Abstract
Background
Peru's HIV epidemic is concentrated among men who have sex with men (MSM). The contribution of alcohol use disorders (AUDs) to known high-risk behaviors associated with HIV transmission in this context has not been well characterized.
Methods
Between June and October 2011, 5,148 sexually active MSM were recruited using convenience sampling in five cities to participate in a cross-sectional bio-behavioral survey. Five high-risk sexual criteria previously associated with incident HIV infection in this setting were selected a priori as the dependent outcomes. Screening for AUDs used the validated Alcohol Use Disorders Identification Test (AUDIT) and AUDS were stratified by severity. Unadjusted and adjusted odds ratios (AOR) were computed to establish the independent correlates of the five dependent outcomes.
Results
The majority (62.8%) of participants met screening criteria for having an AUD, which were independently correlated with each of the following high-risk sexual risk behaviors in the previous 6 months: 1) >5 sexual partners [AOR = 1.76; (1.54–2.02)]; 2) sex with an HIV-infected partner [AOR = 1.29; (1.03–1.62)]; 3) having a sexually transmitted infection [AOR = 1.38; (1.13–1.68)]; 4) being a sex worker [AOR = 1.61; (1.40–1.87)]; and 5) unprotected sex during last encounter [AOR = 1.22; (1.09–1.38)]. Recent drug use was also correlated with having >5 sexual partners [AOR = 1.42 (1.19–1.71)], sex work [AOR = 1.97 (1.63–2.39)] and unprotected sex during last encounter [AOR = 1.31 (1.11–1.54)]. For each dependent variable, the association with AUDs significantly increased with increasing AUD severity.
Conclusions
AUDs are highly prevalent among MSM in Peru and are associated with increased HIV risk-taking behaviors that are associated with HIV transmission. Strategies that target problematic drinking such as medication-assisted therapy, behavioral counseling and structural interventions could potentially reduce risky behaviors and ultimately reduce HIV transmission among MSM in Peru.
Background
While HIV prevalence in Peru remains low at 0.2%, it underestimates the country's concentrated HIV epidemic among men who have sex with men (MSM) [1]. From 1996 to 2002, HIV prevalence from serosurveillance studies among MSM increased from 18.5% to 22.3% in Lima [2]. HIV infection in this group has been associated with homosexual self-identification, high-risk sexual behaviors, cocaine use before or during sex, and sexually transmitted infections (STI) [3]. Nonetheless, the extent to which these risk behaviors are mediated by the disinhibiting use of alcohol and/or other drugs is not well characterized.
Though many studies assessing the association between alcohol use and HIV risk behaviors have been hampered by the use of non-validated measures of alcohol use and non-specific or non-validated definitions of HIV risk that correlate with HIV incidence, they have nevertheless shown correlations with a variety of risky sexual behaviors [4]–[7]. Specifically, global, situational, and to a lesser extent event-level studies in North America and Africa have demonstrated associations between alcohol use and risky sexual behaviors [8]–[12]. International experts have recently called for more comprehensive services for MSM with or at risk for HIV, including screening for and treatment of substance use disorders [13]. The extent to which alcohol consumption meets screening criteria as a treatable alcohol use disorder (AUD) in most available studies has yet to be examined.
The lack of rigorous screening for having an AUD, a chronic and relapsing condition that can be effectively treated using behavioral and/or pharmacological treatments, and its association with validated high-risk sexual behaviors associated with incident HIV infections has yet to be examined globally or even in the Peruvian context.
Methods
Ethics Statement
This research project was approved by the Institutional Review Boards of Impacta, Peru and of Yale University. All procedures were explained to participants, who then read and signed informed consent forms.
Study participants
Between June and October 2011, 5,575 Peruvian MSM were recruited using modified snowball methods and peer-educator outreach in previously mapped venues frequented by MSM in Lima and four other cities: Ica, Piura, Iquitos and Pucallpa. Sample size was large based on calculations of previous HIV prevalence and incidence data. Eligibility included age ≥18, being genetically male, and self-reporting at least one male sexual partner in the previous 12 months.
