Dear Sir,
My name is Xiang Wang, from the Department of Urology of Huashan Hospital at Fudan University in China. In this letter, we present our experience with the diagnosis and treatment of a patient with severe penile aspergillosis. Fungus is a common pathogen that can cause balanoposthitis. Candida albicans is considered to be the most common pathogen that causes balanoposthitis, and is responsible for up to 35% of all cases of infectious balanitis 1. Other fungal infections of the penis are rare. Aspergillus flavus, the most common cause of superficial fungal infections, is often found in the air. The common clinical syndromes caused by A. flavus include chronic granulomatous sinusitis, keratitis, cutaneous aspergillosis, wound infections and osteomyelitis following trauma and inoculation of the fungus 2. However, balanoposthitis caused by A. flavus has rarely been reported. In this report, we describe a case of a severe penile A. flavus infection, as well as the treatment administered to this patient.
The patient was a 61-year-old man who was admitted to the Urology Clinic of Huashan Hospital of Fudan University (Shanghai, China) because of aggravating skin erosion and bleeding on his glans. The problem began with a reddish rash that was found at the patient's coronary groove 3 years before presentation, which was later followed by swelling and extravasation of purulent secretion. The patient had been previously treated with unknown creams and oral antibiotics at a local private clinic. The lesion deteriorated over time. The glans appeared eroded and was bleeding upon presentation to our clinic. In addition, the corpus cavernosum of the penis had detached from the glans and a urethral perforation had occurred at the ventral side (Figure 1). The patient had difficulty with sexual activity and urination. All of the treatments he had tried at other hospitals had been ineffective and partial amputation of his penis was suggested before he came to our hospital. The patient did not have a history of immunodeficiency or penile injury.
Figure 1.

Severe ulceration and necrosis at the coronary groove, as well as a ventral urethral perforation.
A series of serological studies, including human immunodeficiency virus (HIV), rapid plasma reagin (RPR), herpes simplex virus (HSV) and tissue cultures for screening bacteria and Mycobacterium tuberculosis, were performed at our hospital. All results were negative. Therefore, a penile biopsy was performed, which revealed chronic inflammation with fungal infection of the glans (Figure 2). The specimen was then sent for fungal culture. Seven days after the specimen was cultured, a velvety, golden-yellow mould grew on Czapek's agar. Based on the morphological characteristics of the fungus, an A. flavus infection was diagnosed.
Figure 2.
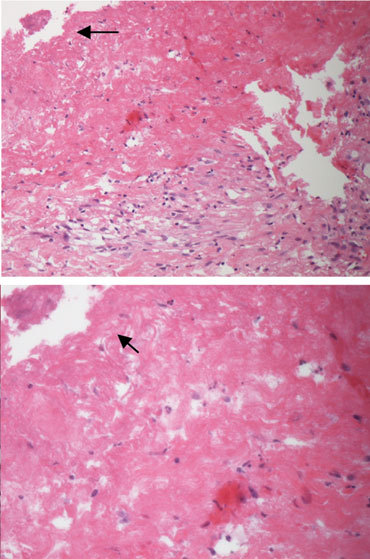
Histological appearance of the glans biopsy, showing chronic inflammation and a fungal infection (black arrows indicate the fungi).
The treatment included medication and surgery. First, the patient underwent suprapubic cystostomy and debridement. After surgery, the lesion was washed with 0.5% neomycin solution daily to prevent bacterial infection and eliminate necrotic tissue. Meanwhile, itraconazole (200 mg, twice a day) combined with tinidazole (400 mg, twice a day) was administered intravenously for 20 days. One month later, vitalized tissue was found at the site of the lesion. Plastic surgery was performed to close the wound and repair the ruptured urethra in a one-stage procedure. The glans was sutured to the corpus cavernosum in two layers and the urethral perforation was sutured transversely with 4-0 absorbable suture (Ethicon's coated Vicryl suture, Ethicon, Inc., Johnson & Johnson Medical, China). Twenty days after the operation, the wound was completely healed, and the patient was able to urinate normally and experienced a return of his erections (Figure 3). At the patient's 1-year follow-up, natural urination and erection were found to have persisted without occurrence of urethral stricture.
Figure 3.

The penis is completely healed and natural urination has resumed.
Balanitis is a common condition seen in male patients who present to urology clinics, and can be caused by different pathological entities. Diabetes mellitus, HIV infection and iatrogenic immunosuppression are often found to be underlying medical conditions in patients with fungal balanitis 3. However, balanitis caused by Aspergillus has been reported rarely. Cutaneous aspergillosis can be classified as either (i) primary, following direct inoculation of Aspergillus at sites of skin injury, or (ii) secondary, which occurs by haematogenous spread 4. According to the case history and the serological tests we performed, this patient had none of the aforementioned underlying medical conditions that are commonly associated with fungal balanitis. The only possible risk factor that this patient possessed for fungal balanitis was his long-term use of unknown creams that may have contained glucocorticoids, which could have suppressed local immune responses.
