Abstract
OBJECTIVES
The goal of this study was to determine the ability of a single, resting high-sensitivity troponin T (hsTnT) measurement to predict abnormal myocardial perfusion imaging (MPI) in patients presenting with acute chest pain to the emergency department (ED).
BACKGROUND
HsTnT assays precisely detect very low levels of troponin T, which may be a surrogate for the presence and extent of myocardial ischemia.
METHODS
We included all patients from the ROMICAT I (Rule Out Myocardial Infarction Using Computer Assisted Tomography) trial, an observational cohort study, who underwent both single-photon emission computed tomography (SPECT)-MPI stress testing and 64-slice computed tomography angiography (CTA) and in whom hsTnT measurements were available. We assessed the discriminatory value of hsTnT for abnormal SPECT-MPI and the association of reversible myocardial ischemia by SPECT-MPI and the extent of coronary atherosclerosis by CTA to hsTnT levels.
RESULTS
Of the 138 patients (mean age 54 ± 11 years, 46% male), 19 (13.7%) had abnormal SPECT-MPI. Median hsTnT levels were significantly different between patients with normal and abnormal SPECT-MPI (9.41 pg/ml [interquartile range (IQR): 5.73 to 19.20 pg/ml] vs. 4.89 pg/ml [IQR: 2.34 to 7.68 pg/ml], p = 0.001). Sensitivity of 80% and 90% to detect abnormal SPECT-MPI was reached at hsTnT levels as low as 5.73 and 4.26 pg/ml, respectively. Corresponding specificity was 62% and 46%, and negative predictive value was 96% and 96%, respectively. HsTnT levels had good discriminatory ability for prediction of abnormal SPECT-MPI (area under the curve: 0.739, 95% confidence interval: 0.609 to 0.868). Both reversible myocardial ischemia and the extent of coronary atherosclerosis (combined model r2 = 0.19 with partial of r2 = 0.12 and r2 = 0.05, respectively) independently and incrementally predicted the measured hsTnT levels.
CONCLUSIONS
In patients with acute chest pain, myocardial perfusion abnormalities and coronary artery disease are predicted by resting hsTnT levels. Prospective evaluations are warranted to confirm whether resting hsTnT could serve as a powerful triage tool in chest pain patients in the ED before diagnostic testing and improve the effectiveness of patient management.
Keywords: coronary computed tomographic angiography, high-sensitivity troponin T, myocardial perfusion imaging, single-photon emission computed tomography
Traditionally, cardiac troponin T (TnT) has been considered a specific marker for myocardial necrosis and thus represents a diagnostic hallmark for the diagnosis of acute myocardial infarction as well as a predictor of major adverse cardiac events (1,2). Although conventional TnT assays were unreliable for the detection of troponin <0.01 ng/ml, a novel, so-called “high-sensitivity” assay demonstrates greatly improved precision and thus permits the reliable detection of much lower concentrations of TnT with great precision (99th percentile of hsTnT for a normal reference population: 13 pg/ml, imprecision <10%) (3–6). Hitherto, the new assays detect measurable amounts of TnT at lower levels than those pre-specified for myocardial necrosis, even in patients without symptoms of cardiovascular disease, and predict cardiovascular morbidity and mortality in patients with and without overt coronary artery disease (CAD) (7–10). In addition, Sabatine et al. (11) recently demonstrated a stress-induced rise in cardiac troponin I levels as measured with a high-sensitivity assay that correlated with reversible myocardial ischemia as demonstrated by single-photon emission computed tomography–myocardial perfusion imaging (SPECT-MPI). These observations led to the intriguing hypothesis that these new assays may permit tracking of CAD development over time and also permit the detection of acute myocardial ischemia. This hypothesis has been supported by our previous results demonstrating that hsTnT assays permit improved detection of acute coronary syndromes (ACS) as compared with conventional TnT among patients presenting with acute chest pain to the emergency department (ED), because patients later classified as having unstable angina are identified sooner using hsTnT (12). In addition, this study demonstrated a close association of hsTnT with cardiac structure and function as determined by computed tomography (CT).
To further determine the potential role of hsTnT to risk stratify patients presenting with acute chest pain to the ED, but without objective evidence of ACS on admission, we assessed the discriminatory power of resting hsTnT levels to predict abnormal rest and stress SPECT-MPI. In addition, we assessed whether both myocardial ischemia and coronary atherosclerosis independently predict hsTnT, which would establish hsTnT as a surrogate marker for myocardial injury both in patients with nonobstructive or obstructive CAD.
METHODS
Patient population
Details of the ROMICAT (Rule Out Myocardial Infarction Using Computer Assisted Tomography) study have been previously reported (13). Briefly, ROMICAT was a double-blinded, single-center, prospective observational cohort study of consecutive adult patients at low-to-intermediate likelihood of ACS presenting to the ED of Massachusetts General Hospital with acute chest pain, and whose initial electrocardiogram (ECG) and biomarkers were not indicative of a high likelihood for ACS. The enrollment period was a cumulative period of 18 months ending May 2007. Exclusion criteria were atrial fibrillation, serum creatinine >1.3 mg/dl, and personal history of CAD. All eligible patients who consented underwent ECG-gated contrast-enhanced 64-slice multidetector CT. All patients and caregivers were blinded to the findings of the CT. Patients received standard of care to rule out ACS during index hospitalization, including serial ECGs, biomarkers, and cardiac testing (stress test or cardiac catheterization), as clinically utilized by the physicians caring for the patient. The institutional review board approved the study protocol, and all patients provided written informed consent.
For this study, we only included patients who underwent clinically indicated rest and stress SPECT-MPI for risk stratification during index hospitalization. We excluded patients with myocardial infarction during index hospitalization.
