Abstract
Objective
To evaluate a multidimensional model testing disease activity, mood disturbance, and poor sleep quality as determinants of fatigue in patients with rheumatoid arthritis (RA).
Method
The data of 106 participants were drawn from baseline of a randomized comparative efficacy trial of psychosocial interventions for RA. Sets of reliable and valid measures were used to represent model constructs. Structural equation modeling was used to test the direct effects of disease activity, mood disturbance, and poor sleep quality on fatigue, as well as the indirect effects of disease activity as mediated by mood disturbance and poor sleep quality.
Results
The final model fit the data well, and the specified predictors explained 62% of the variance in fatigue. Higher levels of disease activity, mood disturbance, and poor sleep quality had direct effects on fatigue. Further, disease activity was indirectly related to fatigue through its effects on mood disturbance, which, in turn, was related to poor sleep quality. Mood disturbance also indirectly influenced fatigue through poor sleep quality.
Conclusion
The findings from this study confirmed the importance of a multidimensional framework in evaluating the contribution of disease activity, mood disturbance, and sleep quality to fatigue in RA using a structural equation approach. Mood disturbance and poor sleep quality played major roles in explaining fatigue along with patient-reported disease activity.
Key Indexing Terms: Rheumatoid arthritis, Fatigue, Mood, Sleep disorders, Psychological factors
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, inflammatory disease characterized by joint pain, stiffness, and inflammation of the synovial tissue in the joints (1, 2). While fatigue is not a required symptom for the diagnosis of RA, persistent fatigue is a problem for greater than 50% of the patients with rheumatoid arthritis (3, 4). In many instances, fatigue may contribute to work disability and interfere with role functioning in RA, thus adding significantly to patients’ disease burden (5, 6). Despite the prevalence and effect of fatigue, research on the use of biologic agents and disease-modifying drugs in the treatment of fatigue is limited and inconclusive (7). Because of ambiguities in the etiology and treatment of fatigue, the management of fatigue in clinical practice is a challenge to clinicians and patients alike.
The identification of factors that contribute to RA fatigue may lead to enhanced approaches to treatment and management. Disease activity and excessive inflammation have been postulated to contribute significantly to fatigue in RA (8). Pain and fatigue in RA tend to be positively correlated (9, 10), leading researchers to conclude that fatigue may be the product of the inflammatory response or a secondary response to other disease characteristics (8). However, studies analyzing the association between disease activity and fatigue in RA have not demonstrated that inflammation is an important explanatory factor in fatigue (9, 11, 12, 13, 14). For example, Bergman et al. (13) found weak associations between fatigue and erythrocyte sedimentation rate (ESR), tender and swollen joints, and the 28-joint Disease Activity Score (DAS28), and a much stronger correlation between patients’ global health rating and fatigue in a cohort of 2096 RA patients. Using a multivariate approach, Riemsma et al (9) found that pain, low efficacy expectations, and problematic support explained 37% of the variance in fatigue, while ESR, rheumatoid factor, and hemoglobin did not contribute to fatigue. In a more recent study finding similar results Van Hoogmoed et al. (14), reported that pain, disability, depression, and low self-efficacy were associated with greater fatigue, but that inflammatory indices were not correlated with fatigue severity.
In view of these conflicting results, a multidimensional approach, incorporating psychosocial factors, may be warranted in analyzing the factors that contribute to fatigue in RA. In addition to pain and fatigue, many RA patients have problems with mood and sleep. For example, between 20% and 30% of patients experience significant depressive symptoms or may suffer from a mood disorder (15), while greater than 50% report problems with sleep continuity, insomnia, and poor sleep quality (16). Poor sleep may result from depression, and depression and poor sleep may jointly contribute to fatigue in RA (17). Thus, fatigue may be the product of RA disease activity, along with depression and poor sleep. It is also possible that disease activity may affect fatigue indirectly, by leading to mood disturbance and/or sleeping difficulties. Therefore, it is possible that depression and poor sleep quality may be potential mechanisms through which disease activity contributes to fatigue. These mechanisms could then be targeted for the management of fatigue in RA. Current research, however, has not addressed the direct and indirect contributions of disease activity to fatigue through these mechanisms. Thus, questions regarding the etiology of fatigue in RA are largely unresolved.
