Abstract
Background & objectives:
There are only a few studies on aetiology of portal hypertension among adults presenting to tertiary care centres in India; hence we conducted this study to assess the aetiological reasons for portal hypertension in adult patients attending a tertiary care centre in southern India.
Methods:
Causes of portal hypertension were studied in consecutive new adult patients with portal hypertension attending department of Hepatatology at a tertiary care centre in south India during July 2009 to July 2010.
Results:
A total of 583 adult patients (>18 yr old) were enrolled in the study. After non-invasive testing, commonest causes of portal hypertension were cryptogenic chronic liver disease (35%), chronic liver disease due to alcohol (29%), hepatitis B (17%) or hepatitis C (9%). Of the 203 patients with cryptogenic chronic liver disease, 39 had liver biopsy - amongst the latter, idiopathic non cirrhotic intrahepatic portal hypertension (NCIPH) was seen in 16 patients (41%), while five patients had cirrhosis due to non alcoholic fatty liver disease. Fifty six (10%) adult patients with portal hypertension had vascular liver disorders. Predominant causes of portal hypertension in elderly (>60 yrs; n=83) were cryptogenic chronic liver disease (54%) and alcohol related chronic liver disease (16%).
Interpretation & conclusions:
Cryptogenic chronic liver disease was the commonest cause of portal hypertension in adults, followed by alcohol or hepatitis B related chronic liver disease. Of patients with cryptogenic chronic liver disease who had liver biopsy, NCIPH was the commonest cause identified. Vascular liver disorders caused portal hypertension in 10 per cent of adult patients. Cryptogenic chronic liver disease was also the commonest cause in elderly patients.
Keywords: cryptogenic chronic liver disease, non cirrhotic intrahepatic portal hypertensionn, vascular liver disorders
Portal hypertension can present as oesophageal variceal bleeding, ascites or hypersplenism. It is important to understand the cause of portal hypertension to put in place strategies to prevent/ameliorate the same. The causes of portal hypertension in a country can vary over time. With increasing affluence, better standards of living as well as change to more sedentary lifestyle in India, metabolic syndrome leading to non-alcohol related fatty liver disease (NAFLD) as well as alcohol related cirrhosis are expected to increase in the coming years while hepatitis B or C virus related cirrhosis may be expected to decline. In addition, for as yet unclear reasons, some vascular disorders causing non-cirrhotic portal hypertension-like idiopathic non cirrhotic intrahepatic portal hypertension (NCIPH) and portal vein thrombosis [also known as extra-hepatic portal vein obstruction (EHPVO)] in children are known to be more common in India1.
The different causes of portal hypertension are likely to vary in frequency among patients of different age groups and different socio-economic classes. While portal vein thrombosis is the predominant cause of paediatric portal hypertension in India2,3, hepatic Wilson's disease is another important cause in this age group2. There are a few studies focussed on the cause of portal hypertension in adults in India4,5. A study from eastern India reported hepatitis B as the most important cause of portal hypertension in adults.4 Studies from other parts of the world have reported hepatitis C and alcohol as the predominant aetiology of chronic liver disease6,7,8.
This study was conducted to document the aetiology of portal hypertension in adult patients attending a tertiary care centre in southern India.
Material & Methods
Consecutive patients with portal hypertension (defined as presence of gastro-oesophageal varices and/or ascites with serum to ascites albumin gradient >1.1 g/dl) seen in the department of Hepatology, Christian Medical College & Hospital, Vellore, Tamil Nadu, India, from July 2009 to July 2010 were prospectively enrolled in this study, after obtaining their consent. Only adult patients with age >18 yr were included in the study. The study protocol was approved by the Institution Review Board and Ethics Committee.
All patients had the following evaluation to ascertain the aetiology of portal hypertension - history (especially regarding alcohol intake), physical examination, laboratory tests [liver function tests, hepatitis B surface antigen (HBsAg), hepatitis C virus (HCV) antibody, serum ceruloplasmin and serum ferritin] and ultrasound abdomen. Further aetiological evaluation such as serology for autoimmune liver disease, Doppler scan of portal vein and hepatic venous outflow tract was done as and when indicated. Liver biopsy was done when deemed necessary.