Study procedures
After informed consent procedures and pre-test HIV counseling, participants underwent HIV and syphilis testing followed by a 45-minute computer-assisted self-administered interview (CASI) assessing sexual risk behaviors and alcohol and drug use. Afterwards, they underwent post-test counseling, receipt of test results and treatment using Peruvian national guidelines.
Variable definitions
The 5 dependent variables, high-risk sexual behaviors associated with incident HIV infection, were decided a priori using the Alaska sexual risk criteria for behaviors during the previous 6 months [14]: 1) having a STI; 2) self-identification as a sex worker; 3) no condom use during last anal intercourse; 4) anal intercourse with more than 5 partners; and 5) being a sexual partner of an HIV-infected male.
AUDs were defined using the World Health Organization's validated 10-item Alcohol Use Disorders Identification Test (AUDIT), validated in Spanish, with standard cut-offs to define any AUD (score ≥8). Participants with AUDs, were further divided into severity levels, including alcohol dependence (score ≥20), harmful drinking (score = 17–19) and hazardous drinking (score = 8–16). Though the AUDIT was initially created as a screening instrument, these AUD cut-offs were subsequently validated for their association with a clinically-defined AUD and the scores have high internal consistency, high sensitivity and specificity and positive predictive value [15]. Other independent variables included “sex work”, defined as receiving money, goods or rent in exchange for sex, “low income”, defined as earning less than the local minimum legal wage (750 Soles/month [$283 US/month]) and “drug use” in the three months prior to the study. Drug use was defined if they injected drugs or reported any use of marijuana, “pasta” or powder cocaine, amphetamines, poppers or ecstasy in the previous 3 months. Unlike the timeframe for the dependent variables (past 6 months), the 3-month time period for drug use was selected in order to allow for comparisons with previous Peruvian HIV Sentinel Surveillance studies.
Data Analyses
Of the 5,575 participants initially recruited, 5,148 (92%) agreed to full participation by completing both HIV testing and the 45-minute behavioral survey. Statistical analyses were performed on this final sample with and complete data using the IBM SPSS Statistics software, version 19. Bivariate logistic regression analyses were conducted to determine associations between each of the 5 dependent high-risk sexual risk behaviors described above with covariates assessing: 1) demographic factors, 2) AUDs and 3) drug use. Covariates significant at p<0.10 were subsequently included in multivariate logistic regression analyses. Non-parametric testing was used for variables that were not normally distributed. Adjusted odds ratios (with 95% confidence intervals) were reported; p<0.05 was deemed statistically significant.
Results
During the 5-month study period, among the 5,148 final study participants, the majority was below 30 years old, earned low incomes and had at least some secondary schooling. Time constraints were the most common reason for survey non-completion. Table 1 summarizes the characteristics of the 5,148 participants with complete data. With regard to sexual orientation, over half (58%) identified themselves as ‘gay’ with the rest identifying as bisexual (30%) or heterosexual (13%). Using standardized screening measures, nearly two thirds (62.8%) of participants met criteria for having an AUD with most of these being in the hazardous drinking category (AUDIT 8–16). Of those meeting AUD screening criteria, 27% had alcohol dependence (AUDIT ≥20).
Table 1. Sociodemographic, alcohol use and sexual behavioral characteristics of the study sample (N = 5148).
