Abstract
Objective
To better understand preferred approaches that health care professionals could employ when caring for parents who are at risk for giving birth to an extremely premature infant.
Methods
Women who were at high risk of having a periviable birth were recruited from three tertiary care hospitals with Level 3 neonatal intensive care units. These women, as well as their partners, physicians, and nurses underwent structured interviews both before and after delivery. Interviews were analyzed for advice that was provided to health care professionals who could be involved in the future counseling of antenatal patients at high risk of periviable delivery.
Results
Forty women, 14 fathers, and 52 health care providers participated in the interview process. Two main themes were identified – namely, the fundamental importance of information provision and support. Nevertheless, although all participants agreed about the importance of these actions, several areas of discordance among participants were noted. Nearly one-third of parents emphasized the importance of “hope”; 60% and 45% recommended the provision of supplementary written and internet materials, respectively. In contrast, most health care providers expressed the importance of “objectivity,” and only 15% and 5% thought written or internet materials, respectively, were desirable, given the concern that supplementary information sources could be misleading.
Conclusion
Both patients and providers agree about the centrality of information provision and emotional support for women at risk for periviable delivery. This study not only elucidates preferred approaches and methods by which this information and support could be optimized, but also shows pitfalls that, if not avoided, may impair the relationship between provider and patient.
During the last several decades, neonatal care has made such substantive advances that newborns who were not able to survive now routinely do so.1–3 At present, there have been reports of neonatal survival at gestational ages as young as 22 weeks.4 Yet, even if survival is possible at such a young gestational age, it is by no means assured. Indeed, the gestational age period from 22–26 weeks, a period commonly considered “periviable”, is one during which uncertainty about survival, as well as morbidity-free survival, predominates.3–5
This uncertainty is particularly relevant when a parturient in the periviable period presents with signs and symptoms that indicate she is at high risk to deliver in the near future. In a very short time, she and her family will be confronted with an enormous volume of information concerning the range of possible treatments and outcomes that she and her child (or children, in the case of multiple gestations) could have. The discussion of these treatments and outcomes is of great importance for several reasons. First, this discussion can help a family prepare for, and begin to cope with, the possible adverse medical outcomes they may experience after delivery. Additionally, the discussion can assist a family in their choice of obstetric interventions for fetal indications and pediatric interventions with regard to life support.
The potential ramifications of the discussion and the related decision making that must occur in the periviable period only serve to emphasize how important it is that it be conducted in as optimal an environment as possible. Yet, there have been few evaluations of the actual discussions that occur and the circumstances that need to be present to enhance the value of these discussions. We hypothesized that qualitative investigation of the participants who engaged in actual periviable situations and decision making would help to better understand preferred approaches that health care professionals could employ when caring for expectant parents who are at risk for giving birth to an extremely premature infant.
Materials and Methods
Between April 2005 and September 2008, women who were at high risk of having a periviable birth were recruited from three tertiary care hospitals with Level 3 neonatal intensive care units (NICUs). Women who were potentially eligible for consent were identified by research staff at each institution by reviewing daily hospital admissions for antepartum care. Women were only approached for enrollment if they were at high risk of preterm delivery between 21 0/7 and 25 6/7 weeks due to an acute event (e.g. premature rupture of membranes), at least 18 years of age, English speaking, and had discussed obstetric and neonatal treatment decisions with a physician in relation to their acute obstetrical event. The partners of women who enrolled, as well as the care providers (physicians and nurses) who had spoken to them about treatment decisions, were contacted and asked to participate as well.
After consent, the subjects of the investigation (i.e. the woman, her partner, and her physician and nurse providers) underwent structured interviews both before and after delivery. In addition, relevant medical data (e.g. estimated gestational age, diagnosis at admission) were abstracted from the medical record. This study used the qualitative collective case study method described by Stake6. There were a total of four types of semi-structured interview guides to reflect discussions during different circumstances (antenatal, postnatal, stillbirth, end-of-life) with different wording for the parents and health care professionals. Interview guides were based on the Ottawa Decision Support Framework, and included: (a) demographic and clinical characteristics; (b) perceptions of health care conditions; (c) perceptions of roles of others in decision making; and (d) resources used to make the decisions (e.g. support, skills, and advice).7 For all versions of the interview guides, there were several questions related to the advice that the interviewee would like to provide to health care professionals in similar situations.