The major purpose of this research was to examine a model describing the interrelations among disease activity, mood disturbance, and poor sleep quality as determinants of fatigue in an urban sample of patients with rheumatoid arthritis. Structural equation modeling was adopted to illustrate the complexity of relations among variables in the proposed model (see Figure 1). It was hypothesized that disease activity would be positively associated with fatigue directly and/or indirectly through the potential mediators of mood disturbance and poor sleep quality. Specifically, the model proposed that higher levels of disease activity would lead to greater mood disturbance, which in turn would contribute to poor sleep quality. Further, higher levels of disease activity and poor sleep quality were expected to contribute to greater fatigue. Finally, it was also hypothesized that the effect of disease activity on fatigue would, at least in part, be indirect, through its effects on mood disturbance and sleep quality.
Figure 1.
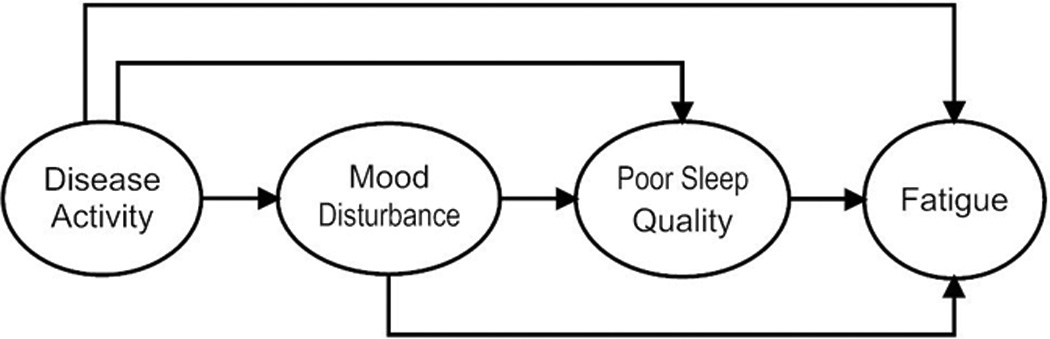
Hypothesized direct and indirect effects disease activity mood disturbance and poor sleep quality on fatigue.
MATERIALS AND METHODS
Patient sample
Participants were recruited through flyers posted in clinics in the Divisions of Rheumatology at Cedars Sinai Medical Center (CSMC) and the University of California, Los Angeles (UCLA), and through advertisements in local newspapers, announcing a treatment outcome study designed to help patients manage RA. Patients were referred to CSMC to determine medical eligibility after they had passed a telephone screening. After obtaining informed consent to participate in the project, the study rheumatologist (MW) at CSMC conducted a diagnostic evaluation to verify the RA diagnosis. Participants had to (1) be 18 years of age or older; (2) fulfill the American College of Rheumatology revised criteria for RA; (3) have a stable disease- modifying drug regimen for 3 months prior to study entry; (4) have a stable disease course for 3 months; (5) be free of serious comorbid medical conditions such as diabetes, congestive heart failure, renal failure, cancer, or fibromyalgia, which would confound interpretations of health status; and (6) not be pregnant.
At UCLA, eligible patients gave a second informed consent to participate in an evaluation of psychiatric status, physical functioning, and psychosocial adjustment. The Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (18) was administered, and psychiatric diagnoses were made in a consensus meeting with the principal investigator (PN) and project psychiatrist (MI). Patients who had a serious psychiatric condition such as bipolar disorder, psychosis, or posttraumatic stress disorder, or who were at risk for suicide, were ineligible to participate. Because none of the patients had any of those conditions, no patients were excluded after the diagnostic evaluation.
Data collection
This research reports on baseline data collected from all eligible participants who qualified for a treatment outcome study examining the efficacy of behavioral interventions for RA. At baseline, the psychosocial functioning and disease activity of participants were evaluated. The psychosocial component of the evaluation included self-report assessments of disease activity, mood disturbance, sleep, and fatigue, which are the focus of this report. In addition, reports of medication use were obtained, including analgesics/nonsteroidal antiinflammatory drugs, biologic agents, disease-modifying antirheumatic drugs (DMARD), and “other” (drugs for other medical conditions, including psychotropic agents).
Measures
The structural model tested in our study (Figure 1) was composed of the constructs of disease activity, mood disturbance, poor sleep quality, and fatigue. Multiple reliable and valid measures were used to serve as indicators in the model to increase the reliability of each construct
The latent variable, disease activity, included 2 indicators representing joint pain/tenderness and RA disease activity as measured in the Rapid Assessment of Disease Activity in Rheumatology scale (RADAR; 19). The RADAR joint pain/tenderness assesses degree of pain/tenderness in 10 joints on the right and left sides of the body. Items are rated on a 4-point Likert scale; the sum score may range from 0 to 60, with higher scores indicating more severe joint pain/tenderness. For self-perceived RA disease activity, respondents rated “How active has your arthritis been over the past 6 months?” and “How active is your arthritis today?” on 10-point visual analog scales, higher scores indicating greater perceived disease activity. Scores on the 2 scales were totaled to create a single disease activity variable. The RADAR has been shown to be an efficient, valid proxy for physician assessments of disease activity and joint pain (20).