In the study subjects (all of whom had portal hypertension), chronic liver disease was defined as presence of any of the following changes noted in the liver on imaging (ultrasound, CT or MRI scan): volume reduction/re-distribution, irregular margins, coarse texture or nodular liver. Cirrhosis was reported only when histological confirmation of the same was obtained.
In patients with chronic liver disease or cirrhosis, the following criteria were used to define different aetiologies of liver disease - alcohol related : history of significant alcohol consumption (>30 g/day for >10 yr)9; hepatitis B virus related: HBsAg positive; HCV related: HCV antibody positive; Wilson's disease: low serum ceruloplasmin, elevated 24 h urinary copper and presence of Kayser Fleischer ring on slit lamp examination of eye (≥2 criteria satisfied)10; autoimmune liver disease: based on the simplified criteria for autoimmune hepatitis (≥7 points)11; haemochromatosis: transferrin saturation >45 per cent, compatible liver histology; primary biliary cirrhosis: positive for anti-mitochondrial antibody with characteristic liver histology13; primary sclerosing cholangitis14: typical cholangiogram with no obvious cause for secondary sclerosing cholangitis; biliary cirrhosis: long standing biliary obstruction; NAFLD: characteristic liver histologic features and negative workup for an alternative aetiology15; cryptogenic: aetiology of portal hypertension not evident after non-invasive evaluation.
The three vascular liver disorders were defined as follows: portal vein thrombosis: portal vein showing cavernoma formation (on Doppler scan), Budd Chiari syndrome: block in hepatic venous outflow tract (on Doppler scan) and NCIPH: Doppler showing patent portal vein and hepatic venous outflow tract, no obvious aetiology of chronic liver disease and liver biopsy negative for cirrhosis / advanced fibrosis16. Diagnosis of hepatocellular carcinoma was based on focal liver lesion with typical enhancement pattern on CT/MRI scan, elevated serum alpha foetoprotein level and liver biopsy.
Age at first presentation to our centre, sex, place of residence, and socio-economic score (as per modified Kuppuswamy's score17) of the patients were also documented.
We retrospectively looked for presence of risk factors for NAFLD [body mass index (BMI), dyslipidemia, diabetes mellitus] among patients with cryptogenic chronic liver disease, who did not have liver biopsy. Patients with BMI ≥27.5 kg/m2 were considered obese18. Dyslipidemia was considered as fasting serum triglycerides >150 mg% and/or low high-density lipoproteins (<40 mg% in males, <50 mg% in females)19. Diabetes mellitus was defined by ongoing management of diabetes mellitus (i.e. diet restriction, oral hypoglycaemic agents or Insulin) or presence of high fasting sugar (≥126 mg%)19.
Statistical analysis: Different aetiologies of portal hypertension were analysed in all adults (19-59 yr age) and in elderly (>60 yr old) age groups. Male : female ratios was also analysed in different aetiological groups. SPSS version 16 Inc. USA was used for analysis. Continuous variables were expressed in mean and standard deviation or median and range. Fisher's exact test (discrete variable) was used for comparison in two unrelated samples and a 2-tailed P value of <0.05 was considered as significant.
Results
During the study period, a total of 610 new patients with portal hypertension were seen, 27 patients aged <18 yr were excluded from this study. Thus, 583 adult patients (>18 yr old), including 83 elderly patients (>60 yr), constituted the study population.