All interviews were digitally recorded and held in private. To avoid recall bias, an attempt was made to interview physicians and nurses as soon as possible after the parents’ antenatal interview. Physicians who participated in this study were identified by parents as the physician (attending obstetrician, maternal-fetal medicine attending physician or fellow, or neonatal attending physician or fellow) who had spoken to them about life support treatment decisions for the infant. Nurses in this study included obstetric and neonatal staff nurses and neonatal nurse practitioners (NNPs) who were identified by parents as those who clarified (staff RNs) or provided (NNPs) information. Interviews lasted approximately 30 to 45 minutes. Parents and physicians were subsequently contacted every week until 25 weeks of gestation or delivery of the infant to ask about their decisions regarding life support. Postnatal interviews were conducted regardless of infant outcome (i.e. survival or death) and were typically performed within a three weeks of the delivery. If the infant was born between 22 and 25 weeks of gestation, parents and infants were also followed for the first 28 days of the infant’s life or until two months of age if the infant was determined to be clinically unstable.
All interviews were transcribed verbatim, coded using a code book with 32 predetermined codes, and entered into the Atlas.ti software program (Berlin, Germany). This program is designed to store and retrieve coded data and is specifically useful for qualitative analysis. Codes were assigned by two members of the research team, who coded all of the transcripts independently and then met to compare coding and, in cases when coding was discordant, discuss the coding until agreement was reached. After a case summary of each participant’s interviews was prepared, matrices were developed for each type of interview (antenatal, postnatal and end-of-life) to be able to compare data within and across cases. Matrices displayed thematically coded data stratified by the originator (parents, physicians, nurses). For this analysis, which is concerned with the provision of antenatal advice, coded data from all interviews that were related to the provision of this advice were reviewed. Two investigators (KK and TM) independently reviewed all relevant coded data in an effort to identify and describe patterns. The final description of the categories related to the provision of advice was prepared after consensus was reached between the two research team members.
The data are derived from a study which is examining the decision making and the decision support needs of parents regarding life support decisions made over time for extremely premature infants. The present analysis focuses on the interviews that were conducted antenatally and the portions of these interviews that were coded to reflect the provision of advice to health care professionals who could be involved in the future counseling of antenatal patients at high risk of periviable delivery. Approval for this study was obtained by the Institutional Review Boards of Northwestern University, the University of Illinois at Chicago, and Rush University Medical Center.
Results
Of the 63 women who were approached, 50 agreed to participate. Forty of the 50 women were successfully enrolled, with the remainder becoming clinically unstable or giving birth before the initial interview could be conducted. In addition to enrolling these 40 women, antenatal interviews were also conducted with 14 fathers and 52 health care providers. Seventeen fathers did not meet eligibility criteria (they either were not involved in decision making, out of the country, or did not speak English) and nine could not be contacted or interviewed before delivery.
