Abstract
Purpose
To investigate the extent to which clinicians avoid well-established drug-drug interactions that cause statin-induced myopathy. We hypothesised that clinicians would avoid combining erythromycin or verapamil/diltiazem respectively with atorvastatin or simvastatin. In patients with statin-fibrate combination therapy, we hypothesised that gemfibrozil was avoided to the preference of bezafibrate or fenofibrate. When combined with verapamil/diltiazem or fibrates, we hypothesized that the dispensed doses of atorvastatin/simvastatin would be decreased.
Methods
Cross-sectional analysis of nationwide dispensing data. Odds ratios of interacting erythromycin, verapamil/diltiazem versus respective prevalence of comparator drugs doxycycline, amlodipine/felodipine in patients co-dispensed interacting statins simvastatin/atorvastatin versus patients unexposed (pravastatin/fluvastatin/rosuvastatin) was calculated. For fibrates, OR of gemfibrozil versus fenofibrate/bezafibrate in patients co-dispensed any statin was assessed.
Results
OR of interacting erythromycin versus comparator doxycycline did not differ between patients on interacting and comparator statins either in patients dispensed high or low statin doses (adjusted OR 0.87; 95% CI 0.60–1.25 and 0.92; 95% CI 0.69–1.23). Interacting statins were less common among patients dispensed verapamil/diltiazem as compared to patients on amlodipine/felodipine (OR high dose 0.62; CI 0.56–0.68 and low dose 0.63; CI 0.58–0.68). Patients on any statin were to a lesser extent dispensed gemfibrozil compared to patients not dispensed a statin (OR high dose 0.65; CI 0.55–0.76 and low dose 0.70; CI 0.63–0.78). Mean DDD (SD) for any statin was substantially higher in patients co-dispensed gemfibrozil 178 (149) compared to patients on statin monotherapy 127 (93), (p<0.001).
Conclusions
Prescribers may to some extent avoid co-prescription of statins with calcium blockers and fibrates with an increased risk of myopathy. We found no evidence for avoiding co-prescriptions of statins and antibiotics with an increased risk of statin-induced adverse drug reactions. Co-prescription of statins and gemfibrozil is paradoxically associated with a marked increased statin dose, further aggravating the risk for severe myopathy.
Introduction
The introduction of HMG-CoA reductase inhibitors, (statins) has had a major impact on the modern management of cardiovascular disease. In high risk populations, statin treatment decreases morbidity and mortality by 30% and has therefore become widely used [1].
Although considered relatively safe, statins are associated with adverse drug reactions [2] including statin induced myopathy. The incidence of rhabdomyolysis has, in clinical trials, ranged from 0.1–0.6% [3] which may underestimate the occurrence in ‘real world’ patients due to the exclusion of patients with risk factors. Known risk factors are increased age, female gender, dispensed statin dose and combination of drugs that increase the statin plasma level including erythromycin, diltiazem, verapamil and gemfibrozil [4]–[9]. There are currently five statins available on the Swedish market: simvastatin, atorvastatin, pravastatin, fluvastatin and rosuvastatin. The metabolism of simvastatin and atorvastatin depends heavily on the hepatic cytochrome P450 enzyme (CYP) 3A4 and is therefore susceptible for interactions with macrolides such as erythromycin, the calcium antagonists diltiazem and verapamil, – potent inhibitors of this enzyme [2], [10]–[18]. The remaining statins, are either eliminated unchanged (pravastatin and rosuvastatin) or are subject for a clearance based on other metabolic pathways (fluvastatin), and may therefore be an alternative for patients in need of long-term treatment with these drugs [2], [11], [14], [19]–[21]. Another strategy may be to use drugs with a similar indication that do not significantly inhibit CYP3A4 such as doxycycline instead of erythromycin and any of the alternative calcium antagonists amlodipine or felodipine instead of diltiazem or verapamil, or to decrease the administered statin dose [22]–[24]. Fibrates are another group of drugs used for the treatment of patients with hyperlipidemia. Gemfibrozil increases the plasma level for most statins due to interaction on transport protein level and has been associated with a large increased risk for myopathy (OATPBA1, p-glycoprotein P) [3], [5], [25]–[30]. For the group of patients at risk for stroke or heart infarction already being treated with a statin and in need for additional lipid-lowering treatment, a better alternative would therefore be fenofibrate or bezafibrate (Table 1) [5], [27], [31]–[34]. These differences are also reflected by respective labelling of the drugs and can be recognised using an interaction software program. In Sweden, SFINX (Swedish Finnish interaction X referencing) alerts approximately 80% of Swedish doctors for drug-drug interactions at the moment of prescribing [35]–[37].
Table 1. Rationale for the choice of study drugs.