Mood disturbance was included as a latent variable with 2 indicators representing the Center for Epidemiological Studies Depression Scale (CES-D; 21) and the Perceived Stress Scale (PSS; 22). The CES-D consists of 20 items and was designed to assess the existence of depressive symptomatology in community samples and nonpsychiatric groups. Scores may range from 0 to 60, with higher scores signifying the presence of more symptomatology. The PSS, comprising 10 items, measures the degree to which participants find their lives to be unpredictable, uncontrollable, and overwhelming. The PSS assesses the cognitive and emotional burden of feeling stressed rather than events that may lead to stress. Scores may range from 0 to 40, higher scores indicating greater perceived stress.
The Pittsburgh Sleep Quality Index (PSQI; 23) measured patients’ sleep quality. The PSQI is a 19-item scale that has demonstrated strong internal consistency and diagnostic validity in the evaluation of self-reported sleep disturbance. Seven sleep component scores are derived and each may range from 0 (no difficulty) to 3 (severe difficulty). Three indicators of the latent variable poor sleep quality were adopted, representing PSQI component scores (24): (1) sleep efficiency, the sum of sleep duration and habitual sleep efficacy subscales; (2) perceived sleep quality, the sum of subjective sleep quality, sleep latency, and sleeping medication use subscales; and (3) daily disturbances, the sum of sleep disturbances and daytime dysfunction subscales. Two indicators were used to measure the latent variable, fatigue: the Multidimensional Assessment of Fatigue (MAF) Global Fatigue Index (25) and the Vitality Subscale of the Medical Outcomes Study Short Form-36 (SF-36; 26) questionnaire. The MAF consists of 16 items measuring severity and effect of fatigue and has been used in RA research (24). Scores may range from 1 to 50, higher scores representing more severe fatigue. The SF-36 Vitality Subscale is a 4-item subscale with 2 positively worded items (“Did you feel full of pep?” and “Did you have a lot of energy?”) and 2 negatively worded items (“Did you feel worn out?” and “Did you feel tired?”). Scores may range from 0 to 100, higher scores indicating higher levels of vitality.
Statistical analyses
Structural equation modeling was used to test the hypotheses exploring the proposed relations among disease activity, mood disturbance, sleep quality, and fatigue. The hypothesized model was tested using Bentler’s structural equations program (EQS 6.1) with the maximum likelihood method of estimation (27). The model was assessed using multiple fit criteria: χ2 goodness-of-fit statistic, the ratio of χ2 to the degrees of freedom (χ2/df), the Comparative Fit Index (CFI), the standardized root mean residual (SRMR), and the root mean square error of approximation (RMSEA). A statistically nonsignificant χ2 (p > .05) is suggestive of a good match between the data and the hypothesized model. Additionally, a ratio of χ2 to degrees of freedom value < 2 (χ2/df < 2) is considered another indicator of good model fit. A CFI value > .90 is considered evidence of a good-fitting model (28). For SRMR and RMSEA, the joint criteria of an SRMR < .09 and an RMSEA < .06 is considered optimal to minimize the rates of type I and type II error (29). Model modifications were performed based on results from the Wald test and the Lagrange multiplier (LM) test, along with theoretical considerations.
Covariates
The associations between medication use (i.e., analgesics/non-steroidal antiinflammatory drugs, biologic agents, DMARD, and other medications) and the indicator variables of sleep disturbance and fatigue were also assessed to determine their potential effect on model findings. If statistically significant, relevant covariates would have been partitioned from the indicators of the noted outcomes prior to SEM analyses.
RESULTS
Sample characteristics
A total of 106 patients were included in the study. Table 1 shows demographic characteristics of the sample. The sample consisted of 88 females and 18 males, with an average age of 56.09 years and illness duration of 11.23 years. Participants came from a range of ethnicities. Whites were the most prevalent group, but patients from African-American, Hispanic, and Asian ethnicities were also represented. The sample can be characterized as middle to upper middle class, possessing almost 16 years of education on average, and a median household income of greater than $50,000.
Table 1.
