Abstract
Among the different DNA anomalies that can be present in the male gamete, DNA fragmentation is the most frequent, particularly in infertile subjects. There is now consistent evidence that a sperm containing fragmented DNA can be alive, motile, morphologically normal and able to fertilize an oocyte. There is also evidence that the oocyte is able to repair DNA damage; however, the extent of this repair depends on the type of DNA damage present in the sperm, as well as on the quality of the oocyte. Thus, it is important to understand the possible consequences of sperm DNA fragmentation (SDF) for embryo development, implantation, pregnancy outcome and the health of progeny conceived, both naturally and by assisted reproductive technology (ART). At present, data on the consequences of SDF for reproduction are scarce and, in many ways, inconsistent. The differences in study conclusions might result from the different methods used to detect SDF, the study design and the inclusion criteria. Consequently, it is difficult to decide whether SDF testing should be carried out in fertility assessment and ART. It is clear that there is an urgent need for the standardisation of the methods and for additional clinical studies on the impact of SDF on ART outcomes.
Keywords: assisted reproduction, COMET, DNA fragmentation, ICSI, in vitro fertilization-embryo transfer, sperm chromatin structure assay, spermatozoa, TUNEL
Introduction
At fertilisation, the spermatozoon delivers the paternal genome to the oocyte for embryo formation. Any type of damage present in the DNA of paternal and/or maternal origin can lead to an interruption of the reproductive process. The types of DNA disorder found in the male gamete include chromosomal aberrations (mostly deletions and aneuploidies), epigenetic modifications on histone tails and DNA, mutations, base oxidation and sperm DNA fragmentation (SDF). SDF, in particular, might be the most frequent cause of paternal DNA anomaly transmission to progeny, as it is found in a high percentage of spermatozoa in subfertile and infertile men, as well as in heavy smokers, aged men, subjects exposed to toxicants or to radiochemotherapies. The percentage of DNA-fragmented spermatozoa in an ejaculate negatively correlates with semen quality.1, 2, 3 However, such correlations are not as strict as expected, indicating that SDF may be an independent predictor of sperm fertility potential. Our group recently demonstrated the existence of two sperm populations characterized by different degrees of SDF: one of these populations (named propidium iodide dimmer (PIdim) for its staining with a PI nuclear probe, see below) comprises only DNA-fragmented sperm and is strictly correlated with poor semen quality. By contrast, the other population (named propidium iodide brighter (PIbr), see below) comprises sperm with variable percentages of DNA fragmentation which are completely unrelated to semen quality.4 Sperm in the PIbr population can retain an apparently normal morphology and motility, thereby increasing their chances of being selected for intracytoplasmic sperm injection (ICSI) purposes. This finding represents a significant problem, as it is now clear that a spermatozoon with fragmented DNA can fertilize an oocyte.5 There are several studies demonstrating that the oocyte and the embryo retain the ability to repair DNA damage that may be present in the paternal genome (reviewed in Ref. 6); however, whether all types of damage can be repaired is not yet clear. For instance, double-stranded DNA breaks appear to be less repairable than single-stranded breaks and, thus, have a greater impact on embryo development.7 In addition, the oocyte quality is another important determinant, because oocyte immaturity, maternal age and external factors may affect the ability to repair DNA damage.
The type and severity of SDF are determined by the underlying mechanisms of SDF induction. In the following sections, we will review the possible mechanisms producing DNA fragmentation and the damage type, as well as the clinical studies that have focused on the consequences of this damage for natural and assisted reproduction. In addition, the methods currently available to detect SDF will be critically reviewed. The differences among the methods will be addressed and their strengths and pitfalls discussed.
Mechanisms generating DNA fragmentation
SDF may originate in the testis, or it may occur as a consequence of different insults after spermiation and during transit in the male genital tract. Of importance, for assisted reproductive technology (ART), SDF occurs after ejaculation, when sperm are deprived of seminal plasma and incubated in vitro for a short time.8
DNA fragmentation of differentiating germ cells could occur in the testis as part of the apoptotic process (which is known as the abortive apoptosis theory) or during chromatin compaction, and in particular, replacement of histones by protamines (the defective maturation theory). Following release from the testis, oxidative stress is thought to be the main mechanism responsible for the occurrence of DNA fragmentation and DNA base oxidation.
The abortive apoptosis theory
The abortive apoptosis theory was originally developed by Sakkas et al.9 According to this theory, DNA fragmentation is induced by activated endonucleases, which mostly lead to DNA double-stranded breaks. The theory is based on studies demonstrating high expression of Fas receptors (also known as CD95),10 as well as the presence of ultrastructural apoptosis-like features such as cytoplasmic vacuoles,11 in ejaculated sperm. This evidence led Sakkas et al.9 to hypothesize that sperm with fragmented DNA in the ejaculate might be derived from germinal cells whose apoptotic process in the testis has not been completed. The recent identification in semen of membrane-bound, anucleated, round structures termed M450 bodies (termed as such because of their staining with merocyanine 540), which probably represent apoptotic bodies,12, 13 is indirect evidence supporting the abortive apoptosis theory. In particular, M450 bodies represent impairment of the physiological phagocytosis process in the male genital tract. The finding that M540 bodies are particularly abundant in the semen of subfertile subjects13 and are highly correlated with the percentage of PIdim DNA-fragmented sperm in the ejaculate (Muratori et al., unpublished data, 2011) further supports the abortive apoptotic theory as one of the mechanisms causing SDF.
Although data supporting the abortive apoptosis theory have accumulated, the relationship between SDF and the expression of apoptotic markers is still not as strict as expected,14 and there is no association between apoptosis-like ultrastructures and the percentage of sperm with DNA fragmentation.3 Accordingly, this mechanism cannot completely explain the occurrence of DNA fragmentation in spermatozoa.
Defective maturation theory
According to the defective maturation theory, DNA breaks that occur during the replacement of histones by protamines, as part of the process that leads to DNA compaction, fail to undergo complete religation.15, 16, 17 DNA break generation is important to reduce the torsional stress in a DNA helix, thereby facilitating histone disassembly. The enzyme responsible for creating DNA nicks is likely to be topoisomerase II, which is able to induce both single- and double-stranded breaks.16, 18 Topoisomerase II is also the main enzyme of the DNA repair system for elongating spermatids.18 Recently, it has been shown that topoisomerase II is inhibited by poly(ADP-ribose) polymerase enzymes, which are activated as a consequence of DNA strand break formation.19 It is likely that any alteration occurring in the complex DNA repair process can have dramatic consequences for the genomic integrity of the gamete.
Oxidative stress
Emerging evidence indicates that the abortive apoptosis and defective chromatin packaging mechanisms cannot completely explain the occurrence of SDF in the ejaculate. There are reports demonstrating that there is more DNA fragmentation in sperm in the caudal epididymis and the ejaculate than in the testicular sperm.20, 21 Although the number of patients included in these studies and the number of testicular sperm analysed were relatively small, these results seem to indicate that SDF mainly occurs after sperm release from the testis. Following spermiation, the generation of reactive oxygen species (ROS) is considered the main cause of SDF. Excessive intrinsic ROS production may result from the presence of immature spermatozoa retaining cytoplasmic droplets.22 Genitourinary infections may serve as another potential source of ROS. There is also evidence that after ejaculation, SDF may increase spontaneously during laboratory handling and storage8 and following external insults.23, 24
The positive relationship between intrinsic ROS production and DNA fragmentation in semen samples,25 and the prevention of DNA damage following treatment with ROS scavengers and antioxidants26, 27 (discussed below) serve as indirect evidence that oxidative stress can cause SDF. There is also a high correlation found between SDF and the level of 8-hydroxy-2'-deoxyguanosine (8-OHdG), the main marker of oxidative stress in DNA, in the analysis of sperm selected by density–gradient centrifugation.28 To a much lesser extent, the relationship between SDF and 8-OHdG has also been demonstrated in unselected sperm.28, 29 It should be mentioned, however, that other studies do not show a clear relationship between SDF and 8-OHdG30, 31 or between SDF and other signs of sperm oxidative stress, such as malonaldehyde formation,32 suggesting that further studies are warranted to define the relationship between oxidative damage and SDF.