| Labelled indications for groups of drugs according to FASS1 | Drugs (ATC code2) | Role of study drug | Rationale | Labelling according to FASS1 with regard to interactions leading to myopathy |
| HMG-CoA 3 | Simvastatin | CYP3A44 | Metabolism heavily dependent on | Co-administration with erythromycin is |
| Reductase inhibitors | (C10AA01) | interacting | CYP3A44. Its combination with | contraindicated. Co-administration with |
| statins | statin | inhibitors of this enzyme results in a | verapamil and gemfibrozil should be | |
| Used as first line | marked increase in plasma levels | avoided. Co-administration with diltiazem | ||
| treatment against | 11,12,14] and an elevated risk of | and verapamil should be used with caution | ||
| hyper | myopathy [2]. | and include close clinical monitoring / | ||
| cholesterolemia | dose reductions. | |||
| Atorvastatin | CYP3A44 | Metabolism dependent on | Combination with inhibitors of CYP3A44 | |
| (C10AA05) | interacting | CYP3A44 [10]. Its combination with | such as erythromycin, diltiazem and | |
| statin | inhibitors of this enzyme results in an | verapamil should be avoided/include | ||
| increase in plasma level [14], [16], [17] | close clinical monitoring/dose reductions. | |||
| and an elevated risk of myopathy | ||||
| 2,15]. | ||||
| Pravastatin | Comparator | Comparator statin. Mainly excreted | No warnings are issued regarding the co- | |
| (C10AA03) | statin | unchanged through the kidneys and | administration with inhibitors of | |
| via the bile into the faeces and not | CYP3A44. | |||
| subject for significant interactions on | ||||
| the basis of CYP3A44 inhibition | ||||
| 11,14,19]. | ||||
| Fluvastatin | Comparator | Is extensively metabolized by CYP2C95 | No warnings are issued regarding the co- | |
| (C10AA04) | statin | and not subject for significant interactions | administration with inhibitors of CYP3A44. | |
| on the basis of CYP3A44 inhibition [20]. | ||||
| Rosuvastatin | Comparator | Comparator statin. Ninety percent is being | No warnings are issued regarding the co- | |
| (C10AA07) | statin | excreted unchanged through the faeces [2]. | administration with inhibitors of CYP3A44. | |
| Plasma levels not elevated in the presence | ||||
| of potent inhibitors of CYP3A44 [21]. | ||||
| Antibiotics | Erythromycin | Interacting | A macrolide being a potent inhibitor of | Should not be used concomitantly with |
| Used against airway | (J01FA01) | antibiotic | CYP3A44 and p-glykoprotein [12], [16]. | simvastatin or atorvastatin. |
| infections, atypical | Doxycycline | Comparator | A tetracycline being metabolized to a very | No warnings are issued regarding the co- |
| pneumonia and | (J01AA02) | antibiotic | little extent [22]. | administration with statins. |
| patients allergic to | ||||
| penicillin. | ||||
| Calcium - | Verapamil | Interacting | Strong inhibitor of CYP3A44. Has | Co-administration with simvastatin, or |
| antagonists | (C08DA01) | calcium | increased simvastatin exposure and been | atorvastatin, should be used with caution and |
| Sharing indications | antagonist | associated with rhabdomyolysis [2], [12]. | lead to a dose reduction. | |
| against hypertension | Diltiazem | Interacting | Inhibitor of CYP3A44. Increased | Co-administration with a statin metabolised |
| and angina pectoris. | (C08DB01) | calcium | simvastatin exposure and is associated | by CYP3A44 should be avoided or include |
| Only verapamil and | antagonist | with rhabdomyolysis [18]. | close clinical monitoring. | |
| diltiazem may be used | Amlodipine | Comparator | Weak inhibitor CYP3A44. Clinically | No warnings are issued regarding the co- |
| for the treatment of | (C08CA01) | calcium | significant interactions with statins are | administration with statins. |
| atrial fibrillation. | antagonist | unlikely [23], [24]. | No warnings are issued regarding the co- | |
| Felodipine | Comparator | No significant inhibitor of CYP3A44 [24]. | administration with statins. | |
| (C08CA02) | calcium | |||
| antagonist | ||||
| Fibrates | Gemfibrozil | Interacting | Marked and clinically significant | Co-administration with statins should be |
| Used for the treatment | (C10AB04) | fibrate | pharmacokinetic interactions with statins | avoided. |
| of | on the basis of membrane transporter | |||
| hypertriglyceridemia | inhibition [25]–[30]. Concomitant use is | |||
| or when treatment of | associated with an increased risk of | |||
| statin is not tolerated | rhabdomyolysis [2], [3], [5]. | |||
| Fenofibrate | Comparator | Do not affect the plasma exposure of | Due to a pharmacodynamic interaction co- | |
| (C10AB05) | fibrate | statins [31]–[34]. | administration with statins should be used | |
| with caution. | ||||
| Bezafibrate | Comparator | Do not affect the plasma exposure of | Due to a pharmacodynamic interaction co- | |
| (C10AB02) | fibrate | statins [27]. | administration with statins should be used | |
| with caution. |
The Swedish summary of product characteristics [35].
Anatomical Therapeutic Chemical code.
3-hydroxy-3-methylglutaryl-coenzyme A.
Cytochrome P450 enzyme (CYP) 3A4.
Cytochrome P450 enzyme (CYP) 2C9.
The current study aims to investigate the compliance to guidelines on drug-drug interactions with the potential to cause statin induced myopathy on behalf of the prescribing doctors. We hypothesised that physicians in Sweden would avoid the combined use of statins and drugs that inhibit their metabolism and/or, when combined with drugs used on continuous basis, i.e. verapamil/diltiazem or fibrates, reduce the statin dose.
Methods
Ethics statement
This was a database study that included data on the entire Swedish population 18 years or older. Hence we did not interfere with the treatment of these individuals nor in any other way. Since the data was anonymized and none of the individuals were identifiable, the integrity of the individuals was not judged to be violated. This view was also supported by the Regional Ethics Committee in Stockholm, Karolinska Institute, which waived the need for written informed consent from the participants and approved the study as a whole.
Study design
The study design was a retrospective, cross-sectional analysis of patients being dispensed prescription drugs in Sweden during the period from 15 August to 15 December 2011. The choice of a four-month-study-period was based on the Swedish regulation and experience that most patients on long-term/chronic treatment repeat their drug-dispensing every third to fourth month. We selected all individuals, 18 years or older, that were dispensed any of the drugs presented in Table 1. The cohort was established on data obtained from the Swedish Prescribed Drug Register [38].
Data source
The Swedish Prescribed Drug Register contains data with unique patient identifiers for all dispensed prescriptions for the whole population of Sweden. The data collection is administered by the National Corporation of Swedish Pharmacies, a state-owned company responsible for the provision of pharmaceutical services at a nationwide level. Data on all dispensed prescriptions is transferred monthly to the National Board of Health and Welfare. The drugs were classified according to the Anatomical Therapeutic Chemical (ATC) classification system. We selected all individuals, 18 years and older, dispensed any of the drugs presented in Table 2.