Cardiac biomarker testing
A sample of blood for biomarker testing (high-sensitivity troponin T [hsTnT]) was taken at the time of computed tomography angiography (CTA), at a median of 4.2 h from initial presentation. Blood was immediately processed and frozen at −80°C, until it was assayed with a pre-commercial hsTnT assay (Roche Diagnostics, Penzberg, Germany) on an Elecsys 2010 platform (14–16). Given enhanced sensitivity, the high-sensitivity assay is reported with units of picograms/milliliter (rather than nanograms/ milliliter for conventional troponin T assays) and is reported to have a coefficient of variation of 8% at 10 pg/ml (14). For the present analysis, hsTnT had an inter-run coefficient of variation of 3.6% and 2.9% at concentrations of 42 and 2,820 pg/ml, respectively. All blood was tested on the first freeze-thaw cycle.
SPECT-MPI
SPECT-MPI using Tc-99m-MIBI was performed according to American College of Cardiology/American Heart Association image acquisition guidelines using a standard 1-day protocol (17). The median time between hsTnT draw and CTA (which were both performed at the same time) and SPECT was 12 h. The patient was first injected with sestamibi at rest, and ungated images were obtained. Subsequently, sestamibi was injected at peak stress, and gated SPECT images were obtained 30 to 60 min later. Average isotope doses for sestamibi were in the range of 9 to 11 mCi for the rest images and 27 to 33 mCi for the stress images. Patients performed a treadmill exercise or had pharmacological stress testing with adenosine if unable to exercise. Beta-blockers were held before stress testing for all patients. Patients were instructed not to consume coffee or other products containing caffeine for 24 h before the test. During both types of stress testing, heart rate, blood pressure, and 12-lead ECG were recorded at baseline and every minute thereafter, and as needed appropriately. One minute before completion of symptom-limited exercise (test endpoint as defined in the current practice guideline [18]), radiotracer was injected intravenously. A dual-head Siemens gamma camera (E-CAM or C-CAM, Siemens Medical Solutions, Forchheim, Germany) equipped with a low-energy, high-resolution collimator (32 views per camera head in 64 × 64 matrix) was used for image acquisition.
The nuclear images were analyzed separately by 2 independent readers who were blinded to the clinical history, the CTA results, and the patient’s outcome. Readers were also blinded to each other’s readings. Discrepancies were adjudicated by a third reader. Analysis was done in a semiquantitative fashion using a standard 17-segment model and a 5-point scoring system (19) using commercially available SPECT image analysis program (4DM, Ann Arbor, Michigan). Analysis was performed blinded to the results of CTA and cardiac biomarkers. Global summed scores were computed for the stress images (summed stress score [SSS], reflecting the combined extent and severity of ischemia plus scar) and rest images (summed rest score [SRS], reflecting the extent and severity of myocardial scar), as well as their difference (summed difference score [SDS], reflecting the combined extent and magnitude of myocardial ischemia). An MPI result was considered to be abnormal if the SSS was ≥4 and/or the SDS ≥1 (primary endpoint) (20,21). Transient ischemic dilation (TID) was estimated from the semiautomated analysis of the ratio of the left ventricle volume on rest and stress MPI images.
CTA
CT imaging was performed using a standard 64-slice multidetector CT coronary angiography scanner (Sensation 64, Siemens Medical Solutions) protocol that was acquired at end-inspiration and included the administration of sublingual nitroglycerin (0.6 mg) and intravenous beta-blocker (metoprolol 5 to 20 mg) for those with a baseline heart rate >60 beats/min and no other contraindications. A test bolus protocol was used to determine the optimal timing of contrast injection (20 ml of contrast agent followed by 40 ml of saline, flow rate of 5 ml/s). Contrast agent (80 to 100 ml, Iodixanol 320 g/cm3, Visipaque, GE Healthcare, Princeton, New Jersey) with 40 ml of saline was injected intravenously at a rate of 5 ml/s. CT images were acquired in spiral mode, gantry rotation time of 330 ms, 64 × 0.6-mm slice collimation, tube voltage of 120 kV, effective tube current of 850 to 950 mAs, with ECG-correlated tube current modulation when appropriate. For coronary artery assessment, axial images were reconstructed using a medium-sharp convolution kernel with a slice thickness of 0.75 mm and increment of 0.4 mm.
For the detection of CAD, the 17-segment model based on the American Heart Association classification with the addition of the posterior left ventricular branch as segment 16 and the ramus intermedius as segment 17 was used (22). For each of the 17 segments, coronary atherosclerotic plaque, plaque composition (calcified, mixed, or noncalcified), and significant stenosis (defined as luminal narrowing >50% diameter) was visually classified as either present or absent as previously described and determined by 2-reader consensus using a Leonardo workstation (Siemens Medical Solutions) as previously validated (23). The extent of coronary plaque burden was scored from 0 to 17 and treated as a continuous variable.
Statistical analysis
Baseline demographics of patients with normal and abnormal stress tests were compared with the Fisher exact test for categorical variables and 1-way analysis of variance or Kruskal-Wallis test for continuous variables. For pairwise comparisons, the Student t test or Wilcoxon rank sum test was used.
The Wilcoxon rank sum test was used to determine the significance of differences in hsTnT levels between normal and abnormal SPECT-MPI patients. The probability of having an abnormal stress test at different hsTnT levels was calculated using unadjusted logistic regression. In order to determine cutoff values of hsTnT representing different sensitivities (60%, 70%, 80%, 90%) for abnormal SPECT-MPI, receiver-operating characteristic curves were constructed, and the area under the curve (AUC) (24) was estimated. Specificity, positive predictive value (PPV) and negative predictive value (NPV) including 95% confidence intervals [CI] for an abnormal SPECT-MPI were determined for each level of sensitivity. The C-statistic values, which are equal to the AUC for each level of sensitivity, were calculated. Following the intention-to-treat principle, the number of true negative stress tests that could be saved for each false negative test (hsTnT below the cutoff, but with an abnormal SPECT-MPI) was calculated for each level of sensitivity.