Methods to detect SDF
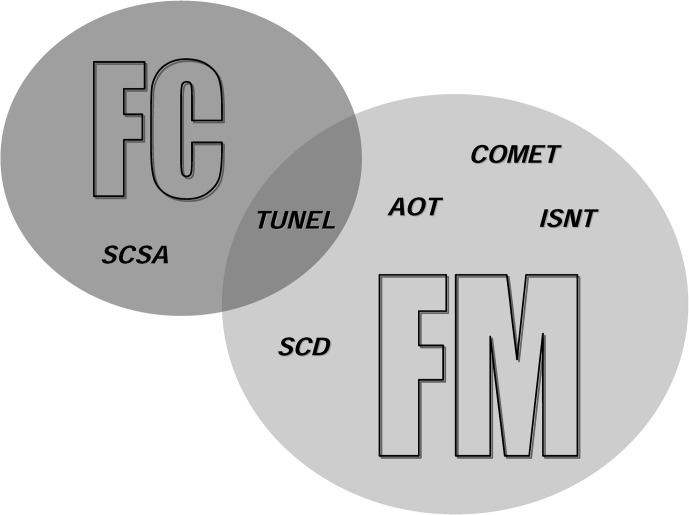
Several methods are currently available to evaluate SDF (Figure 1), namely, the sperm chromatin structure assay (SCSA), terminal deoxynucleotidyl transferase-mediated fluorescein-dUTP nick-end labelling (TUNEL), in situ nick translation, the single-cell gel electrophoresis assay (also known as COMET), the acridine orange test and the sperm chromatin dispersion test (also known as Halosperm). Importantly, SDF can be revealed by flow cytometry and/or fluorescence microscopy (Figure 1) depending on the method used. However, whereas flow cytometry may be used to objectively analyse hundreds of thousands of cells, fluorescence microscopy relies on a subjective analysis that is usually limited to several hundred cells. Recently, other differences between flow cytometry and fluorescence microscopy have been highlighted.33 In the case of severe oligozoospermia (fewer than two million sperm/ejaculate), only fluorescence microscopy can be used.
Figure 1.
Assays used to evaluate sperm DNA fragmentation and measurement technologies that can be used. AOT, acridine orange test; COMET, single-cell gel electrophoresis assay; FC, flow cytometry; FM, fluorescence microscopy; ISNT, in situ nick translation; SCD, sperm chromatin dispersion test; SCSA, sperm chromatin structure assay; TUNEL, terminal deoxynucleotidyl transferase-mediated fluorescein-dUTP nick-end labelling.
The important questions about these methods are whether they reveal the same type of damage, whether they obtain comparable results, and, last but not least, whether they are standardized. At the moment, standardisation is defined only for the SCSA method.34 Lack of standardisation is particularly important, as we have recently outlined for the TUNEL assay.35, 36 The different data in the literature for the levels of SDF in fertile and subfertile men, and the lack of agreement among the different studies evaluating the impact of SDF on ART outcomes, reflect how different methods may affect the results (see below). For example, a systemic meta-analysis of papers reporting the relationship between sperm DNA damage and ART outcomes published by Li et al.37 shows how, when data are pooled according to the method (TUNEL and SCSA) employed in the study, completely different conclusions can be drawn. The two most heavily employed techniques to reveal SDF are TUNEL and SCSA. Although the two techniques show correlated results,34 they are not equivalent and reveal different types of damage;37, 38 consequently, the results from studies detecting SDF with these methods are not comparable. In particular, the TUNEL assay quantifies the amount of cellular DNA breakage by incorporating fluorescent dNTPs at single- and double-stranded DNA ends in the presence of the enzyme terminal deoxynucleotidyl transferase. The SCSA method determines the extent of cellular DNA denaturation (induced by acids or heat treatment) by measuring the metachromatic shift of acridine orange from green (indicative of intercalation into double-stranded DNA) to red fluorescence (indicative of association with single-stranded DNA). Even if the induced denaturation is facilitated at the sites of DNA breaks, the target sites for the two methods do not overlap exactly.34
Another method frequently used in clinical investigations is COMET (a single-cell gel electrophoresis assay), which is a relatively simple method for detecting DNA damage in individual cells.39 This method consists of several steps: cells are embedded in agarose; lysis is carried out in neutral or alkaline conditions; then the lysed cells are subjected to electrophoresis, DNA staining and microscopic image analysis.40 Damaged cells appear as a ‘comet' with a brightly fluorescent head and tail, whose length and fluorescence intensity depend on the number of DNA strand breaks.41 The Comet assay is a rapid and sensitive method that allows the evaluation of DNA fragmentation on a few sperm; thus, it can be employed in cases of severe oligozoospermia. The disadvantages of the Comet assay are the lack of standardized protocols and the need for software to conduct image analysis.42
Recently, some of these methods have been modified in order to improve their accuracy and reliability, to enhance their potential clinical utility, and to measure other types of DNA damage. The TUNEL/PI procedure, recently developed in our laboratory, improves the cytometric detection accuracy of SDF by excluding M540 bodies from sperm fluorescence analysis.4 Another advantage of TUNEL/PI is its ability to distinguish between two sperm populations whose percentages of DNA damage show different relationships with semen quality. In particular, SDF in PIbr population is of interest, as, being unrelated to semen quality, a DNA-fragmented sperm in this population may be motile and with an apparent normal morphology.4 TUNEL after decondensation with dithiothreitol,43 developed in Aitken's Laboratory, should better define the status of chromatin damage with respect to simple TUNEL, because it facilitates greater accessibility of the sperm nuclei to the terminal deoxynucleotidyl transferase enzyme. Moreover, coupling this technique to a stain for dead cells 43 allows the detection of DNA fragmentation in live sperm. In principle, live sperm should have the greatest impact on reproductive outcomes; consequently, the detection of SDF in live sperm should improve the predictive power of SDF. However, Aitken et al.44 failed to better discriminate between fertile and infertile subjects by measuring the levels of SDF in live vs. total (live+dead) sperm. A modified version of COMET was proposed by Simon et al.,45 by pretreating sperm samples with the enzyme formamidopyrimidine DNA glycosylase (FpG), which converts 8-OHdG into DNA breaks. Hence, the resultant amount of SDF from the modified COMET assay is the sum of the native DNA breakage and the occurrence of 8-OHdG, the latter being the hallmark of oxidative damage to DNA. With this method, the predictive power of SDF, in terms of ART outcomes, was improved for both in vitro fertilisation (IVF) and ICSI cycles.
Clinical correlates
What can we learn from treatments to reduce SDF?
Only a few clinical studies have been performed using SDF as a primary or secondary end point after the in vivo treatment of patients with pharmacological approaches. These studies involved only small numbers of recruited patients and employed empirical treatments, such as antioxidants, with unknown mechanisms of action. In addition, very few of these studies had a randomized placebo-controlled design. In general, these studies show that the treatments had only limited effects on SDF, averaging about 20% reduction of SDF 29, 46, 47, 48 with the exception of the study by Greco et al.,27 which demonstrated a 60% reduction of SDF in men seeking treatment for infertility. Later, Greco's group20 demonstrated higher implantation and pregnancy rates by using ICSI with sperm from men who has been treated with antioxidants and responded to the treatment with a decrease in SDF. However, in this study,20 which was neither randomized nor placebo-controlled, about 30% of the patients did not respond to the antioxidant treatment.
