Abstract
Now-a-days reproductive health problems along with infertility in male is very often observed. Various Assisted Reproductive Technologies have been introduced to solve the problem, but common people cannot afford the cost of such procedures. Various ayurvedic and other alternative medicines, along with regular yoga practice are proven to be not only effective to enhance the reproductive health in men to produce a successful pregnancy, but also to regulate sexual desire in men who practice celibacy. Yoga is reported to reduce stress and anxiety, improve autonomic functions by triggering neurohormonal mechanisms by the suppression of sympathetic activity, and even, today, several reports suggested regular yoga practice from childhood is beneficial for reproductive health. In this regard the present review is aimed to provide all the necessary information regarding the effectiveness of yoga practice to have a better reproductive health and to prevent infertility.
Keywords: Anxiety, cancer, infertility, sperm count, stress, yoga
INTRODUCTION
Infertility and problems in conception have been a concern through the ages. Infertility in men is the inability to fertilize mature ova after mating with female partner, while, in women it is the inability to naturally conceive a child or to carry a pregnancy to full term. There are many reasons why a couple may not be able to conceive, or may not be competent to conceive without medical aid. Infertility has its impact on about 15% of couples of reproductive age, with nearly half of the cases resulting from male factor infertility.[1] The chance of getting pregnant in each menstrual cycle is very high and it has been reported that eight out of every ten women trying for a baby will fall pregnant within the first 6 months. Women who become pregnant without any medical assistance generally do so within 8 months of trying.[2] It is common for couples to seek help or advice if there is difficulty in conceiving. The point at which they may want to seek out help will depend on various aspects, for example, if they are over 35 years of age or if they have any worrying symptoms, the couple should strive for help after about 6 months of trying.[3] In men, various factors may contribute in infertility, like lifestyle, obesity, smoking, or alcohol consumption, including exposure various occupational and environmental metals. These factors result in decreased quality of sperm, by affecting its structure, development, count, and motility.[4]
Since the beginning of time, humans have employed rituals, folk medicines, and various techniques performed by shamans and other healers or revered members of their culture in an effort to potentiate their ability to conceive. Recently, complementary or alternative therapy is often employed for the same perseverance with the intent to enhance the probability of conception and augment a healthy pregnancy with a positive outcome. What may be considered CAM in one culture or country may be part of the traditional health system in another, for example, yoga, which is considered CAM therapy in the United States, has been part of the health system in India for more than 7000 years.[5] CAM therapy is often used to foster wellness, improve the results of traditional therapies, and in the advancement the quality of life. Yoga is being used by a growing number of youth and adults as a means of improving overall health and fitness. There is also a progressive trend toward use of yoga as a mind-body CAM intervention to improve specific physical and mental health conditions. There are some information about the beneficial impact of yoga practice on reproductive health and fertility among common people, but there is no proper evidence-based literature available, which can throw some light on its impact on reproductive health. To provide researchers and clinicians with therapeutically useful information about yoga, the evidence evaluating yoga as an effective intervention for couples suffering with the problems of infertility, is reviewed and summarized. A brief overview of common causes of infertility today and its yoga therapy is presented in this review.
INFERTILITY IN MEN: COMMON ORIGINS
Lifestyle and spermatogenesis in adult male
Several studies in laboratory animals have examined whether exposure in adulthood to a wide range of chemicals can impair spermatogenesis. This literature is too vast and diverse to consider. In contrast, it is well recognized that demonstration of cause and effect in human studies is more problematic than in laboratory animal studies as laboratory animals are very much less variable in their phenotype and spermatogenesis profile in comparison to the huge variation seen among normal adult human males.[6] In addition, human males are exposed in reality to a complex mixture of environmental chemicals that may cause interactive effects on spermatogenesis.[7,8] Even when considering exposure to one environmental chemical, men will be unevenly exposed, in contrast to the situation in experimental animals where they are exposed to a constant dose under test circumstances and there is small variation between animals in spermatogenesis. Therefore, it is not a similar comparison; accordingly, a different level of proof is probably required to establish cause and effect. Furthermore, there are important differences between species in the set-up and organization of spermatogenesis that may affect vulnerability of the testis to disruption by exogenous factors.[9]
Obesity
Obesity is an important lifestyle-dependent factor that adversely affects spermatogenesis; as 10-30% of adult men in Western countries are now obese, it is likely that this will have an increasing effect on male fertility.[10,11] Several studies have shown up to a three-fold higher incidence of obesity in infertile men than in those with normal semen quality.[12,13] A BMI of >25 is associated with an average 25% reduction in sperm count and motility.[14,15,16] The most potent evidence describing the association is that the alterations in sperm production are secondary to altered hormone changes, i.e., reduced blood testosterone levels.[11,17] Patients with such hormonal profiles often show reduced blood levels of LH and FSH, when an increase might be expected in spite of reduced testosterone levels, one such interpretation is that there is declined intratesticular testosterone levels and thus reduced androgen drive to spermatogenesis.[18,19] However, there may also be intratesticular effects that are unrelated to altered gonadotrophin levels as the reduction in inhibin B levels in obese men is disproportionately larger than the change in FSH levels, suggesting there may be direct effects of the increased obesity on sertoli function in turn permanently lowers sperm counts.[13,14,15,20]
Another explanation for reduced spermatogenesis in obese men could be deposition of fat around the scrotal blood vessels, leading to impaired blood cooling and elevated testicular temperature.[21] Another potential argument to explain reduced sperm counts in obese men is that they accumulate increased amounts of toxicants in their adipose tissue because many of the persistent environmental chemicals are lipophilic.[13,22] Nevertheless, considering the high prevalence of obesity among young men today and the equally high prevalence of low sperm counts, it is possible that the obesity epidemic may be having an impact on spermatogenesis among young men, and it may also render such individuals more susceptible to damaging effects by other lifestyle or environmental exposures. For certain, obesity looks set to play an important role in determining the hormonal and fertility profile of Western men over the coming decades.[11,14,15]
Smoking, alcohol and drugs
Smoking and alcohol consumption usually come top of the list among the Western lifestyle factors commonly suspected to have adverse impacts on health. There is little evidence that either of these has a major impact on spermatogenesis, although meta-analysis supports the view that smoking has a small negative impact.[23,24] Physiologically, the testis is considered to be poised on the brink of hypoxia.[25,26] Therefore, factors that compromise delivery of oxygen to the testis would be suspected to have a detrimental effect. The negative impact of smoking on sperm counts in men is therefore consistent with this thinking. However, in comparison with the fairly dramatic decrease (up to 40%) in sperm counts that is induced in sons by maternal smoking in pregnancy, the reduction (10-17%) in sperm counts in adult men who smoke heavily[27] is modest, and in many individual studies no significant effects were found.[23,28] Although interference with oxygen supply is an obvious mechanism via which smoking could reduce spermatogenesis, other mechanisms may also operate, including exposure to cadmium and activation of the Ah receptor, as is thought to occur with maternal smoking in pregnancy.