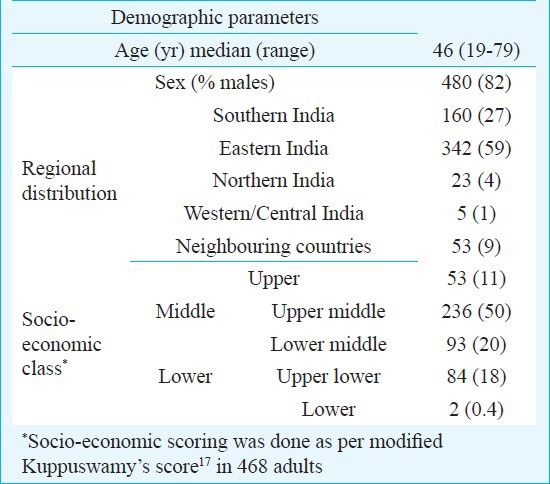
Aetiology of portal hypertension in all adult patients (including the elderly): Baseline demographic details of the 583 adult patients are shown in Table I. After the initial work-up (i.e. prior to liver biopsy) commonest aetiology for portal hypertension was cryptogenic (n=203, 35%) chronic liver disease, followed by alcohol (n=168, 29%), hepatitis B (n=100, 17%) and HCV (n=55, 9%) related chronic liver disease. Other aetiologies were portal vein thrombosis, with or without associated cryptogenic chronic liver disease (n=19, 3%), Budd Chiari syndrome (n=21, 4%), autoimmune liver disease (n=2, 0.3%), biliary aetiology (n=6, 1%), Wilson's disease (n=2, 0.3%), cardiac cirrhosis (n=2) and 1 patient each with splenic vein thrombosis, lymphoma, constrictive pericarditis, myxedema and methotrexate related hepatic fibrosis. Twenty four patients had >1 aetiology for chronic liver disease and portal hypertension: hepatitis B and alcohol (17 patients); hepatitis C and alcohol (7 patients); 25 patients had hepatocellular carcinoma.
Table I.
Demographics of 583 consecutive, new adult patients (including elderly patients) with portal hypertension
Cryptogenic chronic liver disease: Of the 203 patients with cryptogenic chronic liver disease after non-invasive evaluation, 39 (19%) had liver biopsy. After liver biopsy, aetiologies of portal hypertension identified were NCIPH (n=16), NAFLD (n=5), cryptogenic cirrhosis (n=5), hepatic amyloidosis (n=1) and Wilson's disease (n=1). After liver biopsy, eight patients fulfilled the criteria for autoimmune liver disease. The liver biopsy sample was inadequate for evaluation in three patients.
Of the 164 patients with cryptogenic chronic liver disease who did not have liver biopsy, 126 (77%) had a risk factor for NAFLD [diabetes mellitus- 62/164 patients, dyslipidemia- 99/125 patients tested, and/or obesity (BMI >27.5 kg/m2)- 21/83] and five patients satisfied the criteria for probable autoimmune hepatitis.
Vascular liver disorders: Of the 583 patients, 56 (10%) had vascular liver diseases. These comprised portal vein thrombosis with or without associated cryptogenic chronic liver disease (n=19), Budd Chiari syndrome (n=21) and NCIPH (n=16). Age at presentation of patients with portal vein thrombosis, with or without associated cryptogenic chronic liver disease (34, 21-50 yr; median, range) was similar to patients with NCIPH (31, 20-59 yr) and Budd Chiari syndrome (34, 19-58 yr).
In the 16 NCIPH patients, the liver biopsies (12 were transjugular and 4 were percutaneous) showed no significant fibrosis (5 patients), mild portal/periportal fibrosis (10), moderate periportal fibrosis (1 patient), mild peri-sinusoidal fibrosis (1), abnormal portal venous ectasia (6), mild diffuse sinusoidal dilatation (9); no patient had cirrhosis or severe fibrosis.
In patients with Budd Chiari syndrome (n=21), 11 had isolated hepatic vein block, four had isolated inferior vena cava block and six had combined block of hepatic vein and inferior vena cava. Of the 44 patients with vascular liver disorders who had their socio-economic status assessed two belonged to upper class (NCIPH:1; BCS:1), 30 belonged to middle class (portal vein thrombosis:7; NCIPH:13; BCS:10) and 12 belonged to lower class (portal vein thrombosis:6; NCIPH:1; BCS:5).
Socio-economic class distribution: Socio-economic class scoring was done in 468 adult patients - the majority belonged either to middle class (n=329; 70%) or lower class (n=86; 18%) (Table I).