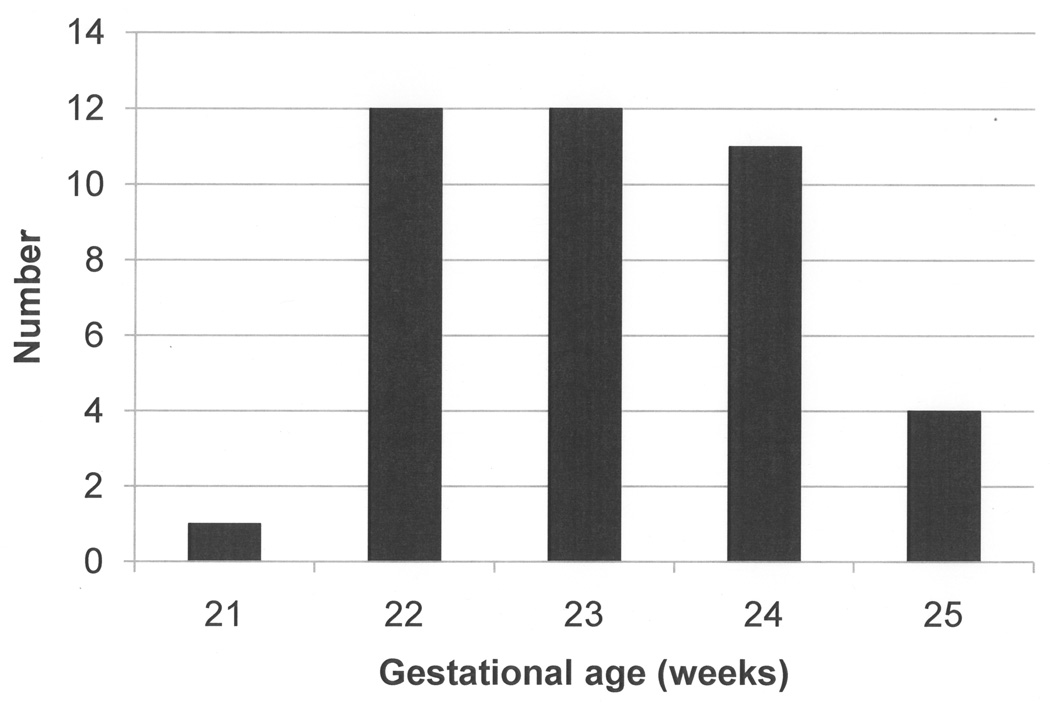
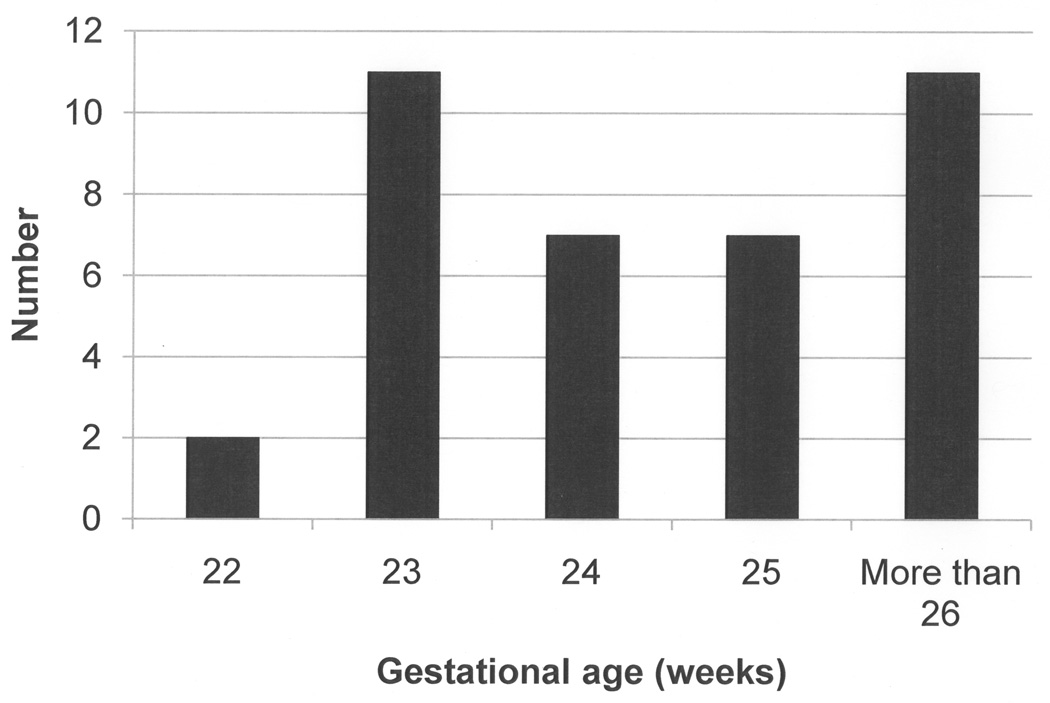
The gestational ages at which women were enrolled are presented in Figure 1. All women, with the exception of one with preeclampsia, were hospitalized for pathologies associated with spontaneous preterm birth (i.e. cervical insufficiency, preterm labor, premature rupture of membranes). Seven (17.5%) of the mothers were nulliparous, and fourteen of the 33 (42.4%) who were multiparous had a prior preterm delivery. Additional demographic characteristics of the parents as well as of the health care providers who participated in the antenatal interviews are summarized in Tables 1 and 2, respectively. The women in the study ultimately delivered 46 infants (including two sets of twins and two sets of triplets), the gestational ages of whom are presented in Figure 2. In two cases the gestational age at delivery could not be confirmed by medical record, as the women delivered at institutions other than the perinatal center at which they were enrolled. There were seven stillbirths, ten neonatal deaths, and one unknown outcome during the study period.