Overall, published studies on in vivo treatments aimed at reducing SDF have shown few beneficial effects. There could be several reasons for the limited efficacy of oral anti-oxidants, including biases in patient selection, length of therapy, type of antioxidant (single or cocktail), effective absorption of the drugs in the reproductive tract and intra-individual variability of SDF. Concerning the last point, data on intra-individual variation of TUNEL/flow cytometry and SCSA results seem to indicate that sperm DNA damage is consistent over time or at least show that there is less intra-individual variation with respect to other semen parameters in normozoospermic subjects.49 Recently, reports have shown that the intra-individual variation in DNA damage detected by SCSA is high when the extent of DNA damage in the patients is elevated.50
It is clear that larger, multicentre, fully randomized and placebo-controlled studies are urgently needed in order to define whether it is possible to reduce SDF by in vivo treatments. Such studies should be performed in men with high basal SDF levels. In view of the demonstration that multiple causes result in SDF in the ejaculate (see above), additional strategies, based on increasing the efficiency and the quality of spermatogenesis, should be developed. In a recent Cochrane database systematic review,51 which includes 34 randomized controlled studies on the effect of antioxidant treatment on pregnancy rate, some beneficial effects of antioxidant supplementation on pregnancy rate were suggested, warranting further head-to-head comparison studies. Moreover, in the same review,51 the authors concluded that SDF should be included among the measured outcomes of these studies. At present, only the study by Greco et al.27 evaluated the SDF parameter and met the criteria to be included in a meta-analysis for evaluation of the effect of antioxidants on SDF.51
Another possible use of treatments to reduce SDF is related to sperm cryopreservation. There are numerous studies demonstrating that SDF and apoptotic markers increase after cryopreservation, mostly because of an increase in oxidative stress.31, 52, 53, 54 Thus, antioxidants could be added to cryopreservation media, as suggested by studies showing some efficacy of genistein and resveratrol in reducing post-thaw SDF.53, 54
Finally, several studies have evaluated the relationship between varicocele and SDF, and the effect of varicocele surgical or microsurgical repair on SDF. Men with varicoceles exhibit higher SDF levels than fertile men or donors, but these levels are not higher than those of men with other or unknown (idiopathic) causes of SDF.21, 55, 56, 57 Varicocelectomy has been associated with a significant decrease in SDF in all of the studies published to date.58, 59, 60, 61, 62 Interestingly, in some of these studies, SDF was the only seminal parameter to improve after varicocelectomy.60, 61
Relationship to the outcome of natural and assisted reproduction
During the past decade, several authors proposed the assessment of SDF as a parameter to predict male fertility potential. Because SDF reflects, but does not precisely overlap with the extent of poor quality sperm,1, 2, 3 its assessment might, indeed, provide additional prognostic and diagnostic values. In view of the finding that fertilisation may occur normally even when SDF is present,5, 63, 64 any sperm DNA damage that cannot be effectively repaired by the oocyte may affect the subsequent post-fertilisation steps, such as embryo and foetal development. Therefore, the assessment of sperm DNA status may be of particular significance in cases in which fertilisation is normal but implantation fails or early miscarriage occurs. Indeed, studies performed in animal models, in which DNA fragmentation has been induced in spermatozoa by radiation63 or by freeze–thawing without cryoprotectant,64 have demonstrated extensive damage in both developing embryos and progeny.
Few studies, mainly employing SCSA to detect SDF, have been undertaken to evaluate the impact of SDF on fertility in vivo in humans.65, 66, 67 These studies demonstrate a reduced probability of pregnancy arising from sperm from men with high SDF, with an overall calculated odds ratio of 7.5% and a 95% confidence interval of 2.5–22.6.65 Importantly, this appears also to be true of men with normal semen parameters,67 suggesting that the evaluation of SDF is of additional value to semen analysis. Similar results have been obtained for first-level ART (intrauterine insemination),68, 69, 70, 71 irrespective of the method used for evaluating SDF. In particular, an extended study by Bungum et al.,69 performed on a total of 998 intrauterine insemination cycles, showed significantly lower odds ratios for clinical pregnancy (CP) and delivery when the male partners had a DNA fragmentation index of more than 30% as measured by SCSA, leading the authors to suggest routine measurement of SDF in the assessment of infertile couples.
However, at this time, data demonstrating that such testing has the predictive power to inform the clinical management of infertile couples in a cost-effective manner are lacking, and this approach has not been supported in professional guidelines.
Published studies report conflicting results on the impact of sperm DNA integrity on the outcome of IVF or ICSI, in particular on the effect of sperm DNA integrity on fertilisation rate (FR) and embryo cleavage. A possible explanation for these differences is the different methods used to detect DNA integrity in these studies. In addition, the lack of standardisation of methods used to evaluate SDF is another factor affecting the results, as differences arise even when the same method is used. In Table 1, results on the impact of SDF on second-level ARTs from different studies are divided on the basis of the three main assays employed to detect SDF: SCSA, TUNEL and COMET. In particular, the three table panels (SCSA, TUNEL and COMET) show the impact of SDF on the different end points of the studies with the three methods. As can be observed, all of the studies performed with SCSA, which use FR as one of the end points, do not reveal a significant impact of SDF on it. Conversely, when TUNEL is used (Table 1, TUNEL panel), the data on the impact of SDF on FR are more variable; although most studies (8/10) show no significant effect. With the COMET assay, high levels of SDF had an effect on FR in IVF cycles but not in ICSI (Table 1). It should be noted that there are few studies evaluating the impact of SDF on ART using COMET, and all of these studies are from the same research group (Table 1, COMET panel). Overall, it appears that the amount of SDF does not correspond closely to the fertilisation ability of sperm when evaluated by SCSA or TUNEL, as was also indicated in a recent meta-analysis by Zini et al.73 This is also in line with recent literature,5 demonstrating that sperm with fragmented DNA retain the ability to fertilize oocytes. This issue merits further investigation in light of recent evidence of the existence of two sperm populations characterized by different (and opposing) relationships between their DNA fragmentation and semen quality4 (see above).
Table 1. Relationship between SDF and second-level ART according to the method used to detect SDF (studies showing a significant effect on at least one parameter are in bold).
| Method for SDF detection | Authors | ART | Results |
|---|---|---|---|
| SCSA | Bungum et al.69 (2007) | IVF | CP (33.7% with SDF≤30% 29% with SDF>30%); PL (24.4% with SDF≤30% 19% with SDF>30%), n=388 |