Regional distribution: Most of the study patients were from eastern and southern parts of India. After the initial evaluation, cryptogenic chronic liver disease was significantly more common in patients from eastern compared to southern India (137/342 vs 39/160; P<0.001).
Analysis of male: female ratios in different aetiologies of portal hypertension: Marked male preponderance was noted in patients with chronic liver disease due to alcohol [male:female (male:female ratio) : 166:2 (83.0)] or hepatitis B [93:7 (13.3)]. In contrast, male preponderance was lesser in patients with cryptogenic chronic liver disease [129:43 (3)]; HCV related chronic liver disease [38:17 (2.3)] and vascular liver disorders: NCIPH [10:6 (1.7)], portal vein thrombosis [12:7 (1.7)] and Budd Chiari syndrome [11:10 (1.1)].
Aetiology of portal hypertension in elderly patients: In 83 elderly patients (71 males; age: 64, 60-79 yr; median, range) causes of portal hypertension were chronic liver disease which was cryptogenic (n=45) or related to alcohol (n=13), hepatitis B (n=12), hepatitis C (n=10); biliary cirrhosis (n=2) and myxedema (n=1). Liver biopsy, done in three patients with cryptogenic chronic liver disease, showed amyloidosis (n=1), cryptogenic cirrhosis (n=1) and inadequate liver sample (n=1). Of the 42 patients with cryptogenic chronic liver disease, a risk factor for NAFLD was noted in 32 patients (diabetes mellitus: 16/42, dyslipidemia: 21/29 tested and/or obesity: 2/19). Four patients had hepatocellular carcinoma.
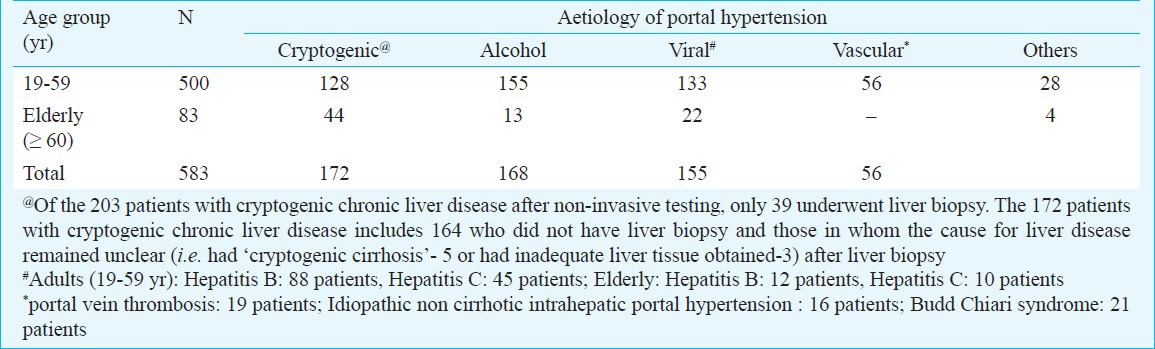
Table II depicts broad aetiologies of portal hypertension in different age groups after a complete work-up (this includes the aetiologies identified after liver biopsy in patients with cryptogenic chronic liver disease). On comparison with adults aged 19-59 yr, elderly patients (>60 yr) had significantly higher proportion of cryptogenic chronic liver disease (P<0.001) and lesser proportion of alcohol related liver disease (P<0.005) and vascular liver disease (P<0.001). The proportion of patients with hepatitis virus induced liver disease was the same in both age groups.
Table II.
Age group-wise break-up of aetiology of portal hypertension, after complete aetiological evaluation (including liver biopsy), in 583 consecutive, new adult patients
Discussion
In this study, majority of patients were from middle socio-economic class, and cryptogenic chronic liver disease was found to be the predominant cause of portal hypertension, followed by chronic liver disease related to alcohol and hepatitis B. This is at variance to reports from other countries, where alcohol and hepatitis C were the main causes of portal hypertension6,7,8. In our study, among patients with cryptogenic chronic liver disease who underwent liver biopsy, commonest cause of portal hypertension identified after the biopsy was NCIPH; majority of cryptogenic chronic liver disease patients who did not have liver biopsy, had >1 risk factor for NAFLD, this could suggest NAFLD as a cause of portal hypertension in these patients.
