Abstract
Background
Many critically ill (CI) patients are transferred to other care facilities instead of to home at hospital discharge.
Objective
To identify patient factors associated with hospital discharge to care facility following CI, and to estimate the magnitude of risk associated with each factor.
Methods
Retrospective cohort study conducted in a medical intensive care unit. We studied 548 survivors of CI. Multivariable logistic regression was employed to identify independent risk factors for discharge to care facility. Only the first 72 hours of intensive care were analyzed.
Results
Approximately one-quarter of the survivors of CI were discharged to a care facility instead of to home (143/548, 26.1%). This event occurred more commonly in older patients, even after adjustment for severity of illness and comorbidities (odds ratio [OR] 1.8 for patients ≥ 65 years of age versus patients < 65 years; 95% confidence interval [CI] 1.1–3.1, p=0.02). The risk was greatest for patients who received mechanical ventilation (OR 3.4; 95% CI 2.0–5.8; p<0.001) or had hospitalizations characterized by severe cognitive dysfunction (OR 8.1; 95% CI 1.3–50.6; p=0.02) or poor strength and/or mobility (OR 31.7; 95% CI 6.4–157.3; p<0.001). The model showed good discrimination (area under the curve 0.82; 95% CI 0.77–0.86).
Conclusion
Our model, which did not include baseline function or social variables, provided good discrimination between patients discharged to care facility following CI and patients discharged to home. These results suggest that future research should focus on the debilitating effects of respiratory failure and on conditions with cognitive and neuromuscular sequelae.
CINAHL key words: critical illness, critical care nursing, chronic disease, long term care, nursing homes
INTRODUCTION
Why do some survivors of critical illness return home on hospital discharge, while others are discharged to another care facility? This question has received very little attention despite its likely importance as a patient-centered outcome, particularly for many older adults. The decision to discharge a patient to a care facility rather than to home following critical illness may be influenced by multiple factors unrelated to the health of the patient, including patient finances and health care coverage, the availability and sophistication of potential caregivers, the organizational characteristics of the health care system, and the preferences of the patient. Still, patient-related health factors are likely a key determinant in this outcome, given that many survivors of critical illness remain highly dependent on supportive care or have active medical problems requiring complex treatments at the time of hospital discharge.
Although previous studies [1–3] have examined the determinants of functional decline and institutionalization in the general population of hospitalized patients, the patient factors associated with hospital discharge of critically ill patients to a care facility rather than to home have not been clearly defined. Previous studies of post-ICU outcomes have typically focused either on subsets of patients [4–9], or on predicting certain discrete outcomes, such as the need for prolonged mechanical ventilation [10,11]. In addition, some studies utilized variables which are not routinely collected by clinicians, such as the Charlson comorbidity score [8,12,13], making it more difficult to translate the results of such studies to the clinical arena.
A better understanding of readily identifiable patient health factors related to discharge to a care facility is needed to guide future research in this underdeveloped area. Information regarding the magnitude of risk associated with common clinical conditions and treatments would be valuable in focusing future prospective efforts to predict and to improve long-term outcomes after critical illness. Such information is sorely needed by clinicians providing care to ICU patients and counsel to their families and surrogate decision-makers. To address this need, we conducted a retrospective cohort study in a population of critically ill medical patients who survived to hospital discharge. We performed a multivariable analysis of readily identifiable patient factors hypothesized to be associated with discharge to a care facility instead of to home, and estimated the magnitude of risk associated with each factor. We further hypothesized that the discrimination of the model would be robust to changes in ICU length of stay.
METHODS
The study was performed in a single medical ICU located within a large teaching hospital in Chicago, Illinois, USA. This hospital serves as both a tertiary care center and as a source of primary care for the surrounding community. The hospital’s medical ICU has long been a “closed” unit staffed by a team of residents and one or two fellows in pulmonary and critical care who rotate monthly, and a full-time intensivist who rotates every two weeks.
The study population was derived from an existing clinical research database comprised of patients enrolled in previous studies of critically ill patients. This database includes all patients admitted to this medical ICU during the following periods: July 1997 to February 1998 (604 consecutive admissions), November/December 2001 (125 consecutive admissions), and March/April 2002 (145 consecutive admissions). Patients were excluded from this study if they died during the index hospitalization, were residing in a care facility 2 weeks prior to the index hospital admission, or were hospitalized for longer than 6 months. To ensure independence of observations, only the first admission for each patient was analyzed. This research was conducted in accordance with the ethical standards set forth in the Helsinki Declaration of 1975. Additionally, this study was approved by the Institutional Review Board at the University of Chicago hospitals and met all requirements for waiver of consent.