Figure 1.
Gestational age (weeks) at enrollment
Table 1.
Characteristics of the parental participants
| Characteristic | Mothers N = 40 |
Fathers N = 14 |
|---|---|---|
| Age (years) | 28.3 ± 6.5 | 31.0 ± 9.1 |
| Education (years) | 13.0 ± 4.0 | 12.3 ± 4.5 |
| Race | ||
| Black/ African American | 60% | 50% |
| Hispanic/Latino | 28% | 29% |
| White | 5% | 21% |
| Asian | 3% | 0% |
| Other | 5% | 0% |
| Marital Status | ||
| Married | 35% | 43% |
| Single, living with partner | 25% | 36% |
| Single | 33% | 21% |
| Other | 8% | 0% |
| Religion | ||
| Roman Catholic | 25% | 36% |
| Protestant | 63% | 29% |
| Other | 13% | 36% |
| Income ($) | ||
| < 30,000 | 40% | 21% |
| 30,000–50,000 | 20% | 21% |
| 50,001–70,000 | 10% | 21% |
| 70,000–90,000 | 5% | 0% |
| > 90,000 | 10% | 29% |
| Not reported | 15% | 7% |
All data presented as mean ± standard deviation or %
Table 2.
Characteristics of the physician and nurse participants
| Characteristic | Physicians N = 35 |
Nurses N = 17 |
|---|---|---|
| Age (years) | 40.2 ±9.2 | 40.3 ± 11.8 |
| Years in practice | 14.0 ± 9.5 | 15.6 ± 11.0 |
| Specialty | ||
| General obstetrics | 9% | NA |
| Maternal-fetal medicine | 54% | NA |
| Neonatology | 37% | NA |
| Registered nurse | NA | 94% |
| Neonatal nurse practitioner | NA | 6% |
| Race | ||
| Black/ African American | 11% | 18% |
| Hispanic or Latino | 6% | 0% |
| White | 43% | 71% |
| Asian | 37% | 6% |
| Other | 3% | 6% |
| Gender | ||
| Male | 40% | 0% |
| Female | 60% | 100% |
| Religion | ||
| Roman Catholic | 31% | 29% |
| Protestant | 23% | 41% |
| Jewish | 14% | 0% |
| Other | 33% | 18% |
All data presented as mean ± standard deviation or %
NA = Not applicable
Figure 2.
Gestational age (weeks) at delivery
During the interviews, all participants, when commenting on the advice they would provide to health care professionals, focused on two major themes – namely, the fundamental importance of information provision and support. With regard to information, the majority (70%) of the parents communicated the importance of providing clear information so that they could understand the situation and be better prepared to participate in decision making. Most of these parents also noted the importance of providing this information as quickly as possible. They stressed that this information was so important because of their general lack of knowledge about prematurity and its consequences. As one father, whose partner was hospitalized at 22 2/7 weeks, noted: “I am thinking that nothing really could happen (and that my baby) is going to be just a little bit smaller than the average baby.” Additionally, parents offered advice for the content, style, and format of the information. All indicated that they wanted information on the options for treatment for the mother and infant and the range of potential outcomes for the infant. Nearly one-third of the parents stressed the importance of honesty, but also the importance of hope. As one parent noted: “Share everything….not just all of the gloomy stuff because you can imagine how a mother would feel (when she is) 23 weeks and (her) bag of waters breaks.” Parents also suggested that their relative lack of preexisting knowledge could limit understanding unless information was given slowly, with a limit of jargon, and if at all possible, by repetition over multiple visits. Indeed, parents commented on the usefulness of supplemental resources, such as written materials, before they were asked about management decisions. One mother said, “You can go over what they’ve discussed once they’ve left.” As implied by this statement, parents voiced the conviction that this information would be used as a supplement, and not a substitute, for the information that the physician presented.