| Characteristic | N = 5148 (%) |
| Mean Age (± S.D.a) | 29.5±9 |
| Monthly income | |
| None | 1192 (23.2) |
| Less than minimum legal wageb | 2406 (46.7) |
| Greater than minimum legal wage | 1532 (29.8) |
| Education | |
| Primary or less only | 832 (16.2) |
| Some secondary | 2484 (48.3) |
| Some tertiary | 1820 (35.4) |
| Geographic Distribution | |
| Greater Lima | 2725 (52.9) |
| Iquitos | 608 (11.8) |
| Piura | 594 (11.5) |
| Pucallpa | 604 (11.7) |
| Ica | 601 (11.7) |
| Sexual Orientation (self-defined) | |
| Homosexual (gay) | 2956 (57.4) |
| Bisexual | 1531 (29.7) |
| Heterosexual | 643 (12.5) |
| Transgender | |
| Yes | 700 (13.6) |
| No | 4427 (86.0) |
| Sexual Role | |
| Insertive only | 1990 (38.7) |
| Receptive only | 1756 (34.1) |
| Versatile (both insertive and receptive) | 1380 (26.8) |
| Self-reported sexually transmitted infections (STI) in the prior 12 months | |
| No | 3842 (74.6) |
| Yes (any) | 1289 (25.0) |
| STI in past 6–12 months | 658 (51.0) |
| STI in past 6 months | 631(49.0) |
| Previously tested for HIV | |
| Yes | 3003 (58.3) |
| No | 2123 (41.2) |
| Unprotected sex during past sexual encounter | |
| Yes | 2377 (46.2) |
| No | 2749 (53.4) |
| Any drug use in past 3 months (cocaine, pasta, amphetamines, marijuana, MDMAc, poppers) | |
| Yes | 459 (8.9) |
| No | 4337 (84.2) |
| Alcohol Use Disorders (AUD) | |
| No AUD or social drinking | 1879 (36.5) |
| Any AUD | 3233 (62.8) |
| Hazardous Use | 1905 (58.9) |
| Harmful Use | 468 (14.5) |
| Dependent Use | 860 (26.6) |
Percentages of non-missing data are shown.
S.D. = Standard Deviation.
Minimum legal wage in Peru: 750 Soles/month (US $283/month).
MDMA = 3,4-methylenedioxy-N-methylamphetamine (Ecstasy).
Bivariate sex-risk correlates of alcohol use disorders
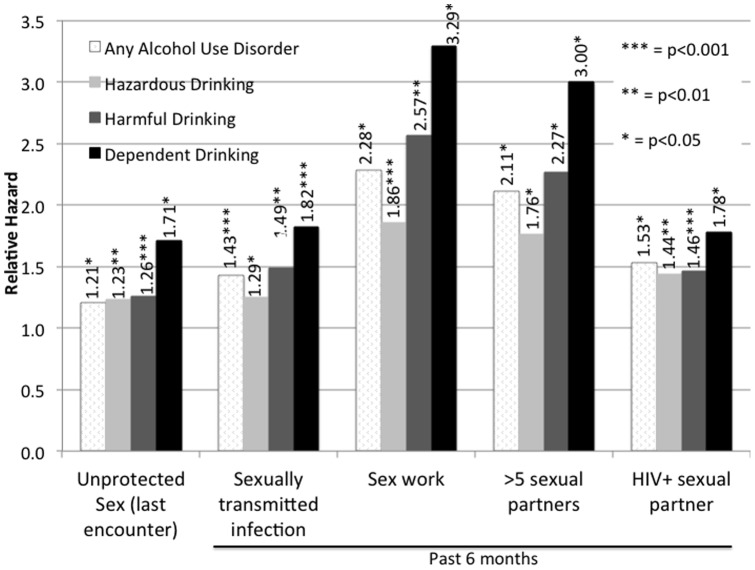
Figure 1 depicts the extent to which any AUD (AUDIT ≥8), stratified by hazardous, harmful, or dependent drinking, was associated with each of the five dependent high-risk behaviors in the bivariate analysis. Importantly, having an AUD was independently associated with each of the five high-risk behaviors, with the strongest associations observed for those who had increased AUD severity and: a) were sex workers or b) had >5 male sexual partners in the previous 6 months. Sex workers and participants with multiple partners in the previous six months were more than twice as likely to have an AUD compared to participants who did not engage in sex work or who had fewer sexual partners, respectively. Strikingly, for all 5 dependent variables, the associations with AUDs incrementally increased with higher levels of AUD severity (hazardous<harmful<dependent drinking). For example, participants reporting more than 5 male partners had 1.8, 2.3 and 3.0-fold higher odds of being hazardous, harmful and dependent alcohol drinkers, respectively, compared to those without an AUD.
Figure 1. Bivariate correlation between alcohol use disorders and alcohol use severity and high-risk HIV risk behaviors.
