30) subjects between 45 and 70 years of age, having symptomatic OA knee for at least 6 months before study entry and who were not currently participating in any exercise program, were divided using systematic sampling into two groups (Groups A and B). Both male and female pparticipants who had grade 2 or 3 as criteria of Kellgren and Lawrence with at least two of the following symptoms: (1) stiffness 30 minutes, (2) crepitus, bony tenderness, (3) bony enlargement, or (4) absence of palpable warmth were included in the study. Patients diagnosed as a case of unilateral knee OA, having ≤ 6 cm in Visual Analog Scale (VAS), with symptoms of locking or instability, secondary OA, trauma during last 3 months, and axial deviation >15° in valgus/varus were excluded from the study. Patients having diseases of other systems that could have created difficulty during the study follow-up, chronic use of a knee brace, cane, or walker; or a prior diagnosis of inflammatory arthritis, severe OA (stage 4 according to Kellegren and Lawrence radiological classification) were also not included in the study.
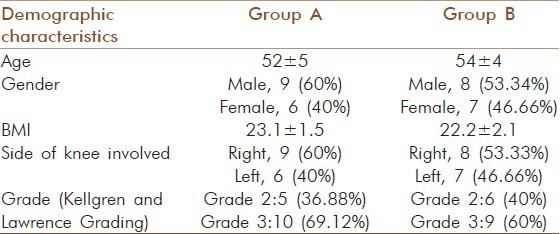
The first patient was allocated to Group A and second patient was allocated to Group B accordingly, thus Group A (n = 15; Iyengar yoga, EMG biofeedback, Knee strengthening exercise and TENS) and Group B (n = 15; EMG biofeedback, Knee strengthening exercise and TENS). The sociodemographic characteristics of the patients are provided in Table 1.
Table 1.
Demographic details of Group-A and Group B
The study has been approved by the institutional scientific committee and institutional ethical committee. It was conducted at the outpatient physiotherapy department of C.U. Shah Physiotherapy College. All the participants completed all the sessions of intervention (no drop outs). During the treatment sessions none of the patient's experienced any adverse effects.
Outcome measures
The VAS was used to measure the subject's current level of pain intensity. VAS involves a 10-cm horizontal line with No pain anchored at the left end and pain as bad as it could be anchored at the right end. The patients were asked to place a mark on the line that represented the severity of his or her pain at the moment. The Modified WOMAC version includes 24 questions. This list contains some sentences that people have used to describe themselves when they have trouble with their knee. Total score for WOMAC is 96. Out of which there is maximum 10 score for pain, 8 score for stiffness, and 68 score for physical function. It is a reliable and valid instrument for measuring the disability in chronic unilateral knee OA patients.[13] The above outcome measures were assessed at baseline and after 8 weeks of intervention in Group A and Group B.
Interventions
Iyengar yoga techniques
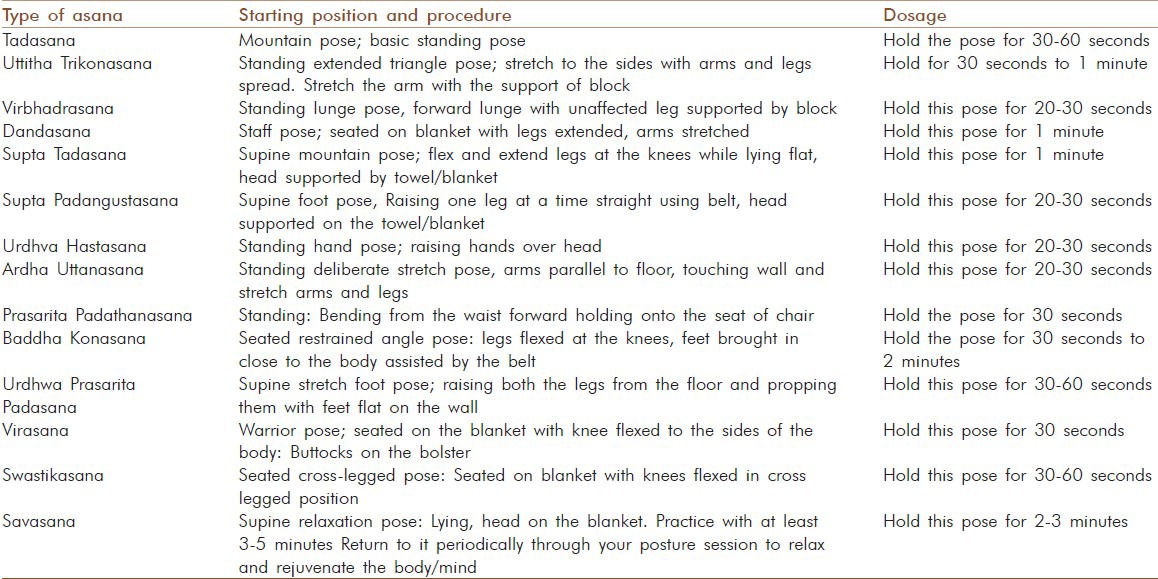
3 times/week for 8 weeks, 1 session 90 minutes.[14]
In this Iyengar Yoga, assistive devices such as blocks, belts, and blankets were used to support the parts of the body while perform the asana. Postures were performed in standing, sitting, and supine positions. All participants were encouraged to stretch as fully as possible while not exceeding the limits of their comfort and were encouraged to use props as needed. All the asanas were performed for three repetitions/sessions. List of asanas performed in modified Iyengar yoga is provided in Table 2.