In India, portal hypertension due to cryptogenic chronic liver disease could be caused by cirrhosis due to occult or prior hepatitis B infection, NAFLD or autoimmune disease or by NCIPH. Though a previous report from our centre noted serum HBV DNA positivity in only 3.3 per cent patients with cryptogenic chronic liver disease20, other studies from India have reported occult hepatitis B in up to 9 per cent patients with chronic liver disease21. All patients with cryptogenic chronic liver disease in the current study were HBsAg negative, however serum anti hepatitis B core antibody and serum HBV DNA were not done in all. Thus, the current study findings do not indicate the contribution of occult hepatitis B infection as the cause of chronic liver disease in the patients studied.
Of the 39 patients with cryptogenic chronic liver disease who had liver biopsy, cirrhosis due to NAFLD was found in five patients. In majority of patients (n=164) with cryptogenic chronic liver disease who did not have liver biopsy, a risk factor for NAFLD was found in 77 per cent of patients suggesting that NAFLD cirrhosis could be the cause for liver disease in these patients. However, liver biopsy was not done and risk factors for NAFLD were not assessed in all patients, this is a limitation of this study. Further, 21 per cent patients with cryptogenic chronic liver disease who underwent liver biopsy had autoimmune liver disease. Gupta et al22 found a prevalence of 3.4 per cent of autoimmune liver diseases in patients with chronic liver disease.
In an adult with idiopathic portal vein thrombosis, it is difficult to differentiate Extrahepaticportal vein obstruction (EHPVO) from portal vein thrombosis secondary to an intrahepatic pathology like NCIPH or cryptogenic cirrhosis. This is recognised as a difficult area to define1,23. In the present study, patients with portal vein thrombosis secondary to a known cause of liver disease (e.g. alcohol related chronic liver disease and portal vein thrombosis) were included in respective aetiology groups.
Similar to our prior study24, predominant diagnosis in patients with ‘cryptogenic’ intrahepatic portal hypertension after liver biopsy was NCIPH. Thus, NCIPH mimics cryptogenic cirrhosis, clinically and on investigations, and can only be differentiated by liver biopsy23. However, as all patients with cryptogenic chronic liver disease did not have liver biopsy, the aetiological break up in all patients with cryptogenic chronic liver disease is not known. NCIPH occurs secondary to microvascular occlusion of intra-hepatic small portal vein radicles. Multiple hypotheses regarding the pathogenesis have been proposed. One such hypothesis entails linking of gut disorders and subsequent hyper-coagulability in portal circulation25. Role of deficiency of ADAMTS 13 (a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13), a von Willebrand factor-cleaving protease, is also being actively explored26. The reason for clustering of NCIPH in India and in middle/lower socio-economic strata needs to be further explored27,28. In our study, of the 17 NCIPH patients, 14 were from middle and lower socio-economic strata.
Elderly patients comprised 14 per cent of our patients. Cryptogenic, alcohol, hepatitis B and hepatitis C related chronic liver disease were the commonest causes of portal hypertension among them.
Alcohol intake in India is steadily increasing, with decrease in the initiation age29. This alarming trend is noticed in many areas of the country29,30. In our study, alcohol intake was a contributory factor in 29 per cent of patients with portal hypertension, which is significantly more than a prior study from eastern India4. This may be a reflection of referral bias, socio-economic situation or can be a reflection of a changing trend.
Further studies on aetiology of portal hypertension in adults and in elderly are needed from different parts of India, especially to analyse variations in different socio-economic categories. Further studies are also needed to know the cause of cryptogenic chronic liver disease, the commonest cause of portal hypertension, noted in this study. This information will help guide steps to prevent portal hypertension in India.
Acknowledgment
The authors are grateful for funds received from the Fluid Research Fund at Christian Medical College (Vellore, India) for this study.