Table 2. Prevalence of study drugs used in the adult Swedish population (≥18 years of age) and corresponding demographics, 15th August to 15th December, 2011.
| Study drugs | n | n/1000 individuals | Mean age (SD1) | Women (%) | Percentage of drugs2 prescribed from primary care | Mean number of drugs (SD1) | Mean dispensed DDD3 statin (SD1) |
| CYP3A4 4 | |||||||
| interacting | |||||||
| statins | |||||||
| simvastatin | 562 723 | 74 | 69 (11) | 45 | 84 (459075/548 863) | 6.8 (3.9) | 113 (68) |
| atorvastatin | 75 950 | 10 | 67 (10) | 43 | 70 (51 773/73 968) | 7.6 (4.2) | 209 (159) |
| Comparator | |||||||
| statins | |||||||
| rosuvastatin | 26 964 | 3.6 | 65 (10) | 44 | 67 (17 417/25 939) | 7.2 (4.2) | 202 (155) |
| pravastatin | 14 891 | 2.0 | 70 (11) | 50 | 83 (12 056/14 608) | 7.6 (4.3) | 125 (66) |
| fluvastatin | 311 | 0.041 | 71 (11) | 61 | 78 (163/209) | 7.6 (4.6) | 67 (47) |
| CYP3A4 3 | |||||||
| interaction with | |||||||
| statins | |||||||
| erythromycin5 | 8 795 | 1.2 | 46 (17) | 66 | 74 (6 286/8 505) | 5.4 (4.6) | NA6 |
| verapamil | 14 114 | 1.9 | 72 (13) | 61 | 76 (10 522/13820) | 7.7 (4.4) | NA |
| diltiazem | 11 341 | 1.5 | 73 (11) | 58 | 79 (8 726/11 091) | 8.7 (4.5) | NA |
| Pharmacokinetic | |||||||
| interaction with | |||||||
| all statins | |||||||
| gemfibrozil | 3 726 | 0.49 | 66 (11) | 33 | 84 (3 055/3 638) | 7.9 (4.5) | NA |
| Comparator | |||||||
| drugs | |||||||
| doxycycline | 143 564 | 19 | 52 (18) | 59 | 81 (112 531/138 641) | 5.9 (4.6) | NA |
| amlodipine | 255 969 | 34 | 69 (12) | 47 | 86 (216 892/251 344) | 6.6 (3.9) | NA |
| felodipine | 209 425 | 27 | 71 (12) | 50 | 87 (177 688/204 341) | 6.8 (3.9) | NA |
| bezafibrate | 2 571 | 0.34 | 66 (11) | 41 | 80 (2 017/2 509) | 8.5 (4.5) | NA |
| fenofibrate | 1 728 | 0.23 | 63 (11) | 38 | 67 (1 126/1 687) | 8.1 (4.7) | NA |
Standard Deviation.
Defined as a seven-digit Anatomical Therapeutic Chemical (ATC) code. The remaining proportions were prescribed from a specialist care setting.
Mean dispensed Daily Defined Dose.
Cytochrome P450 enzyme (CYP) 3A4.
In addition to affect CYP3A4 erythromycin is a potent inhibitor of p-glycoprotein.
Non Applicable.
Variables
We hypothesised that physicians in Sweden would avoid the combined use of statins and drugs that inhibit their metabolism. If so, the odds ratio between the prevalences of interacting drugs to comparator drug users would be lower among patients co-dispensed a statin whose metabolism may be inhibited, similar to a methodology used previously [39]:
 |
Thus, for antibiotics and calcium antagonists, the outcome measures were odds ratios of each of the two types of interacting drugs (erythromycin, verapamil/diltiazem) versus respective comparator drugs (doxycycline, amlodipine/felodipine) in patients co-dispensed interacting statins (simvastatin, atorvastatin) versus patients being unexposed (instead dispensed pravastatin, fluvastatin, rosuvastatin). For fibrates, the outcome measure was odds ratios of gemfibrozil versus fenofibrate/bezafibrate in patients co-dispensed any type of statins. To investigate the effect of statin dose on prescribing patterns, respective outcome variable was split into 3 categories where odds ratios in patients dispensed high and low daily dose statins were compared with a respective reference population. Daily doses for respective drug were estimated by dividing the total amount dispensed daily defined doses (mg) with the number of days included in the study period (n = 122) [40]. High statin daily doses were defined as ≥40 mg for atorvastatin, fluvastatin, pravastatin, and simvastatin and ≥20 mg for rosuvastatin.
In the statistical analysis, factors considered potential effect modifiers were age, gender and medical setting. The variable age was divided into three groups (18–45, 46–64 and ≥65) and, along with the other explanatory variables treated as category variables. Information on medical setting was based on the variable “Prescribers’ working place” in the SPDR and whether the lipid lowering drug was being prescribed from a primary or specialist care unit. Primary care was defined as care provided by health care professionals that often play a role in the local community and act as a first point of consultation for all patients within the health care system. Secondary care was defined as care provided by medical specialists often associated with a hospital such as cardiologists, endocrinologists or other internists.
Regarding the treatment groups airway antibiotics and calcium antagonists, the medical setting was defined according to the place where respective statins were dispensed. In order to be able to categorize the reference group for the fibrates, the medical setting was instead defined from the place which the respective fibrate was dispensed.
In addition to these odds ratios, dispensed Defined Daily Doses (DDD) was estimated for the Swedish population as a whole and in specific subgroups (mean, SD) [40]. Concomitantly dispensed drugs were defined as the occurrence of several unique 7-digit ATC codes within the study period.
Analysis
To study associations between statins and the interacting drugs and to control for potential effect modifiers we used unconditional logistic regression. The associations are presented as odds and odds ratios (OR) with 95% confidence intervals (CI). The departure from 1 (no association) is statistically significant at the 5% level, two-tailed, if the 95% CI does not include 1. All statistical calculations were performed in IBM SPSS Statistics 20.0 (SPSS Inc., Chicago, IL, USA). Two sample t-tests were used to compare different means.
Results
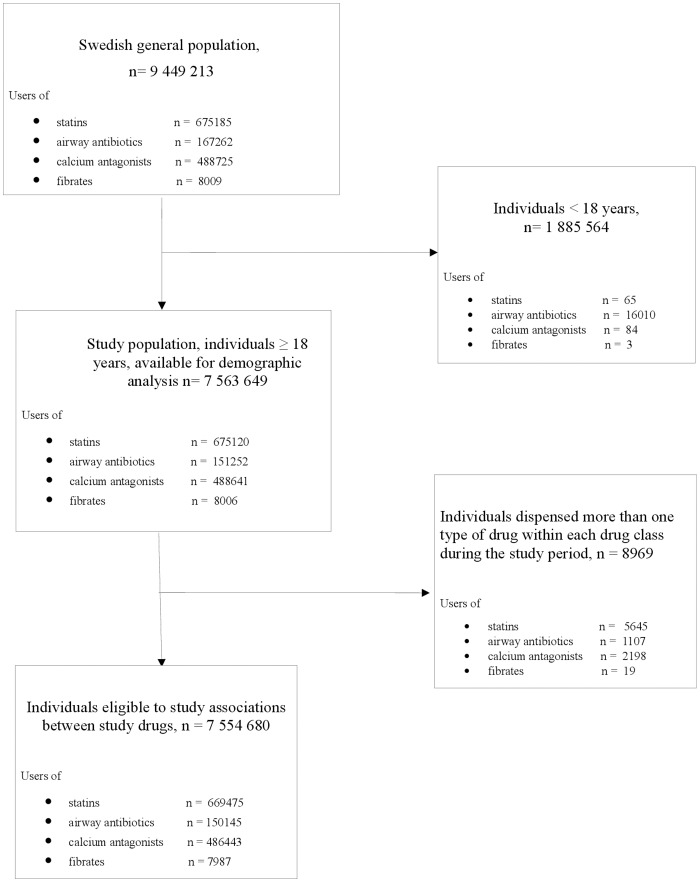
Individuals in the Swedish population 18 years and older (n = 7 563 649) were included in the study [41]. To minimize the possible bias of patients who changed interacting drugs, comparator drugs and/or statins within the 4-month-study period, associations between different classes of drugs was based on the 7 554 680 individuals who had been dispensed no more than one of the drugs in each therapeutic area (e.g. those who had been dispensed both an interacting drug and a comparator drug were excluded) (Figure 1).