Data collection
Data were collected by querying the existing electronic database and by reviewing medical records. Because factors that are identifiable early in the course of intensive care are potentially more valuable clinically, we restricted our analysis to the first 72 hours of intensive care. All exposure variables listed subsequently were hypothesized a priori to be associated with the primary outcome of discharge to CF instead of to home. Age, gender, race, and body mass index (BMI) at the time of ICU admission were recorded. BMI was stratified according to National Institutes of Health clinical guidelines [14]. Obesity class II (35 kg/m2 ≤ BMI < 40 kg/m2) and extreme obesity (BMI ≥ 40 kg/m2) were collapsed into a single category, as has been done previously [15].
The presence or absence of a number of chronic medical conditions was recorded. These included: previous diagnosis of a neurodegenerative disorder (dementia [any etiology], Parkinson’s disease, or similar functionally limiting disorder); chronic renal failure requiring dialysis; diabetes mellitus for at least five years; advanced (stage IV) solid organ malignancy; cirrhosis complicated by ascites or encephalopathy; congestive heart failure (CHF) class III or IV by New York Heart Association (NYHA) criteria [16]; and severe chronic pulmonary disease (obstructive lung disease with an FEV1 < 30%; restrictive lung disease with a TLC < 50%; or any chronic pulmonary disease associated with dyspnea most days of the week, the use of home oxygen, or chronic ventilatory support).
We also recorded a number of acute illness variables. Acute Physiology and Chronic Health Evaluation (APACHE) II scores were calculated [17]. Each subject’s index hospitalization was examined through the first 72 hours of intensive care for the occurrence of the following phenomena: acute renal failure requiring dialysis; the use of invasive mechanical ventilation; the isolation of resistant organisms; the presence of severe cognitive dysfunction; and the presence of poor strength and/or mobility. Definitions of the latter three variables are provided below.
All clinically obtained cultures were queried for the presence of the following resistant organisms: methicillin-resistant Staphylococcus aureus, Vancomycin-resistant enterococcus faecalis or faecium, Escherichia coli or Klebsiella pneumoniae resistant to ceftazidime or ceftriaxone, Enterobacter cloacae, Proteus mirabilis, Serratia marcescens, Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia. No attempt was made to distinguish between colonization and infection.
Criteria were established a priori for the presence of severe cognitive dysfunction and for poor strength/mobility using a combination of previously published adverse prognostic criteria and clinically relevant variables with face validity for predicting discharge to a care facility. Severe cognitive dysfunction was considered to be present if the patient exhibited any of the following: (1) severe coma, with either (a) Glasgow Coma Scale < 5 on ICU admission & again 72 hrs later off sedation [18]; or (b) coma on the 3rd day of ICU with abnormal brain stem reflexes or absent motor response to voice or pain [19]; (2) use of intracranial pressure monitoring; or (3) chest compressions during the current hospitalization of at least 5 minutes’ duration and/or associated with absent pupillary responses or motor response to pain 72 hrs after the event (off sedation) [20]. Poor strength/mobility was considered to be present if the patient exhibited any of the following: (1) inability to raise legs against gravity on ICU admission; (2) recent (< 30 days) hip fracture; or (3) stage III or IV decubitus ulcers.
The primary outcome measure was discharge to CF (versus the patient’s or a caregiver’s home). Enrollment in home hospice was considered equivalent to discharge to a care facility for the purpose of this study. Care facilities included the following categories: acute care facility, long-term acute care hospital, hospice (home or inpatient), and other skilled nursing facility (nursing home without rehabilitation, nursing home with subacute rehabilitation, and acute rehabilitation).
Statistical analysis
Analyses were performed using SAS 9.1 (SAS Institute Incorporated, Cary, NC). Bivariate analyses were used to evaluate the association of chronic and acute illness variables with discharge to a care facility versus to home at hospital discharge. Comparisons were performed using a two-sample t-test, two-sample Mood’s median test, chi-square test, or Fisher exact test, as appropriate. We then developed a multivariable logistic regression model to identify independent patient factors associated with discharge to a care facility (dependent variable), and to estimate the magnitude of risk associated with each factor. Age (≥ 65 years versus < 65 years [reference]), race, gender, BMI, and all collected chronic and acute illness variables were included in the model. Period of admission was included in the model (1997/1998 [reference] versus 2001 versus 2002) to adjust for the potential for secular trends in discharges to care facilities between 1997 and 2002. ICU length of stay was not included in the model because this information is not routinely available to the clinician within 72 hours after the onset of intensive care. To test the hypothesis that the inclusion of ICU length of stay in the model would not appreciably alter the model’s discrimination nor modify the risk factors for discharge to a care facility identified by the model, we repeated the multivariable analysis with the addition of ICU length of stay as a variable. Model discrimination was assessed by calculating the area under the receiver operating characteristic curve (AUC) and model fit was assessed using the Hosmer-Lemeshow Goodness-of-fit test statistic. A two-tailed p-value <0.05 was used to define statistically significant differences.