Table 2.
Types of yoga applied and its dosage
EMG Biofeedback (3 times in a week)
For 8 weeks with 45 duration of each session was provided for the quadriceps muscles. Channels I and II were attached to Vastus Medialis and Lateralis muscles, respectively. Two active surface electrodes were placed parallel to the muscle fibers and inactive ones were placed at equal distances far from the two active electrodes. The ground electrodes were placed between active and inactive electrodes. This equipment shows muscle activity obtained during exercises with visual and auditory signals, increasing with increments in muscle activity. Thus, the patient got a feedback about how much muscle contractions were made during exercise.
Knee strengthening exercises
3 times/week, 3 sets of 10–15 repetitions for 8 weeks.
Emphasis was to build muscle strength using both legs. Progress was according to the Progressive resisted Exercise (PRE) principle. The Basic Program Exercises that were provided were straight leg raise, short-arc lift, side lying abduction, standing hamstring curl, and toe raise.
TENS: (3 times/week)
Frequency, 0–100 Hz; Pulse duration, 50 ms; size of electrode, 5 × 7 cm 2 electrode, the lateral and medial knee; Treatment time, 20 minutes.
Data analysis
The obtained data were analysed with SPSS-16 for Inter and Intra group comparisons. Intergroup analysis was done using Mann–Whitney U test and Intragroup analysis was done using Wilcoxon sign rank test. P values <0.05 were accepted as indicating significant differences between pre-and post-intervention data.
RESULTS
The baseline values of VAS (P = 0.233) and Modified WOMAC score (P = 0.245) showed no significant difference (P > 0.05) between in either of the Groups A and B suggesting that sample assignment was successful.
Compared to the baseline values, Group A showed a more reduced VAS (56.83%) and Modified WOMAC (59.21%) score than Group B (VAS 38.15% and Modified WOMAC 34.08%) after 8 weeks of intervention. The pre- and post-intervention ratings of VAS and Modified WOMAC score showed a statistically significant reduction of pain intensity and functional disability in Group A compared with Group B (P < 0.05) shown in Table 3.
Table 3.
Mann whitney of visual analog scale–pain and Western ontario McMaster universities scale
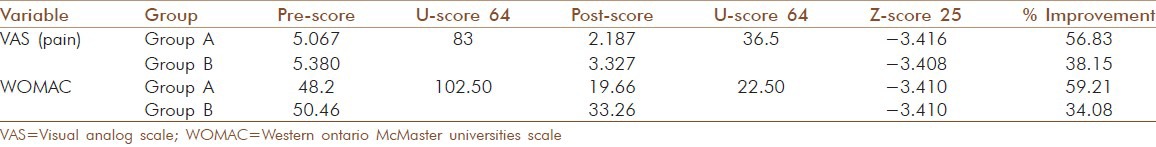
Statistical analysis also showed 56.83% improvement in Group A and 38.15% improvement in Group B. When comparing the percentage of reduction of pain intensity between Groups A and B, Group A showed more reduction in pain intensity at the end of the treatment (after 8 weeks) when compared with Group B. Further with respect to reduction in functional disability, Group A showed 59.21% improvement, whereas Group B showed only 34.08% improvement at the end of the treatment (after 8 weeks).
DISCUSSION
The above results depict that an addition of Iyengar Yoga combined with EMG biofeedback, knee muscle strengthening exercises, and TENS is effective in reducing pain and functional disability. This result validates those of earlier studies that have depicted that yoga provides a safe and feasible exercise option for yoga-naive, obese patients over ≥ 50 years of age and offers potential reductions in pain and disability caused by OA.[14]
In yoga, specific asanas that strengthen the quadriceps and other muscles relieve physical stress on the knee joint. Different postures focus on flexibility and increased blood flow, presumably by aligning joints, including the ankles, knees, and hips. Standing postures strengthen and align bones and muscles, particularly of the lower extremities. Stretching is achieved by bending and twisting. Traction and active alignment from the use of one's own muscles, if tolerated, is preferable to passive traction by the use of external postures. Inverted postures rest the legs and help the nervous system function.[15]
Further, the cellular effects of mechanical and fluid pressure on structures such as cartilage suggest that yoga postures might alter joint function. Low levels of intermittent fluid pressure, as occurring during joint distraction, have been shown in vitro to decrease production of catabolic cytokines, such as interleukin-1 and tumor necrosis factor-α.[16] In experimental settings, joint motion preserves cartilage that can be lost by immobilization.[17] Correctly supervised yoga may be one way to provide the motion and forces on joints needed to preserve integrity.