Figure 1. Patient flow chart.
The mean age was 49 years, and 51% were women. The prevalence of the use of study drugs in the Swedish study population is given in Table 2 along with corresponding demographics. Nine percent of the population was dispensed any kind of statin where simvastatin was the most common (7%) (Table 2).
Table 3 shows the prevalences of statins dispensed in combination with potentially interacting drugs in patients dispensed high and low doses of statins. The number of patients dispensed simvastatin/atorvastatin in combination with erythromycin and verapamil/diltiazem was in all 520 and 8445 respectively. The number of patients dispensed any statin in combination with gemfibrozil was 1292.
Table 3. Associations between statins, in patients dispensed drugs with or without a pronounced inhibitory effect on their metabolism.
| Statins | Groups ofdispensedstatin dose1 | Interactivedrugs n (%) | Comparator drugsn (%) | OddsInteractive drugs(vs. Comparatordrugs) | Odds ratiosUnadjusted(95% CI2) | p-values | Odds ratios -adjusted forage, gender, andmedical setting(95% CI2) | p-values |
| erythromycin | doxycycline | |||||||
| (n = 576) | (n = 16199) | |||||||
| CYP3A4 3 | High dose | 76 (13) | 2157 (13) | 0.035 | 0.85 (0.60–1.20) | 0.35 | 0.87 (0.60–1.25) | 0.44 |
| interacting statins: | ||||||||
| simvastatin/ | ||||||||
| atorvastatin | ||||||||
| Low dose | 444 (77) | 12697 (78) | 0.035 | 0.84 (0.63–1.12) | 0.23 | 0.92 (0.69–1.23) | 0.56 | |
| Comparator | 56 (10) | 1345 (8) | 0.042 | |||||
| statins: pravastatin/ | ||||||||
| fluvastatin/ | ||||||||
| rosuvastatin | ||||||||
| (reference group) | ||||||||
| verapamil/ | amlodipine/ | |||||||
| diltiazem | felodipine | |||||||
| (n = 9246) | (n = 176168) | |||||||
| CYP3A4 3 interacting | High dose | 1183 (13) | 24130 (14) | 0.046 | 0.59 (0.54–0.65) | <0.001 | 0.62 (0.56–0.68) | <0.001 |
| statins: simvastatin/ | ||||||||
| atorvastatin | ||||||||
| Low dose | 7262 (79) | 142334 (81) | 0.051 | 0.62 (0.57–0.67) | <0.001 | 0.63 (0.58–0.68) | <0.001 | |
| Comparator statins: | 801 (9) | 9704 (6) | 0.083 | |||||
| pravastatin / | ||||||||
| fluvastatin / | ||||||||
| rosuvastatin | ||||||||
| (reference group) | ||||||||
| gemfibrozil | fenofibrate/ | |||||||
| (n = 3712) | bezafibrate | |||||||
| (n = 4275) | ||||||||
| Pharmacokinetic | High dose | 326 (9) | 514 (12) | 0.63 | 0.63 (0.54–0.73) | <0.001 | 0.65 (0.55–0.76) | <0.001 |
| interaction with | ||||||||
| gemfibrozil: any statin | ||||||||
| Low dose | 966 (26) | 1351 (32) | 0.72 | 0.71 (0.64–0.79) | <0.001 | 0.70 (0.63–0.78) | <0.001 | |
| no statin | 2420 (65) | 2410 (56) | 1.00 | |||||
| (reference group) | ||||||||
Data are based on drug dispensing in individuals ≥18 years of age (n = 7 554 680), 15 August to 15 December, 2011.
High statin doses were defined as 40 mg or more for atorvastatin, fluvastatin, pravastatin.
and simvastatin and 20 mg or more for rosuvastatin.
Confidence Intervals.
Cytochrome P450 enzyme (CYP) 3A4.
The associations between interacting drugs and comparator drugs in the population as a whole and in subgroups were consistently investigated in individuals with high and low statin doses. The odds ratio of the interacting erythromycin versus the comparator doxycycline did not differ between patients on interacting and comparator statins either in patients dispensed high or low doses (adjusted OR 0.87; 95% CI 0.60–1.25 and 0.92; 95% CI 0.69–1.23). However, interacting statins were significantly less common among patients dispensed verapamil/diltiazem as compared to patients on comparator drugs amlodipine/felodipine (adjusted OR 0.62; CI 0.56–0.68 and 0.63; CI 0.58–0.68). Similarly, patients on any kind of statin were less likely to be dispensed gemfibrozil as compared to patients not dispensed a statin (adjusted OR 0.65; CI 0.55–0.76 and 0.70; CI 0.63–0.78).
Table 4 shows the adjusted odds ratios between statins in patientś dispensed drugs with or without a pronounced inhibitory effect on their metabolism in primary care settings, specialist care settings, individuals ≥65 years of age, and in females. The results in the investigated subgroups were mostly consistent with those for the general population. However some differences were noted. The decreased association between interacting statins and patients with verapamil/diltiazem was markedly more pronounced in patients treated in specialist care settings (adjusted OR high dose and low dose statins 0.39; CI 0.33–0.46 and 0.39; CI 0.34–0.44) as compared to patients treated in a primary care settings (adjusted OR 0.79; CI 0.70–0.89 and 0.80; CI 0.72–0.88). In females interacting gemfibrozil versus the comparator fenofibrate/bezafibrate did not differ significantly between individuals on any kind of statin and the females that were not dispensed a statin (adjusted OR 0.92; CI 0.68–1.24 and 0.90; CI 0.75–1.08). Among patients 65 years or older, a trend, however not significant, towards a decreased association between interacting statins and patients with erythromycin was noted (adjusted OR 0.70; CI 0.42–1.17 and 0.74; CI 0.50–1.10).