RESULTS
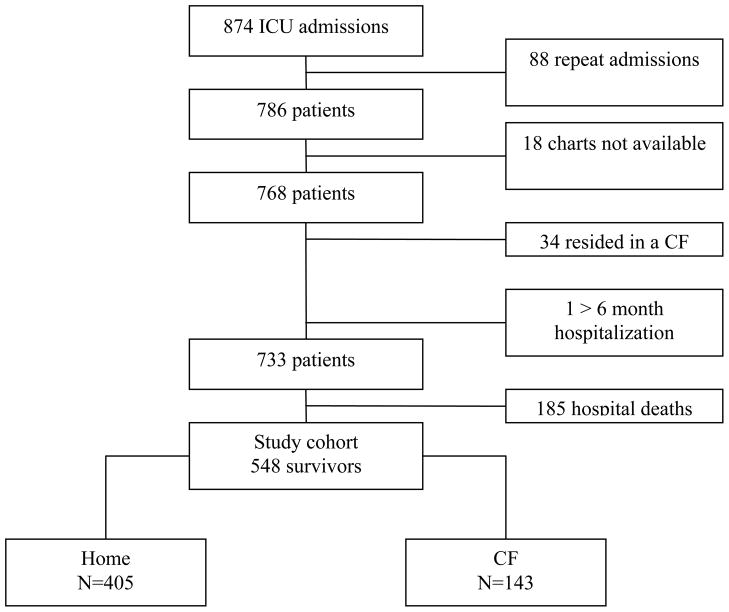
There were 548 survivors (69.7% of all patients admitted to the medical ICU during the study periods) available for analysis (Figure 1). Approximately one quarter of these patients (143/548, 26.1%) were discharged to a care facility instead of to home. Characteristics of the study cohort are shown in Table 1. Patients discharged to a care facility were generally sicker, as indicated by higher APACHE II scores and longer ICU and hospital length of stay (Table 1). They were also more likely to be mechanically ventilated, have severe cognitive dysfunction or poor strength and/or mobility, undergo tracheostomy, or be infected with resistant organisms. In the entire cohort, forty-four resistant organisms were identified in 40 patients. Methicillin-resistant Staphylococcus aureus (20 patients) and Pseudomonas aeruginosa (9 patients) were isolated most commonly, with all other organisms isolated in three or fewer patients.
Figure 1. Derivation of the Study Cohort.
ICU = intensive care unit. CF = care facility.
Table 1. Patient Characteristics.
Data reported as mean ± standard deviation or number (percent) unless otherwise indicated.
| Characteristic | All (n=548) | Home (n=405) | Care Facility (n=143) | p value |
|---|---|---|---|---|
| Age (yrs) | 53.4±18.8 | 50.2±18.4 | 60.2±16.8 | <.001 |
| Pts ≥ 65 years old | 176 (32.1%) | 109 (26.9%) | 67 (46.9%) | <.001 |
| Gender, female | 299 (54.6%) | 213 (52.6%) | 86 (60.1%) | .12 |
| Race* | .33 | |||
| African-American | 388 (72.8%) | 290 (73.8%) | 98 (70.0%) | - |
| Caucasian | 128 (24.0%) | 93 (23.7%) | 35 (25.0%) | - |
| Other | 17 (3.2%) | 10 (2.5%) | 7 (5.0%) | - |
| BMI†,‡ (kg/m2) | 25.6 (21.7, 31.0) | 25.7 (21.7, 31.0) | 25.5 (21.6, 30.9) | 0.64 |
| All categories | 0.45 | |||
| <18.5 | 34 (6.4%) | 21 (5.3%) | 13 (9.3%) | - |
| 18.5 to <25 | 207 (38.8%) | 158 (40.1%) | 49 (35.0%) | - |
| 25 to <30 | 140 (26.2%) | 102 (25.9%) | 38 (27.1%) | - |
| 0 to <35 | 70 (13.1%) | 50 (12.7%) | 20 (14.3% | - |
| ≥35 | 83 (15.5%) | 63 (16.0%) | 20 (14.3%) | - |
| Admission period | 0.16 | |||
| Admitted 7/97 to 2/98 | 370 (67.5%) | 282 (69.6%) | 88 (61.5%) | - |
| Admitted 11/01 to 12/01 | 74 (13.5%) | 49 (12.1%) | 25 (17.5%) | - |
| Admitted 3/02 to 4/02 | 104 (19.0%) | 74 (18.3%) | 30 (21.0%) | - |
| Hospital LOS†,§ (days) | 7.4 (4.0, 14.7) | 5.8 (3.8,10.8) | 15.0 (8.4, 23.0) | <.001 |
| ICU LOS†,§ (days) | 1.9 (1.1, 3.5) | 1.7 (1.0, 2.7) | 3.8 (1.9, 11.0) | <.001 |
| APACHE II score¶ | 15.8±7.0 | 14.5±6.3 | 19.7±7.4 | <.001 |
| Acute conditions# | ||||
| Mechanical ventilation | 143 (26.1%) | 69 (17.0%) | 74 (51.8%) | <.001 |
| ARF requiring dialysis | 12 (2.2%) | 6 (1.5%) | 6 (4.2%) | .09 |
| Tracheostomy | 5 (0.9%) | 1 (0.3%) | 4 (2.8%) | .02 |
| Serious cognitive dysfunction | 10 (1.8%) | 2 (0.5%) | 8 (5.6%) | <.001 |
| Poor strength/mobility | 15 (2.7%) | 2 (0.5%) | 13 (9.1%) | <.001 |
| Resistant organisms | 40 (7.3%) | 23 (5.7%) | 17 (11.9%) | .01 |
| Chronic conditions** | ||||