Most studies that included alcohol as a point of investigation have failed to show a significant impact on sperm counts, at least among those with moderate alcohol consumption.[28,29] In contrast, in chronic alcoholics, there is good evidence for impairment of spermatogenesis and reductions in sperm counts and testosterone levels.[30,31] These effects work via endogenous cannabinoid-type receptors (CB1, CB2)[32,33,34,35] that are expressed in humans and other animals,[32] including on sperm.[36] However, although there are bits of evidence pointing to adverse effects of cannabis use on testosterone levels and on sperm motility.[32,37,38]
Administration of androgenic steroids to men results in reduced spermatogenesis because it causes suppression of LH secretion from the pituitary gland and a resulting suppression of intratesticular testosterone levels; this has been widely evaluated as an approach to male contraception.[39] It is therefore not surprising that use of anabolic steroids by athletes, weightlifters, and bodybuilders can have similar adverse effects;[40,41] as is the case with male contraception, cessation of anabolic steroid use results in recovery of spermatogenesis.[40]
Prescription drugs of numerous types are used widely by normal males, and although effects of such compounds on spermatogenesis cannot really be classified as lifestyle/environmental, if they adversely impact on spermatogenesis such effects may be suspected as having an environmental cause, especially if the drug is taken chronically. An example is sulfasalazine, which has been widely used for the chronic treatment of irritable bowel disorders and which can induce infertility in men[42,43] and in rats[42] via effects probably late in spermatogenesis.[42] Similarly, some chemotherapeutic agents (anti-mitotics such as cyclophosphamide) used for treatment of cancers or of some kidney diseases have well-documented adverse effects on spermatogenesis and/or fertility.[44,45] Of more concern from an environmental perspective is for (largely unsuspected) effects of commonly prescribed drugs that are not necessarily considered as anti-spermatogenic. This is highlighted by a recent study of 165 infertile men (selected from a group of 1768 infertile men) who were taking medications of various sorts at the time of investigation and in whom no hormonal, historical, or other cause for the infertility could be found.[46] The most common medications being taken by these men were H1 receptor antagonists (for allergy relief, such as hay fever), anti-epileptics and antibiotics. When half of the 165 patients switched or ceased their treatment, there was a 93% improvement in semen quality and an 85% increase in conception rate, compared with values of 12 and 10%, respectively, in the control group (men who continued on treatment). Other studies indicate reduced fertility in epileptic men and one explanation is that the drugs used for treatment (carbamazepine, oxcarbazepine, valproate) are associated with adverse effects on sperm number, morphology, or motility.[47] For valproate at least, there is supporting data in rats showing adverse effects on spermatogenesis,[48] although such effects are only obvious with supra-therapeutic dose levels, while at therapeutic dose levels only effects on reproductive hormone levels (reduced oestradiol and LH) are found.[49] Some drugs (e.g., the H2-receptor antagonist, cimetidine) that affect spermatogenesis[50] do so by altering androgen action, which has led to the development of substitute compounds that lack this side effect.
Environmental chemicals on spermatogenesis of adult men
There are three sorts of exposures environmental chemicals: Those that occur occupationally, those that occur in the general or home environment (e.g., pollutants) and those that occur because of our lifestyle choices (e.g., use of skin creams, deodorants, etc.). There is a widespread belief that human exposure to environmental chemicals via one or more of these routes can impair spermatogenesis in adult men and lead to reduced sperm counts. This belief has probably been triggered by the coincidence of concerns about “falling sperm counts” in men[51,52,53] with concerns about the high prevalence of environmental chemicals in the modern environment.[4,7] However, evidence to support this belief is remarkably thin on the ground.
YOGA PRACTICE: IMPACT ON REPRODUCTIVE HEALTH OF MEN
Adopting a regular yoga practice can improve the quality of sperm if one has issues with sperm count or motility. Practicing yoga is also proven to be excellent for prostate health, warding off prostate disorders, and reducing the size of prostate if it has got enlarged. Adopting a regular yoga practice can reduce stress and anxiety levels also, which can improve the overall health of reproductive organs, as it has proven that having less stress in life can improve sex-life and helps to treat mild erectile dysfunction (ED).
Many people in the U.S. today claim to practice yoga for its health benefits without consciously adopting Hindu religious perspectives as growing body of research evidence supports the belief that certain yoga techniques may improve physical and mental health through down-regulation of the HPA axis and the sympathetic nervous system.