Table 4. Associations between statins, in patientś dispensed drugs with or without a pronounced inhibitory effect on their metabolism in primary care setting, specialist care setting, elderly individuals ≥65 years of age and in females under the study period 15 August to 15 December, 2011.
| Statins | Groups ofdispensedstatindoses1 | Individualsprescribed fromprimary care,adjusted2 odds ratios(95% CI3) | Individualsprescribed fromspecialised care,adjusted2 odds ratios(95% CI3) | Individuals ≥65years(n = 1 779 439),adjusted4 oddsratios (95% CI3) | Females (n = 3 818 524),adjusted5 odds ratios(95% CI3) |
| CYP3A4 6 | High dose | 1.01 (0.64–1.60) | 0.84 (0.53–1.35) | 0.70 (0.42–1.17) | 0.88 (0.52–1.49) |
| interacting statins: | |||||
| simvastatin/ | |||||
| atorvastatin | |||||
| Low dose | 0.97 (0.67 – 1.42) | 0.65 (0.35–1.19) | 0.74 (0.50–1.10) | 1.13 (0.75–1.70) | |
| Comparator statins: | |||||
| pravastatin/ | |||||
| fluvastatin/ | |||||
| rosuvastatin | |||||
| (reference group) | |||||
| CYP3A4 6 | High dose | 0.79 (0.70–0.89) | 0.39 (0.33–0.46) | 0.71 (0.63–0.79) | 0.66 (0.58–0.76) |
| interacting statins: | |||||
| simvastatin/ | |||||
| atorvastatin | |||||
| Low dose | 0.80 (0.72–0.88) | 0.39 (0.34–0.44) | 0.74 (0.67–0.81) | 0.69 (0.62–0.77) | |
| Comparator statins: | |||||
| pravastatin/ | |||||
| fluvastatin/ | |||||
| rosuvastatin | |||||
| (reference group) | |||||
| Pharmacokinetic | Highdose | 0.65 (0.54–0.77) | 0.65 (0.48–0.88) | 0.61 (0.49–0.77) | 0.92 (0.68–1.24) |
| interaction with | |||||
| gemfibrozil: any | |||||
| statin | |||||
| Low dose | 0.71 (0.63–0.80) | 0.68 (0.54–0.86) | 0.75 (0.65–0.86) | 0.90 (0.75–1.08) | |
| no statin | |||||
| (reference group) | |||||
High statin doses were defined as 40 mg or more for atorvastatin, fluvastatin, pravastatin and simvastatin and 20 mg or more for rosuvastatin.
Estimates adjusted for gender and age.
Confidence Intervals.
Estimates adjusted for gender and medical setting.
Estimates adjusted for age and medical setting.
Cytochrome P450 enzyme (CYP) 3A4.
The dispensed volumes of CYP3A4 dependent statins were similar among patients in the two groups of calcium channel blockers (mean DDD: 126, SD: 95) and (mean DDD 126, SD: 91) respectively. In contrast, the mean dispensed DDD (SD) for any statin was substantially higher in patients co-dispensed a fibrate 184 (151) as compared to patients on statin monotherapy 127 (93), (p = <0.001). The dispensed DDD (SD) for any statin in patients dispensed gemfibrozil and fenofibrate/bezafibrate was 178 (149) and 188 (150) respectively. This difference was not statistically significant (p = 0.056). The dispensed volumes of any statin in patients co-dispensed any of the three fibrates and in the subgroup of patients that were co-dispensed gemfibrozil in particular were also investigated in different subgroups. A similar marked increase in mean dispensed DDD was noted for primary care patients (175; SD 142 and 169; SD 142), for specialist care patients, (212; SD 168 and 214; SD 172) among patients 65 years or older (171; SD 138 and 159; SD 123) and in females (172; SD 145 and 162; SD 122).
Discussion
In this population based study we showed that co-administration of statins with calcium channel blockers and fibrates respectively, associated with an increased risk of myopathy, may, to some extent, be avoided in clinical practice. We did not find evidence for avoiding concurrent prescriptions of statins and antibiotics with an increased risk of statin-induced myopathy. Co-prescribing of statins and fibrates, including gemfibrozil, is paradoxically associated with a marked increased statin dose, which further aggravates the risk for dose dependent adverse reactions.
The results should be considered in the context of several limitations. Due to the limited number of patients on statins and different airway antibiotics, the confidence interval around the adjusted odds ratio were actually quite large (adjusted OR in high dose and low dose patients 0.87; 95% CI 0.60–1.25 and 0.92; 95% CI 0.69–1.23). Hence the weak, however not statistically significant association measured, may very well be stronger. Even with similar estimates, the use of a larger study population, for example by using a longer study period including more users of antibiotics, could have turned the noted association significant. Although the data have the advantage of being based on information on dispensed rather than prescribed drugs, it was not possible to ascertain whether the medication was actually consumed. Furthermore, although we were able to adjust for gender and age, information regarding other potentially important confounders was missing. Thus, more detailed information on what the individual choice of lipid lowering therapy was based on such as indication for statin therapy (primary vs. secondary therapy), further cardiovascular risk stratifications (high risk vs. low risk), or presence of contraindications/intolerances, was missing. Another uncertainty about the dispensing data relates to the employment of a fixed time window to estimate the use of drug combinations. Although generally regarded valid, applying a time window may be associated with both under- or overestimation of exposure [42], [43]. The reason for the apparent similar prescription pattern of antibiotics in patients on different statins may, except for lack of knowledge regarding the potential risks of these specific drug-drug interactions, reflect a tendency to prioritize adherence to available guidelines for microbial usage. An alternative way to handle a potential interaction between a statin and a drug used for a shorter period of time may be to instruct the patient to suspend the statin prescription until the interacting prescription is complete. Unfortunately the present methodology using register based dispensing data is unable to evaluate such a strategy and may therefore to some extent have underestimated the clinicians’ ability to avoid this specific group of potential interactions. Furthermore, although excluding some other drugs of importance with respect to statin safety [2], the use of comparator drugs in the two different statins groups also enabled us to control for confounding by indication thus strengthening our conclusions. This approach relies on the assumption that interacting and corresponding comparator drugs, as well as the different statins, are used on similar/identical clinical indications, respectively. However, some differences may exist. Although the four calcium antagonists share the indications for hypertonia and angina pectoris, only verapamil and diltiazem can be prescribed for atrium fibrillation/flutter [35]. The possibility to avoid a potential interaction by switching to an alternative calcium channel blocker may therefore be limited; however, it still leaves the option open to use a statin whose metabolism is independent of CYP3A4.