| ICSI | CP (37.3% with SDF≤30% 47.9% with SDF>30%); PL (15.6% with SDF≤30% 23.8% with SDF>30%), n=223 | ||
| Bungum et al.81 (2008) | IVF/ICSI | No statistical differences of SDF values between the groups who achieved CP and who did not. IVF: n=220; ICSI: n=93 | |
| Boe-Hansen et al.70 (2006) | IVF | CP (29% with SDF≤27% 14.3% with SDF>27%); IR (22.5% with SDF≤27% 18.2% with SDF>27%), n=139 | |
| ICSI | CP (27.6% with SDF≤27% 33.3% with SDF>27%); IR (28.6% with SDF≤27% 20.7% with SDF>27%), n=47 | ||
| Gandini et al.82 (2004) | IVF | FR (68.8% with SDF=12.5%), n=12 | |
| ICSI | Patients full-term pregnancy: FR (65.5%±14.9% with SDF=23.7%±21.7%)Failure: FR (73.2%±32.8% with SDF=24.6%±19.6%), n=24 | ||
| Bungum et al.68 (2004) | IVF | CP (36.6% with SDF<27% 22.2% with SDF>27%); IR (33.3% with SDF<27% 19.4% with SDF>27%), n=109 | |
| ICSI | CP (41.5% with SDF<27% 52.9% with SDF>27%); IR (31.6% with SDF<27% 37.5% with SDF>27%), n=66 | ||
| Speyer et al.83 (2010) | IVF | CP (r=−0.054, P=0.453); no pregnancy (r=0.129, P=0.074); PL (r=−0.122, P=0.091), n=124 | |
| ICSI | CP (r=0.184, P=0.022); no pregnancy (r=0.197, P=0.014); PL (r=−0.048, P=0.555), n=96 | ||
| Virro et al.84 (2004) | IVF/ICSI | FR are not statistically different between the high-SDF group (>30%) and low-SDF group (<30%), n=249 | |
| Kennedy et al.75 (2011) | IVF/ICSI | Live birth (r=0.42, P=0.01); no pregnancy (r=0.47, P=0.01), n=233; significant correlation with PL (P<0.001) | |
| Lin et al.74 (2008) | IVF | FR (82.1% with SDF<9% 84.87% with SDF=9%−27% 84.74% with SDF>27%); ER (55.2% with SDF<9% 58.67% with SDF=9%−27% 55.03% with SDF>27%); CP (48.9% with SDF<9% 52.9% with SDF=9%−27% 54.5% with SDF>27%); PL (8.7% with SDF<9% 8.3% with SDF=9%−27% 16.7% with SDF>27%), n=137 | |
| ICSI | FR (79.58% with SDF<9% 77.81% with SDF=9%−27% 79.84% with SDF>27%); ER (59.19% with SDF<9% 52.44% with SDF=9%−27% 53.34% with SDF>27%); CP (52.4% with SDF<9% 52.3% with SDF=9%−27% 47.6% with SDF>27%); PL (9.1% with SDF<9% 13.0% with SDF=9%−27% 40.0% with SDF>27%), n=86 | ||
| TUNEL | Avendano and Oehninger85 (2011) | ICSI | FR (r=−0.020 P=0.890), early embryo cleavage (r=0.044, P=0.763), n=49 |
| Bakos et al.86 (2008) | IVF | FR (negative correlation, P<0.05), embryo cleavage (no correlation), CP (no correlation), n=45 | |
| ICSI | FR (no correlation), embryo cleavage (no correlation), CP (effect, P<0.05), n=68 | ||
| Frydman et al.87 (2008) | IVF | FR (69.9% with SDF<35% 71.7% with SDF≥35%), CP (62.5% with SDF<35% 37.5% with SDF≥35%), IR (42.4% with SDF<35% 24.5% with SDF≥35%), PL (10% with SDF<35% 36.8% with SDF≥35%), live birth (56.2% with SDF<35% 23.5 with SDF≥35%), n=117 | |
| Benchaib et al.88 (2003) | IVF | FR (84.1% with SDF≤10% 70.7% with SDF>10%); percentage of blastocysts (80% with SDF≤10% 50% with SDF>10%), n=50 | |
| ICSI | FR : no effect; percentage of blastocysts (80% with SDF≤10% 50% with SDF>10%); CP (23.8% with SDF<20%, 0% with SDF>20%), n=54 | ||
| Borini et al.89 (2006) | IVF | CP (23.2% with SDF<10%, 15.4% with SDF>10%, P=0.723); PL (15.8% with SDF<10%, 50% with SDF>10%, P=0.194), n=82 | |
| ICSI | CP (45% with SD<10%, 10% with SDF>10%, P=0.007); PL (0% with SDF<10%, 62.5% with SDF>10%, P=0.009), n=50 | ||
| Daris et al.90 (2010) | ICSI | FR (65.6% with SDF≤20% 54.9% with SDF>20%), n=20 | |
| Marchetti et al.91 (2002) | IVF | FR (r=–0.45, P=0.001 in raw semen; r=–0.01, P=NS in selected sperm), n=111 | |
| Sun et al.92 (1997) | IVF | FR (r=−0.16, P<0.05); embryo cleavage rate (r=−0.20, P<0.02), n=143 | |
| Benchaib et al.93 (2007) | IVF | FR (68.3% with SDF<15% 70.6% with SDF>15%); pregnancy/transfer (31.6% (24/76) with SDF<15% 50.0% (4/8) with SDF>15%); PL (9.1% with SDF<15% 50.0% with SDF>15%), n=88 | |
| ICSI | FR (75.4% with SDF<15% 70.3% with SDF>15%); pregnancy/transfer (37.4% (68/182) with SDF<15% 27.8% (10/36) with SDF>15%); PL (8.6% with SDF<15% 30.0% with SDF>15%), n=234 | ||
| Henkel et al.94 (2004) | IVF | FR (r=0.0502, P=0.5234); CP (r=−0.0984, P=0.2102), n=167 | |
| Henkel et al.95 (2003) | IVF | FR (r=0.0113, P=0.8718); ER (r=0.0406, P=0.5855); CP (r=−0.0889, P=0.2016), n=208 | |
| ICSI | FR (r=−0.2678, P=0.0574); ER (r=0.1666, P=0.2475); CP (r=−0.0352, P=0.8065), n=54 | ||
| COMET | Simon et al.45 (2010) | IVF | FR (69.9% with SDF=0%–20% 66.4% with SDF=21%–40% 54.4% with SDF=61%–100% in selected sperm, no differences in raw semen); embryo score (15.5% with SDF=0%–20% 10.7% with SDF=61%–100% in raw semen; 7.3% with SDF=61%–100% in selected semen); embryo transfer (26.7% with SDF=0%–20% 38.1% with SDF=61%–100% in raw semen; 34.1% with SDF=0%–20% 18.7% with SDF=61%–100% in selected sperm), n=230 |
| Alkaline-COMET vs COMET-FpG | |||
| SDF-Pr (Alkaline COMET)=39.5% vs. SDF-NPr (Alkaline COMET)=51.7%, P=0.004 in raw semen; SDF-Pr (Alkaline COMET)=26.9% vs. SDF-NPr (Alkaline COMET)=36.8%, P=0.01 in selected sperm; | |||
| SDF-Pr (COMET-FpG)=54.7% vs. SDF-NPr (COMET-FpG)=71.8%, P=0.009 in raw semen; SDF-Pr (COMET-FpG)=42.2% vs. SDF-NPr (COMET-FpG)=56.0%, P=0.045 in selected sperm, n=73 | |||
| ICSI | FR (no differences between different DFI values); embryo score (no differences between different DFI values); embryo transfer (no differences between different SDF values), n=130 | ||
| Alkaline-COMET vs COMET-FpG | |||
| SDF-Pr (Alkaline COMET)=58.9% vs. SDF-NPr (Alkaline COMET)=67.2%, P=0.109 in raw semen; SDF-Pr (Alkaline COMET)=45.5% vs. SDF-NPr (Alkaline COMET)=51.7%, P=0.243 in selected sperm; | |||
| SDF-Pr (COMET-FpG)=63.1% vs. SDF-NPr (COMET-FpG)=79.9%, P=0.008 in raw semen; SDF-Pr (COMET-FpG)=50.0% vs. SDF-NPr (COMET-FpG)=65.5%, P=0.024 in selected sperm, n=53 | |||
| Simon et al.72 (2011) | IVF | FR (r2=0.243, P=0.050 in raw semen; r2=0.276, P=0.025 in selected sperm); embryo quality (r2=−0.415, P=0.002 in raw semen; r2=−0.373, P=0.007) in selected sperm), n=75 | |
| Lewis et al.96 (2004) | ICSI | There was no significant relationship between SDF and FR, n=77 |
Abbreviations: ART, assisted reproduction techniques; CP, clinical pregnancy; ER, embryo loss; FpG, formamidopyrimidine DNA glycosilase; FR, fertilisation rate; ICSI, intracytoplasmic sperm injection; IR, implantation rate; IVF, in vitro fertilisation; NPr, non-pregnancy; NS, not significant; Pr, pregnancy; PrL, pregnancy loss; SDF, sperm DNA fragmentation.
Most studies (6/9) using TUNEL report a significant impact of SDF on embryo cleavage, blastocyst development and CP parameters (Table 1, TUNEL panel), both with the IVF and ICSI ART techniques. Conversely, studies performed with SCSA obtained more variable results; only half of them report a significant effect of SDF on CP (Table 1, SCSA panel). Furthermore, a meta-analysis of studies that used TUNEL or SCSA to evaluate the impact of SDF on ART outcomes37 revealed a difference in the correlation of SDF with CP, depending on the method of evaluation: CP showed a significant relationship with SDF only in pooled TUNEL studies. Interestingly, the overall predictive value of SDF on CP as assessed by COMET is significant and increases when the COMET assay is performed in conjunction with FpG treatment (hence including the oxidative DNA damage), both for IVF and ICSI45 (Table 1, COMET panel).
Several of the studies reported in Table 1 evaluated the impact of SDF on pregnancy loss (PL). Interestingly, all of the studies using TUNEL (Table 1, TUNEL panel) report a clear, direct relationship between PL and the occurrence and extent of SDF. Conversely, among those studies using SCSA (Table 1, SCSA panel), only the studies by Lin et al.74 and Kennedy et al.75 report a significant impact of high SDF on PL. Studies using COMET did not evaluate PL.