The stress and stress-induced disorders are fast growing epidemics and bane of “modern” society. The holistic science of yoga has proven to be the best method for prevention as well as management of stress and stress-induced disorders by immediately down regulating effect on both the HPA axis response to stress.[54] It was also found that brief yoga-based relaxation training normalizes the function of autonomic nervous system by deviating both sympathetic and parasympathetic indices toward more “normal” middle region of the reference values.[55] Studies show that yoga decreases levels of salivary cortisol,[56,57] and 24-h urine nor-epinephrine and epinephrine levels.[58] These studies suggest that yoga has an immediate quieting effect on the HPA axis response to stress. While the precise mechanism of action has not been determined, it has been hypothesized that some yoga exercises cause a shift toward parasympathetic nervous system dominance, possibly via direct vagal stimulation.[59] Regardless of the pathophysiologic pathway, yoga has been shown to have immediate psychological effects: Decreasing anxiety[56,57] and increasing feelings of emotional and spiritual well-being.[60]
Yoga for men: Childhood and early adulthood
Yoga helps children at an early age to develop strength, endurance, grace, and balance. In fact, many common yoga poses were developed for young boys. Yoga colleges, or schools, exclusively for boys were established in India in the late 19th century to offer young boys a full education, including physical culture. In this day and age, children all through the world can practice yoga to sustain the balanced growth of body and mind. Many of the yogic styles were developed to meet the needs of growing boys combining the art of movement with the classical yoga asanas. Weight-bearing postures of yoga helps in the growth of strong bones, whereas bendings and twistings help to maintain flexibility. Today, stress is endemic not only among adult men but also in growing children, thus, an increasing number of primary and high schools are introducing yoga practices into their curriculum in order to help children to learn at an early age how to manage stress.[61]
This is also the phase of reproductive growth and sexual maturation of growing boys. During puberty, immense alterations take place in the body's chemistry and physiology. The chakras also develop and become more active. Inequities of the chakras, body chemistry, and physiology often point up mood swings. Regular yoga practice helps in maintaining balance in the different chakras and keeps the spirit and soul strong and healthy, thereby benefiting both the body and mind. Yoga poses tone and balances the sex glands, while improving energy. During the teen years, most boys and girls become self conscious about the changes in their bodies that go with sexual development. Boys may suddenly become concerned about whether hair is beginning to grow in the right places, such as on their faces or in the pubic area. They may also be concerned with muscle tone. Regular practice of yoga builds muscle tone and strength and improves energy and balance to enhance physical fitness[62] and performance. According to Indian Philosophy, a healthy spine creates balance and creates sound mind. Poses involving twists and upside-down positions are especially effective. Internal organs are growing and changing during this period and can become upset with diet changes or over stimulation of nerves. Yoga helps to keep organs healthy despite everyday stresses. It also assists in balancing out the mood swings and eliminating the body aches resulting from the hormonal imbalances experienced during sexual maturing. During this growth period, yoga is useful in easing the tension of tight muscles, tendons, and ligaments, and it can also help to strengthen bones. Yoga practice in childhood and early adulthood is also found to be effective to avoid precocious puberty.
Yoga for adult men
The stresses of modern life seem to be accelerating, however, to a greater extent for younger men. Stress seems to come from nearly every façade - work, home, personal relations, everywhere. Along with better management of stress, one can not only help himself to keep the muscle strength and flexibility, but also can improve his reproductive health. It also helps to improve circulation, promote proper functioning of the internal organs, and help to steady the nerves. Regarding reproductive health, Kundalini Yoga is considered the ultimate yoga by which virility and sexual energy are not suppressed. Sexual energy, which is considered the most potent form of biochemical energy in the body, is the one form of energy that can be used for rejuvenating the entire physical apparatus, as well as be used for spiritual growth and transformation; so this energy is certainly important to have in quantity and quality. The ancient holy men, yogis of India were known to maintain their sexual charge and drive right through their life and toward that end by yoga practice. Yoga can also heal any sexual dysfunction, and thereby increase sexual potency and refine sexual energy, so it can be utilized for spiritual transformation. In men, practicing moola bandha has been associated with relieving spermatthorrea, preventing inguinal hernia, and controlling testosterone secretion. Kraftsow[63] clarifies how moola bandha stretches the muscles of the pelvic floor, increases circulation in that area, balances, stimulates, and rejuvenates the area through techniques that increase awareness and circulation. As a result, exercises that utilize moola bandha may be helpful in aiding people who lack sexual vitality and have poor sexual functioning. In numerous sex therapy centers, the practice of moola bandha is used to enhance awareness of genital arousal sensations, and in this way, may be a helpful adjunct for improving sexual desire and arousal. For Indian men who practice brahmacharya, or celibacy, certain yoga poses are thought to control (or reduce) erection and desire.[64] For instance, there is a central pose known as siddhasana in which the practitioner's legs are crossed while seated during which a celibate man can pinch his penis and scrotum with his heels to control his desire. This type of control is considered a highly desirable state to attain for these men choosing celibacy.
Yoga for middle aged men
As men mature, the emphasis of yoga practice progressively shifts from growing bones and muscles, to maintaining and protecting health. In this age, the major problems men suffer from is ED and loss of sexual attractions toward female partner, may be as a result of increased stress and anxiety and other physiological problems including hormonal imbalance which again attributable to their age. Anything that increases anxiety or stress may contribute to ED by interfering with the relaxation fundamental to erection. Yoga is deeply relaxing. Something that damages the arteries or interferes with penile blood flow may also contribute to ED. No wonder that risk factors include: High blood pressure, high cholesterol, heart disease, and diabetes, all of which damage the arteries and reduce blood flow around the body, including into the penis. Obesity and a sedentary lifestyle also increase risk of ED. They are closely linked to the risk factors just mentioned. All these conditions also become more prevalent as men age.