Demographic characteristics of sample (n = 106).
| N (%) | |
|---|---|
| Gender | |
| Male | 18 (16.98) |
| Female | 88 (83.02) |
| Race/Ethnicity | |
| White | 56 (53.83) |
| Hispanic | 16 (15.09) |
| Black | 11 (10.38) |
| Asian/Pacific Islander | 8 (75.45) |
| Other race/ethnicity | 15 (14.15) |
| Marital Status | |
| Married | 46 (43.40) |
| Divorced/Separated | 26 (24.53) |
| Widowed | 9 (8.49) |
| Single | 13 (12.26) |
| Other/unknown | 12 (11.32) |
|
M(SD) |
|
| Age in years | 56.09 (12.45) |
| Yearly median income ($) by zip | 50,850 (22,525) |
| Education in years | 15.95 (2.40) |
| Years since RA diagnosis | 10.75 (11.23) |
SEM Results
Prior to testing the model, the data were screened and results revealed a normal distribution and no multivariate outliers. Further, in the assessment of covariates, none of the associations between medication use and the indicators variables of sleep disturbance and fatigue were found to be statistically significant (correlations among model variables are given in Table 2). The hypothesized model provided a good fit to the data, CFI = .997; χ2(21) = 22.29, p = .383; χ2/df = 1.06; SRMR = .039; RMSEA = .024. However, the Wald test indicated that the impact of deleting the path from disease activity to sleep disturbance on the χ2 of the model would be minimal. Therefore, based on theoretical plausibility, and in an effort to simplify the mode, this path was removed. The fit of this revised model was similar, CFI = .999; χ2(22) = 22.45, p = .433; χ2/df = 1.02; SRMR = .040; RMSEA = .014, and the model now consisted of only statistically significant paths (p < .05; Table 3). The Wald test and the LM test did not indicate any further improvement of the model through the deletion or addition of paths. Overall, the specified predictors explained 19% of the variance in mood disturbance, 22% of the variance in sleep quality, and 62% of the variance in fatigue.
Table 2.
Intercorrelations, means, and standard deviations for study variables (n = 106).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. RADAR total joint | -- | ||||||||
| 2. RADAR disease activity | .617*** | -- | |||||||
| 3. CES-D total | .307*** | .332*** | -- | ||||||
| 4. Perceived stress scale total | .273*** | .295*** | .645*** | -- | |||||
| 5. PSQI sleep efficiency | .064 | .069 | .152 | .135 | -- | ||||
| 6. PSQI sleep quality | .139 | .150 | .329*** | .292*** | .297*** | -- | |||
| 7. PSQI daily disturbances | .165* | .178* | .390*** | .347*** | .352*** | .762*** | -- | ||
| 8. SF-36 vitality subscale | −.381*** | −.411*** | −.357*** | −.318*** | −.212** | −.459*** | −.544*** | -- | |
| 9. MAF global fatigue index | .372*** | .401*** | .349*** | .310*** | .207** | .447*** | .531*** | −.787*** | -- |
| M | 11.45 | 10.60 | 8.87 | 11.35 | 1.43 | 2.43 | 1.71 | 53.73 | 21.03 |
| SD | 9.34 | 6.93 | 9.17 | 6.90 | 1.43 | 2.04 | 1.29 | 23.71 | 10.56 |
p < .05
p < .01
p < .001.
Table 3.
Path coefficients from final revised structural equation model.
| Unstandardized | SE | Standardized | |
|---|---|---|---|
| Direct effects | |||
| Disease activity → Mood disturbance | 3.355*** | .933 | .437 |
| Disease activity → Fatigue | 2.595** | .913 | .285 |
| Mood disturbance → Poor sleep quality | .076*** | .018 | .469 |
| Mood disturbance → Fatigue | .402** | .143 | .338 |
| Poor sleep quality → Fatigue | 3.004*** | .754 | .408 |
| Indirect effects | |||
| Disease activity → Poor sleep quality | .254** | .087 | .205 |
| Disease activity → Fatigue | 2.110** | .698 | .231 |
| Mood disturbance → Fatigue | .227** | .073 | .191 |
p < .01
p < .001
Test of research hypotheses
Inspection of the path coefficients showed that the hypothesized relations among model constructs were generally confirmed (Table 3). As expected, disease activity exerted a positive influence on mood disturbance (β = .44, p < .001), and higher levels of mood disturbance predicted poorer sleep quality (β = .47, p < .001). In turn, poor sleep quality exerted a strong, positive, direct effect on fatigue (β = .41, p < .001). Furthermore, disease activity directly and positively predicted fatigue (β = .29, p = .005). Disease activity was also positively, indirectly related to fatigue through mood disturbance and poor sleep quality (βindirect = .23, p = .003). In addition, mood disturbance directly and indirectly influenced fatigue through poor sleep quality (β = .34, p = .005 and βindirect = .19, p = .002, respectively). The final model with standardized path coefficients is shown in Figure 2.