| Neurodegenerative disorder | 18 (3.3%) | 10 (2.5%) | 8 (5.6%) | .10 |
| Dialysis dependence | 65 (11.9%) | 51 (12.6%) | 14 (9.8%) | .37 |
| Diabetes mellitus > 5 years | 66 (12.0%) | 47 (11.6%) | 19 (13.3%) | .60 |
| Stage IV cancer | 33 (6.0%) | 24 (5.9%) | 9 (6.3%) | .87 |
| Advanced liver disease | 26 (4.7%) | 21 (5.2%) | 5 (3.5%) | .41 |
| CHF NYHA class III or IV | 20 (3.7%) | 14 (3.5%) | 6 (4.2%) | .69 |
| Advanced lung disease | 47 (8.6%) | 32 (7.9%) | 15 (10.5%) | .34 |
Data available for 533 of 548 patients.
Reported as median (interquartile range).
Body mass index (data available for 534 of 548 patients).
Length of stay.
Acute Physiology and Chronic Health Evaluation II score.
During the current hospitalization up to and including the first 72 hours of intensive care.
Present prior to the current hospitalization.
Discharge plans are shown in Table 2. Approximately 20.4% of patients younger than 65 years of age were discharged to a care facility, compared with 38.1% of patients older than 65 years of age (p <.001).
Table 2. Discharge Plans.
Data reported as number (percent)
| Care plan/destination | All (n=548) | < 65 years (n=372) | ≥ 65 years (n=176) |
|---|---|---|---|
| Home | 405 (74%) | 296 (80%) | 109 (62%) |
| Another acute care facility | 21 (4%) | 14 (4%) | 7 (4%) |
| Long term care hospital | 26 (5%) | 20 (5%) | 6 (3%) |
| Other skilled nursing facility* | 87 (16%) | 37 (10%) | 50 (28%) |
| Hospice | 9 (2%) | 5 (1%) | 4 (2%) |
Skilled nursing facilities other than a long term care hospital or hospice
Results of multivariable analysis are reported in Table 3. Older age (≥ 65 years versus < 65 years) was modestly associated with an increased risk of discharge to a care facility after adjustment for severity of illness and comorbidities. Other risk factors were use of mechanical ventilation, severe cognitive dysfunction, and poor strength/mobility; these factors were associated with a substantially increased risk of discharge to a care facility. The model had good discrimination (AUC 0.82; 95% CI 0.77–0.86) and calibration (p=0.59, Hosmer Lemeshow Goodness-of-Fit test). Similar results were obtained when ICU length of stay was included in the model. For instance, older age (≥ 65 years versus < 65 years) conferred a similar risk of discharge to a care facility whether the model included ICU length of stay (OR 2.0; 95% CI 1.2–3.5) or did not include ICU length of stay (OR 1.8; 95% CI 1.1–3.1).
Table 3. Independent Risk Factors for Discharge to a Care Facility.
Results of multivariable logistic regression model.
| Variable | Odds Ratio (95% CI*) | p value |
|---|---|---|
| Age ≥ 65 years (versus age < 65 years) | 1.8 (1.1–3.1) | 0.02 |
| APACHE II (10 point change) | 3.0 (2.0–4.6) | <0.001 |
| Chronic renal failure requiring dialysis | 0.4 (0.2–0.9) | 0.03 |
| Mechanical ventilation† | 3.4 (2.0–5.8) | <0.001 |
| Severe cognitive dysfunction† | 8.1 (1.3–50.6) | 0.02 |
| Poor strength/mobility† | 31.7 (6.4–157.3) | <0.001 |
Confidence interval.