Yoga for aged men
Aging, a process of growing old is natural and hence unavoidable. As aging comes across with numerous health problems, mental disturbances and social distraction, it becomes the most annoying part of everyone's life. All these issues interfere with daily routine of a person and make life more cumbersome. The average life expectancy for a male in the United States in the year 2000 was 74 according to studies by the National Center for Health Statistics at the Centers for Disease Control and Prevention.[65] Seniors can benefit immensely from the practice of yoga. Yoga can help to promote the functioning of the circulatory, immune, and endocrine systems. It can help promote enhanced functioning of the nervous system and the internal organs. It can help calm and relax, thus relieving anxiety and stress. Not only physical limitations, but also depression and anxiety can be part of older men's lives. The focusing practices of yoga can help older men gain greater clarity on their life situations - to accept themselves as they are. As men age, their production of DHEA, as well as testosterone and other androgens or sex hormones decline. It is been estimated that for every year over the age of 40, men's testosterone level drops by 1%.[66] About 20% of men in their 60s have significantly reduced testosterone levels. As testosterone is a key hormone in men's sexual functions, aging-related decline in testosterone levels has a negative impact on men's sexual performance.
THERAPEUTIC WAYS OF YOGA ACTION: ON MALE REPRODUCTIVE HEALTH
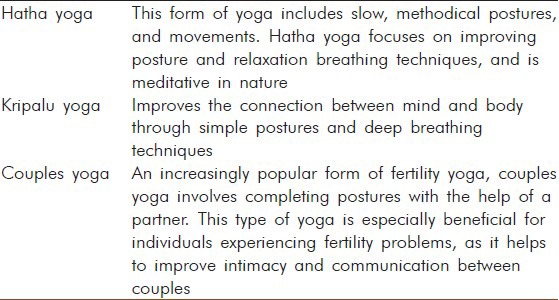
Yoga basically acts as mind-body complementary medicine of male reproductive health by improving health in various ways [Table 1]. It not only acts on endocrine axes to improve reproductive functions in male, but also, helps to improve reproductive health by improving reproductive behavior, mood, and also by reducing anxiety and stress.
Table 1.
Various yogic techniques and their health impacts
Yoga in improvement of reproductive functions
There are reports that shows practice of yoga modulates neuroendocrine axis which results in beneficial changes in the practitioners. Schmidt et al.[67] found a reduction in urinary excretion of catecholamines and aldosterone, a decrease in serum testosterone and luteinizing hormone levels and an increase in cortisol excretion, indicating optimal changes in hormones. Kamei et al.[68] found changes in brain waves and blood levels of serum cortisol during yoga exercise in seven yoga instructors and found that alpha waves increased and serum cortisol significantly decreased.
The field of psychoneuroimmunology has defined the role of stress in reducing effectiveness of the immune system in combating infection and growth of malignant tumors. There are encouraging reports of studies citing the influence of melatonin on prostate tumors. Some studies found an association between meditation practice and levels of melatonin produced by the pineal gland.[69,70] Some studies have reported role of Kundalini Yoga in regulation of terminal prostate cancer.[71] For men, difficulties in the second chakra area usually occur in the prostate gland. On a deeper level, diseases of the pelvic area are often related to blocks in the second chakra, which can be connected to sensual or sexual issues and passion for life in general. This is also the area that carries deepest emotions, including pain and grief. If one does postures that activate the second chakra, especially those with imbalances in the pelvic area, will experience those feelings emerging. Every so often middle-aged men will experience swelling of the prostate, which does not cause pain but causes excessive urination due to the pressure on the bladder. Compression in postures such as the Yoga Mudra and Locust can flush out the prostate, bring in fresh blood and prana and improve tone. Men with inflamed prostates should avoid postures that press down into the pelvis and they should go only halfway into less compressing posture. Pranayama can also be practiced in conjuction with the postures. Kapalabhati is an excellent practice for moving energy into the pelvis and is especially helpful for prostate enlargement, for inflammatory conditions, like prostatitis, dirgha pranayama or ujjayi breath can help cool and relax the area.
Obesity in reproductive age is also found to be a contributor to the male infertility. Yogic practice reported to improve serum adiponectin and leptin levels along with serum lipids and metabolic syndrome risk factors.[72] Yoga and other relaxation techniques are established to have higher potency in regulating adipocity than other complementary and alternative therapies.[73]
Yoga in subduing stress and anxiety
Since the 1970s, meditation and other stress-reduction techniques have been studied as possible treatments for depression and anxiety. One such practice, yoga has received less attention in the medica literature, though it has become increasingly popular in recent decades. Stress, however, is known to raise the likelihood of infertility, and yoga is very effective at reducing stress. Patients suffering from problems in reproductive functions, experience anxiety and depression rates similar to those of patients with cancer, HIV/AIDS. And even patients without fertility problems can find trying to have a baby-a mysterious process ultimately beyond our control-an anxiety-inducing experience. The links between stress and infertility are complex and not fully understood, but cortisol, the socalled stress hormone, can interfere with normal reproductive functions. Lower stress levels and having a positive mood and outlook can increase the odds that fertility treatments will work. Perhaps the strongest evidence is that reducing stress through yoga can boost fertility.
In 2000, Domar found that 55% of infertility patients had a baby within 1 year of practicing yoga and meditation, along with other relaxation techniques Anxiety responds well to treatments such as cognitive behavioral therapy and/or medication. Non-pharmacological interventions such as mind-body interventions, known to decrease anxiety in several clinical situations, might be offered for treating and preventing anxiety during reproductive age.
Available reviews of a wide range of yoga practices suggest they can reduce the impact of exaggerated stress responses and may be helpful for both anxiety and depression. It mainly acts via down regulating the HPA axis that trigger as a response to a physical or psychological demand (stressor), leading to a cascade of physiological, behavioral, and psychological effects, primarily as a result of the release of cortisol and catecholamines. This response leads to the mobilization of energy needed to combat the stressor through the classic “fight or flight” syndrome.