Log-transformed hsTnT levels were normally distributed and were used to assess associations between hsTnT and SPECT-MPI, coronary CTA, and cardiovascular risk factors. Univariate linear regression analysis was performed, and parameters with p ≤ 0.1 were included in multivariate analysis. The baseline model (Model 1) adjusted the association of hsTnT and cardiac stress testing for age and sex (strong association of these with hsTnT in prior studies) (6). In a second model, we further adjusted for other traditional CAD risk factors.
The association of reversible myocardial ischemia (SDS) and atherosclerotic plaque burden (number of coronary segments with any plaque) with hsTnT was assessed independently using linear regression analysis. Adjusted and partial r-squares were calculated to determine the extent to which variation of log-transformed hsTnT levels could be explained by reversible ischemia and plaque burden. Any increase in adjusted r-square was interpreted as incremental improvement in the model.
All of the statistical analyses were performed with SAS software (version 9.2, SAS Institute, Cary, North Carolina). All probability values were 2-sided, with a level of significance of <0.05.
RESULTS
Study population
We included 138 patients with acute chest pain (mean age 54 ± 11 years, 46% male) who underwent clinically indicated exercise treadmill testing SPECT-MPI (n = 99) or adenosine SPECT-MPI (n = 39) for risk stratification during index hospitalization. In 7 patients, hsTnT values were missing, including in 1 patient with abnormal myocardial perfusion by SPECT-MPI. HsTnT levels, measured on average 4 h after presentation, were low (median: 5.43 pg/ml [inter-quartile range (IQR): 2.42 to 8.71 pg/ml], range: 0 to 42.4 pg/ml). The majority (86%) had values below the 99th percentile of hsTnT for a normal reference population (13 pg/ml).
HsTnT and SPECT-MPI
Overall, 19 (13.7%) patients had abnormal SPECT-MPI, among them 10 patients with SDS ≥1 and 9 with SSS ≥4. Seven of the 10 patients with SDS ≥1 also had SSS ≥4. Mean SSS, SRS, and SDS were 1.23 ± 4.46, 0.82 ± 3.21, and 0.41 ± 1.81, respectively. Mean left ventricular ejection fraction was 65.5 ± 11.4% and mean TID was 0.97 ± 0.16. Seven of the 19 patients (5 with abnormal SDS and 2 with only abnormal SSS) also had significant stenosis on CTA or invasive angiography (if available). The stenosis location correlated with the location of the perfusion defect in all 7 patients. There were no differences in cardiovascular risk profile, medication use, and extent of plaque by CTA between patients with normal (n = 119, 86%) and abnormal (n = 19, 14%) SPECT-MPI (Table 1). However, significantly more patients with abnormal SPECT-MPI had significant coronary stenosis than those with a normal SPECT-MPI (p = 0.003).
Table 1.
Baseline Characteristics of the Study Population
| Characteristic | Overall Cohort (N =138) | Normal SPECT-MPI (n =119) | Abnormal SPECT-MPI (n =19) | p Value* |
|---|---|---|---|---|
| Age, yrs | 54 ± 11 | 53 ± 11 | 56 ± 12 | 0.26 |
| Male | 63 (46) | 58 (49) | 5 (26) | 0.08 |
| Cardiovascular risk factors | ||||
| Body mass index, kg/m2 | 30 ± 6 | 30 ± 6 | 30 ± 6 | 0.85 |
| Diabetes mellitus | 16 (12) | 11 (9) | 5 (26) | 0.05 |
| Hypertension | 56 (41) | 50 (42) | 6 (32) | 0.46 |
| Hyperlipidemia | 59 (43) | 51 (43) | 8 (42) | 1.00 |
| Family history of CAD | 36 (26) | 33 (28) | 3 (16) | 0.40 |
| Tobacco use | 40 (29) | 33 (28) | 7 (37) | 0.42 |
| Medications at presentation | ||||
| Aspirin | 44 (32) | 38 (32) | 6 (32) | 1.00 |
| Statin | 46 (33) | 40 (34) | 6 (32) | 1.00 |
| Nitroglycerin | 4 (3) | 3 (3) | 1 (5) | 0.45 |
| Beta-blocker | 32 (23) | 31 (26) | 1 (5) | 0.07 |
| TIMI score | 0.12† | |||
| 0 Points | 63 (46%) | 57 (48%) | 6 (32%) | |
| 1 Point | 50 (36%) | 43 (36%) | 7 (37%) | |
| 2 Points | 19 (14%) | 14 (11%) | 5 (26%) | |
| 3 Points | 6 (4%) | 5 (4%) | 1 (5%) | |
| Coronary CTA | ||||
| Presence of any plaque | 72 (52) | 61 (51) | 11 (58) | 0.63 |
| Segments with any plaque | 1 [0–3] | 1 [0–3] | 1 [0–7] | 0.21 |
| Presence of significant stenosis | 13 (9) | 7 (6) | 6 (32) | 0.003 |
| Biomarkers (other than hsTnT) | ||||
| hsCRP, pg/ml | 1.44 [0.71–2.98] | 1.42 [0.69–2.93] | 1.66 [1.82–3.34] | 0.85 |
| NT-proBNP, pg/ml | 41 [21–100] | 40 [20–102] | 52 [32–100] | 0.25 |
Values are mean ± SD, median [interquartile range], or n (%).
p value for differences between normal and abnormal stress testing (includes exercise treadmill and adenosine single-photon emission computed tomography-myocardial perfusion imaging (SPECT-MPI).
Mantel-Haenszel trend test.
CAD = coronary artery disease; CTA = computed tomography angiography; hsCRP = high-sensitivity C-reactive protein; hsTnT = high-sensitivity troponin T; NT-proBNP = amino-terminal pro–B-type natriuretic peptide; TIMI = Thrombolysis In Myocardial Infarction.