Figure 2.
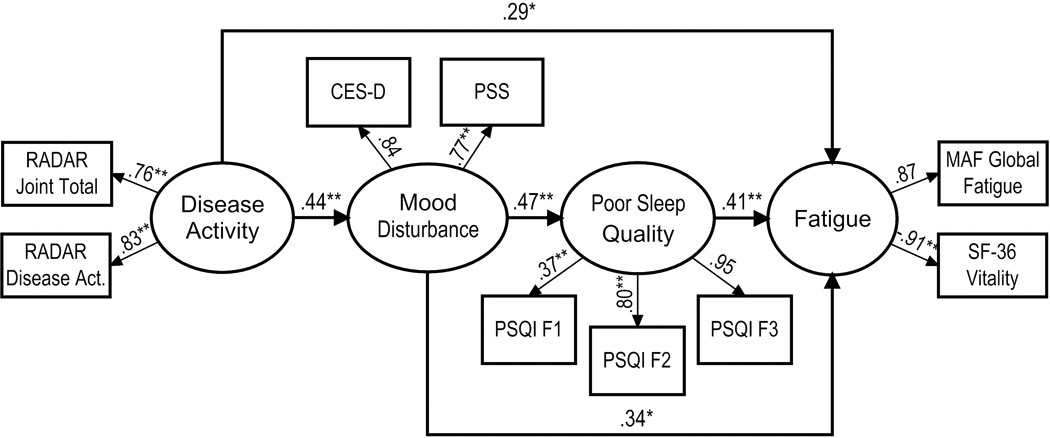
Final model with estimated path coefficients and factor loadings. RADAR Joint Total = Rapid Assessment of Disease Activity in Rheumatoloy Joint Total score; RADAR Disease Act. = Rapid Assessment of Disease Activity in Rheumatology Disease Activity score; CES-D = Center for Epidemiological Studies Depression scale; PSS = Perceived Stress Scale; PSQI F1 = Pittsburgh Sleep Quality Index sleep efficiency fact; PSQI F2 = Pittsburgh Sleep Quality Index perceived sleep quality factor; PSQI F3 = Pittsburgh Sleep Quality Index daily disturbances factor; MAF Global Fatigue = Multidimensional Assessment of Fatigue Global Fatigue index; SF-36 Vitality = Vitality Subscale of the SF-36. *p < .01, ** p < .001.
DISCUSSION
The causes of fatigue in RA are difficult to interpret in clinical practice. While RA fatigue has been viewed as the byproduct of the inflammatory response and heightened disease activity, previous research has shown that disease activity is inconsistently related to fatigue, and that psychosocial factors may play a crucial role in this symptom (13, 14). Accordingly, the goal of our research was to evaluate a multidimensional model, based on the assumption that several factors may contribute to fatigue in RA. A structural equation modeling approach was adopted to illustrate both direct and indirect mechanisms through which disease activity could potentially contribute to fatigue in an urban sample of patients with RA. Specifically, we examined whether RA disease activity would contribute to fatigue through mood disturbance and poor sleep quality.
The initial model examined the hypothesis that disease activity would contribute to mood disturbance and poor sleep quality, which in turn would contribute to higher fatigue. The path from mood disturbance to poor sleep quality was also examined. While this model had very good fit, because the path from disease activity to poor sleep quality was not significant, an alternative model was examined that eliminated this path. This alternative model had slightly better fit and served as a more restrained explanation of the data. The final model revealed a significant, indirect path from disease activity to mood disturbance, from mood disturbance to poor sleep quality, and from poor sleep quality to fatigue. Both disease activity and mood disturbance retained direct relationships with fatigue.
Our findings extend the work of previous research showing that pain and depression are both related to RA fatigue (6, 10), and that patients who have a history of an affective disorder have more fatigue with RA than patients who do not (30). Importantly, the data also revealed that RADAR scores, comprising both joint pain and reports of disease activity, were related to fatigue through mood disturbance, which in our study was measured by depression and perceived stress. Mood disturbance thus may serve as an important pathway through which disease activity exacerbates fatigue. Other research has shown a significant relationship between RA disease activity and depression (31), but our study has provided a new perspective on how these variables may act conjointly to affect fatigue.