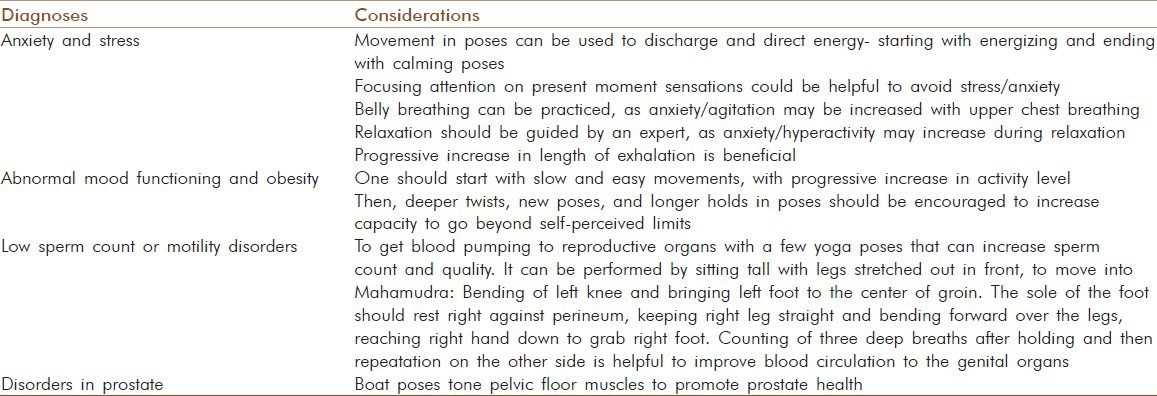
In this respect, yoga functions like other self-soothing techniques, such as meditation, relaxation, and exercise [Table 2]. By reducing perceived stress and anxiety, yoga appears to modulate stress response systems. Tooley et al.[74] found significantly higher plasma melatonin levels in experienced meditators in the period immediately following meditation compared with the same period at the same time on a control night. It was concluded that meditation can affect plasma melatonin levels. It remains to be determined whether this is achieved through decreased hepatic metabolism of the hormone or via a direct effect on pineal physiology. Either way, facilitation of higher physiological melatonin levels at appropriate times of day might be one avenue through which the claimed health promoting effects of meditation occur. These observations suggest that yogic practices can be used as psychophysiologic stimuli to increase endogenous secretion of melatonin, which, in turn, might be responsible for improved sense of well-being.
Table 2.
Yogic practices to improve male reproductive health
Yoga in improving mood and functioning
In a German study published in 2005, women who described themselves as “emotionally distressed” are treated with 90-minute yoga classes a week for 3 months. At the end of 3 months, women in the yoga group reported improvements in perceived stress, depression, anxiety, energy, fatigue, and well-being. Depression scores improved by 50%, anxiety scores 30%, and overall well-being scores by 65%. Initial complaints of headaches, back pain, and poor sleep quality also resolved much more often in the yoga group than in the control group. In an another 2005 study examined the effects of a single yoga class for inpatients at the New Hampshire psychiatric hospital, 113 participants among patients with bipolar disorder, major depression, and schizophrenia it is found after yoga class, tension, anxiety, depression, anger, hostility, and fatigue dropped significantly. Further controlled trials of yoga practice have demonstrated improvements in mood and quality of life for elderly, people caring for patients with dementia, breast cancer survivors, and patients with epilepsy.[75]
CONCLUSION
The high prevalence of low sperm counts in young men across the world today is a cause for concern, especially when considered together with the trend for first pregnancy in the female partner (and thus reduced female fertility). As this review has shown, evidence for widespread or major effects of individual lifestyle or environmental factors on spermatogenesis in adulthood, and prenatal exposures of males (reflective of maternal lifestyle and/or exposures) can have major impact on capacity to produce sperm in adulthood, although the overall importance of such effects is difficult to measure because of the inherent difficulties in accurately relating events that are separated by two or more decades. However, it seems intuitively likely that the major changes to our lifestyles, diets, and activity levels over recent decades will have impacted negatively on spermatogenesis in adulthood, as all available evidence points toward negative effects of sedentary lifestyles and obesity on testis function (testosterone levels and sperm production); potential effects of environmental pollutants can only exacerbate such effects. Realistically, the likelihood is that small effects of several different factors may combine together to induce more substantial negative effects on spermatogenesis.[76,77] Thus, the present review postulates that complementary and alternative medicine (CAM), yoga, triggers neurohormonal mechanisms that reduces stress and anxiety, improves autonomic functions and thus, improves reproductive health. However, there is a definite need for more directed scientific research to be carried out to elucidate the effects and the mechanisms of such impacts of yoga on male reproductive physiology. Considering the scientific evidence discussed so far, it is fair to conclude that yoga can be beneficial in the prevention of infertility and improve male reproductive health.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. Fertil Steril. 2002;77:873–82. doi: 10.1016/s0015-0282(02)03105-9. [DOI] [PubMed] [Google Scholar]
- 2.Society for Assisted Reproductive Technology, American Fertility Society. Assisted reproductive technology in the United States and Canada: 1991 results from the Society for Assisted Reproductive Technology generated from the American Fertility Society registry. Fertil Steril. 1991;59:956–62. doi: 10.1016/s0015-0282(16)55910-x. [DOI] [PubMed] [Google Scholar]
- 3.Chehval MJ, Mehan DJ. Chorionic gonadotropins in the treatment of the subfertile male. Fertil Steril. 1979;31:666–8. doi: 10.1016/s0015-0282(16)44058-6. [DOI] [PubMed] [Google Scholar]
- 4.Sengupta P. Environmental metal toxicants in physiology and pathophysiology of male reproduction. Drug Chem Toxicol. 2013;36:353–68. doi: 10.3109/01480545.2012.710631. [DOI] [PubMed] [Google Scholar]