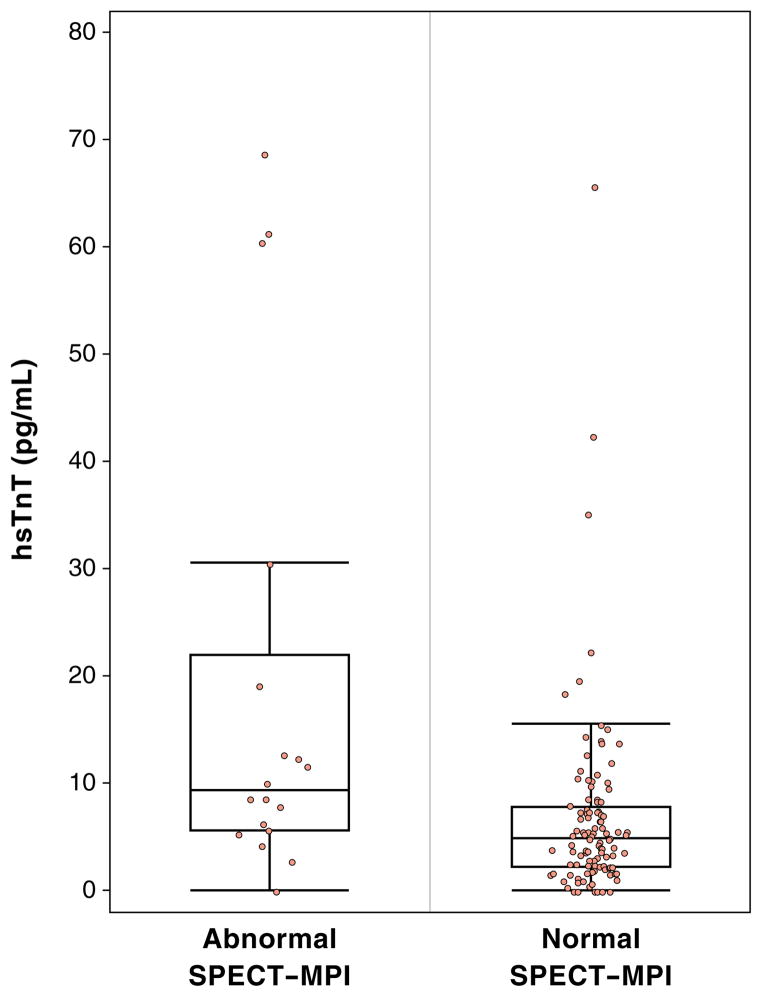
Median hsTnT levels were twice as high in patients with abnormal SPECT-MPI compared with those with normal SPECT-MPI (9.41 pg/ml [IQR: 5.73 to 19.20] vs. 4.89 pg/ml [IQR: 2.34 to 7.68], p = 0.001) (Fig. 1). This difference was independent of age and sex and other traditional cardiovascular risk factors (p = 0.02).
Figure 1. HsTnT Levels Between Patients With Normal and Abnormal SPECT-MPI.
Median high-sensitivity troponin T (hsTnT) levels were significantly higher in patients with abnormal single-photon emission computed tomography–myocardial perfusion imaging (SPECT-MPI) compared with those with normal SPECT-MPI (9.41 pg/ml [interquartile range (IQR): 5.73 to 19.20 pg/ml] vs. 4.89 pg/ml [IQR: 2.34 to 7.68 pg/ml], p = 0.001).
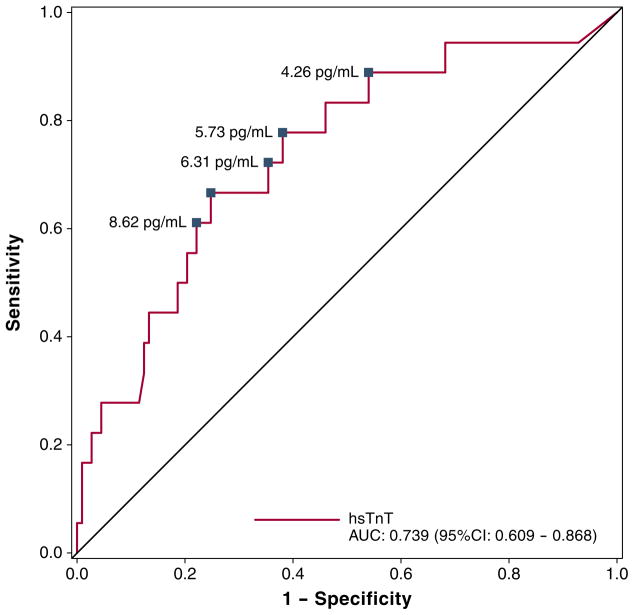
The probability of having an abnormal SPECT-MPI increased from 9% (95% CI: 5% to 16%) at a hsTnT value of 3 pg/ml, to 13% (95% CI: 8% to 21%) for a hsTnT value of 10 pg/ml, and to 21% (95% CI: 13% to 33%) for a hsTnT level of 20 pg/ml. The odds for abnormal SPECT-MPI increased by 2-fold per doubling of hsTnT levels (odds ratio: 2.19 [95% CI: 1.41 to 3.39], p = 0.002). Consequently, hsTnT had good discriminatory value for abnormal SPECT-MPI (AUC: 0.739, 95% CI: 0.609 to 0.868) (Fig. 2).
Figure 2. ROC Curve for hsTnT Values for Prediction of Abnormal SPECT-MPI Results.
HsTnT had good discriminatory value for abnormal SPECT-MPI (area under the curve [AUC]: 0.739, 95% confidence interval [CI]: 0.609 to 0.868). The hsTnT cutoffs for sensitivities of 60%, 70%, 80%, and 90% are marked on the receiver-operating characteristic (ROC) curve. Other abbreviations as in Figure 1.