Bivariate and Multiple Logistic Regression Associations with High Risk Behaviors
Table S1 provides extensive details for model building through inclusion of bivariate and multivariate modeling for each of the five dependent HIV-related risk behaviors. Specifically, bivariate analysis demonstrated significant correlations between all the dependent variables and AUDs, sex work, bisexual orientation, transgender identity, receptive anal intercourse and living outside Lima. The strongest correlates of having >5 sexual partners were being involved in sex work and having an AUD, while the strongest correlate of having an HIV-infected partner was heterosexual self-identification. Sex workers were more likely to identify as transgendered compared to participants who did not engage in sex work. Sex workers and transgendered participants were less likely to engage in unprotected sex during their last sexual encounter, with unadjusted odds ratios of 0.86 and 0.64 respectively. Though recent drug use was less commonly reported, it also correlated with three of the dependent variables: 1) having >5 sexual partners [AOR = 1.42 (1.19–1.71)]; 2) sex work [AOR = 1.97 (1.63–2.39)]; and 3) unprotected sex during last encounter [AOR = 1.31 (1.11–1.54)].
Table 2 summarizes the final multiple regression findings from Table S1 for each of the 5 high-risk behavior outcomes. After construction of the multivariate logistic regression models, meeting screening criteria for having an AUD remained the only covariate significantly associated with all 5 dependent high-risk behaviors. Recreational drug use independently correlated with three of the five high-risk behaviors and was most strongly associated with being a sex worker.
Table 2. Correlates of HIV-related risk behaviors associated with HIV transmission (N = 5,148).
| Covariates | Adjusted Odd Ratios (95% Confidence Intervals) for dependent variables | ||||
| >5 sexual partners | HIV-infected partner | STI | Sex work | Unprotected sex (last encounter) | |
| Any alcohol use disorder | 1.76 (1.54–2.02) *** | 1.29 (1.03–1.62)* | 1.38 (1.13–1.68)** | 1.61 (1.40–1.87) *** | 1.22 (1.09–1.38) *** |
| Any recent drug use | 1.42 (1.19–1.71) *** | 1.04 (0.80–1.36) | -γ | 1.97 (1.63–2.39) *** | 1.31 (1.11–1.54) *** |
| Client of sex worker | 1.54 (1.29–1.84) *** | 1.33 (1.03–1.74)* | 1.15 (0.91–1.46) | 2.90 (2.41–3.50) *** | -γ |
| Salary above minimum wage | 1.43 (1.25–1.64) *** | 1.45 (1.17–1.79) *** | 1.23 (1.02–1.49)* | 0.91 (0.78–1.06) | -γ |
| Bisexual or heterosexual | 0.85 (0.72–1.01) | 2.41 (1.85–3.14) *** | 0.90 (0.72–1.14) | 1.79 (1.53–2.09) *** | 0.90 (0.78–1.04) |
| Transgender | 1.47 (1.21–1.78) *** | 0.77 (0.52–1.13) | -γ | 4.0 (3.27–4.89) *** | 0.72 (0.60–0.86) *** |
| Receptive/versatile sexual role | 1.34 (1.14–1.58) *** | 0.83 (0.64–1.06) | 1.32 (1.04–1.67)* | -γ | 0.71 (0.61–0.82) *** |
| Resident of Lima (capital) | 0.80 (0.71–0.91) *** | 0.87 (0.71–1.07) | 0.61 (0.51–0.73) *** | 0.65 (0.57–0.75) *** | 0.85 (0.76–0.96)** |
| >30 years old | -γ | -γ | 0.72 (0.59–0.88) *** | 0.61 (0.52–0.71) *** | 0.9 (0.8–1.01) |
| >5 sexual partners | N/A | -γ | 1.30 (1.08–1.57)** | 2.71 (2.36–3.12) *** | -γ |
| HIV-infected partner | -γ | N/A | -γ | 1.37 (1.10–1.72)** | -γ |
| STI | 1.30 (1.08–1.57)** | -γ | N/A | 1.32 (1.08–1.62)** | -γ |
| Sex work | 2.67 (2.33–3.07) ** | 1.38 (1.10–1.72)** | 1.31 (1.08–1.60)* | N/A | 0.81 (0.72–0.92) *** |
| Unprotected sex (last encounter) | -γ | -γ | -γ | 0.81 (0.70–0.93)** | N/A |
p<0.001; **p<0.01; *p-value<0.05.