It appears that TUNEL is more sensitive as a predictor of PL than SCSA, as was also revealed in a recent meta-analysis.73 Another study76 demonstrated that there was high DNA damage (aneuploidy and SDF) in the male partners in couples with a history of recurrent miscarriages, suggesting a ‘paternal factor' in early miscarriage.
Conclusions and future directions
As of today, DNA fragmentation is the most frequent DNA alteration in sperm, and its clinical relevance is now emerging. DNA fragmentation has an important impact, independent of the parameters of classic semen analysis, on both natural and assisted reproduction. In particular, it is now evident that DNA fragmentation is associated with alterations in embryo quality, leading to a decreased rate of implantation or an increased rate of early miscarriage in ART. However, pharmacological treatments (based on the administration of anti-oxidants) aimed at decreasing SDF have demonstrate little beneficial effect, indicating the need for developing additional strategies to reduce SDF. In this respect, more attention should be paid to define the type, as well as the origin, of DNA damage in sperm.
In our opinion, there are several points that should be considered regarding the introduction of SDF into the routine analysis of male infertility and before the application of ART procedures. Although solid data from several studies show that there is more SDF in infertile or subfertile males than fertile males, it is less clear whether knowledge of this parameter is helpful in providing treatment guidance for infertile couples. As mentioned above, the evaluation of SDF may be useful in those couples who are eligible for first-level ART, as the extent of SDF has been found to correlate strongly with the outcome of intrauterine insemination application. Conversely, studies on the impact of SDF on the outcome of second-level ART are inconsistent, leaving doubts about the clinical utility of SDF in decision-making for couples undergoing these procedures.73, 77 Although there are several possible reasons for conflicting results (including patient selection and age of the female partner), the technique used to evaluate SDF can significantly affect the second-level ART outcome and yield markedly different results (Table 1). It appears that those methods that directly evaluate the occurrence of DNA strand breaks (such as TUNEL, COMET and COMET/FpG) better define the relationship between SDF and ART outcomes. Not only is standardisation needed for both assays, but also the definition of threshold values of SDF in fertile men must be determined. These studies are difficult, and more subjects need to be enrolled in future studies so that the many confounding factors can be considered. These factors include age, partner lifestyle, oocyte quality, the experience of the ART centre and so on.
There are certain categories of patient who may benefit from SDF evaluation before undergoing ART or attempting to conceive naturally: subjects who have been heavily exposed to toxicants or radiochemotherapies, which may lead to persistent SDF;78, 79 those affected by diabetes, who may have increased SDF;80 male partners in couples who have experienced repetitive, unexplained PL;73 or male partners in couples who have experienced repeated, unexplained failure of fertilisation. In addition, it has been shown that cancer patients may have increased SDF in their semen, even before chemotherapy.78, 79 The increased SDF in cancer patients may be a problem for semen cryopreservation and the eventual utilisation of cryopreserved semen for ARTs because the deleterious effects of the cryopreservation procedure may further increase SDF. In these cases, the evaluation of SDF may be useful to the clinician for counselling the couple.
The authors declare no competing financial interests.
References
- Lopes S, Sun JG, Jurisicova A, Meriano J, Casper RF. Sperm deoxyribonucleic acid fragmentation is increased in poor-quality semen samples and correlates with failed fertilization in intracytoplasmic sperm injection. Fertil Steril. 1998;69:528–32. doi: 10.1016/s0015-0282(97)00536-0. [DOI] [PubMed] [Google Scholar]
- Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, et al. DNA integrity in human spermatozoa: relationships with semen quality. J Androl. 2000;21:33–44. [PubMed] [Google Scholar]
- Muratori M, Piomboni P, Baldi E, Filimberti E, Pecchioli P, et al. Functional and ultra-structural features of DNA fragmented human sperm. J Androl. 2000;21:903–12. [PubMed] [Google Scholar]
- Muratori M, Marchiani S, Tamburrino L, Tocci V, Forti G, et al. Nuclear staining identifies two populations of human sperm with different DNA fragmentation extent and relationship with semen parameters. Human Reprod. 2008;23:1035–43. doi: 10.1093/humrep/den058. [DOI] [PubMed] [Google Scholar]
- Yamauchi Y, Riel JM, Ward MA.Paternal DNA damage resulting from various sperm treatments persists after fertilization and is similar prior and after DNA replication J Androl 2011. e-pub ahead of print 5 May 2011; doi: 10.2164/jandrol.111.013532. [DOI] [PMC free article] [PubMed]
- Ménézo Y, Dale B, Cohen M. DNA damage and repair in human oocytes and embryos: a review. Zygote. 2010;18:357–65. doi: 10.1017/S0967199410000286. [DOI] [PubMed] [Google Scholar]
- Derijck A, van der Heijden G, Giele M, Philippens M, de Boer P. DNA double-strand break repair in parental chromatin of mouse zygotes, the first cell cycle as an origin of de novo mutation. Hum Mol Genet. 2008;17:1922–37. doi: 10.1093/hmg/ddn090. [DOI] [PubMed] [Google Scholar]
- Muratori M, Maggi M, Spinelli S, Filimberti E, Forti G, et al. Spontaneous DNA fragmentation in swim up selected human spermatozoa during long term incubation. J Androl. 2003;24:253–62. doi: 10.1002/j.1939-4640.2003.tb02670.x. [DOI] [PubMed] [Google Scholar]
- Sakkas D, Mariethoz E, Manicardi G, Bizzaro D, Bianchi PG, et al. Origin of DNA damage in ejaculated human spermatozoa. Rev Reprod. 1999;4:31–7. doi: 10.1530/ror.0.0040031. [DOI] [PubMed] [Google Scholar]
- Sakkas D, Mariethoz E, St John JC. Abnormal sperm parameters in humans are indicative of an abortive apoptotic mechanism linked to the Fas-mediated pathway. Exp Cell Res. 1999;251:350–5. doi: 10.1006/excr.1999.4586. [DOI] [PubMed] [Google Scholar]
- Baccetti B, Strehler E, Capitani S, Collodel G, de Santo M, et al. The effect of follicle stimulating hormone therapy on human sperm structure (Notulae seminologicae 11) Hum Reprod. 1997;12:1955–68. doi: 10.1093/humrep/12.9.1955. [DOI] [PubMed] [Google Scholar]
- Muratori M, Porazzi I, Luconi M, Marchiani S, Forti G, et al. AnnexinV binding and merocyanine staining fail to detect human sperm capacitation. J Androl. 2004;25:797–810. doi: 10.1002/j.1939-4640.2004.tb02858.x. [DOI] [PubMed] [Google Scholar]