Health care providers also stressed the importance of providing clear information to families who are at acute risk for having an extremely premature infant, and similarly focused on the relevance of management options and outcome data. In contrast to patients, however, the health care professionals (physicians and nurses alike) stressed the importance, when providing information, of “objectivity” and the avoidance of offering “false hope.” Said one physician, “I am not the one who is taking care of (the baby) for the rest of (its) life so….it’s important for (me) to try to be objective.” The providers echoed the patients’ suggestions that repeated visits, particularly after a patient’s initial anxiety has subsided, were an important component of information transfer, and nurses agreed that supplemental sources of information (including written text, video, and internet) would be helpful. Physicians, however, were less sanguine with regard to whether supplemental sources of information would be of value. For example, 60% and 45% of parents recommended the provision of written and internet materials, respectively, but these materials were only recommended by 15% and 5% of physicians. Some physicians were concerned that the clinical condition could change so rapidly that these static resources could not be used effectively. Several providers warned against using resources such as the internet and television programs which could contain inaccurate information and could give “false hope”. Lastly, health care providers were uniform in their emphasis on the importance of collaboration among the many members of the entire care team (i.e. physicians, nurses, social workers), both so patients would receive consistent information and providers could be updated about changes in their collaborators’ management plans. One obstetrician noted: “I think one of the things that really helped me is continuous communication with the NICU because giving the same kind of information to the patient makes us stronger in how we counsel.” A nurse reflected on the unique and important position she could occupy: “(I can) repeat what I’ve heard other people say and to try to explain how the ob/gyn said it this way but the neonatologist said it this way, but they’re really kind of saying the same thing.”
The other theme that predominated during the interviews with regard to advice was the importance of providing “support” to families through a variety of means. Words that parents used to indicate the kind of behavior they desired included: “kind”, “soft”, “gentle”, “caring”, and “attentive”. Much of the advice centered on demonstrating compassion and empathy. Parents offered advice for nurses in particular, noting the value of sitting with the family in order to alleviate their anxiety. A few parents stressed the importance of getting to know the parent to “individualize care”, such that they would be understood as individuals. Said one parent: “treat people as people and not numbers”.
Physicians and nurses echoed many of these patient sentiments. Both types of providers stressed the importance of developing an empathetic relationship that demonstrates to the patients that providers understand their situation. According to one physician, “I am 100% sure that developing a relationship quickly with a patient is important…because they don’t want to hear anything from you if you don’t have that.” A majority of nurses (53%) additionally noted the importance of providing emotional support by having nurses present in silence with the parent and not pressuring parents to discuss difficult topics before they were ready. Although not discussed by other interviewees, a few nurses advised health care professionals that the provision of spiritual support was an important component in the care of parents confronted with a high probability of periviable delivery.
Discussion
In this study, we have investigated the advice that would be helpful to health care providers who are confronted with a patient at acutely high risk of periviable preterm birth. The two primary themes that predominated in the structured interviews related to the crucial importance of providing information and support to women and their partners. Moreover, there were multiple specific suggestions as to preferred approaches and methods by which this information and support could be optimized. Both patients and providers emphasized the importance of providing clear, consistent factually-based information about management and outcomes. Patient and providers, however, did differ with regard to several specific suggestions about information and support. Although patients desired factual information from their providers, they also wanted to ensure that only “gloomy” information was not conveyed and that other supplemental sources of information would be available. Health care providers, in contrast, repeatedly emphasized their desire not to provide “false hope” and their concern that some supplemental sources of information could be misleading.