The odds for abnormal SPECT-MPI increased 4-fold per doubling of hsTnT levels (odds ratio: 4.40 [95% CI: 1.93 to 10.00], p = 0.0004) among patients with abnormal SPECT-MPI who also had significant stenosis.
To provide clinically relevant thresholds, we determined the specificity, PPV, and NPV of hsTnT for SPECT-MPI testing results at predefined levels of sensitivity of 60%, 70%, 80%, and 90%, as well as the diagnostic accuracy of hsTnT at values corresponding to the 99th percentile of a healthy reference population (13 pg/ml) (6) (Table 2). High sensitivities of 80% and 90% for abnormal SPECT-MPI still rendered reasonable specificities of 62% and 46%, respectively, but most importantly, resulted in a consistently high NPV of 96%. Remarkably, the 99th percentile of a healthy reference population (13 pg/ml) rendered excellent specificity and NPV (96% each) but poor sensitivity (26%).
Table 2.
Utility of Various HsTnT Cutoff Values for Identifying Chest Pain Patients With Abnormal SPECT-MPI Results
| Cut Points for HsTnT (pg/ml) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |
|---|---|---|---|---|---|
| Target sensitivity | |||||
| 60% | 8.62 | 61% (35–83) | 78% (69–85) | 31% (16–48) | 93% (85–97) |
| 70% | 6.31 | 72% (47–90) | 65% (55–73) | 25% (14–38) | 94% (86–98) |
| 80% | 5.73 | 78% (52–94) | 62% (52–71) | 25% (14–38) | 95% (87–97) |
| 90% | 4.26 | 89% (65–99) | 46% (37–56) | 21% (12–32) | 96% (87–100) |
| 99th percentile of a reference group (6) | 13.00 | 28% (10–53) | 98% (81–94) | 28% (10–53) | 88% (81–94) |
CI = confidence interval; hsTnT = high-sensitivity troponin T; NPV = negative predictive value; PPV = positive predictive value; SPECT-MPI = single-photon emission computed tomography–myocardial perfusion imaging.
Translating these numbers according to the intention-to-treat principle, 27.0, 18.5, 15.6, and 13.6 true negative SPECT-MPI tests could be saved at sensitivities of 60%, 70%, 80%, and 90%, respectively, for a penalty of 1 false negative test (abnormal SPECT-MPI).
Myocardial ischemia and coronary atherosclerosis independently predict hsTnT
To assess whether hsTnT is a marker of both upstream (coronary atherosclerosis) and downstream (myocardial ischemia) aspects of cardiovascular disease, we determined whether both are associated with elevated hsTnT levels. In univariate analysis, SSS, SRS, and SDS, as well as left ventricular ejection fraction and TID ratio, were significantly associated with hsTnT (β= 0.07, 0.08, and 0.19; −0.02 and 1.24, respectively, all p ≤ 0.01) (Table 3). In adjusted analysis, SSS, SRS, and SDS remained significant predictors of hsTnT (β = 0.06, 0.07, and 0.16, respectively, all p < 0.005).
Table 3.
SPECT-MPI Stress Test Parameters as Predictors of Log-Transformed HsTnT Concentrations
| SPECT-MPI (Both Exercise and Adenosine, N = 138)
| ||||||
|---|---|---|---|---|---|---|
| SPECT Parameters | Univariate
|
Multivariate (Model 1)
|
Multivariate (Model 2)
|
|||
| β | p Value | β | p Value | β | p Value | |
| SSS | 0.07 | <0.0001 | 0.07 | <0.0001 | 0.06 | 0.0002 |
| SRS | 0.08 | 0.0008 | 0.07 | 0.001 | 0.07 | 0.005 |
| SDS | 0.19 | <0.0001 | 0.17 | <0.0001 | 0.16 | <0.0001 |
| LVEF by gated SPECT | −0.02 | 0.003 | −0.02 | 0.004 | −0.02 | 0.01 |
| TID ratio | 1.24 | 0.01 | 1.04 | 0.02 | 0.84 | 0.07 |
Model 1 was adjusted for age and sex; Model 2 for age, sex, diabetes, and hypertension.
LVEF = left ventricular ejection fraction; SDS = summed difference score; SRS = summed rest score; SSS = summed stress score; TID = transient ischemic dilation; other abbreviations as in Table 2.
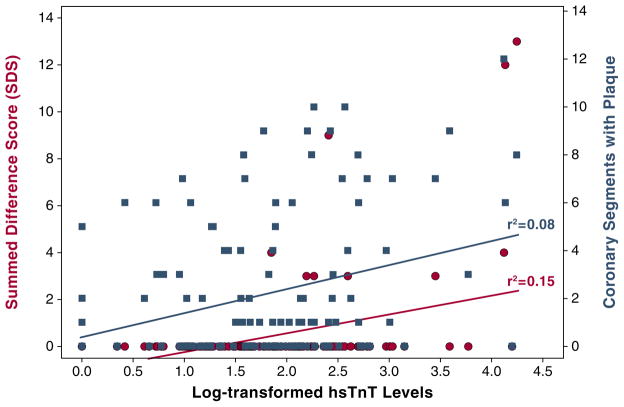
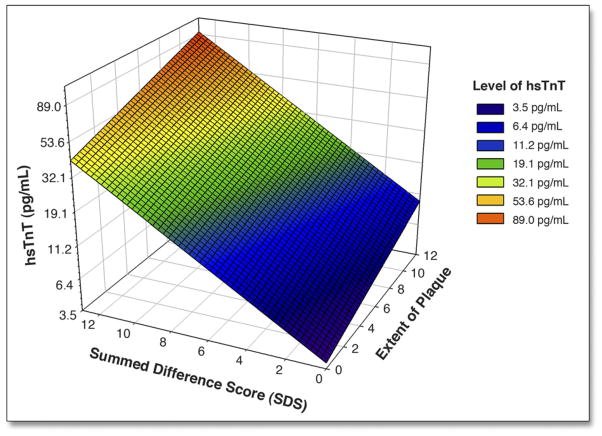
Among a total of 2,346 CTA segments from 138 patients assessed for plaque burden, 78 segments (3.3%) were considered indeterminate. In separate linear regression models, both the extent of reversible myocardial ischemia (SDS) and extent of coronary atherosclerosis were associated with hsTnT (SDS r2 = 0.15, p < 0.0001; plaque r2 = 0.08, p < 0.0004) (Fig. 3). Combined information on myocardial ischemia and coronary atherosclerosis explained nearly 20% of the variability in hsTnT, and the 2 variables were independent of each other (combined model r2 = 0.19 with partial r2 = 0.12 for SDS and partial r2 = 0.05 for plaque) (Fig. 4). Notably, addition of significant coronary disease (>50% stenosis on CTA) to the model did not result in improvement (model r2 = 0.18). However, analysis stratified by plaque composition suggested that mixed plaque was significantly associated with hsTnT levels (β = 0.17, p = 0.02), whereas noncalcified (β = 0.015, p = 0.87) and calcified (β = 0.07, p = 0.06) plaque were not.