- 5.Sengupta P. Health impacts of yoga and pranayama: A state-of-the-art review. Int J Prev Med. 2012;3:444–58. [PMC free article] [PubMed] [Google Scholar]
- 6.Sengupta P. Story of Laboratory Rat Age Determination: How is it Old when set against Human Age. Biomed Int. 2011;2:81–9. [Google Scholar]
- 7.Sharpe RM. Lifestyle and environmental contribution to male infertility. Br Med Bull. 2000;56:630–42. doi: 10.1258/0007142001903436. [DOI] [PubMed] [Google Scholar]
- 8.Chandra AK, Goswami H, Sengupta P. Dietary calcium induced cytological and biochemical changes in thyroid. Environ Toxicol Pharmacol. 2012;34:454–65. doi: 10.1016/j.etap.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Sharpe RM. Regulation of spermatogenesis. In: Knobil E, Neill JD, editors. The physiology of reproduction. New York, NY: Raven Press; 1994. pp. 1363–434. [Google Scholar]
- 10.Hammoud AO, Gibson M, Petersen CM, Hamilton BD, Carrell DT. Obesity and male reproductive potential. J Androl. 2006;27:619–26. doi: 10.2164/jandrol.106.000125. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen TL, Hagen C, Wraae K, Brixen K, Petersen PH, Haug E, et al. Visceral and subcutaneous adipose tissue assessed by magnetic resonance imaging in relation to circulating androgens, sex hormone-binding globulin, and luteinizing hormone in young men. J Clin Endocrinol Metab. 2007;92:2696–705. doi: 10.1210/jc.2006-1847. [DOI] [PubMed] [Google Scholar]
- 12.Magnusdottir EV, Thorsteinsson T, Thorsteindottir S, Heimisdottir M, Olafsdottir K. Persistent organochlorines, sedentary occupation, obesity and human male subfertility. Hum Reprod. 2005;20:208–15. doi: 10.1093/humrep/deh569. [DOI] [PubMed] [Google Scholar]
- 13.Hammoud AO, Gibson M, Petersen CM, Meikle AW, Carrell DT. Impact of male obesity on infertility: A critical review. Fertil Steril. 2008;90:897–904. doi: 10.1016/j.fertnstert.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 14.Jensen TK, Andersson AM, Jørgensen N, Andersen AG, Carlsen E, Petersen JH, et al. Body mass index in relation to semen quality and reproductive hormones among 1558 Danish men. Fertil Steril. 2004;82:863–70. doi: 10.1016/j.fertnstert.2004.03.056. [DOI] [PubMed] [Google Scholar]
- 15.Sengupta P, Chaudhuri P, Bhattacharya K. A small-scale cross-sectional study for the assessment of cardiorespiratory fitness in relation to body composition and morphometric characters in fishermen of Araku valley, Andhra Pradesh, India. Int J Prev Med. 2013 In Press. [PMC free article] [PubMed] [Google Scholar]
- 16.Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, Witt MA, et al. Impact of body mass index values on sperm quality and quantity. J Androl. 2006;27:450–2. doi: 10.2164/jandrol.05124. [DOI] [PubMed] [Google Scholar]
- 17.Gould DC, Kirby RS, Amoroso P. Hypoandrogen-metabolic syndrome: A potentially common and underdiagnosed condition in men. Int J Clin Pract. 2007;61:341–4. doi: 10.1111/j.1742-1241.2006.01239.x. [DOI] [PubMed] [Google Scholar]
- 18.Raman JD, Schlegel PN. Aromatase inhibitors for male infertility. J Urol. 2002;167:624–9. doi: 10.1016/S0022-5347(01)69099-2. [DOI] [PubMed] [Google Scholar]
- 19.Kawakami E, Hirano T, Hori T, Tsutsui T. Improvement in spermatogenic function after subcutaneous implantation of a capsule containing an aromatase inhibitor in four oligozoospermic dogs and one azoospermic dog with high plasma estradiol-17 beta concentrations. Theriogenology. 2004;62:165–78. doi: 10.1016/j.theriogenology.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 20.Winters SJ, Wang C, Abdelrahaman E, Hadeed V, Dyky MA, Brufsky A. Inhibin-B levels in healthy young adult men and prepubertal boys: Is obesity the cause for the comtemporary decline in sperm count because of fewer Sertoli cell? J Androl. 2006;27:560–4. doi: 10.2164/jandrol.05193. [DOI] [PubMed] [Google Scholar]
- 21.Shafik A, Olfat S. Scrotal lipomatosis. Br J Urol. 1981;53:50–4. doi: 10.1111/j.1464-410x.1981.tb03128.x. [DOI] [PubMed] [Google Scholar]
- 22.Pelletier C, Despres JP, Tremblay A. Plasma organochlorine concentrations in endurance athletes and obese individuals. Med Sci Sports Exerc. 2002;34:1971–5. doi: 10.1249/01.MSS.0000040820.48707.99. [DOI] [PubMed] [Google Scholar]
- 23.Vine MF. Smoking and male reproduction: A review. Int J Androl. 1996;19:323–37. doi: 10.1111/j.1365-2605.1996.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 24.Vine MF, Margolin BH, Morrison HI, Hulka BS. Cigarette smoking and sperm density: A meta-analysis. Fertil Steril. 1994;61:35–43. [PubMed] [Google Scholar]
- 25.Maddocks S, Hargreave TB, Reddie K, Fraser HM, Kerr JB, Sharpe RM. Intratesticular hormone levels and the route of secretion of hormones from the testis of the rat, guinea pig, monkey and human. Int J Androl. 1993;16:272–8. doi: 10.1111/j.1365-2605.1993.tb01191.x. [DOI] [PubMed] [Google Scholar]
- 26.Piner J, Sutherland M, Millar M, Turner KJ, Newall D, Sharpe RM. Changes in vascular dynamics of the adult rat testis leading to transient accumulation of seminiferous tubule fluid after administration of a novel 5-hydroxytryptamine (5-HT) agonist. Reprod Toxicol. 2002;16:141–50. doi: 10.1016/s0890-6238(02)00008-4. [DOI] [PubMed] [Google Scholar]