During the current hospitalization up to and including the first 72 hours of intensive care
The multivariable logistic regression model included the following variables (but which were not significantly associated with the outcome): gender, race, neurodegenerative disorder, diabetes mellitus for greater than 5 years, Stage IV cancer, liver disease, Class III or IV CHF, advanced lung disease, acute renal failure requiring dialysis, tracheostomy, infection with resistant organisms, admission period. 519 of 548 observations used.
DISCUSSION
In a multivariable model incorporating clinical information routinely documented during the first 72 hours of intensive care, we identified older age, mechanical ventilation, severe cognitive dysfunction, and poor strength/mobility as patient factors that are strongly and independently associated with discharge to a care facility following critical illness. This study provides new information regarding the magnitude of the risk for discharge to a care facility associated with these factors, and shows that significant differences are present early in the course of critical illness between those patients ultimately discharged to a care facility and those patients who are discharged to home. This conclusion is bolstered by the finding that the inclusion of ICU length of stay in the model did not appreciably alter our results.
While the findings of our study are not altogether surprising—for example, many conditions leading to severe cognitive dysfunction or poor strength/mobility are not likely to improve sufficiently in the short-term to permit a patient to return home—the magnitude of the risk associated with these factors and with the receipt of mechanical ventilation suggests a research agenda for future study. The model showed good discrimination even though it did not include baseline level of function or social variables associated with long-term care, and even though the retrospective nature of the study permitted only the identification of particularly severe forms of cognitive or neuromuscular disorders. This is likely due to the strong association between certain diseases and therapies and post-ICU outcomes, and highlights these risk factors as deserving of further study. The reasons for the strong association between mechanical ventilation and discharge to care facility—a greater than threefold risk that the patient who survives critical illness will not go home immediately upon hospital discharge, even after adjustment for age and severity of illness—are not provided by our study. A mechanically ventilated patient may be subsequently discharged to a care facility for many reasons, including but not limited to ventilator dependence, cognitive impairment, and skeletal muscle dysfunction and deconditioning due to inflammation and prolonged inactivity [21]. While our study was not designed to explore this relationship further, early mobilization may attenuate this risk [22].
We were interested to discover that dialysis dependence prior to ICU admission actually decreased the risk of transfer to a care facility rather than to home in our model. There are several potential explanations for this finding. (1) Certain care facilities do not accept patients who are dependent on both dialysis and mechanical ventilation. (2) Patients receiving dialysis may have differed from other patients in our study according to payor source, leading to different post-hospitalization care plans. (3) Patients who are dialysis dependant and living at home prior to hospitalization may have a more robust social support structure in place at the time of ICU admission than patients not receiving chronic dialysis, enhancing the ability of the patient to return immediately home upon hospital discharge. (4) Finally, patients receiving dialysis may have been more likely to present with certain rapidly treatable problems, such as pulmonary edema due to missed or inadequate dialysis.
Increased attention has been paid recently to outcomes such as symptom burden [23], functional status [24,25], health-related quality of life [26–28], and other post-ICU patient-centered outcomes [29]. We argue that the need to be transferred to a care facility at hospital discharge rather than to home is an understudied patient-centered outcome. Rady et al [6], using the same primary outcome measure, reported the risk factors for hospital discharge to a care facility in a cohort of octogenarians requiring intensive care. In their study, approximately 21% of all patients (younger and older) were discharged to other care facilities, a rate that is similar to ours (26%). Interestingly, the authors determined through multivariate analysis of hospital survivors that discharge to other care facilities (versus to home) was associated with older age, severity of illness, mechanical ventilation for at least 96 hours, and various admission diagnoses (including neurologic and musculoskeletal disorders), among other factors, findings that are similar to those of our study. Similarly, Feng et al [13], using electronic administrative records, reported the negative association between both increasing age and duration of mechanical ventilation and the likelihood that the patient will return home upon hospital discharge.
However, there are important differences between our study and the work of other investigators. First, because of our hospital’s location on the south side of Chicago, it is likely that our study population includes more underserved patients than the population studied by Rady et al [6]. Second, while Rady et al [6] only studied octogenarians, there was no age criterion for entry into our study. Third, while the analysis of Feng et al. was based upon electronic administrative records, our study analyzed patient factors that are recognized by clinicians and readily obtainable from the patient’s medical record. Fourth, while the analysis of Feng et al included all ICU patients, we elected to focus on survivors of critical illness. Finally, in contrast to the aforementioned studies [6,13], we elected to use only those data available to the clinician in the first seventy-two hours of intensive care. This approach was selected a priori in order to determine if, early in the course of critical illness, there were detectable differences in routinely reported clinical variables or treatments between patients ultimately discharged to home and patients discharged to a care facility. The results of our study suggest that this is so, a finding that has important implications for the design of future studies. Of course, because we exclude non-survivors, the results of our study should not be used by clinicians for clinical decision-making about the utility of continuing life-sustaining treatments.