References
- 1.Okuda K. Non-cirrhotic portal hypertension: why is it so common in India? J Gastroenterol Hepatol. 2002;17:1–5. doi: 10.1046/j.1440-1746.2002.02660.x. [DOI] [PubMed] [Google Scholar]
- 2.Simon EG, Joseph AJ, George B, Zachariah UG, Jeyamani R, Eapen CE, et al. Aetiology of paediatric portal hypertension - experience of a tertiary care centre in South India. Trop Doct. 2009;39:42–4. doi: 10.1258/td.2008.080050. [DOI] [PubMed] [Google Scholar]
- 3.Poddar U, Thapa BR, Rao KL, Singh K. Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West? J Gastroenterol Hepatol. 2008;23:1354–7. doi: 10.1111/j.1440-1746.2007.05102.x. [DOI] [PubMed] [Google Scholar]
- 4.Ray G, Ghoshal UC, Banerjee PK, Pal BB, Dhar K, Pal AK, et al. Aetiological spectrum of chronic liver disease in eastern India. Trop Gastroenterol. 2000;21:60–2. [PubMed] [Google Scholar]
- 5.Verghese J, Navaneethan U, Venkatraman J. Clinical pattern of elderly cirrhosis: an Indian experience. Eur J Gastroenterol Hepatol. 2007;19:1031–3. doi: 10.1097/MEG.0b013e3281ca7034. [DOI] [PubMed] [Google Scholar]
- 6.Michitaka K, Nishiguchi S, Aoyagi Y, Hiasa Y, Tokumoto Y, Onji M Japan Etiology of Liver Cirrhosis Study Group. Etiology of liver cirrhosis in Japan: a nationwide survey. J Gastroenterol. 2010;45:86–94. doi: 10.1007/s00535-009-0128-5. [DOI] [PubMed] [Google Scholar]
- 7.Mendez-Sanchez N, Aguilar-Ramirez JR, Reyes A, Dehesa M, Juorez A, Castneda B, et al. Groupo de Estudio, Asociaon Mexicana de Hepatologyia. Etiology of liver cirrhosis in Mexico. Ann Hepatol. 2004;3:30–3. [PubMed] [Google Scholar]
- 8.Johnson EA, Spier BJ, Leff JA, Lucey MR, Said A. Optimising the care of patients with cirrhosis and gastrointestinal haemorrhage: a quality improvement study. Aliment Pharmacol Ther. 2011;34:76–82. doi: 10.1111/j.1365-2036.2011.04692.x. [DOI] [PubMed] [Google Scholar]
- 9.O’shea RS, Dasarathy S, McCullough AJ Practice Guideline Committee. Alcoholic liver disease. Hepatology. 2010;51:307–28. doi: 10.1002/hep.23258. [DOI] [PubMed] [Google Scholar]
- 10.Roberts EA, Schilsky ML. American Association for the Study of Liver Diseases; College of Gastroenterology. Diagnosis and treatment of Wilson disease: an update. Hepatology. 2008;47:2089–111. doi: 10.1002/hep.22261. [DOI] [PubMed] [Google Scholar]
- 11.Yeoman AD, Westbrook RH, Al-Chalabi T, Carey I, Heaton ND, Portmann BC, et al. Diagnostic value and utility of the simplified International Autoimmune Hepatitis Group (IAIHG) criteria in acute and chronic liver disease. Hepatology. 2009;50:538–45. doi: 10.1002/hep.23042. [DOI] [PubMed] [Google Scholar]
- 12.Bacon Br, Adams PC, Kowdley KV, Powell LW, Tavill AS. American Association for the Study of Live r Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328–43. doi: 10.1002/hep.24330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ. American Association for Study of Liver Diseases. Primary biliary cirrhosis. Hepatology. 2009;50:291–308. doi: 10.1002/hep.22906. [DOI] [PubMed] [Google Scholar]
- 14.Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, Gores GJ. American Association for the Study of Liver Diseases. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660–78. doi: 10.1002/hep.23294. [DOI] [PubMed] [Google Scholar]