- 27.Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007;22:188–96. doi: 10.1093/humrep/del364. [DOI] [PubMed] [Google Scholar]
- 28.Martini AC, Molina RI, Estofan D, Senestrari D, Fiol de Cuneo M, Ruiz RD. Effects of alcohol and cigarette consumption on human seminal quality. Fertil Steril. 2004;82:374–7. doi: 10.1016/j.fertnstert.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 29.Marinelli D, Gaspari L, Pedotti P, Taioli E. Mini-review of studies on the effect of smoking and drinking habits on semen parameters. Int J Hyg Environ Health. 2004;207:185–92. doi: 10.1078/1438-4639-00283. [DOI] [PubMed] [Google Scholar]
- 30.Villalta J, Ballesca JL, Nicolas JM, Martinez de Osaba MJ, Antunez E, Pimentel C. Testicular function in asymptomatic chronic alcoholics: Relation to ethanol intake. Alcohol Clin Exp Res. 1997;21:128–33. [PubMed] [Google Scholar]
- 31.Muthusami KR, Chinnaswamy P. Effect of chronic alcoholism on male fertility hormones and semen quality. Fertil Steril. 2005;84:919–24. doi: 10.1016/j.fertnstert.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 32.Brown TT, Dobs AS. Endocrine effects of marijuana. J Clin Pharmacol. 2002;42(Suppl 11):90S–6. doi: 10.1002/j.1552-4604.2002.tb06008.x. [DOI] [PubMed] [Google Scholar]
- 33.Ricci G, Cacciola G, Altucci L, Meccariello R, Pierantoni R, Fasano S, et al. Endocannabinoid control of sperm motility: The role of the epididymis. Gen Comp Endocrinol. 2007;153:320–2. doi: 10.1016/j.ygcen.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Abel EL. Marihuana and sex: A critical survey. Drug Alcohol Depend. 1981;8:1–22. doi: 10.1016/0376-8716(81)90082-x. [DOI] [PubMed] [Google Scholar]
- 35.Patra PB, Wadsworth RM. Quantitative evaluation of spermatogenesis in mice following chronic exposure to cannabinoids. Andrologia. 1991;23:151–6. doi: 10.1111/j.1439-0272.1991.tb02520.x. [DOI] [PubMed] [Google Scholar]
- 36.Rossato M, Ion Popa F, Ferigo M, Clari G, Foresta C. Human sperm express cannabinoid receptor Cb1, the activation of which inhibits motility, acrosome reaction and mitochondrial function. J Clin Endocrinol Metab. 2005;90:984–91. doi: 10.1210/jc.2004-1287. [DOI] [PubMed] [Google Scholar]
- 37.Diamond F, Ringenberg L, MacDonald D, Barnes J, Hu CS, Duckett G, et al. Effects of drug and alcohol abuse upon pituitary-testicular function in adolescent males. J Adolesc Health Care. 1986;7:28–33. doi: 10.1016/s0197-0070(86)80091-2. [DOI] [PubMed] [Google Scholar]
- 38.Bracken MB, Eskenazi B, Sachse K, McSharry JE, Hellenbrand K, Leo-Summers L. Association of cocaine use with sperm concentration, motility and morphology. Fertil Steril. 1990;53:315–22. doi: 10.1016/s0015-0282(16)53288-9. [DOI] [PubMed] [Google Scholar]
- 39.Anderson RA, Baird DT. Male contraception. Endocr Rev. 2002;23:735–62. doi: 10.1210/er.2002-0002. [DOI] [PubMed] [Google Scholar]
- 40.Knuth UA, Maniera H, Nieschlag E. Anabolic steroids and semen parameters in bodybuilders. Fertil Steril. 1989;52:1041–7. doi: 10.1016/s0015-0282(16)53172-0. [DOI] [PubMed] [Google Scholar]
- 41.Karila T, Hovatta O, Seppala T. Concomitant abuse of anabolic androgenic steroids and human chorionic gonadotrophin impairs spermatogenesis in power athletes. Int J Sports Med. 2004;25:257–63. doi: 10.1055/s-2004-819936. [DOI] [PubMed] [Google Scholar]
- 42.O’Morian C, Smethurst P, Dore CJ, Levi AJ. Reversible male infertility due to sulphasalazine: Studies in man and rat. Gut. 1984;25:1078–84. doi: 10.1136/gut.25.10.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feagins LA, Kane SV. Sexual and reproductive issues for men with inflammatory bowel disease. Am J Gastroenterol. 2009;104:768–73. doi: 10.1038/ajg.2008.90. [DOI] [PubMed] [Google Scholar]
- 44.Buchanan JF, Davis LJ. Drug-induced infertility. Drug Intell Clin Pharm. 1984;18:122–32. doi: 10.1177/106002808401800205. [DOI] [PubMed] [Google Scholar]
- 45.Nudell DM, Monoski MM, Lipshultz LI. Common medications and drugs: How they affect male fertility. Urol Clin North Am. 2002;29:965–73. doi: 10.1016/s0094-0143(02)00079-4. [DOI] [PubMed] [Google Scholar]
- 46.Hayashi T, Miyata A, Yamada T. The impact of commonly prescribed drugs on male fertility. Hum Fertil. 2008;11:191–6. doi: 10.1080/14647270701739566. [DOI] [PubMed] [Google Scholar]
- 47.Isojarvi JI, Lofgren E, Juntunen KS, Pakarinen AJ, Paivansato M, Rautakorpi I, et al. Effect of epilepsy and antiepileptic drugs on male reproductive health. Neurology. 2004;62:247–53. doi: 10.1212/01.wnl.0000098936.46730.64. [DOI] [PubMed] [Google Scholar]
- 48.Nishimura T, Sakai M, Yonezawa H. Effects of valproic acid on fertility and reproductive organs in male rats. J Toxicol Sci. 2000;25:85–93. doi: 10.2131/jts.25.85. [DOI] [PubMed] [Google Scholar]
- 49.Sveberg Roste L, Tauboli E, Isojarvi JI, Pakarinen AJ, Huhtaniemi IP, Knip M, et al. Effects of chronic valproate treatment on reproductive endocrine hormones in female and male Wistar rats. Reprod Toxicol. 2002;16:767–73. doi: 10.1016/s0890-6238(02)00054-0. [DOI] [PubMed] [Google Scholar]
- 50.Van Thiel DH, Gavaler JS, Smith WI, Paul G. Hypothalamic-pituitary-gonadal dysfunction in men using cimetidine. N Engl J Med. 1979;300:1012–5. doi: 10.1056/NEJM197905033001803. [DOI] [PubMed] [Google Scholar]