Was not included in multivariate analysis.
Discussion
To our knowledge, this study is the first to examine the prevalence of AUDs among Peruvian MSM using the AUDIT, which has been internationally validated for distinguishing between the various levels of severity of AUDs and assessed them in relationship to risk behaviors associated with HIV transmission. Our study confirms findings from a recent cross-sectional study of Peruvian MSM that documents a high prevalence of alcohol-related problems, but which used the CAGE questionnaire. Their study, unlike ours, found problem drinking to be associated with previous sexual coercion, alcohol consumption during recent sex, sex work and self-reported HIV+ status [6]. In that study, unlike ours, they assessed the correlates of “problematic drinking” and not the association of alcohol consumption specifically on HIV risk behaviors associated with HIV transmission.
Though AUDs vary in severity, our assessment that deployed an internationally-validated screening instrument demonstrates that the prevalence of AUDs is extremely high in this population with nearly two thirds (62.8%) of participants meeting screening criteria for having an AUD. Over a third (37%) met criteria for hazardous drinking (binge drinking), which despite being the least severe type of AUD, remains highly problematic because of the increased likelihood for progression over time to harmful drinking or alcohol dependence. Hazardous drinking necessitates, at a minimum, counseling with the recommendation to reduce drinking linked to provision of educational materials that not only provide information about alcohol's potential for harm to the patient and to others, but motivation to reduce heavy drinking due to the increased likelihood of progressing toward more severe AUDs. For HIV prevention purposes, reducing the progression to alcohol dependence, or more severe drinking, would likely be associated with decreased HIV risk behaviors since heavy drinking days are associated with increased risk-taking [16]. Those meeting screening criteria for harmful drinking should likewise undergo counseling content similar to that for hazardous drinking, but would also require additionally monitoring and ongoing counseling. The interventions for hazardous and harmful drinking can be brief and may take various forms, ranging from providing 5 minutes of counseling about cutting down on drinking, to several brief sessions, depending on the severity of alcohol consumption and its effect on health, legal or social problems. At a minimum, the AUDIT creators suggest that the content of counseling sessions: (i) present screening results; (ii) identify risks and discuss consequences; (iii) provide medical advice; (iv) solicit patient commitment; (v) identify specific goals, specifically reduced drinking or abstinence; and (vi) give advice and encouragement [17].
Alcohol intoxication and drug use increases sexual risk behaviors via various mechanisms including drinking environments, expectancies about its sexual enhancement, its neurocognitive effects and associated poor decision-making [12]. Within MSM communities, the association between alcohol and/or drug use and sex may be even more pronounced for a number of reasons. First, gay bars have historically been among the few safe gathering spaces for MSM, functioning in some cases as “de facto community centers” [18]. Second, disinhibiting substances may help overcome the taboo associated with stigmatizing behaviors. Finally, men whose first MSM sexual encounter that involved alcohol or drugs are more likely to continue using them in subsequent sexual encounters [18]. Equally disturbing is the high proportion of participants (16.7%) meeting screening criteria for alcohol dependence, over 50% higher than the 10% prevalence reported in the general Peruvian population in 2002, using the 9th Edition of the World Health Organization's International Classification of Diseases criteria (ICD-9) for alcohol dependence [19].
Central to our study was that the presence of AUDs was significantly associated with all five high risk behaviors assessed in our survey, based on the Alaska sexual risk criteria, that have been associated with HIV transmission [14]. Specifically, AUDs were associated with: 1) having more than five sexual partners; 2) unprotected sex during last sexual encounter; 3) having a STI; 4) commercial sex work; and 5) sex with an HIV-infected partner – in the previous six months. Moreover, there was an increasing linear association between AUD severity level and all of these outcomes.
