Abstract
The diagnosis and treatment of hemospermia presents significant difficulty, especially if it persists or recurs. In this retrospective study, we assessed whether transurethral seminal vesiculoscopy is feasible and effective in the diagnosis and treatment of hemospermia. To address this complex condition, we report our experience in a population of patients treated with transurethral seminal vesiculoscopy. From February 2006 to July 2008, 72 hemospermic patients underwent transurethral seminal vesiculoscopy examination and treatment at our urology center. Transurethral seminal vesiculoscopy was performed by a 7-F or 8-F rigid ureteroscope. The endoscopic procedure was conducted through the normal anatomic route of the seminal tracts. In this series, the mean follow-up period was 21.7 months. Definite diagnosis was made for 93.1% patients, and 94.4% patients were cured or showed a decrease in their symptoms. Postoperative complications were not observed in the study. Our study proves that transurethral seminal vesiculoscopy is effective in the diagnosis and treatment of hemospermia with minimal complication.
Keywords: diagnosis, hemospermia, transurethral seminal vesiculoscopy, treatment
Introduction
Hemospermia is defined as the appearance of blood in the ejaculate. Hemospermia is painless, benign and self-limiting in most cases, but it often invokes considerable anxiety and is frightening to the patient. Hemospermia is usually due to inflammatory or infectious causes. Recurrent or persistent hemospermia may indicate a more serious underlying pathology, especially in patients over 40 years old 1. In a recent study on the incidence of prostate cancer in patients with hemospermia, Han et al. 2 reported that prostate cancer was present in nearly 14% of men with hemospermia. Men perceive bloody ejaculation as an alarming physical symptom and seek help from an urologist. After a complete urological examination, including imaging studies and cystoscopy, malignancy or other significant diseases may be ruled out in the majority of cases. However, for many of the patients, the exact cause of hemospermia remains undefined, while their symptoms persists or recur. This is unsatisfactory for both the patients and urologists, and remains a dilemma. Under such circumstances, a defined approach is required to establish a diagnosis and effectively treat the condition. In the present study, we developed an endoscopic technology called transurethral seminal vesiculoscopy, using which the ejaculatory duct and seminal vesicle can be observed under direct view. It facilitates the exclusion of underlying pathology, evaluation of seminal vesicle disease and treatment of hemospermia.
Patients and methods
Patients and preoperative examinations
From February 2006 to July 2008, a total of 72 hemospermic patients, who underwent transurethral seminal vesiculoscopy examination and treatment by retrograde investigation through the seminal tract in our urology center, were enrolled in our study. All the patients had experienced hemospermia for at least the past 3 months and failed conservative therapy consisting of at least 4 weeks of antibiotics. Patient preoperative examinations included routine and special evaluations. Routine examinations included urinalysis and blood tests to determine the levels of erythrocytes, leukocytes, platelets, hemoglobin, blood urea nitrogen, creatinine and coagulation time.
Special examinations included transrectal ultrasonography, pelvic computed tomography or magnetic resonance imaging, and serum prostate-specific antigen (PSA). All serum PSA levels were less than 4.0 ng mL−1. Positive imaging findings were observed in most patients, which mainly included increased seminal vesicle size and calculi (Figure 1).
Figure 1.
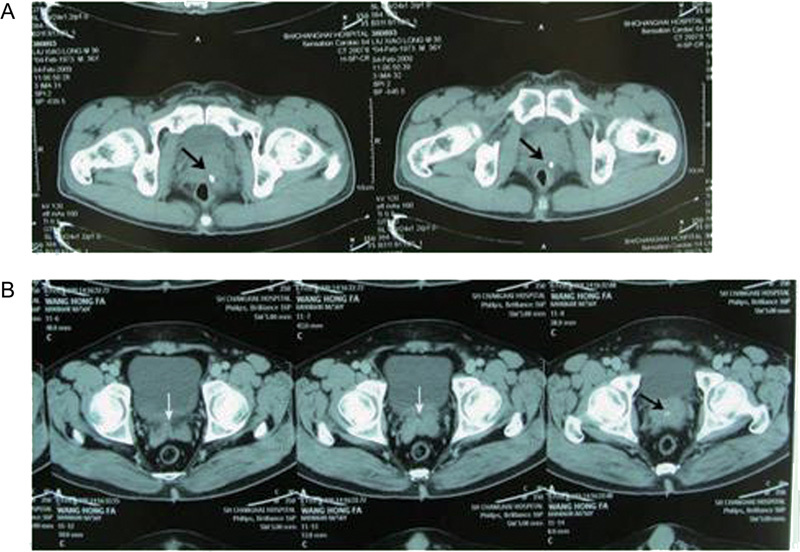
(A): Calculi were present in the left seminal vesicle (↓). (B): Calculi were present in the verumontanum lumen (↓), as were seminal vesicles that were larger in size (↓).