The model also found that poor sleep quality was related to fatigue. Previous research has found a high prevalence of sleep disturbance in RA16, and that both pain and depression may contribute to poor sleep (17). Using daily diary data, Goodchild, et al (32) found that the previous night’s discomfort was associated with lower sleep efficiency and poorer sleep quality in RA. Our results demonstrated that while mood disturbance contributed significantly to poor sleep quality, disease activity was related to poor sleep quality only through mood disturbance. Thus, coupled with the findings above, mood disturbance was an important mediational variable through which disease activity contributed to both poor sleep and fatigue.
Our findings suggest that fatigue in RA may have multiple determinants. Previous studies, using multidimensional models, have also documented the importance of such variables as pain, mood, and coping processes in explaining RA fatigue (9, 14). Importantly, the findings of this research illustrate the significance of conceptualizing the links between disease activity and functional outcomes in RA. A possible reason for the inconsistent relationship between disease activity and fatigue in RA in previous studies may be that the indirect relationships between disease activity, psychological factors, and fatigue had not been analyzed. Importantly, this research has shown that the contribution of disease activity to fatigue is largely explained by mechanisms underlying mood disturbance and poor sleep. Our findings also have clinical relevance, suggesting that treatments that focus on better mood regulation and sleep may contribute to improvement in patients’ fatigue and vitality. Findings reported by Hewlett, et al (33) and Evers, et al (34) indicate that cognitive-behavior therapy may promote improvement in fatigue and mood in patients with RA. Thus, successful treatment for RA disease activity may not lead to reduced fatigue unless problems in mood and sleep are adequately addressed.
It is important to note that, while all measures in the study had demonstrated validity, the use of self-report may have contributed in some degree to the magnitude of the relationships that were observed among constructs. The report of poor sleep or short sleep duration may reflect the existence of anxious-ruminative traits or inadequate resources for managing stress (35, 36). The PSQI, for example, has been shown to be more closely related to depression and psychological distress than to polysomnographic abnormalities (37, 38). While the PSQI is one of the best-established and widely used self-report measures of sleep quality, other instruments may also be appropriate for measuring sleep quality in RA and should be considered in future research (39). The measurement of the perception of sleep health in medical populations remains an important challenge because of the difficulty in separating illness-related symptoms from those associated with reports of sleep quality.
Despite the excellent fit of the model that we examined, the study possessed some limitations that warrant a cautious interpretation of the results. First, because the findings from this research were based on an urban RA sample recruited to participate in psychosocial research, they may not be generalizable to other patient populations such as those residing in rural areas or those out of the mainstream of clinical care. Second, while the findings are consistent with the model that was hypothesized, the cross-sectional design precluded an interpretation of causality or directionality among variables. The structural equation model that was examined was based only on hypothesized relationships between the variables chosen. Nonrecursive, synergistic relationships may exist between variables that were examined, leading to the consideration of other plausible models linking disease activity with fatigue. Poor sleep, for example, may contribute to both mood disturbance and pain (40), which in turn may lead to greater fatigue. Longitudinal research and studies adopting daily assessment procedures that identify the ebb and flow of RA disease activity, mood disturbance, sleep, and fatigue (41) would clarify the directional and mediational mechanisms that we examined.
ACKNOWLEDGMENT
The authors wish to acknowledge Kate Jackson, B.A., and Sarosh J. Motivala, Ph.D., who contributed to the diagnostic evaluation and assessment of participants in the project.
Supported by AR R01-049840 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institute of Health (P.M. Nicassio). Also supported in part by T32-MH19925, HL 079955, AG034588, AG026364, CA119159, DA 027558, RR00827, P30-AG028748, General Clinical Research Centers Program, the UCLA Cousins Center at the Semel Institute for Neurosciences, and the UCLA Older Americans Independence Center Inflammatory Biology Core.