- 51.Chandra AK, Sengupta P, Goswami H, Sarkar M. Excessive Dietary Calcium in the Disruption of Structural and Functional Status of Adult Male Reproductive System in Rat with Possible Mechanism. Mol Cell Biochem. 2012;364:181–91. doi: 10.1007/s11010-011-1217-3. [DOI] [PubMed] [Google Scholar]
- 52.Chandra AK, Sengupta P, Goswami H, Sarkar M. Effects of dietary magnesium on testicular histology, steroidogenesis, spermatogenesis and oxidative stress markers in adult rats. Indian J Exp Biol. 2013;51:37–47. [PubMed] [Google Scholar]
- 53.Swan SH, Elkin EP, Fenster L. The question of declining sperm density revisited: An analysis of 101 studies published 1934–1996. Environ Health Perspect. 2000;108:961–6. doi: 10.1289/ehp.00108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K, Ramaratnam S. Yoga for anxiety: A systematic review of the research evidence. Br J Sports Med. 2005;39:884–91. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for Depression: The Research Evidence. J Aff Dis. 2005;89:13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 56.Michalsen A, Grossman P, Acil A, Langhorst J, Ludtke R, Esch T, et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three month intensive yoga program. Med Sci Monit. 2005;11:555–61. [PubMed] [Google Scholar]
- 57.West J, Otte C, Geher K, Johnson J, Mohr DC. Effects of Hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann Behav Med. 2004;28:114–8. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]
- 58.Selvamurthy W, Sridharan K, Ray US, Tiwary RS, Hedge KS, Radhakrishnan U, et al. A new physiological approach to control essential hypertension. Ind J Physiol Pharmacol. 1998;42:205–13. [PubMed] [Google Scholar]
- 59.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 60.Moadel AB, Shaw C, Wylie-Rossett J, Harris MS, Patel SR, Hall CB, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J Clin Oncol. 2007;25:1–9. doi: 10.1200/JCO.2006.06.6027. [DOI] [PubMed] [Google Scholar]
- 61.Brown Patricia Leigh. New York: The New York Times; 2002. “Latest Way to Cut Grade School Stress: Yoga”. [Google Scholar]
- 62.Sengupta P, Sahoo S. A cross sectional study to evaluate the fitness pattern among the young fishermen of Coastal Orissa. Indian J Pub Heal Res Dev. 2013;4:193–7. [Google Scholar]
- 63.Kraftsow G. [Last accessed on 2012 Nov 2]. as quoted at Available from: http://www.viniyoga.com .
- 64.Alter JS. Seminal truth: A modern science of male celibacy in north India. 1997;11:275–98. doi: 10.1525/maq.1997.11.3.275. [DOI] [PubMed] [Google Scholar]
- 65.Statistics from the Centers for Disease Control and Prevention, quoted in Maggie Fox, “Healthy Older Americans,” a Reuters’ news release dated Sep 12. 2002:23–209. [Google Scholar]
- 66.Sengupta P. The laboratory rat: Relating its age with human's. Int J Prev Med. In Press. [PMC free article] [PubMed] [Google Scholar]
- 67.Schmidt T, Wijga A, Von Zur Muhlen A, Brabant G, Wagner TO. Changes in Cardiovascular risk factors and hormones during a comprehensive residential three month kriya yoga training and vegetarian nutrition. Acta Phys Scand Suppl. 1997;161:158–62. [PubMed] [Google Scholar]
- 68.Kamei T, Toriumi Y, Kimura H, Ohno S, Kumano H, Kimura K. Decrease in serum cortisol during yoga exercise is correlated with alpha wave activation. Percept Mot Skills. 2000;90:1027–32. doi: 10.2466/pms.2000.90.3.1027. [DOI] [PubMed] [Google Scholar]
- 69.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychos Med. 2003;65:571–81. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 70.Coker KH. Meditation and prostate cancer: Integrating a mind/body intervention with traditional therapies. Semin Urol Oncol. 1999;17:111–8. [PubMed] [Google Scholar]
- 71.Shannahoff-Khalsa DS. Patient perspectives: Kundalini yoga meditation techniques for psycho-oncology and as potential therapies for cancer. Integr Cancer Ther. 2005;4:87–100. doi: 10.1177/1534735404273841. [DOI] [PubMed] [Google Scholar]
- 72.Lee JA, Kim JW, Kim DY. Effects of yoga exercise on serum adiponectin and metabolic syndrome factors in obese postmenopausal women. Menopause. 2012;19:296–301. doi: 10.1097/gme.0b013e31822d59a2. [DOI] [PubMed] [Google Scholar]
- 73.Bertisch SM, Wee CC, McCarthy EP. Use of Complementary and Alternative Therapies by Overweight and Obese Adults. Obesity. 2008;16:1610–5. doi: 10.1038/oby.2008.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000;53:69–78. doi: 10.1016/s0301-0511(00)00035-1. [DOI] [PubMed] [Google Scholar]
- 75.Brown RP, Gerbarg PL. Sudarshan Kriya Yogic Breathing in the Treatment of Stress, Anxiety, and Depression: Part I-Neurophysiologic Model. J Alt Compl Med. 2005;1:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 76.Sengupta P. Chemosterilization: Spermatogenesis, Steroidogenesis, Reproductive Functions, and Behavior from Historical Perspective to Contemporary Practice. J Basic Clin Repro Sci. 2013;2:1–2. [Google Scholar]
- 77.Sengupta P. Challenge of infertility: How protective the yoga therapy is? Ancient Sci Life. 2012;32:275–76. doi: 10.4103/0257-7941.113796. [DOI] [PMC free article] [PubMed] [Google Scholar]