Yoga may also benefit those with knee OA via quadriceps strengthening and general stretching. Quadriceps strengthening has long been noted to be of importance in the development of knee OA, and there is ample evidence that muscle-strengthening exercises improve pain reduction and functional disability.[18] Asanas using assistive devices emphasize stretching thus may be of particular benefit in treating OA. In this context it can be stated that Iyengar Yoga could be best-suited yoga style for treatment of OA.
The main limitation of this study was its small sample size. A larger sample would be required to validate and generalize the results of this study to the population. Further the design did not support long-term follow-up of the patients after the study, to understand if they continued practicing yoga and deriving benefits from its practice even after completion of the study.
CONCLUSION
Iyengar Yoga as an add on treatment in combination with EMG biofeedback, knee muscle strengthening exercise, and TENS can be used as choice viable of treatment for patient with chronic unilateral Tibiofemoral OA in terms of pain and functional disability.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Tok F, Aydemir K, Peker F, Safaz I, Ali M. Germany: Springer-Verlag; 2009. The effects of electrical stimulation combined with continuous passive motion versus isometric exercise on symptoms, functional capacity, quality of life and balance in knee osteoarthritis: Randomized clinical trial. [DOI] [PubMed] [Google Scholar]
- 2.Burkhardt CS. Chronic pain. Nurs Clin North Am. 1990;25:863–70. [PubMed] [Google Scholar]
- 3.Pelletier JP, DiBattista JA, Roughley P, McCollum R, Martel-Pelletier J. Cytokines and inflammation in cartilage degradation. Rheum Dis Clin North Am. 1993;19:545–68. [PubMed] [Google Scholar]
- 4.Dicesare PE, Abramson SB. Pathogenesis of osteoarthritis. In: Harris ED, Budd RC, Genovese MC, editors. Kelley's textbook of Rheumatology. 7th ed. Vol. 2. Netherlands: Elsevier Saunders; 2005. pp. 1493–513. [Google Scholar]
- 5.Doherty M, Jones A, Cawston T. Osteoarthritis. In: Isenberg DA, editor. Oxford textbook of rheumatology. 3rd ed. Oxford: Oxford University Press; 2004. pp. 1091–118. [Google Scholar]
- 6.Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in general population The Chingford Study. J Rheumatol. 1993;20:331–5. [PubMed] [Google Scholar]
- 7.Buly RL, Sculco TP. Recent advances in total knee replacement surgery. Curr Opin Rheumatol. 1995;7:107–113. doi: 10.1097/00002281-199503000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese adults with knee osteoarthritis; the arthritis, diet and activity promotion trial. Arthritis Rheum. 2004;50:1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 9.New York: Schocken Books; 1979. BKS Iyengar Light on Yoga. [Google Scholar]
- 10.Ingersoll CD, Knight KL. Patellar location changes following EMG biofeedback or progressive resistive exercises. Med Sci Sports Exer. 1991;23:1122–78. [PubMed] [Google Scholar]
- 11.Krebs DE. Clinical electromyographic feedback following meniscectomy. A multiple regression experimental analysis. Phys Ther. 1981;61:1017–21. doi: 10.1093/ptj/61.7.1017. [DOI] [PubMed] [Google Scholar]
- 12.Levitt R, Deisinger JA, Remondet Wall J, Ford L, Cassisi JE. EMG feedback assisted postoperative rehabilitation of minor arthroscopic knee surgeries. J Sports Med Phys Fitness. 1995;35:218–23. [PubMed] [Google Scholar]
- 13.Roorda L, Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthrits of the hip and knee. Clin Rheumatol. 1986;5:231–41. doi: 10.1007/BF02032362. [DOI] [PubMed] [Google Scholar]
- 14.Kolasinski SL, Garfinkel M, Tsai AG, Matz W, Van Dyke A, Schumacher HR. Iyengar yoga for treating symptoms of osteoarthritis of the knees: A pilot study. J Altern Complement Med. 2000;11:689–93. doi: 10.1089/acm.2005.11.689. [DOI] [PubMed] [Google Scholar]
- 15.Raman K. Chennai, India: Eastwest Books; 1998. A matter of health. Integration of yoga and Western medicine for prevention and cure. [Google Scholar]
- 16.van Valburg AA, Van Roy HL, Lafeber FP, Bijlsma JW. Beneficial effects of intermittent fluid pressure of low physiological magnitude on cartilage and inflammation in osteoarthritis. An in vitro study. J Rheumatol. 1998;25:515–20. [PubMed] [Google Scholar]
- 17.Fam AG, Schumacher HR, Jr, Clayburne G, Villanueva T, Baker D, Jimenez SA. Effect of joint motion on experimental calcium pyrophosphate dihydrate crystal induced arthritis. J Rheumatol. 1990;17:644–55. [PubMed] [Google Scholar]
- 18.Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, et al. Reduced quadriceps strength relative to body weight: A risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41:1951–9. doi: 10.1002/1529-0131(199811)41:11<1951::AID-ART9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]