The clinical presentation of cutaneous aspergillosis is characterized by the presence of violaceous macules, papules, plaques or nodules, haemorrhagic bullae, ulcerations with central necrosis with or without eschar formation, pustules or subcutaneous abscesses 4. In this case, macules and papules were initially present at the patient's coronary groove. The lesion deteriorated over time, showing swelling, extravasation of purulent secretion, tissue erosion and bleeding. Urethral perforation occurred after an abscess on the ventral side of the penis became ulcerated. Although this patient presented with the typical symptoms of cutaneous aspergillosis, the infrequency of penile aspergillosis led to misdiagnosis before he came to our hospital. The diagnosis of aspergillosis depends on pathological examination and fungal culture, which was not performed at the other hospitals.
The appropriate treatment of cutaneous aspergillosis includes a combination of antifungal chemotherapy and surgical debridement, if necessary. The antifungal drugs commonly used to treat cutaneous aspergillosis are amphotericin-B 5, terbinafine 6, caspofungin 7, itraconazole and flucytosine 8. Despite the advent of efficacious antifungal therapy, combined surgical therapy is still advocated in the treatment of these patients 9, 10. In the present case, we chose itraconazole as our antifungal agent. Plastic surgery was performed to close the wound and repair the urethral perforation after the tissue at the site of the lesion healed and became vitalized.
Through this letter, we hope to emphasize the appropriate diagnostic and treatment methods that should be used in cases of penile aspergillosis. In this case, the biopsy revealed chronic inflammation and fungal infection at the glans, which led us to perform fungal culture to identify the exact pathogen. The patient recovered completely on being given effective antifungal medication and after plastic surgery.
References
- Dockerty WG, Sonnex C. Candidal balano-posthitis: a study of diagnostic methods. Genitourin Med. 1995;71:407–9. doi: 10.1136/sti.71.6.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedayati MT, Pasqualotto AC, Warn PA, Bowyer P, Denning DW. Aspergillus flavus: human pathogen, allergen and mycotoxin producer. Microbiology. 2007;153:1677–92. doi: 10.1099/mic.0.2007/007641-0. [DOI] [PubMed] [Google Scholar]
- Carmen L, Alcina F, Carlos R, Acácio GR. Infectious balanoposthitis: management, clinical and laboratory features. Int J Dermatol. 2009;48:121–4. doi: 10.1111/j.1365-4632.2009.03966.x. [DOI] [PubMed] [Google Scholar]
- Mishri LK, Catherine MS, Mohammed B, Mohammed S, Asha K. Cutaneous and paranasal aspergillosis in an immunocompetent patient. Int J Dermatol. 2000;39:835–6. doi: 10.1046/j.1365-4362.2000.00095-3.x. [DOI] [PubMed] [Google Scholar]
- Sayime A, Bulent E, Berna G, Guliz U, Erkin K. Treatment of two postoperative endophthalmitis cases due to Aspergillus flavus and Scopulariopsis spp. with local and systemic antifungal therapy. BMC Infect Dis. 2007;7:87. doi: 10.1186/1471-2334-7-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang QQ, Li L, Zhu M, Zhang CY, Wang JJ. Primary cutaneous aspergillosis due to Aspergillus flavus: a case report. Chin Med J. 2005;118:255–7. [PubMed] [Google Scholar]
- Khan ZU, Ahmad S, Mokaddas E, Said T, Nair MP, et al. Cerebral aspergillosis diagnosed by detection of Aspergillus flavus-specific DNA, galactomannan and (1→3)-β-D-glucan in clinical specimens. J Med Microbiol. 2007;56:129–32. doi: 10.1099/jmm.0.46549-0. [DOI] [PubMed] [Google Scholar]
- Chan YH, Seok CE, Rong MB, Kyung WM. Free flap coverage of extensive soft tissue defect in cutaneous Aspergillosis: a case report. J Korean Med. 2008;23:920–3. doi: 10.3346/jkms.2008.23.5.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roilides E, Farmaki E. Human immunodeficiency virus infection and cutaneous aspergillosis. Arch Dermatol. 2000;136:412–4. doi: 10.1001/archderm.136.3.412. [DOI] [PubMed] [Google Scholar]
- Herron MD, Vanderhooft SL, Byington C, King JD. Aspergillosis in a 24-week newborn: a case report. J Perinatol. 2003;23:256–9. doi: 10.1038/sj.jp.7210876. [DOI] [PubMed] [Google Scholar]