REFERENCES
- 1.Wolfe F, Cathey M. The assessment and prediction of functional disability in rheumatoid arthritis. J Rheumatol. 1991;18:1298–1306. [PubMed] [Google Scholar]
- 2.Escalante A, Del Rincón I. The disablement process in rheumatoid arthritis. Arthritis Rheum. 2002;47:333–342. doi: 10.1002/art.10418. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe F, Hawley DJ, Wilson K. The prevalence and meaning of fatigue in rheumatic disease. J Rheumatol. 1996;23:1407–1417. [PubMed] [Google Scholar]
- 4.Tack BB. Self-reported fatigue in rheumatoid arthritis: a pilot study. Arthritis Care Res. 1990;3:154–157. [PubMed] [Google Scholar]
- 5.Belza BL, Henke CJ, Yelin EH, Epstein WV, Gilliss CL. Correlates of fatigue in older adults with rheumatoid arthritis. Nurs Res. 1993;42:93–99. [PubMed] [Google Scholar]
- 6.Mancuso CA, Paget SA, Charlson ME. Adaptations made by rheumatoid arthritis patients to continue working: a pilot study of workplace challenges and successful adaptations. Arthritis Care Res. 2000;13:89–99. [PubMed] [Google Scholar]
- 7.Chauffier K, Salliot C, Berenbaum F, Sellam J. Effect of biotherapies on fatigue in rheumatoid arthritis: A systematic review of the literature and meta-analysis. Rheumatology. 2012;51:60–68. doi: 10.1093/rheumatology/ker162. [DOI] [PubMed] [Google Scholar]
- 8.Aletaha D, Landewe R, Karonitsch T, Bathon J, Boers M, Bombardier C, et al. Reporting disease activity in clinical trials of patients with rheumatoid arthritis: EULAR/ACR collaborative recommendations. Arthritis Rheum. 2008;59:1371–1377. doi: 10.1002/art.24123. [DOI] [PubMed] [Google Scholar]
- 9.Riemsma RP, Rasker JJ, Taal E, Griep EN, Wouters JM, Wiegman O. Fatigue in rheumatoid arthritis: the role of self-efficacy and problematic social support. Br J Rheumatol. 1998;37:1042–1046. doi: 10.1093/rheumatology/37.10.1042. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe F. Determinants of WOMAC function, pain and stiffness scores: evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology (Oxford) 1999;38:355–361. doi: 10.1093/rheumatology/38.4.355. [DOI] [PubMed] [Google Scholar]
- 11.Pollard LC, Choy EH, Gonzalez J, Khoshaba B, Scott DL. Fatigue in rheumatoid arthritis reflects pain, not disease activity. Rheumatology (Oxford) 2006;45:885–889. doi: 10.1093/rheumatology/kel021. [DOI] [PubMed] [Google Scholar]
- 12.Repping-Wuts H, Fransen J, van Achterberg T, Bleijenberg G, van Riel P. Persistent severe fatigue in patients with rheumatoid arthritis. J Clin Nurs. 2007;16:377–383. doi: 10.1111/j.1365-2702.2007.02082.x. [DOI] [PubMed] [Google Scholar]
- 13.Bergman MJ, Shahouri SS, Shaver TS, Anderson JD, Weidensaul DN, Busch RE, et al. Is fatigue an inflammatory variable in rheumatoid arthritis (RA)? Analyses of fatigue in RA, osteoarthritis, and fibromyalgia. J Rheumatol. 2009;36:2788–2794. doi: 10.3899/jrheum.090561. [DOI] [PubMed] [Google Scholar]
- 14.van Hoogmoed D, Fransen J, Bleijenberg G, van Riel P. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology (Oxford) 2010;49:1294–1302. doi: 10.1093/rheumatology/keq043. [DOI] [PubMed] [Google Scholar]
- 15.Covic T, Tyson G, Spencer D, Howe G. Depression in rheumatoid arthritis patients: demographic, clinical, and psychological predictors. J Psychosom Res. 2006;60:469–476. doi: 10.1016/j.jpsychores.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Abad VC, Sarinas PS, Guilleminault C. Sleep and rheumatologic disorders. Sleep Med Rev. 2008;12:211–228. doi: 10.1016/j.smrv.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Wolfe F, Michaud K, Li T. Sleep disturbance in patients with rheumatoid arthritis: evaluation by medical outcomes study and visual analog sleep scales. J Rheumatol. 2006;33:1942–1951. [PubMed] [Google Scholar]
- 18.Spitzer RL, Williams JBW, Gibbon M. Structured clinical interview for DSM-III-R (SCID) New York: Biometrics Research; 1987. [Google Scholar]
- 19.Wong AL, Wong WK, Harker J, Sterz M, Bulpitt K, Park G, et al. Patient self-report tender and swollen joint counts in early rheumatoid arthritis. J Rheumatol. 1999;26:2551–2561. [PubMed] [Google Scholar]
- 20.Calvo FA, Calvo A, Berrocal A, Pevez C, Romero F, Vega E, et al. Self-administered joint counts in rheumatoid arthritis: Comparison with standard joint counts. J Rheumatol. 1999;26:536–539. [PubMed] [Google Scholar]