The results from investigating the population as a whole were mostly consistent when focusing in the two investigated medical settings in the elderly and in females although some differences were noted. The decreased association between interacting statins and patients with verapamil/diltiazem was markedly more pronounced in patients treated in the specialist care as compared to patients treated in the primary care. This may indicate an increased knowledge concerning cardiovascular drug-drug interactions in the specialist care. Due to a decreased clearance resulting in an increased exposure for statins, elderly patients and females are more susceptible for drug interactions that may lead to myopathy [4], [8], [9]. Consequently this group of patients demands a pronounced care when prescribing medications. However, except for an unsignificant trend towards a decreased association between interacting statins and patients with erythromycin in the elderly no such care was noted. In fact, focusing on the females the significant decrease of interacting gemfibrozil in patients co-dispensed statins seen in the general population was lost (adjusted OR high dose and low dose statins 0.92; CI 0.68–1.24 and 0.90; CI 0.75–1.08).
Although there is quite an abundance of data regarding the crude prevalences of drug-drug interactions with a potential to cause myopathy in different contexts [44]–[48] information regarding to what degree clinicians actually avoid these interactions is limited. Ming et al. [44] and Bakhai et al. [45] performed two large nationally representative register based trials on the subject using US administrative/electronic medical records and General Practice Research Database respectively. Using the US administrative records, Ming et al. showed that the proportion of patients prescribed verapamil/diltiazem and macrolides was decreased in patients co-prescribed statins dependent on CYP3A4 for their metabolism as compared to non-3A4 statins (4.3% vs. 4.8% and 2.9% vs. 3.6%) which may indicate some degree of effort to avoid dangerous drug combinations on the behalf of the prescribing physician [44]. According to Bakhai et al. the proportion of verapamil/diltiazem in patients with atorvastatin and simvastatin was decreased as compared to in patients with rosuvastatin, pravastatin and fluvastatin (6.08% and 4.35% vs. 5.80%, 6.66% and 8.14% respectively), data that may point in the same direction [45]. Both studies also provided data on the exposures of a CYP3A4-metabolized statin with a labeled CYP3A4 inhibitor in patients 65 years or older. Thus, Ming et al. found that the prevalence of interactions was in the same level as compared to that of the population as a whole [44]. Bakhai and co-workers noted that for patients 65 years or older, the exposure for CYP3A4 inhibitors of any kind was similar in patients prescribed CYP3A4 statins vs. patients with non-3A4 statins, which resembled the picture seen in the population as a whole [45]. However, as this data was not stratified according to different inhibitors (i.e. calcium antagonists and macrolides) it was not possible to conclude on the age specific effort to avoid dangerous drug combinations in specific therapeutic groups. Devold et al. performed a large scale register study involving the entire Norwegian population that primarily focused on a new reimbursement policy favoring the use of simvastatin [48]. They noted that the reduction in use of statins without a potential to interact from 2004 to 2006 was similar in patients exposed and not exposed to CYP3A4 inhibitors which may indicate a lack of avoidance of statin associated drug interactions [48].
One alternative way of handling a pharmacokinetic interactions between two drugs used for a longer period of time may be to reduce the dose of the drug whose plasma exposure may be elevated. Interestingly, the statin dose in patients that were co-dispensed gemfibrozil was 40% higher than patients on statin monotherapy. This increase was similar when investigated in patients treated in primary care setting (+34%), even more pronounced in the specialist care setting (+69%), and also increased among patients 65 years or older (+25%) and in females (+28%). It is tempting to speculate that his may reflect a clash between safety regulations, that primarily focus on limiting the risk of adverse drug reactions, and clinical guidelines, emphasizing the importance to reach target lipid levels. Among patients that despite an increased statin dose do not reach these targets, a fibrate is added, a trend that may be more pronounced at the specialist care unit. Although this group of patients may very well be at higher risk for cardiovascular diseases, the decision to add gemfibrozil instead of bezafibrate or fenofibrate, without adjusting the statin dose, is unfortunate. Gemfibrozil interacts with statins not only pharmacodynamically but also increases its plasma level 1.5- to 3-fold which can result in plasma levels far exceeding the therapeutic range and an unacceptable benefit – risk balance [25]–[30].
In Sweden, SFINX, a software program used to warn for potential drug-drug interactions provide guidance on how to handle interactions, including the ones studied herein. It is available through either a website solution or as a part of a computerised decision support system (CDSS) that alerts the physician when about to prescribe a potentially inappropriate combination of drugs. This CDSS covers the prescriptions of approximately 80% of Swedish physicians [36], [49]. Apparently the Swedish physicians often fail to take advantage of this tool. Prescribers’ tendency to override DDI alerts is a well known problem described from several clinical contexts [50]–[53]. The present study further emphasizes the need to overcome this barrier.
In conclusion, prescribers may to some extent avoid co-prescription of statins with calcium blockers and fibrates with an increased risk of myopathy. We found no evidence for avoiding co-prescriptions of statins and antibiotics with an increased risk of statin-induced adverse drug reactions. Co-prescription of statins and gemfibrozil is paradoxically associated with a marked increased statin dose, further aggravating the risk for severe myopathy.
Acknowledgments
Dr Anders Håkansson contributed important input regarding the indications for the antibiotics studied.
Funding Statement
This study was has been enabled by grants received by Buster Mannheimer from the Swedish Society for Medical Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manusript.