Figure 3. Correlation of HsTnT With Extent of Reversible Myocardial Ischemia as Well as With Coronary Atherosclerotic Plaque.
The levels of log-transformed high-sensitivity troponin T (hsTnT) were correlated separately to summed difference score (SDS) (red circles), a measure of reversible myocardial ischemia, and to coronary segments containing any plaque (blue squares), a measure of atherosclerotic plaque burden. The correlation coefficients were r2 = 0.15 (p < 0.0001) and r2 = 0.08 (p = 0.0004), respectively.
Figure 4. Association of Estimated HsTnT Levels With Reversible Myocardial Ischemia and Coronary Plaque Extent.
The levels of log-transformed high-sensitivity troponin T (hsTnT) were estimated with a linear regression model using the extent of reversible myocardial ischemia (summed difference score [SDS]) and the number of coronary artery segments containing any atherosclerotic plaque as predictors. For better clinical interpretation, the labeling of the y-axis was back-transformed from log-hsTnT levels into hsTnT levels with a unit of picograms/milliliter. Combined information on myocardial ischemia and coronary atherosclerosis explained nearly 20% of the variability in hsTnT (r2 = 0.19), and the 2 variables were independent of each other. The estimated levels of hsTnT are illustrated by different colors as shown in the color key.
Furthermore, hsTnT levels in those with abnormal SPECT-MPI increased with the presence and severity of CAD: patients with abnormal SPECT-MPI and matching stenosis on CTA (n = 7, 30.5 pg/ml [IQR: 8.62 to 61.3]), patients with abnormal SPECT-MPI and matching stenosis who were revascularized (n = 4, 60.9 pg/ml [IQR: 36.1 to 65 pg/ml]), and patients with abnormal SPECT-MPI, but without significant CAD (n = 12, 8.00 pg/ml [IQR: 5.4 to 12.4 pg/ml]) as compared with those with normal SPECT-MPI (4.89 pg/ml [IQR: 2.34 to 7.68 pg/ml]), all p < 0.03.
DISCUSSION
In this substudy of ROMICAT I, we assessed the diagnostic accuracy of a single hsTnT measurement for the detection of abnormal rest stress SPECT-MPI and CAD in patients presenting to the ED with acute chest discomfort, but without objective evidence for ACS. We found that hsTnT levels measured on average 4 h after ED presentation were significantly higher in abnormal as compared with normal SPECT-MPI patients, independent of age, sex, and other cardiovascular risk factors. Most importantly, hsTnT had excellent NPV (96%) for normal SPECT-MPI while maintaining reasonable PPV and specificity. The discriminatory value of hsTnT was very good (AUC: 0.768). For example, at a sensitivity level of 90%, hsTnT correctly predicted 16 normal SPECT-MPI at a penalty of 1 abnormal SPECT-MPI. These results are supported by subanalyses demonstrating the independent association of hsTnT with both reversible myocardial ischemia and the extent of CAD. Moreover, whereas hsTnT levels were significantly higher in patients with abnormal SPECT-MPI compared with normal SPECT-MPI patients, the level of hsTnT in those with abnormal SPECT-MPI increased with the presence and severity of CAD. The fact that mixed plaque was associated with high hsTnT levels suggests that hsTnT may be a predictor of culprit lesions for unstable angina pectoris. Overall, these data suggest that early resting hsTnT could serve as a powerful triage tool in chest pain patients in the ED before diagnostic testing and thus could improve the effectiveness of patient management.
HsTnT for management of acute chest pain patients
The major finding of this double-blinded cross-sectional cohort study is that resting hsTnT levels drawn about 4 h after ED presentation, but about 12 h before stress testing, predict abnormal myocardial perfusion independent of cardiovascular risk factors or time of presentation to ED after onset of symptoms. The predictive ability occurs at very low levels of hsTnT (9.41 pg/ml vs. 4.89 pg/ml, p = 0.001 for normal vs. abnormal SPECT-MPI), well below detection levels of conventional TnT and the 99th percentile of hsTnT in a healthy reference population (6). Excellent discriminatory power (AUC: 0.739, 95% CI: 0.609 to 0.868) was maintained at hsTnT values between 4 and 8 pg/ml, corresponding to sensitivities of 60% to 90%. Most importantly, hsTnT rendered an excellent NPV of 96% while maintaining fair specificity and PPV (i.e., 90% sensitivity, 46% specificity, 21% PPV). This means that hsTnT can be utilized to predict abnormal SPECT results.
Overall, our findings suggest that early resting hsTnT may improve the effectiveness of the management of patients with acute chest pain and low-to-intermediate risk for ACS. Given the low prevalence of abnormal SPECT-MPI and ACS in this population and the risks and costs associated with diagnostic testing, early hsTnT testing may eliminate the need for imaging in a substantial number of patients who currently undergo 1 or more diagnostic imaging tests. If confirmed in prospective evaluations, a substantial fraction of patients with acute chest pain may be eligible for immediate and safe discharge by utilizing a strategy involving hsTnT for risk stratification.