The association of high-risk sexual behaviors and AUDs has important implications for HIV prevention. Higher levels of alcohol consumption, beyond “sensible drinking” criteria, is associated with social and sexual disinhibition, including decreased condom use [20]–[23]. Effective treatment of AUDs would likely significantly reduce sexual risk behaviors and ultimately HIV transmission. A number of studies have shown that behavioral interventions to reduce alcohol consumption alone have a small or negligible effect; the most effective method to treat AUDs is treatment with medication-assisted therapies [24]. Though it is seductive to speculate that the disinhibiting effects of alcohol directly cause the high risk-taking behaviors observed in this sample, but the cross-sectional nature of this study only allows us to examine the strength of such associations without proving causality. Event-level granularity that establishes concurrency between alcohol use and risky behaviors, however, is needed to determine if it is the disinhibiting effects of alcohol or, alternatively, unique personality traits, that directly contribute to increased sexual risk [25], [26]. Specifically, personality traits associated with sexual adventurism have been independently associated with lack of condom use and alcohol abuse, but not all individuals who are sexually adventurous use alcohol or drugs [27], [28]. Disentangling causality would therefore better inform interventions for MSM because the type of intervention needed would differ significantly between those whose sexual risk is preceded by alcohol use versus others whose personality traits lead to sexual adventurism [25].
The independent association between AUDs and having had a recent STI is of interest. The presence of STIs, especially ulcerative ones, facilitates HIV transmission [29]. Since the presence of STIs is an indicator of high-risk behaviors in general [30] and AUDs in our sample were associated with recent STIs, there is an urgent need to screen simultaneously for AUDs and acute HIV infection (AHI) among MSM presenting to STI clinics. This is particularly relevant since AHI is associated with high levels of onward HIV transmission since viral replication is inordinately high [31] and the presence of AUDs is associated with disinhibition and sexual risk.
Interestingly, having an AUD was one of the strongest correlates for engaging in sex work. Among the transgendered community in Peru, many transgendered women are involved in sex work [32]. Many sex workers admit to consuming increased levels of alcohol during their sexual encounters with clients, upon the insistence of their clients. Additionally sex workers often recruit clients in nightlife venues where drinking is prevalent. The more time a sex worker spends in such venues, the more likely they are to engage clients. Increased time in these settings, however, potentially results in increased time consuming alcohol [33].
Independent from having an AUD, drug use was associated with three of the five high-risk HIV behaviors, with the exception of having recently had a STIs or sex with a known HIV-infected partner. These data are consistent with prior studies documenting a relationship between drug use and risky sex among MSM [26], [34]. It should be noted, however, that the prevalence of drug use by participants in this study was 6 times lower than the prevalence of AUDs. In our study, less than 9% of subjects had used drugs, primarily marijuana and inhaled, sniffed and “pasta” (free-based” cocaine). These data are distinct from North American MSM, who report high levels of drug use, especially club drugs that are associated with high HIV risk behaviors [35]. Our findings confirm the high prevalence of alcohol use from a recent trial that included MSM from Peru and the U.S. where 52% of Peruvian MSM reported high levels of alcohol use during sex while only 5% reported concomitant drug use. Among U.S. MSM in the same study, equal proportions reported drug and alcohol use (39% and 38%, respectively) [36]. So, while it is important to design risk reduction intervention strategies aimed at lowering drug use, such strategies should be specifically targeted at the small subset of MSM that use drugs. Problematic alcohol use, on the other hand, is more widespread among MSM and in addition to individual-level interventions, should simultaneously be addressed as part of national HIV prevention interventions, including structural interventions that target the setting [37].
In light of the associations between AUDs and sexual risk behaviors, HIV risk reduction interventions should be developed to address not only sexual behavioral risks, but also alcohol consumption. Whereas current HIV prevention strategies do not ignore alcohol problems, most address it in a limited manner. It is therefore possible that problematic alcohol use negatively interferes with current evidence-based HIV prevention interventions that don't address alcohol problems. A multisite HIV Prevention Trials Network study that aimed to address alcohol use in the context of HIV risk behavior found that participants who showed signs of problematic alcohol use one year following the completion of alcohol use reduction interventions were more likely to relapse to having unprotected sex with multiple partners compared with those who remained completely alcohol-free after completing the intervention [38].