This work builds on the work of others who have investigated preferred modes of communication with families who are involved in decision making in the periviable period. Partridge et al surveyed parents of surviving very low birth weight infants regarding discussions that had occurred in the antenatal period.8 These parents advocated that physicians incorporate additional information about neonatal issues other than death and disability (such as “pain and suffering”), and noted that there were relatively infrequent discussions of patients’ individual characteristics (e.g. financial circumstances or religious beliefs) that patients may want to incorporate into their decision making. A similar conclusion about the importance of psychosocial information was arrived at by Lamiani et al.9 Payot and colleagues noted how important it is for providers to avoid “detachment” or emotional distance from the patients, while others have emphasized the need for providers to convey information that contains as much useful factual content as possible and avoid contradicting one another about this content.10,11
The information that does exist, however, often has not been derived from the wide variety of participants involved in the periviable counseling experience, and similarly has not reflected actual ongoing care. The conclusions of Limiani et al, for example, were drawn from observations of simulated conversations, while others’ conclusions have been derived from individuals who were not actually experiencing an acute event.9,12,13 Partridge et al did ascertain opinions of actual patients, although the retrospective survey was only of those whose infants had survived, which may have introduced bias.8 Payot et al prospectively investigated decision making among thirteen couples and their providers, although these providers were limited to neonatologists.10 Miquel-Verges et al, in addition to focusing only on women with pregnancies complicated by a congenital anomaly, also limited their analysis to neonataologists only.14
Limitations of the study include the fact that it was conducted among individuals in a single urban center, who may not have beliefs or opinions that are representative of those throughout the country. Also, the study patient population, although diverse, was composed of 40 women and 14 partners, and we cannot be certain that additional information would not be gained from additional interviews. The strengths of the present study include that the information was based on the cases of 40 women in the antenatal period, who were acutely confronted with the need to make decisions regarding a potential periviable preterm birth. Suggested advice was obtained from women, their partners, and their multiple different health care providers, allowing a wider exploration of suggestions and conflicts that could arise between professionally as well as between professionals and patients. Recall bias was limited by obtaining the information as the medical events were actually evolving, and performing the interviews as soon as possible after counseling.
Indeed, the information obtained illustrates potential points of concordance and discordance between providers and patients. Although both providers and patients agreed about the importance of information and support, their specific suggestions were less uniform. Providers voiced the need to provide information but typically emphasized that objectivity was ideal, whereas patients, despite desiring clear information, also consistently noted that they wanted to feel that individual circumstances were taken into account. Disparity was also noted regarding the concept of hope. Whereas providers were specifically cautious about providing hope, perceiving it as conflicting with objective information, most patients perceived no such conflict. And, despite all participants noting the importance of repeated information, physicians in particular were concerned that supplemental information (e.g. written documents or internet sites), which patients in fact desired, could be misleading and more hindrance than help.
When a woman presents and is at high risk of delivering an infant in the periviable period, communication is of the utmost importance given the gravity of the decisions that need to be made with regard to obstetric and neonatal care. The factual content of the discussion is complicated, and the acuteness of the situation as well as the multiple people who are involved adds further layers of complexity and greater probability that a communication breakdown will occur.15,16 The data from the present study provide insight for health care professionals into the approaches that can be used to enhance information transfer, and into pitfalls that, if not avoided, can lead to missed or misconstrued information and the fracture of the therapeutic bond.
Acknowledgement
The authors thank the research team members who participated in patient recruitment and coordination between clinical research centers: Co-investigators – Drs. Rama Bhat and Sarah Kilpatrick at the University of Illinois at Chicago Medical Center (UIMC); Drs. Rob Kimura, Michael Hussey, Howard Strassner at Rush University Medical Center (RUMC); research specialists – Ms. Maria Reyes (RUMC), Ms. Michelle Huntley and Ms. Lara Stein (Northwestern University), and Drs. Dennie Rogers and Ramkrishna Mehendale (UIMC). The authors also thank the parents who shared their stories, and the physicians and nurses who participated in the study.
Funded by a grant (NIH RO1 07904) from the National Institute of Nursing Research.
Footnotes
Financial Disclosure: The authors did not report any potential conflicts of interest.