Surgical procedure
Transurethral seminal vesiculoscopy was performed by a 7-F or 8-F rigid ureteroscope with laryngeal mask general anesthesia or spinal anesthesia. The patient was asked to lie in the lithotomy position and the endoscopic procedure was performed through the normal anatomic path of the distal seminal tracts. A surgeon and an assistant are enough to perform the operation; the basic principles of the procedure remain the same as performing ureteroscopy.
After examinations of the urethra and bladder, the ureteroscope was inserted retrograde through the orifice of the verumontanum guided by a 0.032-inch Zebra guidewire under direct vision (Supplementary video 1). After entering the lumen of the verumontanum, the bilateral ejaculatory duct orifices were identified and were always shaded behind a thin transparent membraniform wall. A puncture in the wall with a 0.032-inch Zebra guidewire was made. Using this guidewire, the ureteroscope was injected with ease into the seminal vesicles to inspect the internal structures. Typical normal seminal vesicles can be seen clearly with multiple cellulae and folds that take the form of a honeycomb with ivory white and jell-like seminal plasma (Supplementary video 2).
The usual interventional techniques used in our cases include blood clot or prunosus jell-like plasma draining, holmium laser lithotripsy or removal using endoscopic instruments, if a calculus is present, and biopsy of any other suspicious mucosal lesions. After the procedure, an antibiotic (typically a 0.5% Levofloxacin injection, a quinolone antibacterial drug, which is a kind of yellowish green [the color clarity liquid]) was used to wash both the seminal vesicles under low pressure. A urethral Foley catheter was placed overnight.
Results
Our 72 patients ranged from 21 to 76 years old, the mean age was 48.8 years and the mean follow-up period was 21.7 months (range: 12–29 months). The transurethral seminal vesiculoscope was successfully inserted into the verumontanum lumen in every patient. In the seminal vesicles of the hemospermic patients, blood clots or prunosus jell-like plasma were present (Supplementary video 3). Inflammatory mucosal edema, congestion and hemorrhages were observed constantly. Muddy or particulate calculi are also detected frequently in the lumen of the verumontanum or seminal vesicles in the hemospermic patients (Supplementary video 4 and 5). In only five patients, we failed to identify ejaculatory duct orifices, and in the remaining 67, we were able to advance the scope retrograde into the seminal vesicle.
In the study, we were able to diagnose 93.1% (67/72) of the patients with hemospermia, the exception being the five patients, in whom we could not identify the ejaculatory duct orifices. In these 67 patients, significant inflammatory mucosal edema, congestion and inflammatory hemorrhages were found. These symptoms were seen in only a single vesicle in 58.3% (42/72) of patients and in both vesicles in 34.7% (25/72) of patients. Stricture or obstruction at the level of the verumontanum orifice or stenosis of the ejaculatory duct was also found in those patients. Calculi were present in one or both seminal vesicles and in the verumontanum lumen in 24 patients (33.3%). Biopsy of the 67 patients revealed inflammatory but benign tissue, with no evident malignancy or hypertrophy.
Symptoms of hemospermia disappeared in 97.2% (70/72) of our patients after subsequent ejaculation three to five times during the follow-up period. In the five patients in whom we failed to identify ejaculatory duct orifices, two patients experienced a decrease in symptoms and in one patient the symptoms completely disappeared.
Postoperative complications, such as epididymitis, retrograde ejaculation, urinary incontinence or rectal injury, were not observed in the present study.
Discussion
Transurethral seminal vesiculoscopy is a new technique that deals with the use of ureteroscope in diagnosis and treatment of seminal tract disease. The first reported endoscopy of the seminal vesicle was in 1996 using ex vivo specimens obtained at radical cystectomy and prostatectomy 3. The first report of in vivo endoscopic evaluation of the seminal vesicles was reported in 2002 4. Recently, several reports have described the endoscopic technique using a ureteroscope for the evaluation and treatment of patients with seminal tract disorders 5. The first case of laser lithotripsy of a seminal vesicle stone endoscopic procedure was performed in 2005 6. However, the technique is still at an immature stage. Owing to the lack of enough experience and cases, its effect needs further observation.
Hemospermia remains difficult both to diagnose and treat, especially because of its recurrent and persistent nature till today. In this study, we attempted to use transurethral seminal vesiculoscopy for the diagnosis and treatment of hemospermia. To our knowledge, the present study is the first large-scale report of transurethral seminal vesiculoscopy for the diagnosis and treatment of hemospermia. We found the technique to be both feasible and effective in this study. A definite diagnosis was made in 93.1% of patients and 97.2% of our cohort had their symptoms disappear or diminish. We were able to directly observe the strictures, hemorrhages and calculi associated with hemospermia, and also excluded malignancy with biopsy. Pathological examination of biopsy specimens revealed normal or inflammatory but benign tissues.