Given that a significant proportion of participants scored 20 or higher on the AUDIT, suggestive of meeting criteria for alcohol dependence, they should be referred to a specialist for diagnostic evaluation and treatment for dependent alcohol use, which can be effectively treated using evidence-based practices. Three medications are approved for the treatment of AUDs, including disulfiram, acamprosate [24] and both the oral and extended-release formulation of naltrexone. Disulfuram, through inhibition of aldehyde dehydrogenase, causes acute sickness (e.g., aversion therapy through flushing, nausea, headache, sweating, weakness, increased blood pressure) when alcohol is ingested and does not reduce craving. It should be reserved only for highly motivated patients whose medication adherence is strictly observed. Both acamprosate and naltrexone reduce craving. In a large multisite trial, however, the use of naltrexone was superior to acamprosate either alone or in combination with weekly cognitive behavioral counseling sessions or combined with acamprosate [39]. Naltrexone reduces relapse to heavy alcohol use by blocking opioid receptors in the mesolimbic reward pathway that become activated by ethanol such that the pleasure-response associated with drinking (“the buzz”) is blunted. Alternatively, acamprosate works through a different mechanism involving modulation and/or normalization of alcohol-disrupted brain activity, particularly in the GABA and glutamate neurotransmitter systems. If naltrexone proves to be effective at lowering the levels of heavy drinking days among Peruvian MSM, it has the potential to reduce HIV risk behaviors as well as improve ART adherence for HIV-infected individuals with AUDs, and ultimately decreasing community-wide HIV transmission [4].
Though the findings from this study have important implications for HIV prevention among Peruvian MSM with AUDs, and perhaps all MSM with AUDs, there are some methodological limitations. Convenience samples recruited through a non-statistically determined referral chain mechanism may result in a non-representative sample of Peruvian MSM. Though the large sample size, multisite recruitment of this sample and similar findings from a previous population-based study showing that the majority of MSM (over 90%) had been to a gay bar in the previous 6 months [20] may, in part, decrease these concerns, it is critical to note that our sample is not necessarily representative of all MSM. Our study was cross-sectional, only allowing us to demonstrate high correlation, but not causality. Last, our study relied on self-report for alcohol and drug use and sexual risk behaviors. While concerns about social desirability response for culturally stigmatizing drug and alcohol use and sexual risk behaviors may result in under-reporting, the use of the anonymous CASI assessment and the remarkably high responses to these questions reduce these concerns. Notwithstanding these limitations, the large sample size and consistent and strong correlation between AUDs and drug use and validated sexual risk behaviors associated with HIV transmission suggest a relationship that is worthy of future intervention.
Conclusions
The prevalence of AUDs is high among MSM in Peru and associated with increased levels of HIV risk-taking behaviors. The increasing severity of AUDs is associated with the increasing likelihood that MSM engage in high-risk behaviors that can result in HIV transmission. These findings may, in part, explain the continued concentrated HIV epidemic among MSM and have important implications for HIV prevention, diagnosis and entry into and retention in care. These individuals would greatly benefit from strategies that reduce problematic drinking, including medication-assisted therapy, behavioral counseling and structural interventions.
Supporting Information
Correlates of HIV-related risk behaviors associated with HIV transmission.
(DOCX)
Acknowledgments
The authors gratefully acknowledge the subjects who gave their time to participate in this study, as well as the staff at Impacta and all other participating organizations and health centers throughout Peru for their involvement and dedication to the study.