HsTnT, myocardial ischemia, and CAD
Recently published data suggest that hsTnT is a marker for cardiac structure and function (12) and potentially vulnerable coronary atherosclerotic plaque (24). Thus, in this study, we hypothesized that very low levels of hsTnT, well below established cutoffs for myocardial infarction, can serve as a composite marker of both reversible myocardial ischemia and extent and composition of CAD. Our findings support this hypothesis, as both the presence of mixed plaque and reversible ischemia were significantly and independently associated with hsTnT levels. This could provide a mechanistic explanation for previous observations demonstrating that mixed plaque is the primary driver of the association of plaque burden with cardiovascular events (25,26). Taken together with other studies, our data generate the hypothesis that increased hsTnT may be a result of provocable ischemia both in the presence and absence of significant coronary disease, potentially via plaque rupture with distal embolization (Fig. 5).
Figure 5. Various Pathophysiological Mechanisms for the Release of HsTnT in the Circulation.
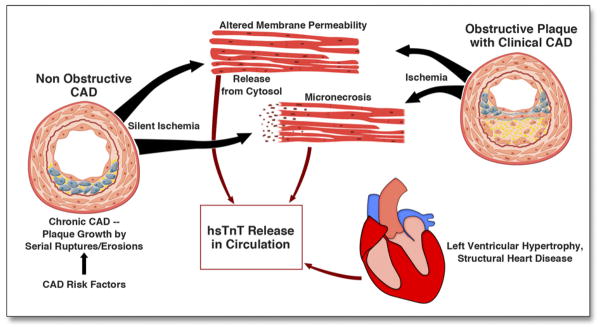
CAD = coronary artery disease; HsTnT = high-sensitivity troponin T.
The source and nature for detectable hsTnT levels remain debated, but there is agreement that they do not represent the traditional level of myocardial necrosis seen as a result of thrombotic occlusion (27). More likely, very low levels of circulating troponin may represent myocyte stress or damage (28), possibly as a result of changes in cell membrane permeability (29). Stress-induced myocardial ischemia leading to a quantifiable rise in high-sensitivity troponin I has been recently demonstrated in patients with stable angina (11). Our findings extend this observation because we demonstrate a strong association of resting pre-stress hsTnT levels with reversible myocardial ischemia in acute chest pain patients.
Furthermore, hsTnT may constitute, not only an attractive diagnostic and prognostic marker in patients with acute chest pain presenting to the ED, but also a potential therapeutic target for pharmacological interventions in primary and secondary prevention strategies.
Study limitations
In this study, hsTnT testing was performed contemporaneously with the CT scan and on average 4 h after ED presentation and 12 h before cardiac stress testing. Thus, the value of earlier or serial hsTnT for risk stratification as suggested previously (30,31) could not be established. In addition, a pre-commercial hsTnT assay was used that permitted detection of lower hsTnT levels than a commercially available assay. However, the reproducibility of low hsTnT concentrations may be limited. Our results are not generalizable to the overall population of patients presenting with acute chest pain to the ED, because this was a single-center study with enrollment limited to weekday daytime hours that excluded patients with prior CAD and enrolled very few elderly patients. Our study was a cross-sectional observational study and thus is limited to generating a hypothesis.
CONCLUSIONS
In acute chest pain patients undergoing SPECT imaging for risk assessment, myocardial perfusion abnormalities, as well as the extent of CAD, are predicted by resting hsTnT levels. If confirmed in prospective evaluations, resting hsTnT could serve as a powerful triage tool in chest pain patients in the ED before diagnostic testing and thus could improve the effectiveness of patient management by eliminating the need for imaging in a substantial number of these patients.
Acknowledgments
The authors thank the Radiology Educational Media Services (REMS) of the Massachusetts General Hospital, Boston Massachusetts, for their support in the artworks.
This work was supported by the NIH (R01 HL080053). The reagents for high-sensitivity troponin assays were provided free by Roche Diagnostics. Drs. Ahmed, Uthamalingam, and Rogers received support from NIH grant T32HL076136. Dr. Truong also received support from NIH grants K23HL098370 and L30HL093896. Dr. Januzzi has received grant support from Roche Diagnostics, Siemens Diagnostics, and BRAHMS.