A substantial portion of ICU services are delivered to patients older than 65 years of age [30,31]. Unfortunately, our study was not powered sufficiently to perform detailed analyses of this subgroup (data not shown). Our study did demonstrate that patients discharged to a care facility were generally older than those discharged to home, and that patients ≥ 65 years of age have nearly twice the odds as patients < 65 years of age to be discharged to a care facility, even after controlling for severity of illness and other acute and chronic conditions. Still, nearly two-thirds of patients 65 years of age or older were able to be discharged home. Thus, our study suggests that age alone is not a clinically useful predictor of this outcome, similar to its lack of utility in predicting mortality from critical illness once severity of illness and comorbidities that tend to accrue with age are taken into account [32]. Our model did not include baseline level of function, which has been shown to be associated with mortality [33,34], institutionalization [2,3,34,35], and functional decline [2,35] in older hospitalized adults; with functional outcome in seriously ill hospitalized adults (both older and younger patients) [1]; and, in more limited studies of older critically ill patients, with increased short- [36] and long-term [37] mortality. These unmeasured factors may help explain why our multivariable model had good (AUC 0.82), but not excellent (AUC typically >0.9) [38,39] ability to discriminate between patients who are discharged to a care facility and patients who are discharged to home.
Implications
To our knowledge, our study is the first to demonstrate that significant differences are present early in the course of critical illness between those patients ultimately discharged to a care facility and those patients who are discharged to home. Our findings should encourage efforts to validate these results in a more contemporary cohort, to understand the mechanisms that contribute to the observed associations, and to develop and test interventions that reduce the need for discharge to locations other than home. While our model performed well utilizing only routinely available clinical information obtained from patients’ charts, future research should investigate whether incorporating certain additional variables would improve the model’s performance. These variables include the patient’s prehospital level of function, payor source, the availability of potential caregivers, the development of delirium or predisposing factors for its development [40], and clinical events and treatments that occur after the first 72 hours of intensive care.
Limitations
Our study has several limitations. (1) The decision to restrict the analysis to the first 72 hours of intensive care excluded potentially valuable clinical data that may have refined the model and increased its accuracy. An alternative approach would have been to analyze the patient’s entire hospitalization, and perform a separate analysis of the first 72 hours of intensive care in order to determine the relative influence of “early” versus “late” events on discharge destination. (2) Our analysis found no evidence of secular trends in discharge of critically ill patients from our hospital to other care facilities. Still, our model may be sensitive to changes in clinical practice or in health care delivery that have occurred in the years following our patients’ treatment. Our findings should be replicated in a more contemporaneous cohort to ensure that they are robust to these changes. (3) Because this study was performed in a single university-affiliated medical ICU, the results may not apply to other patient populations or other local health care systems. (4) The retrospective design limited our analysis to those data contained within the electronic database or the medical record, preventing us from including baseline level of function or the availability of potential caregivers in the analysis. It also prevented us from detecting less obvious forms of cognitive dysfunction or poor strength/mobility and from classifying plans for post-hospitalization care into precise categories. (5) Finally, care should be taken not to equate the study’s primary outcome measure—discharge to a care facility—with care dependency or level of function. As mentioned previously, the decision to transfer a patient to a care facility takes many factors into account besides functional status including the need to administer complex medical therapies, the availability of caregivers, financial considerations (including payer source), and patient preferences, among others.
Conclusions
We identified patient factors associated with an increased risk of hospital discharge to a care facility in a cohort of survivors of critical illness treated in a medical ICU, using only that clinical information routinely documented in the medical record during the first 72 hours of intensive care. In analyses adjusting for severity of illness, we identified older age, mechanical ventilation, and conditions with severe cognitive and neuromuscular sequelae as patient factors that are strongly associated with discharge to a care facility following critical illness. These results should help in the planning of studies in more contemporary cohorts.
SUMMARY OF KEY POINTS.
Why do some survivors of critical illness return home on hospital discharge, while others are discharged to another care facility? This issue has not been well studied, despite the importance of this outcome to patients and their families. In this issue, Gehlbach et al. report that certain patient health factors are strongly associated with patient discharge to a care facility following critical illness. In a retrospective cohort study of survivors of critical illness, the following observations were made:
Patients who received mechanical ventilation had a greater than three-fold odds ratio for discharge to a care facility.
Patients with hospitalizations characterized by severe cognitive dysfunction or poor strength and/or mobility had significantly increased odds of being discharged to a care facility.
Discharge to a care facility occurred more commonly in older patients, even after adjustment for severity of illness and comorbidities.