- 21.Radloff L. The CES-D Scale: A self-report depression scale for research in general populations. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22.Cohen AS, Williamson GM. Perceived stress in a probability sample of the United States. In: Scapacan S, Oskamp S, editors. The social psychology of health. 4th ed. Newbury Park, CA: Sage Publications; 1988. pp. 31–67. [Google Scholar]
- 23.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 24.Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep. 2006;29:112–116. doi: 10.1093/sleep/29.1.112. [DOI] [PubMed] [Google Scholar]
- 25.Belza BL. Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol. 1995;22:639–643. [PubMed] [Google Scholar]
- 26.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 27.Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software; 2005. [Google Scholar]
- 28.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 88:588–606. 980. [Google Scholar]
- 29.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;16:1–55. [Google Scholar]
- 30.Jump RL, Fifield J, Tennen H, Reisine S, Giuliano AJ. History of affective disorder and the experience of fatigue in rheumatoid arthritis. Arthritis Care Res. 2004;51:239–245. doi: 10.1002/art.20243. [DOI] [PubMed] [Google Scholar]
- 31.Godha D, Shi L, Mavronicolas H. Association between tendency towards depression and severity of rheumatoid arthritis from a national representative sample: the Medical Expenditure Panel Survey. Curr Med Res Opin. 2010;26:1685–1690. doi: 10.1185/03007991003795808. [DOI] [PubMed] [Google Scholar]
- 32.Goodchild CE, Treharne GJ, Booth DA, Bowman SJ. Daytime patterning of fatigue and its associations with the previous night’s discomfort and poor sleep among women with primary Sjogren’s syndrome or rheumatoid arthritis. Musculoskeletal Care. 2010;9:107–117. doi: 10.1002/msc.174. [DOI] [PubMed] [Google Scholar]
- 33.Hewlett S, Ambler N, Almeida C, Cliss A, Hammond A, Kitchen K, et al. Self-management of fatigue in rheumatoid arthritis: A randomised controlled trial of group cognitive-behavioural therapy. Ann Rheum Dis. 2011;70:1060–1067. doi: 10.1136/ard.2010.144691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evers AW, Kraaimaat FW, van Riel PL, de Jong AJ. Tailored cognitive-behavioral therapy in early rheumatoid arthritis for patients at risk: A randomized controlled trial. Pain. 2002;100:141–153. doi: 10.1016/s0304-3959(02)00274-9. [DOI] [PubMed] [Google Scholar]
- 35.Fernandez-Mendoza J, Calhoun SL, Bixler EO, Karataraki M, Liao D, Vela-Bueno A, et al. Sleep misperception and chronic insomnia in the general population: Role of objective sleep duration and psychological profiles. Psychosom Med. 2011;73:88–97. doi: 10.1097/PSY.0b013e3181fe365a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanable PA, Aikens JE, Tadimeti L, Caruana-Montaldo B, Mendelson WB. Sleep latency and duration estimates among sleep disorder patients: Variability as a function of sleep disorder diagnosis, sleep history, and psychological characteristics. Sleep. 2000;23:71–79. [PubMed] [Google Scholar]
- 37.Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–571. [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor-Gjevre RM, Gjevre JA, Nair B, Skomro R, Lim HJ. Components of sleep quality and sleep fragmentation in rheumatoid arthritis and osteoarthritis. Musculoskeletal Care. 2011 Jun 5; doi: 10.1002/msc.208. (E-pub ahead of print) [DOI] [PubMed] [Google Scholar]
- 39.Wells GA, Li T, Kirwin JR, Peterson J, Aletaha D, Boers M, et al. Assessing quality of sleep in patients with rheumatoid arthritis. J Rheumatol. 2009;36:2077–2086. doi: 10.3899/jrheum.090362. [DOI] [PubMed] [Google Scholar]
- 40.Luyster FS, Chasens ER, Wasko MC, Dunbar-Jacob J. Sleep quality and functional disability in patients with rheumatoid arthritis. J Clin Sleep Med. 2011;7:49–55. [PMC free article] [PubMed] [Google Scholar]
- 41.Broderick JE, Schwartz JE, Schneider S, Stone AA. Can end-of-day reports replace momentary assessment of pain and fatigue? J Pain. 2009;10:274–281. doi: 10.1016/j.jpain.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