- Marchiani S, Tamburrino L, Maoggi A, Vannelli GB, Forti G, et al. Characterization of M540 bodies in human semen: evidence that they are apoptotic bodies. Mol Hum Reprod. 2007;13:621–31. doi: 10.1093/molehr/gam046. [DOI] [PubMed] [Google Scholar]
- Sakkas D, Moffatt O, Manicardi GC, Mariethoz E, Tarozzi N, et al. Nature of DNA damage in ejaculated human spermatozoa and the possible involvement of apoptosis. Biol Reprod. 2002;66:1061–7. doi: 10.1095/biolreprod66.4.1061. [DOI] [PubMed] [Google Scholar]
- Sakkas D, Manicardi G, Bianchi PG, Bizzaro D, Bianchi U. Relationship between the presence of endogenous nicks and sperm chromatin packaging in maturing and fertilizing mouse spermatozoa. Biol Reprod. 1995;52:1149–55. doi: 10.1095/biolreprod52.5.1149. [DOI] [PubMed] [Google Scholar]
- Marcon L, Boissonneault G. Transient DNA strand breaks during mouse and human spermiogenesis new insights in stage specificity and link to chromatin remodeling. Biol Reprod. 2004;70:910–8. doi: 10.1095/biolreprod.103.022541. [DOI] [PubMed] [Google Scholar]
- McPherson S, Longo FJ. Chromatin structure function alterations during mammalian spermatogenesis: DNA nicking and repair in elongating spermatids. Eur J Histochem. 1993;37:109–28. [PubMed] [Google Scholar]
- Leduc F, Maquennehan V, Nkoma GB, Boissonneault G. DNA damage response during chromatin remodeling in elongating spermatids of mice. Biol Reprod. 2008;78:324–32. doi: 10.1095/biolreprod.107.064162. [DOI] [PubMed] [Google Scholar]
- Meyer-Ficca ML, Lonchar JD, Ihara M, Meistrich ML, Austin CA, et al. Poly(ADP-ribose) polymerases PARP1 and PARP2 modulate topoisomerase II beta (TOP2B) function during chromatin condensation in mouse spermiogenesis. Biol Reprod. 2011;84:900–9. doi: 10.1095/biolreprod.110.090035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco E, Scarselli F, Iacobelli M, Rienzi L, Ubaldi F, et al. Efficient treatment of infertility due to sperm DNA damage by ICSI with testicular spermatozoa. Hum Reprod. 2005;20:226–30. doi: 10.1093/humrep/deh590. [DOI] [PubMed] [Google Scholar]
- Moskovtsev SI, Jarvi K, Mullen JB, Cadesky KI, Hannam T, et al. Testicular spermatozoa have statistically significantly lower DNA damage compared with ejaculated spermatozoa in patients with unsuccessful oral antioxidant treatment. Fertil Steril. 2010;93:1142–6. doi: 10.1016/j.fertnstert.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Aitken J, Krausz C, Buckingham D. Relationships between biochemical markers for residual sperm cytoplasm, reactive oxygen species generation, and the presence of leukocytes and precursor germ cells in human sperm suspensions. Mol Reprod Dev. 1994;39:268–79. doi: 10.1002/mrd.1080390304. [DOI] [PubMed] [Google Scholar]
- Said TM, Agarwal A, Falcone T, Sharma RK, Bedaiwy MA, et al. Infliximab may reverse the toxic effects induced by tumor necrosis factor alpha in human spermatozoa: an in vitro model. Fertil Steril. 2005;83:1665–73. doi: 10.1016/j.fertnstert.2004.11.068. [DOI] [PubMed] [Google Scholar]
- Perdichizzi A, Nicoletti F, la Vignera S, Barone N, D'Agata R, et al. Effects of tumour necrosis factor-alpha on human sperm motility and apoptosis. J Clin Immunol. 2007;27:152–62. doi: 10.1007/s10875-007-9071-5. [DOI] [PubMed] [Google Scholar]
- Henkel R, Kierspel E, Stalf T, Mehnert C, Menkveld R, et al. Effect of reactive oxygen species produced by spermatozoa and leukocytes on sperm functions in non-leukocytospermic patients. Fertil Steril. 2005;83:635–42. doi: 10.1016/j.fertnstert.2004.11.022. [DOI] [PubMed] [Google Scholar]
- Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol. 2008;59:2–11. doi: 10.1111/j.1600-0897.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- Greco E, Iacobelli M, Rienzi L, Ubaldi F, Ferrero S, et al. Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J Androl. 2005;26:349–53. doi: 10.2164/jandrol.04146. [DOI] [PubMed] [Google Scholar]
- de Iuliis GN, Thomson LK, Mitchell LA, Finnie JM, Koppers AJ, et al. DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-hydroxy-2'-deoxyguanosine, a marker of oxidative stress. Biol Reprod. 2009;81:517–24. doi: 10.1095/biolreprod.109.076836. [DOI] [PubMed] [Google Scholar]
- Oger I, da Cruz C, Panteix G, Menezo Y. Evaluating human sperm DNA integrity: relationship between 8-hydroxydeoxyguanosine quantification and the sperm chromatin structure assay. Zygote. 2003;11:367–71. doi: 10.1017/s0967199403002442. [DOI] [PubMed] [Google Scholar]
- Zribi N, Chakroun NF, Elleuch H, Abdallah FB, Ben Hamida AS, et al. Sperm DNA fragmentation and oxidation are independent of malondialdheyde. Reprod Biol Endocrinol. 2011;9:47. doi: 10.1186/1477-7827-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zribi N, Feki Chakroun N, El Euch H, Gargouri J, Bahloul A, et al. Effects of cryopreservation on human sperm deoxyribonucleic acid integrity. Fertil Steril. 2010;93:159–66. doi: 10.1016/j.fertnstert.2008.09.038. [DOI] [PubMed] [Google Scholar]
- Montjean D, Ménézo Y, Benkhalifa M, Cohen M, Belloc S, et al. Malonaldehyde formation and DNA fragmentation: two independent sperm decays linked to reactive oxygen species. Zygote. 2010;18:265–8. doi: 10.1017/S0967199409990311. [DOI] [PubMed] [Google Scholar]
- Muratori M, Forti G, Baldi E. Comparing flow cytometry and fluorescence microscopy for analyzing human sperm DNA fragmentation by TUNEL labeling. Cytometry A. 2008;73:785–7. doi: 10.1002/cyto.a.20615. [DOI] [PubMed] [Google Scholar]
- Evenson DP, Kasperson K, Wixon RL. Analysis of sperm DNA fragmentation using flow cytometry and other techniques. Soc Reprod Fertil Suppl. 2007;65:93–113. [PubMed] [Google Scholar]
- Muratori M, Tamburrino L, Tocci V, Costantino A, Marchiani S, et al. Small variations in crucial steps of TUNEL assay coupled to flow cytometry greatly affect measures of sperm DNA fragmentation. J Androl. 2010;31:336–45. doi: 10.2164/jandrol.109.008508. [DOI] [PubMed] [Google Scholar]
- Muratori M, Tamburrino L, Marchiani S, Guido C, Forti G, et al. Critical aspects of detection of sperm DNA fragmentation by TUNEL/flow cytometry. Syst Biol Reprod Med. 2010;56:277–5. doi: 10.3109/19396368.2010.489660. [DOI] [PubMed] [Google Scholar]
- Li Z, Wang L, Cai J, Huang H. Correlation of sperm DNA damage with IVF and ICSI outcomes: a systematic review and meta-analysis. J Assist Reprod Genet. 2006;23:367–76. doi: 10.1007/s10815-006-9066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez JG. The predictive value of sperm chromatin structure assay. Hum Reprod. 2005;20:2365–7. doi: 10.1093/humrep/dei014. [DOI] [PubMed] [Google Scholar]
- Singh NP, McCoy MT, Tice RR, Schneider EL. A simple technique for quantification of low levels of DNA damage in individual cells. Exp Cell Res. 1988;17:184–91. doi: 10.1016/0014-4827(88)90265-0. [DOI] [PubMed] [Google Scholar]
- Shen H, Ong C. Detection of oxidative DNA damage in human sperm and its association with sperm function and male infertility. Free Radic Biol Med. 2000;28:529–36. doi: 10.1016/s0891-5849(99)00234-8. [DOI] [PubMed] [Google Scholar]