- 15.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–23. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 16.Hillaire S, Bonte E, Denninger MH, Casadevall N, Cadranel JF, Lebrec D, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patients. Gut. 2002;51:275–80. doi: 10.1136/gut.51.2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mishra D, Singh HP. Kuppuswamy's socioeconomic status scale--a revision. Indian J Pediatr. 2003;70:273–4. doi: 10.1007/BF02725598. [DOI] [PubMed] [Google Scholar]
- 18.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.Tellez-Avila FI, Sanchez-Avila F, Garcia-Saenz-de-Sicilia M, Chavez-Tapia NC, Franco-Guzman AM, Lopez-Arce G, et al. Prevalence of metabolic syndrome, obesity and diabetes type 2 in cryptogenic cirrhosis. World J Gastroenterol. 2008;14:4771–5. doi: 10.3748/wjg.14.4771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radhakrishnan S, Abraham P, Raghuraman S, Kabrawala M, Eapen CE, Sridharan G, et al. Infrequent occurrence of silent HBV infection among Indian patients with chronic liver disease. Indian J Gastroenterol. 2001;20:87–9. [PubMed] [Google Scholar]
- 21.Chaudhuri V, Tayal R, Nayak B, Acharya SK, Panda SK. Occult hepatitis B virus infection in chronic liver disease: full-length genome and analysis of mutant surface promoter. Gastroenterology. 2004;127:1356–71. doi: 10.1053/j.gastro.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Gupta R, Agarwal SR, Jain M, Malhotra V, Sarin SK. Autoimmune hepatitis in the Indian subcontinent: 7 years experience. J Gastroenterol Hepatol. 2001;16:1144–8. doi: 10.1046/j.1440-1746.2001.02602.x. [DOI] [PubMed] [Google Scholar]
- 23.Madhu K, Ramakrishna B, Zachariah U, Eapen CE, Kurian G. Non-cirrhotic intrahepatic portal hypertension. Gut. 2008;57:1529. doi: 10.1136/gut.2008.165480. [DOI] [PubMed] [Google Scholar]
- 24.Madhu K, Avinash B, Ramakrishna B, Eapen CE, Shyamkumar NK, Zachariah U, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension: common cause of cryptogenic intrahepatic portal hypertension in a Southern Indian tertiary hospital. Indian J Gastroenterol. 2009;28:83–7. doi: 10.1007/s12664-009-0030-3. [DOI] [PubMed] [Google Scholar]
- 25.Eapen CE, Nightingale P, Hubscher SG, Lane PJ, Plant T, Velissaris D, et al. Non-cirrhotic intrahepatic portal hypertension: associated gut diseases and prognostic factors. Dig Dis Sci. 2011;56:227–35. doi: 10.1007/s10620-010-1278-2. [DOI] [PubMed] [Google Scholar]
- 26.Mackie I, Eapen CE, Neil D, Lawrie AS, Chitolie A, Shaw JC, et al. Idiopathic noncirrhotic intrahepatic portal hypertension is associated with sustained ADAMTS13 Deficiency. Dig Dis Sci. 2011;56:2456–65. doi: 10.1007/s10620-011-1729-4. [DOI] [PubMed] [Google Scholar]
- 27.Sarin SK. Non-cirrhotic portal fibrosis. Gut. 1989;30:406–15. doi: 10.1136/gut.30.3.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dhiman RK, Chawla Y, Vasishta RK, Kakkar N, Dilawari JB, Trehan MS, et al. Non-cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol. 2002;17:6–16. doi: 10.1046/j.1440-1746.2002.02596.x. [DOI] [PubMed] [Google Scholar]
- 29.Das SK, Balakrishnan V, Vasudevan DM. Alcohol: its health and social impact in India. Natl Med J India. 2006;19:94–99b. [PubMed] [Google Scholar]
- 30.Alcohol atlas of India. Chennai: IAPA; 2008. [accessed on April 13, 2013]. Indian Alcohol Policy Alliance (IAPA) Available from: http://www.indianalcoholpolicy.org/alcohol_atlas_download.html . [Google Scholar]