We would like to highlight two points:
First, we wanted to address the factors leading to recurrent or persistent hemospermia in the absence of malignancy. In our study, obstruction or stricture at the level of the verumontanum orifice or ejaculatory duct was found in almost all cases. Calculi cause obstruction at these levels (Supplementary video 4 and 5), and the thickening of the membraniform wall that is shaded on the ejaculatory duct orifices usually results in stricture of the ejaculatory duct. We hypothesize that the thickening of the membraniform wall was caused by inflammatory stimulation. The membraniform wall has been mentioned in previous seminal vesiculoscopy literature 4 in a context similar to our study, but we are unaware of its specific anatomical role. However, from our experience with hemospermic patients, it was indeed obviously thicker than in a normal male and led to stricture of the ejaculatory duct. We speculate that this kind of obstruction or stricture may be the basic pathophysiology of persistent or recurrent hemospermia. Specifically, infection may first stimulate thickening of the membraniform wall, leading to a stricture that aggravates the infection due to impaired drainage. In some cases, infection and stricture also contribute to the formation of calculi, and conversely the calculi also cause obstruction and frequent recurrence of infection. In brief, stricture, infection and calculi create a vicious cycle that induces an infection that cannot be improved or eradicated despite the use of antibiotics and finally results in persistent or recurrent hemospermia. We conclude that hemospermia can be cured by transurethral seminal vesiculoscopy, because it can break the vicious cycle by facilitating dilation of the stricture, removal of calculi, elimination of obstructions and drainage of infection. The five patients in whom identification of the ejaculatory duct orifices failed still experienced a decrease or disappearance of their symptoms, which was likely caused by our technique. Specifically, we think the improvement in these patients may have been due to dilatation of the verumontanum orifice and the resultant decreased pressure in the verumontanum lumen, which may have contributed to drainage of the infection.
Second, the practice of transurethral seminal vesiculoscopy is not very difficult, but failure does still occur for most cases. In our experience, the success lies in identifying the orifices of the verumontanum or ejaculatory ducts. We identified two hints that may be helpful. The first is regarding how to deal with the difficulty in identifying the orifice of the verumontanum. In our cases, if the orifice could not be identified, we resected the verumontanum using a coagulating electrode and probed using a Zebra guidewire to confirm the verumontanum lumen. The second tip is regarding how to identify the bilateral ejaculatory duct orifices. The ejaculatory duct orifices rarely open into the verumontanum lumen directly; rather, they are usually covered by a thin, transparent, membraniform substance and placed medialy zygomorphic (Supplementary video 1). In some cases, the membranes are too thick to identify. However, if the procedure is performed under low-pressure saline irrigation or no irrigation, the membraniform substances protrude out a little, allowing the identification of the ejaculatory duct orifices. To confirm this, a puncture at the suspected orifices with a 0.032-inch Zebra guidewire can be made. However, in a few cases, the ejaculatory duct can still not be identified, as happened with five patients in our study. Unfortunately, the reasons for this failure remain unclear.
To limit postoperative complications, the endoscopic procedure must be performed under low-pressure saline irrigation cautiously to avoid damage to the prostate or to the rectum. In the present study, postoperative complications, such as epididymitis, retrograde ejaculation or rectal injury, were not observed. However, only short-term complications were assessed. It is possible that seminal vesiculoscopy may cause some damage to the seminal tract or may cause future fertility problems.
Persistent or recurrent hemospermia presents a therapeutic dilemma. In this study, we evaluated transurethral seminal vesiculoscopy as a new approach for the diagnosis and treatment of hemospermia. We found this technique to be an effective management tool with minimal complications. Future work should be aimed at avoiding failure operations (for example, failed to identify ejaculatory duct orifices) and observing patients for a longer term to ensure that no complications arise.
Supplementary Information accompanies the paper on Asian Journal of Andrology website (http://www.nature.com/aja).
Supplementary Information
References
- Amhad I, Krishna NS. Haemospermia. J Urol. 2007;177:1613–8. doi: 10.1016/j.juro.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Han M, Brannigan RE, Antonor J AV, Roohl KA, Catalona WJ. Association of hemospermia with prostate cancer. J Urol. 2004;172:2189–92. doi: 10.1097/01.ju.0000144565.76243.b1. [DOI] [PubMed] [Google Scholar]
- Shimada M, Yoshida H. Ex vivo ultrathin endoscopy of the seminal vesicles. J Urol. 1996;156:1388–90. [PubMed] [Google Scholar]
- Yang SC, Rha KH, Byon SK, Kim JH. Techniques in endourology-transutricular seminal vesiculoscopy. J Endourol. 2002;16:343–5. doi: 10.1089/089277902760261347. [DOI] [PubMed] [Google Scholar]
- Li L, Jiang C, Song C, Zhou Z, Song B, et al. Transurethral endoscopy technique with a ureteroscope for diagnosis and management of seminal tracts disorders: a new approach. J Endourol. 2008;22:719–24. doi: 10.1089/end.2007.0130. [DOI] [PubMed] [Google Scholar]
- Cuda SP, Brand TC, Thibault GP, Stack RS. Case report: Endoscopic laser lithotripsy of seminal-vesicle stones. J Endourol. 2006;20:916–8. doi: 10.1089/end.2006.20.916. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