Acknowledgments
Sponsor’s Role
The CHEST Foundation of the American College of Chest Physicians—ASP Geriatric Development Initiative (GDI) Award (Supported by: Atlantic Philanthropies, the John A. Hartford Foundation, the CHEST Foundation of the American College of Chest Physicians, and the Association of Subspecialty Professors) provided support for the overall project. Dr. Gehlbach also receives support from grant number K23HL088020 from the National Heart, Lung, and Blood Institute. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The sponsors had no role in subject recruitment, data collection or analysis, or the preparation of the paper.
Footnotes
All work was performed at the University of Chicago.
Author contributions
Brian Gehlbach was involved in the conception and design of the study; the acquisition, analysis, and interpretation of data; the drafting and revision of the article; and the final approval of the manuscript. Victor Salamanca was involved in the acquisition, analysis, and interpretation of data; the revision of the article; and the final approval of the manuscript. Joseph Levitt was involved in the acquisition, analysis, and interpretation of data; the revision of the article; and the final approval of the manuscript. Greg A. Sachs was involved in the conception and design of the study; the analysis and interpretation of data; the revision of the article; and the final approval of the manuscript. Mary Kate Sweeney was involved in the acquisition of data, the revision of the article, and the final approval of the manuscript. Anne Pohlman was involved in the acquisition, analysis, and interpretation of data; the revision of the article; and the final approval of the manuscript. Jeff Charbeneau was involved in the analysis and interpretation of data, the revision of the article, and the final approval of the manuscript. Jerry Krishnan was involved in the analysis and interpretation of data, the revision of the article, and the final approval of the manuscript. Jesse Hall was involved in the conception and design of the study, the analysis and interpretation of data, the revision of the article, and the final approval of the manuscript.
References
- 1.Wu AW, Damiano AM, Lynn J, et al. Predicting future functional status for seriously ill hospitalized adults: the SUPPORT prognostic model. Ann Intern Med. 1995;122:342–350. doi: 10.7326/0003-4819-122-5-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 2.Gill TM, Williams CS, Tinetti ME. The combined effects of baseline vulnerability and acute hospital events on the development of functional dependence among community-living older persons. J Gerontol A Biol Sci Med Sci. 1999;54:M377–M383. doi: 10.1093/gerona/54.7.m377. [DOI] [PubMed] [Google Scholar]
- 3.Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol A Biol Sci Med Sci. 1996;51:M189–M194. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- 4.Chelluri L, Pinsky MR, Donahoe MP, Grenvik A. Long-term outcome of critically ill elderly patients requiring intensive care. JAMA. 1993;269:3119–3123. [PubMed] [Google Scholar]
- 5.Nierman DM, Schechter CB, Cannon LM, Meier DE. Outcome prediction model for very elderly critically ill patients. Crit Care Med. 2001;29:1853–1859. doi: 10.1097/00003246-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Rady MY, Johnson DJ. Hospital discharge to care facility. A patient-centered outcome for the evaluation of intensive care for octogenarians. Chest. 2004;126:1583–1591. doi: 10.1378/chest.126.5.1583. [DOI] [PubMed] [Google Scholar]
- 7.Kurek CJ, Dewar D, Lambrinos J, Booth FV, Cohen IL. Clinical and economic outcome of mechanically ventilated patients in New York State during 1993: analysis of 10,473 cases under DRG 475. Chest. 1998;114:214–222. doi: 10.1378/chest.114.1.214. [DOI] [PubMed] [Google Scholar]
- 8.Quality of Life After Mechanical Ventilation in the Aged Study Investigators. 2-Month mortality and functional status of critically ill adult patients receiving prolonged mechanical ventilation. Chest. 2002;121:549–558. doi: 10.1378/chest.121.2.549. [DOI] [PubMed] [Google Scholar]
- 9.Friedrich JO, Wilson G, Chant C. Long-term outcomes and clinical predictors of hospital mortality in very long stay intensive care unit patients: a cohort study. Crit Care. 2006;10:R59. doi: 10.1186/cc4888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Troche G, Moine P. Is the duration of mechanical ventilation predictable? Chest. 1997;112:745–751. doi: 10.1378/chest.112.3.745. [DOI] [PubMed] [Google Scholar]
- 11.Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 199;27:1714–1720. doi: 10.1097/00003246-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Feng Y, Amoateng-Adjepong Y, Kaufman D, Gheorghe C, Manthous CA. Age, duration of mechanical ventilation, and outcomes of patients who are critically ill. Chest. 2009;136:759–764. doi: 10.1378/chest.09-0515. [DOI] [PubMed] [Google Scholar]