ABBREVIATIONS AND ACRONYMS
- ACS
acute coronary syndrome
- AUC
area under the curve
- CAD
coronary artery disease
- CI
confidence interval
- CT
computed tomography
- CTA
computed tomography angiography
- ECG
electrocardiogram
- ED
emergency department
- hsTnT
high-sensitivity troponin T
- IQR
interquartile range
- MPI
myocardial perfusion imaging
- NPV
negative predictive value
- PPV
positive predictive value
- SDS
summed difference score
- SPECT
single-photon emission computed tomography
- SRS
summed rest score
- SSS
summed stress score
- TID
transient ischemic dilation
- TnT
troponin T
Footnotes
All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–95. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction re-defined—a consensus document of the Joint European Society of Cardiology/ American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 3.Wu AH, Fukushima N, Puskas R, Todd J, Goix P. Development and preliminary clinical validation of a high sensitivity assay for cardiac troponin using a capillary flow (single molecule) fluorescence detector. Clin Chem. 2006;52:2157–9. doi: 10.1373/clinchem.2006.073163. [DOI] [PubMed] [Google Scholar]
- 4.Apple FS, Murakami MM. Serum 99th percentile reference cutoffs for seven cardiac troponin assays. Clin Chem. 2004;50:1477–9. doi: 10.1373/clinchem.2004.036129. [DOI] [PubMed] [Google Scholar]
- 5.Wu AH, Jaffe AS. The clinical need for high-sensitivity cardiac troponin assays for acute coronary syndromes and the role for serial testing. Am Heart J. 2008;155:208–14. doi: 10.1016/j.ahj.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem. 2010;56:254–61. doi: 10.1373/clinchem.2009.132654. [DOI] [PubMed] [Google Scholar]
- 7.Daniels LB, Laughlin GA, Clopton P, Maisel AS, Barrett-Connor E. Minimally elevated cardiac troponin T and elevated N-terminal pro-B-type natriuretic peptide predict mortality in older adults: results from the Rancho Bernardo Study. J Am Coll Cardiol. 2008;52:450–9. doi: 10.1016/j.jacc.2008.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Otsuka T, Kawada T, Ibuki C, Seino Y. Association between high-sensitivity cardiac troponin T levels and the predicted cardiovascular risk in middle-aged men without overt cardiovascular disease. Am Heart J. 2010;159:972–8. doi: 10.1016/j.ahj.2010.02.036. [DOI] [PubMed] [Google Scholar]
- 9.deFilippi CR, de Lemos JA, Christenson RH, et al. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–502. doi: 10.1001/jama.2010.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Omland T, de Lemos JA, Sabatine MS, et al. A sensitive cardiac troponin T assay in stable coronary artery disease. N Engl J Med. 2009;361:2538–47. doi: 10.1056/NEJMoa0805299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabatine MS, Morrow DA, de Lemos JA, Jarolim P, Braunwald E. Detection of acute changes in circulating troponin in the setting of transient stress test-induced myocardial ischaemia using an ultrasensitive assay: results from TIMI 35. Eur Heart J. 2009;30:162–9. doi: 10.1093/eurheartj/ehn504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Januzzi JL, Jr, Bamberg F, Lee H, et al. High-sensitivity troponin T concentrations in acute chest pain patients evaluated with cardiac computed tomography. Circulation. 2010;121:1227–34. doi: 10.1161/CIRCULATIONAHA.109.893826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol. 2009;53:1642–50. doi: 10.1016/j.jacc.2009.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Latini R, Masson S, Anand IS, et al. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation. 2007;116:1242–9. doi: 10.1161/CIRCULATIONAHA.106.655076. [DOI] [PubMed] [Google Scholar]
- 15.Kurz K, Giannitsis E, Zehelein J, Katus HA. Highly sensitive cardiac troponin T values remain constant after brief exercise- or pharmacologic-induced reversible myocardial ischemia. Clin Chem. 2008;54:1234–8. doi: 10.1373/clinchem.2007.097865. [DOI] [PubMed] [Google Scholar]
- 16.Filusch A, Giannitsis E, Katus HA, Meyer FJ. High-sensitive troponin T: a novel biomarker for prognosis and disease severity in patients with pulmonary arterial hypertension. Clin Sci. 2010;119:207–13. doi: 10.1042/CS20100014. [DOI] [PubMed] [Google Scholar]
- 17.Hansen CL, Goldstein RA, Akinboboye OO, et al. Myocardial perfusion and function: single photon emission computed tomography. J Nucl Cardiol. 2007;14:e39–60. doi: 10.1016/j.nuclcard.2007.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) J Am Coll Cardiol. 2002;40:1531–40. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]
- 19.Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 20.Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535–43. doi: 10.1161/01.cir.97.6.535. [DOI] [PubMed] [Google Scholar]
- 21.Zellweger MJ, Weinbacher M, Zutter AW, et al. Long-term outcome of patients with silent versus symptomatic ischemia six months after percutaneous coronary intervention and stenting. J Am Coll Cardiol. 2003;42:33–40. doi: 10.1016/s0735-1097(03)00557-6. [DOI] [PubMed] [Google Scholar]
- 22.Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51:5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 23.Bamberg F, Dannemann N, Shapiro MD, et al. Association between cardiovascular risk profiles and the presence and extent of different types of coronary atherosclerotic plaque as detected by multidetector computed tomography. Arterioscler Thromb Vasc Biol. 2008;28:568–74. doi: 10.1161/ATVBAHA.107.155010. [DOI] [PubMed] [Google Scholar]
- 24.Korosoglou G, Lehrke S, Mueller D, et al. Determinants of troponin release in patients with stable coronary artery disease: insights from CT angiography characteristics of atherosclerotic plaque. Heart. 2011;97:823–31. doi: 10.1136/hrt.2010.193201. [DOI] [PubMed] [Google Scholar]
- 25.Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54:49–57. doi: 10.1016/j.jacc.2009.02.068. [DOI] [PubMed] [Google Scholar]
- 26.Pundziute G, Schuijf JD, Jukema JW, et al. Evaluation of plaque characteristics in acute coronary syndromes: non-invasive assessment with multi-slice computed tomography and invasive evaluation with intravascular ultrasound radiofrequency data analysis. Eur Heart J. 2008;29:2373–81. doi: 10.1093/eurheartj/ehn356. [DOI] [PubMed] [Google Scholar]
- 27.de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304:2503–12. doi: 10.1001/jama.2010.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feng YJ, Chen C, Fallon JT, et al. Comparison of cardiac troponin I, creatine kinase-MB, and myoglobin for detection of acute ischemic myocardial injury in a swine model. Am J Clin Pathol. 1998;110:70–7. doi: 10.1093/ajcp/110.1.70. [DOI] [PubMed] [Google Scholar]
- 29.Remppis A, Scheffold T, Greten J, et al. Intracellular compartmentation of troponin T: release kinetics after global ischemia and calcium paradox in the isolated perfused rat heart. J Mol Cell Cardiol. 1995;27:793–803. doi: 10.1016/0022-2828(95)90086-1. [DOI] [PubMed] [Google Scholar]
- 30.Keller T, Zeller T, Ojeda F, et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011;306:2684–93. doi: 10.1001/jama.2011.1896. [DOI] [PubMed] [Google Scholar]
- 31.Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–67. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]