- McKelvey-Martin VJ, Melia N, Walsh IK, Johnston SR, Hughes CM, et al. Two potential clinical applications of the alkaline single-cell gel electrophoresis assay: (1) human bladder washings and transitional cell carcinoma of the bladder; and (2) human sperm and male infertility. Mutat Res. 1997;375:93–104. doi: 10.1016/s0027-5107(97)00005-5. [DOI] [PubMed] [Google Scholar]
- Zini A, Sigman M. Are tests of sperm DNA damage clinically useful? Pros and cons. J Androl. 2009;30:219–29. doi: 10.2164/jandrol.108.006908. [DOI] [PubMed] [Google Scholar]
- Mitchell LA, de Iuliis GN, Aitken RJ. The TUNEL assay consistently underestimates DNA damage in human spermatozoa and is influenced by DNA compaction and cell vitality: development of an improved methodology. Int J Androl. 2011;34:2–13. doi: 10.1111/j.1365-2605.2009.01042.x. [DOI] [PubMed] [Google Scholar]
- Aitken RJ, de Iuliis GN, Finnie JM, Hedges A, McLachlan RI. Analysis of the relationships between oxidative stress, DNA damage and sperm vitality in a patient population: development of diagnostic criteria. Hum Reprod. 2010;25:2415–26. doi: 10.1093/humrep/deq214. [DOI] [PubMed] [Google Scholar]
- Simon L, Brunborg G, Stevenson M, Lutton D, McManus J, et al. Clinical significance of sperm DNA damage in assisted reproduction outcome. Hum Reprod. 2010;25:1594–608. doi: 10.1093/humrep/deq103. [DOI] [PubMed] [Google Scholar]
- Tunc O, Tremellen K. Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J Assist Reprod Genet. 2009;26:537–44. doi: 10.1007/s10815-009-9346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ménézo YJ, Hazout A, Panteix G, Robert F, Rollet J, et al. Antioxidants to reduce sperm DNA fragmentation: an unexpected adverse effect. Reprod Biomed Online. 2007;14:418–21. doi: 10.1016/s1472-6483(10)60887-5. [DOI] [PubMed] [Google Scholar]
- Moskovtsev SI, Lecker I, Mullen JB, Jarvi K, Willis J, et al. Cause-specific treatment in patients with high sperm DNA damage resulted in significant DNA improvement. Syst Biol Reprod Med. 2009;55:109–15. doi: 10.1080/19396360902787944. [DOI] [PubMed] [Google Scholar]
- Sergerie M, Laforest G, Boulanger K, Bissonnette F, Bleau G. Longitudinal study of sperm DNA fragmentation as measured by terminal uridine nick end-labelling assay. Hum Reprod. 2005;20:1921–7. doi: 10.1093/humrep/deh885. [DOI] [PubMed] [Google Scholar]
- Erenpreiss J, Bungum M, Spano M, Elzanaty S, Orbidans J, et al. Intra-individual variation in sperm chromatin structure assay parameters in men from infertile couples: clinical implications. Hum Reprod. 2006;21:2061–4. doi: 10.1093/humrep/del134. [DOI] [PubMed] [Google Scholar]
- Showell MG, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. . Cochrane Database Syst Rev. 2011;1:CD007411. doi: 10.1002/14651858.CD007411.pub2. [DOI] [PubMed] [Google Scholar]
- Branco CS, Garcez ME, Pasqualotto FF, Erdtman B, Salvador M. Resveratrol and ascorbic acid prevent DNA damage induced by cryopreservation in human semen. Cryobiology. 2010;60:235–7. doi: 10.1016/j.cryobiol.2009.10.012. [DOI] [PubMed] [Google Scholar]
- Toro E, Fernández S, Colomar A, Casanovas A, Alvarez JG, et al. Processing of semen can result in increased sperm DNA fragmentation. Fertil Steril. 2009;92:2109–12. doi: 10.1016/j.fertnstert.2009.05.059. [DOI] [PubMed] [Google Scholar]
- Thomson LK, Fleming SD, Aitken RJ, de Iuliis GN, Zieschang JA, et al. Cryopreservation-induced human sperm DNA damage is predominantly mediated by oxidative stress rather than apoptosis. Hum Reprod. 2009;24:2061–70. doi: 10.1093/humrep/dep214. [DOI] [PubMed] [Google Scholar]
- Saleh RA, Agarwal A, Sharma RK, Said TM, Sikka SC, et al. Evaluation of nuclear DNA damage in spermatozoa from infertile men with varicocele. Fertil Steril. 2003;80:1431–6. doi: 10.1016/s0015-0282(03)02211-8. [DOI] [PubMed] [Google Scholar]
- Enciso M, Muriel L, Fernández JL, Goyanes V, Segrelles E, et al. Infertile men with varicocele show a high relative proportion of sperm cells with intense nuclear damage level, evidenced by the sperm chromatin dispersion test. J Androl. 2006;27:106–11. doi: 10.2164/jandrol.05115. [DOI] [PubMed] [Google Scholar]
- Smith R, Kaune H, Parodi D, Madariaga M, Rios R, et al. Increased sperm DNA damage in patients with varicocele: relationship with seminal oxidative stress. Hum Reprod. 2006;21:986–93. doi: 10.1093/humrep/dei429. [DOI] [PubMed] [Google Scholar]
- Werthman P, Wixon R, Kasperson K, Evenson DP. Significant decrease in sperm deoxyribonucleic acid fragmentation after varicocelectomy. Fertil Steril. 2008;90:1800–4. doi: 10.1016/j.fertnstert.2006.09.019. [DOI] [PubMed] [Google Scholar]
- Smit M, Romijn JC, Wildhagen MF, Veldhoven JL, Weber RF, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2010;183:270–4. doi: 10.1016/j.juro.2009.08.161. [DOI] [PubMed] [Google Scholar]
- Zini A, Azhar R, Baazeem A, Gabriel MS. Effect of microsurgical varicocelectomy on human sperm chromatin and DNA integrity: a prospective trial. Int J Androl. 2011;34:14–9. doi: 10.1111/j.1365-2605.2009.01048.x. [DOI] [PubMed] [Google Scholar]
- Lacerda JI, del Giudice PT, da Silva BF, Nichi M, Fariello RM, et al. Adolescent varicocele: improved sperm function after varicocelectomy. Fertil Steril. 2011;95:994–9. doi: 10.1016/j.fertnstert.2010.10.031. [DOI] [PubMed] [Google Scholar]
- la Vignera S, Condorelli R, Vicari E, D'Agata R, Calogero AE.Effects of varicocelectomy on sperm DNA fragmentation, mitochondrial function, chromatin condensation, and apoptosis J Androle-pub ahead of print 2 June 2011; doi: 10.2164/jandrol.111.013433. [DOI] [PubMed]
- Fatehi AN, Bevers MM, Schoevers E, Roelen BA, Colenbrander B, et al. DNA damage in bovine sperm does not block fertilization and early embryonic development but induces apoptosis after the first cleavages. J Androl. 2006;27:176–88. doi: 10.2164/jandrol.04152. [DOI] [PubMed] [Google Scholar]
- Fernández-Gonzalez R, Moreira PN, Pérez-Crespo M, Sánchez-Martín M, Ramirez MA, et al. Long-term effects of mouse intracytoplasmic sperm injection with DNA-fragmented sperm on health and behavior of adult offspring. Biol Reprod. 2008;78:761–72. doi: 10.1095/biolreprod.107.065623. [DOI] [PubMed] [Google Scholar]
- Evenson DP, Wixon R. Data analysis of two in vivo fertility studies using Sperm Chromatin Structure Assay-derived DNA fragmentation index vs. pregnancy outcome. Fertil Steril. 2008;90:1229–31. doi: 10.1016/j.fertnstert.2007.10.066. [DOI] [PubMed] [Google Scholar]
- Spanò M, Bonde JP, Hjøllund HI, Kolstad HA, Cordelli E, et al. Sperm chromatin damage impairs human fertility. The Danish First Pregnancy Planner Study Team. Fertil Steril. 2000;73:43–50. doi: 10.1016/s0015-0282(99)00462-8. [DOI] [PubMed] [Google Scholar]
- Giwercman A, Lindstedt L, Larsson M, Bungum M, Spano M, et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: a case–control study. Int J Androl. 2010;33:e221–7. doi: 10.1111/j.1365-2605.2009.00995.x. [DOI] [PubMed] [Google Scholar]