References
- 1.Anthony S, Ouden L, Brand R, Verloove-Vanhorick P, Gravenhorst JB. Changes in perinatal care and survival in very preterm and extremely preterm infants in The Netherlands between 1983 and 1995. Eur J Obstet Gynecol Reprod Biol. 2004;112:170–177. doi: 10.1016/s0301-2115(03)00328-2. [DOI] [PubMed] [Google Scholar]
- 2.Fanaroff AA, Hack M, Walsh MC. The NICHD neonatal research network: changes in practice and outcomes during the first 15 years. Semin Perinatol. 2003;27:281–287. doi: 10.1016/s0146-0005(03)00055-7. [DOI] [PubMed] [Google Scholar]
- 3.Doyle LW, Betheras FR, Ford GW, Davis NM, Callanan C. Survival, cranial ultrasound and cerebral palsy in very low birth weight infants: 1980s versus 1990s. J Paediatr Child Health. 2000;36:7–12. doi: 10.1046/j.1440-1754.2000.00452.x. [DOI] [PubMed] [Google Scholar]
- 4.Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity — moving beyond gestational age. New Engl J Med. 2008;358:1672–1681. doi: 10.1056/NEJMoa073059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dani C, Poggi C, Romagnoli C, Bertini G. Survival and major disability rate in infant born at 22–25 weeks of gestation. J Perinat Med. 2009;37:599–608. doi: 10.1515/JPM.2009.117. [DOI] [PubMed] [Google Scholar]
- 6.Stake R. The art of case study research. London: Sage; 1995. [Google Scholar]
- 7.O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G. A decision aid for women considering hormone therapy after menopause: Decision support framework and evaluation. Patient Ed Counsel. 1998;33:267–279. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 8.Partridge JC, Martinez AM, Nishida H, Boo NY, Tan KW, Yeung CY, et al. International comparison of care for very low birth weight infants: Parents’ perceptions of counseling and decision-making. Pediatrics. 2005;116:e263–e271. doi: 10.1542/peds.2004-2274. [DOI] [PubMed] [Google Scholar]
- 9.Lamiani G, Meyer EC, Browning DM, Brodsky D, Todres ID. Analysis of enacted difficult conversations in neonatal intensive care. J Perinatol. 2009;29:310–316. doi: 10.1038/jp.2008.228. [DOI] [PubMed] [Google Scholar]
- 10.Payot A, Gendron S, Lefebvre F, Doucet H. Deciding to resuscitate extremely premature babies. How do parents and neonatologists engage in the decision? Soc Sci Med. 2007;64:1487–1500. doi: 10.1016/j.socscimed.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 11.Kaempf JW, Tomlinson SW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: Medical care guidelines, family choices, and neonatal outcomes. Pediatrics. 2009;123:1509–1515. doi: 10.1542/peds.2008-2215. [DOI] [PubMed] [Google Scholar]
- 12.Keogh J, Sinn J, Hollebone K, Bajuk B, Fischer W, Jui K, et al. Delivery in the grey zone: Collaborative approach to extremely preterm birth. Aust NZ J Obstet Gynecol. 2007;47:273–278. doi: 10.1111/j.1479-828X.2007.00737.x. [DOI] [PubMed] [Google Scholar]
- 13.Lavin JP, Kantak A, Ohlinger J, Kaempf JW, Tomlinson M, Campbell B, et al. Attitudes of obstetric and pediatric health care providers toward resuscitation of infants who are born at the margins of viability. Pediatrics. 2006;118:S169–S176. doi: 10.1542/peds.2006-0913O. [DOI] [PubMed] [Google Scholar]
- 14.Miquel-Verges F, Woods SL, Aucott SW, Boss RD, Sulpar LJ, Donohue PK. Prenatal consultation with a neonataologist for congenital anomalies: Parental perceptions. Pediatrics. 124:e573–e579. doi: 10.1542/peds.2008-2865. [DOI] [PubMed] [Google Scholar]
- 15.Schroeder J. Ethical issues for parents of extremely premature infants. J Ped Child Health. 2008;44:302–304. doi: 10.1111/j.1440-1754.2008.01301.x. [DOI] [PubMed] [Google Scholar]
- 16.Ohlinger J, Kantak A, Lavin JP, Fofah O, Hagen E, Suresh G, et al. Evaluation and development of potentially better practices for perinatal and neonatal communication and collaboration. Pediatrics. 2006;118:S147–S152. doi: 10.1542/peds.2006-0913L. [DOI] [PubMed] [Google Scholar]