- 14.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. National Institute of Health; 1998. [PubMed] [Google Scholar]
- 15.Peake SL, Moran JL, Ghelani DR, Lloyd AJ, Walker MJ. The effect of obesity on 12-month survival following admission to intensive care: a prospective study. Crit Care Med. 2006;34:2929–2939. doi: 10.1097/01.CCM.0000248726.75699.B1. [DOI] [PubMed] [Google Scholar]
- 16.The Criteria Committee of the New York Heart Association. Functional Capacity and Objective Assessment. In: Dolgin M, editor. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9. Little, Brown and Company; Boston, MA: 1994. pp. 253–255. [Google Scholar]
- 17.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 18.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 19.Hamel MB, Goldman L, Teno J, et al. Identification of comatose patients at high risk for death or severe disability. JAMA. 1995;273:1842–1848. [PubMed] [Google Scholar]
- 20.Zandbergen EG, de Haan RJ, Stoutenbeek CP, Koelman JH, Hijdra A. Systematic review of early prediction of poor outcome in anoxic-ischaemic coma. Lancet. 1998;352:1808–1812. doi: 10.1016/S0140-6736(98)04076-8. [DOI] [PubMed] [Google Scholar]
- 21.Winkelman C. Inactivity and inflammation in the critically ill patient. Crit Care Clin. 2007;23:21–34. doi: 10.1016/j.ccc.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones C, Griffiths RD, Humphris G, Skirrow PM. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med. 2001;29:573–580. doi: 10.1097/00003246-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Jackson JC, Hart RP, Gordon SM, et al. Six-month neuropsychological outcome of medical intensive care unit patients. Crit Care Med. 2003;31:1226–1234. doi: 10.1097/01.CCM.0000059996.30263.94. [DOI] [PubMed] [Google Scholar]
- 25.Roche VML, Kramer A, Hester E, Welsh CH. Long-term functional outcome after intensive care. J Am Geriatr Soc. 1999;47:18–24. doi: 10.1111/j.1532-5415.1999.tb01896.x. [DOI] [PubMed] [Google Scholar]
- 26.Vazquez Mata G, Rivera Fernandez R, Gonzalez Carmona A, et al. Factors related to quality of life 12 months after discharge from an intensive care unit. Crit Care Med. 1992;20:1257–1262. doi: 10.1097/00003246-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
- 28.Davidson TA, Caldwell ES, Curtis JR, Hudson LD, Steinberg KP. Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. JAMA. 1999;281:354–360. doi: 10.1001/jama.281.4.354. [DOI] [PubMed] [Google Scholar]
- 29.Daly BJ, Douglas SL, Gordon NH, et al. Composite outcomes of chronically critically ill patients 4 months after hospital discharge. Am J Crit Care. 2009;18:456–465. doi: 10.4037/ajcc2009580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognosis system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–36. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 31.El Solh AA, Ramadan FH. Overview of respiratory failure in older adults. J Intensive Care Med. 2006;21:345–351. doi: 10.1177/0885066606292873. [DOI] [PubMed] [Google Scholar]
- 32.Carson SS, Bach PB. The epidemiology and costs of chronic critical illness. Crit Care Clin. 2002;18:461–476. doi: 10.1016/s0749-0704(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 33.Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 34.Miller EA, Weissert WG. Predicting elderly people’s risk for nursing home placement, hospitalization, functional impairment, and mortality: a synthesis. Med Care Res Rev. 2000;57:259–297. doi: 10.1177/107755870005700301. [DOI] [PubMed] [Google Scholar]
- 35.McCusker J, Kakuma R, Abrahamowicz M. Predictors of functional decline in hospitalized elderly patients: a systematic review. J Gerontol. 2002;57:M569–M577. doi: 10.1093/gerona/57.9.m569. [DOI] [PubMed] [Google Scholar]
- 36.Mayer-Oakes SA, Oye RK, Leake B. Predictors of mortality in older patients following medical intensive care: the importance of functional status. JAGS. 1991;39:862–868. doi: 10.1111/j.1532-5415.1991.tb04452.x. [DOI] [PubMed] [Google Scholar]
- 37.Mattison ML, Rudolph JL, Kiely DK, Marcantonio ER. Nursing home patients in the intensive care unit: risk factors for mortality. Crit Care Med. 2006;34:2583–2587. doi: 10.1097/01.CCM.0000239112.49567.BD. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro DE. The interpretation of diagnostic tests. Stat Methods Med Res. 1999;8:113–134. doi: 10.1177/096228029900800203. [DOI] [PubMed] [Google Scholar]
- 39.Fischer JE, Bachmann LM, Jaeschke R. A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med. 2003;29:1043–1051. doi: 10.1007/s00134-003-1761-8. [DOI] [PubMed] [Google Scholar]
- 40.Pisani MA, Murphy TE, Van Ness PH, Araujo KLB, Inouye SK. Characteristics associated with delirium in older patients in a medical intensive care unit. Arch Intern Med. 2007;167:1629–1634. doi: 10.1001/archinte.167.15.1629. [DOI] [PubMed] [Google Scholar]