References
- 2. Neuvonen PJ, Niemi M, Backman JT (2006) Drug interactions with lipid-lowering drugs: mechanisms and clinical relevance. Clin Pharmacol Ther 80: 565–581. [DOI] [PubMed] [Google Scholar]
- 3. Law M, Rudnicka AR (2006) Statin safety: a systematic review. Am J Cardiol 97: 52C–60C. [DOI] [PubMed] [Google Scholar]
- 4. Ronaldson KJ, O'Shea JM, Boyd IW (2006) Risk factors for rhabdomyolysis with simvastatin and atorvastatin. Drug Saf 29: 1061–1067. [DOI] [PubMed] [Google Scholar]
- 5. Jones PH, Davidson MH (2005) Reporting rate of rhabdomyolysis with fenofibrate + statin versus gemfibrozil + any statin. Am J Cardiol 95: 120–122. [DOI] [PubMed] [Google Scholar]
- 6. Cziraky MJ, Willey VJ, McKenney JM, Kamat SA, Fisher MD, et al. (2006) Statin safety: an assessment using an administrative claims database. Am J Cardiol 97: 61C–68C. [DOI] [PubMed] [Google Scholar]
- 7. Armitage J, Bowman L, Wallendszus K, Bulbulia R, Rahimi K, et al. (2010) Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet 376: 1658–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Egger SS, Ratz Bravo AE, Hess L, Schlienger RG, Krahenbuhl S (2007) Age-related differences in the prevalence of potential drug-drug interactions in ambulatory dyslipidaemic patients treated with statins. Drugs Aging 24: 429–440. [DOI] [PubMed] [Google Scholar]
- 9. Schech S, Graham D, Staffa J, Andrade SE, La Grenade L, et al. (2007) Risk factors for statin-associated rhabdomyolysis. Pharmacoepidemiol Drug Saf 16: 352–358. [DOI] [PubMed] [Google Scholar]
- 10. Lennernas H (2003) Clinical pharmacokinetics of atorvastatin. Clin Pharmacokinet 42: 1141–1160. [DOI] [PubMed] [Google Scholar]
- 11. Neuvonen PJ, Kantola T, Kivisto KT (1998) Simvastatin but not pravastatin is very susceptible to interaction with the CYP3A4 inhibitor itraconazole. Clin Pharmacol Ther 63: 332–341. [DOI] [PubMed] [Google Scholar]
- 12. Kantola T, Kivisto KT, Neuvonen PJ (1998) Erythromycin and verapamil considerably increase serum simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther 64: 177–182. [DOI] [PubMed] [Google Scholar]
- 13. Kantola T, Kivisto KT, Neuvonen PJ (1998) Effect of itraconazole on the pharmacokinetics of atorvastatin. Clin Pharmacol Ther 64: 58–65. [DOI] [PubMed] [Google Scholar]
- 14. Jacobson TA (2004) Comparative pharmacokinetic interaction profiles of pravastatin, simvastatin, and atorvastatin when coadministered with cytochrome P450 inhibitors. Am J Cardiol 94: 1140–1146. [DOI] [PubMed] [Google Scholar]
- 15. Bottorff MB (2006) Statin safety and drug interactions: clinical implications. Am J Cardiol 97: 27C–31C. [DOI] [PubMed] [Google Scholar]
- 16. Siedlik PH, Olson SC, Yang BB, Stern RH (1999) Erythromycin coadministration increases plasma atorvastatin concentrations. J Clin Pharmacol 39: 501–504. [PubMed] [Google Scholar]
- 17. Amsden GW, Kuye O, Wei GC (2002) A study of the interaction potential of azithromycin and clarithromycin with atorvastatin in healthy volunteers. J Clin Pharmacol 42: 444–449. [PubMed] [Google Scholar]
- 18. Mousa O, Brater DC, Sunblad KJ, Hall SD (2000) The interaction of diltiazem with simvastatin. Clin Pharmacol Ther 67: 267–274. [DOI] [PubMed] [Google Scholar]
- 19. Azie NE, Brater DC, Becker PA, Jones DR, Hall SD (1998) The interaction of diltiazem with lovastatin and pravastatin. Clin Pharmacol Ther 64: 369–377. [DOI] [PubMed] [Google Scholar]
- 20. Kivisto KT, Kantola T, Neuvonen PJ (1998) Different effects of itraconazole on the pharmacokinetics of fluvastatin and lovastatin. Br J Clin Pharmacol 46: 49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cooper KJ, Martin PD, Dane AL, Warwick MJ, Raza A, et al. (2003) The effect of erythromycin on the pharmacokinetics of rosuvastatin. Eur J Clin Pharmacol 59: 51–56. [DOI] [PubMed] [Google Scholar]
- 22. Saivin S, Houin G (1988) Clinical pharmacokinetics of doxycycline and minocycline. Clin Pharmacokinet 15: 355–366. [DOI] [PubMed] [Google Scholar]
- 23. Nishio S, Watanabe H, Kosuge K, Uchida S, Hayashi H, et al. (2005) Interaction between amlodipine and simvastatin in patients with hypercholesterolemia and hypertension. Hypertens Res 28: 223–227. [DOI] [PubMed] [Google Scholar]
- 24. Katoh M, Nakajima M, Shimada N, Yamazaki H, Yokoi T (2000) Inhibition of human cytochrome P450 enzymes by 1,4-dihydropyridine calcium antagonists: prediction of in vivo drug-drug interactions. Eur J Clin Pharmacol 55: 843–852. [DOI] [PubMed] [Google Scholar]
- 25. Backman JT, Kyrklund C, Kivisto KT, Wang JS, Neuvonen PJ (2000) Plasma concentrations of active simvastatin acid are increased by gemfibrozil. Clin Pharmacol Ther 68: 122–129. [DOI] [PubMed] [Google Scholar]
- 26. Backman JT, Luurila H, Neuvonen M, Neuvonen PJ (2005) Rifampin markedly decreases and gemfibrozil increases the plasma concentrations of atorvastatin and its metabolites. Clin Pharmacol Ther 78: 154–167. [DOI] [PubMed] [Google Scholar]
- 27. Kyrklund C, Backman JT, Kivisto KT, Neuvonen M, Laitila J, et al. (2001) Plasma concentrations of active lovastatin acid are markedly increased by gemfibrozil but not by bezafibrate. Clin Pharmacol Ther 69: 340–345. [DOI] [PubMed] [Google Scholar]
- 28. Kyrklund C, Backman JT, Neuvonen M, Neuvonen PJ (2003) Gemfibrozil increases plasma pravastatin concentrations and reduces pravastatin renal clearance. Clin Pharmacol Ther 73: 538–544. [DOI] [PubMed] [Google Scholar]