- Bungum M, Humaidan P, Spano M, Jepson K, Bungum L, et al. The predictive value of sperm chromatin structure assay (SCSA) parameters for the outcome of intrauterine insemination, IVF and ICSI. Hum Reprod. 2004;19:1401–8. doi: 10.1093/humrep/deh280. [DOI] [PubMed] [Google Scholar]
- Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22:174–9. doi: 10.1093/humrep/del326. [DOI] [PubMed] [Google Scholar]
- Boe-Hansen GB, Fedder J, Ersbøll AK, Christensen P. The sperm chromatin structure assay as a diagnostic tool in the human fertility clinic. Hum Reprod. 2006;21:1576–82. doi: 10.1093/humrep/del019. [DOI] [PubMed] [Google Scholar]
- Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod. 2002;17:3122–8. doi: 10.1093/humrep/17.12.3122. [DOI] [PubMed] [Google Scholar]
- Simon L, Lutton D, McManus J, Lewis SE. Sperm DNA damage measured by the alkaline Comet assay as an independent predictor of male infertility and in vitro fertilization success. Fertil Steril. 2011;95:652–7. doi: 10.1016/j.fertnstert.2010.08.019. [DOI] [PubMed] [Google Scholar]
- Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23:2663–8. doi: 10.1093/humrep/den321. [DOI] [PubMed] [Google Scholar]
- Lin MH, Kuo-Kuang Lee R, Li SH, Lu CH, Sun FJ, et al. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90:352–9. doi: 10.1016/j.fertnstert.2007.06.018. [DOI] [PubMed] [Google Scholar]
- Kennedy C, Ahlering P, Rodriguez H, Levy S, Sutovsky P. Sperm chromatin structure correlates with spontaneous abortion and multiple pregnancy rates in assisted reproduction. Reprod Biomed Online. 2011;22:272–6. doi: 10.1016/j.rbmo.2010.11.020. [DOI] [PubMed] [Google Scholar]
- Carrell DT, Wilcox AL, Lowy L, Peterson CM, Jones KP, et al. Elevated sperm chromosome aneuploidy and apoptosis in patients with unexplained recurrent pregnancy loss. Obstet Gynecol. 2003;101:1229–35. doi: 10.1016/s0029-7844(03)00339-9. [DOI] [PubMed] [Google Scholar]
- Collins JA, Barnhart KT, Schlegel PN. Do sperm DNA integrity tests predict pregnancy with in vitro fertilization. Fertil Steril. 2008;89:823–31. doi: 10.1016/j.fertnstert.2007.04.055. [DOI] [PubMed] [Google Scholar]
- O'Flaherty C, Hales BF, Chan P, Robaire B. Impact of chemotherapeutics and advanced testicular cancer or Hodgkin lymphoma on sperm deoxyribonucleic acid integrity. Fertil Steril. 2010;94:1374–9. doi: 10.1016/j.fertnstert.2009.05.068. [DOI] [PubMed] [Google Scholar]
- Smit M, van Casteren NJ, Wildhagen MF, Romijn JC, Dohle GR. Sperm DNA integrity in cancer patients before and after cytotoxic treatment. Hum Reprod. 2010;25:1877–83. doi: 10.1093/humrep/deq104. [DOI] [PubMed] [Google Scholar]
- Agbaje IM, McVicar CM, Schock BC, McClure N, Atkinson AB, et al. Increased concentrations of the oxidative DNA adduct 7,8-dihydro-8-oxo-2-deoxyguanosine in the germ-line of men with type 1 diabetes. Reprod Biomed Online. 2008;16:401–9. doi: 10.1016/s1472-6483(10)60602-5. [DOI] [PubMed] [Google Scholar]
- Bungum M, Spanò M, Humaidan P, Eleuteri P, Rescia M, et al. Sperm chromatin structure assay parameters measured after density gradient centrifugation are not predictive for the outcome of ART. Hum Reprod. 2008;23:4–10. doi: 10.1093/humrep/dem353. [DOI] [PubMed] [Google Scholar]
- Gandini L, Lombardo F, Paoli D, Caruso F, Eleuteri P, et al. Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod. 2004;19:1409–17. doi: 10.1093/humrep/deh233. [DOI] [PubMed] [Google Scholar]
- Speyer BE, Pizzey AR, Ranieri M, Joshi R, Delhanty JD, et al. Fall in implantation rates following ICSI with sperm with high DNA fragmentation. Hum Reprod. 2010;25:1609–18. doi: 10.1093/humrep/deq116. [DOI] [PubMed] [Google Scholar]
- Virro MR, Larson-Cook KL, Evenson DP. Sperm chromatin structure assay (SCSA) parameters are related to fertilization, blastocyst development, and ongoing pregnancy in in vitro fertilization and intracytoplasmic sperm injection cycles. Fertil Steril. 2004;81:1289–95. doi: 10.1016/j.fertnstert.2003.09.063. [DOI] [PubMed] [Google Scholar]
- Avendano C, Oehninger S. DNA fragmentation in morphologically normal spermatozoa: how much should we be concerned in the ICSI era. J Androl. 2011;32:356–63. doi: 10.2164/jandrol.110.012005. [DOI] [PubMed] [Google Scholar]
- Bakos HW, Thompson JG, Feil D, Lane M. Sperm DNA damage is associated with assisted reproductive technology pregnancy. Int J Androl. 2008;31:518–26. doi: 10.1111/j.1365-2605.2007.00803.x. [DOI] [PubMed] [Google Scholar]
- Frydman N, Prisant N, Hesters L, Frydman R, Tachdjian G, et al. Adequate ovarian follicular status does not prevent the decrease in pregnancy rates associated with high sperm DNA fragmentation. Fertil Steril. 2008;89:92–7. doi: 10.1016/j.fertnstert.2007.02.022. [DOI] [PubMed] [Google Scholar]
- Benchaib M, Braun V, Lornage J, Hadj S, Salle B, et al. Sperm DNA fragmentation decreases the pregnancy rate in an assisted reproductive technique. Hum Reprod. 2003;18:1023–8. doi: 10.1093/humrep/deg228. [DOI] [PubMed] [Google Scholar]
- Borini A, Tarozzi N, Bizzaro D, Bonu MA, Fava L, et al. Sperm DNA fragmentation: paternal effect on early post-implantation embryo development in ART. Hum Reprod. 2006;21:2876–81. doi: 10.1093/humrep/del251. [DOI] [PubMed] [Google Scholar]
- Daris B, Goropevsek A, Hojnik N, Vlaisavljević V. Sperm morphological abnormalities as indicators of DNA fragmentation and fertilization in ICSI. Arch Gynecol Obstet. 2010;281:363–7. doi: 10.1007/s00404-009-1140-y. [DOI] [PubMed] [Google Scholar]
- Marchetti C, Obert G, Deffosez A, Formstecher P, Marchetti P. Study of mitochondrial membrane potential, reactive oxygen species, DNA fragmentation and cell viability by flow cytometry in human sperm. Hum Reprod. 2002;17:1257–65. doi: 10.1093/humrep/17.5.1257. [DOI] [PubMed] [Google Scholar]
- Sun JG, Jurisicova A, Casper RF. Detection of deoxyribonucleic acid fragmentation in human sperm: correlation with fertilization in vitro. . Biol Reprod. 1997;56:602–7. doi: 10.1095/biolreprod56.3.602. [DOI] [PubMed] [Google Scholar]
- Benchaib M, Lornage J, Mazoyer C, Lejeune H, Salle B, et al. Sperm deoxyribonucleic acid fragmentation as a prognostic indicator of assisted reproductive technology outcome. Fertil Steril. 2007;87:93–100. doi: 10.1016/j.fertnstert.2006.05.057. [DOI] [PubMed] [Google Scholar]
- Henkel R, Hajimohammad M, Stalf T, Hoogendijk C, Mehnert C, et al. Influence of deoxyribonucleic acid damage on fertilization and pregnancy. Fertil Steril. 2004;81:965–72. doi: 10.1016/j.fertnstert.2003.09.044. [DOI] [PubMed] [Google Scholar]
- Henkel R, Kierspel E, Hajimohammad M, Stalf T, Hoogendijk C, et al. DNA fragmentation of spermatozoa and assisted reproduction technology. Reprod Biomed Online. 2003;7:477–84. doi: 10.1016/s1472-6483(10)61893-7. [DOI] [PubMed] [Google Scholar]
- Lewis SE, O'Connell M, Stevenson M, Thompson-Cree L, McClure N. An algorithm to predict pregnancy in assisted reproduction. Hum Reprod. 2004;19:1385–94. doi: 10.1093/humrep/deh227. [DOI] [PubMed] [Google Scholar]