- 29. Schneck DW, Birmingham BK, Zalikowski JA, Mitchell PD, Wang Y, et al. (2004) The effect of gemfibrozil on the pharmacokinetics of rosuvastatin. Clin Pharmacol Ther 75: 455–463. [DOI] [PubMed] [Google Scholar]
- 30. Spence JD, Munoz CE, Hendricks L, Latchinian L, Khouri HE (1995) Pharmacokinetics of the combination of fluvastatin and gemfibrozil. Am J Cardiol 76: 80A–83A. [DOI] [PubMed] [Google Scholar]
- 31. Bergman AJ, Murphy G, Burke J, Zhao JJ, Valesky R, et al. (2004) Simvastatin does not have a clinically significant pharmacokinetic interaction with fenofibrate in humans. J Clin Pharmacol 44: 1054–1062. [DOI] [PubMed] [Google Scholar]
- 32. Pan WJ, Gustavson LE, Achari R, Rieser MJ, Ye X, et al. (2000) Lack of a clinically significant pharmacokinetic interaction between fenofibrate and pravastatin in healthy volunteers. J Clin Pharmacol 40: 316–323. [DOI] [PubMed] [Google Scholar]
- 33. Gustavson LE, Schweitzer SM, Koehne-Voss S, Achari R, Chira TO, et al. (2005) The effects of multiple doses of fenofibrate on the pharmacokinetics of pravastatin and its 3alpha-hydroxy isomeric metabolite. J Clin Pharmacol 45: 947–953. [DOI] [PubMed] [Google Scholar]
- 34. Martin PD, Dane AL, Schneck DW, Warwick MJ (2003) An open-label, randomized, three-way crossover trial of the effects of coadministration of rosuvastatin and fenofibrate on the pharmacokinetic properties of rosuvastatin and fenofibric acid in healthy male volunteers. Clin Ther 25: 459–471. [DOI] [PubMed] [Google Scholar]
- 35.FASS (the Swedish Physicians' Desk Reference), publisher: Läkemedelsindustriföreningen (LIF), Available: www.fass.se/LIF/home/index.jsp. Accessed December 2011.
- 36. Bottiger Y, Laine K, Andersson ML, Korhonen T, Molin B, et al. (2009) SFINX-a drug-drug interaction database designed for clinical decision support systems. Eur J Clin Pharmacol 65: 627–633. [DOI] [PubMed] [Google Scholar]
- 37.Marie Eliasson PlPPc (2011) Project leader PASCAL. Personal communication, October, 2011.
- 38. Wettermark B, Hammar N, MichaelFored C, Leimanis A, Otterblad Olausson P, et al. (2007) The new Swedish Prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16: 726–735. [DOI] [PubMed] [Google Scholar]
- 39. Mannheimer B, Wettermark B, Lundberg M, Pettersson H, von Bahr C, et al. (2010) Nationwide drug-dispensing data reveal important differences in adherence to drug label recommendations on CYP2D6-dependent drug interactions. Br J Clin Pharmacol 69: 411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.WHO Guidelines for ATC classification and DDD assignement. Available: www.whocc.no. Accessed December 2011.
- 41.Statistiska Centralbyrån (SCB), Statistics Sweden. Available: http://www.scb.se. Accessed November 2011.
- 42. Bjerrum L, Rosholm JU, Hallas J, Kragstrup J (1997) Methods for estimating the occurrence of polypharmacy by means of a prescription database. Eur J Clin Pharmacol 53: 7–11. [DOI] [PubMed] [Google Scholar]
- 43. Lau HS, de Boer A, Beuning KS, Porsius A (1997) Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol 50: 619–625. [DOI] [PubMed] [Google Scholar]
- 44. Ming EE, Davidson MH, Gandhi SK, Marotti M, Miles CG, et al. (2008) Concomitant use of statins and CYP3A4 inhibitors in administrative claims and electronic medical records databases. J Clin Lipidol 2: 453–463. [DOI] [PubMed] [Google Scholar]
- 45. Bakhai A, Rigney U, Hollis S, Emmas C (2012) Co-administration of statins with cytochrome P450 3A4 inhibitors in a UK primary care population. Pharmacoepidemiol Drug Saf 5: 485–493. [DOI] [PubMed] [Google Scholar]
- 46. Ratz Bravo AE, Tchambaz L, Krahenbuhl-Melcher A, Hess L, Schlienger RG, et al. (2005) Prevalence of potentially severe drug-drug interactions in ambulatory patients with dyslipidaemia receiving HMG-CoA reductase inhibitor therapy. Drug Saf 28: 263–275. [DOI] [PubMed] [Google Scholar]
- 47. Heerey A, Barry M, Ryan M, Kelly A (2000) The potential for drug interactions with statin therapy in Ireland. Ir J Med Sci 169: 176–179. [DOI] [PubMed] [Google Scholar]
- 48. Devold HM, Molden E, Skurtveit S, Furu K (2009) Co-medication of statins and CYP3A4 inhibitors before and after introduction of new reimbursement policy. Br J Clin Pharmacol 67: 234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Eliasson M, Bastholm P, Forsberg P, Henriksson K, Jacobson L, et al. (2006) Janus computerised prescribing system provides pharmacological knowledge at point of care – design, development and proof of concept. Eur J Clin Pharmacol 62: 251–258. [DOI] [PubMed] [Google Scholar]
- 50. Mannheimer B, Ulfvarson J, Eklof S, Bergqvist M, von Bahr C (2008) A clinical evaluation of the Janus Web Application, a software screening tool for drug-drug interactions. Eur J Clin Pharmacol 64: 1209–1214. [DOI] [PubMed] [Google Scholar]
- 51. Glassman PA, Belperio P, Simon B, Lanto A, Lee M (2006) Exposure to automated drug alerts over time: effects on clinicians' knowledge and perceptions. Med Care 44: 250–256. [DOI] [PubMed] [Google Scholar]
- 52. Glassman PA, Simon B, Belperio P, Lanto A (2002) Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med Care 40: 1161–1171. [DOI] [PubMed] [Google Scholar]
- 53. Ahearn MD, Kerr SJ (2003) General practitioners' perceptions of the pharmaceutical decision-support tools in their prescribing software. Med J Aust 179: 34–37. [DOI] [PubMed] [Google Scholar]