Funding Statement
This work was supported by the Asociacion Civil Impacta Educacion y Salud, Peru; career development grants from the National Institute on Drug Abuse (K24 DA017072, FLA); research grants from the National Institute on Drug Abuse (R01 DA032106, FLA and PV); the Downs International Health Student Travel Fellowship (Yale University, KTL); the Infectious Diseases Society of America Education and Research Foundation Medical Scholars Program (KTL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Carcamo CP, Campos PE, Garcia PJ, Hughes JP, Garnett GP, et al. (2012) Prevalences of sexually transmitted infections in young adults and female sex workers in Peru: a national population-based survey. Lancet Infect Dis 12: 765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sanchez J, Lama JR, Kusunoki L, Manrique H, Goicochea P, et al. (2007) HIV-1, sexually transmitted infections, and sexual behavior trends among men who have sex with men in Lima, Peru. J Acquir Immune Defic Syndr 44: 578–585. [DOI] [PubMed] [Google Scholar]
- 3. Lama JR, Lucchetti A, Suarez L, Laguna-Torres VA, Guanira JV, et al. (2006) Association of herpes simplex virus type 2 infection and syphilis with human immunodeficiency virus infection among men who have sex with men in Peru. J Infect Dis 194: 1459–1466. [DOI] [PubMed] [Google Scholar]
- 4. Azar MM, Springer SA, Meyer JP, Altice FL (2010) A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug and alcohol dependence 112: 178–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Celentano DD, Valleroy LA, Sifakis F, Mackellar DA, Hylton J, et al. (2006) Associations between substance use and sexual risk among very young men who have sex with men. Sexually transmitted diseases 33: 265–271. [DOI] [PubMed] [Google Scholar]
- 6.Deiss RG, Clark JL, Konda KA, Leon SR, Klausner JD, et al.. (2013) Problem drinking is associated with increased prevalence of sexual risk behaviors among men who have sex with men (MSM) in Lima, Peru. Drug Alcohol Depend. [DOI] [PMC free article] [PubMed]
- 7. Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, et al. (2004) Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. Journal of Studies on Alcohol 65: 434–442. [DOI] [PubMed] [Google Scholar]
- 8. Fisher JC, Bang H, Kapiga SH (2007) The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis 34: 856–863. [DOI] [PubMed] [Google Scholar]
- 9. George WH, Stoner SA (2000) Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res 11: 92–124. [PubMed] [Google Scholar]
- 10. Hendershot CS, Stoner SA, Pantalone DW, Simoni JM (2009) Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr 52: 180–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA (2004) Substance use and high-risk sex among men who have sex with men: a national online study in the USA. AIDS Care 16: 1036–1047. [DOI] [PubMed] [Google Scholar]
- 12. Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S (2007) Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci 8: 141–151. [DOI] [PubMed] [Google Scholar]
- 13. Beyrer C, Sullivan PS, Sanchez J, Dowdy D, Altman D, et al. (2012) A call to action for comprehensive HIV services for men who have sex with men. Lancet 380: 424–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sanchez J, Lama JR, Peinado J, Paredes A, Lucchetti A, et al. (2009) High HIV and ulcerative sexually transmitted infection incidence estimates among men who have sex with men in Peru: awaiting for an effective preventive intervention. J Acquir Immune Defic Syndr 51 Suppl 1S47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro M (2001) AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization.
- 16.Mimiaga MJ, Biello KB, Sivasubramanian M, Mayer KH, Anand VR, et al.. (2013) Psychosocial risk factors for HIV sexual risk among Indian men who have sex with men. AIDS Care. [DOI] [PMC free article] [PubMed]
- 17.World Health O (2001) The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care.
- 18. Stall R, Purcell DW (2000) Intertwining Epidemics: A Review of Research on Substance Use Among Men Who Have Sex with Men and Its Connection to the AIDS Epidemic. AIDS and Behavior 4: 181–192. [Google Scholar]
- 19.DEVIDA (2006) Comision Nacional para el Desarrollo y Vida sin Drogas. Encuesta Nacional de Consumo de Drogas en la Poblacion General de Peru.
- 20. Celentano DD, Valleroy LA, Sifakis F, MacKellar DA, Hylton J, et al. (2006) Associations between substance use and sexual risk among very young men who have sex with men. Sex Transm Dis 33: 265–271. [DOI] [PubMed] [Google Scholar]
- 21. Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, et al. (2004) Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. J Stud Alcohol 65: 434–442. [DOI] [PubMed] [Google Scholar]
- 22. Weinhardt LS, Carey MP (2000) Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res 11: 125–157. [PMC free article] [PubMed] [Google Scholar]
- 23. Woolf SE, Maisto SA (2009) Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav 13: 757–782. [DOI] [PubMed] [Google Scholar]
- 24. Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH (2010) Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet 376: 367–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Difranceisco W, Ostrow DG, Chmiel JS (1996) Sexual adventurism, high-risk behavior, and human immunodeficiency virus-1 seroconversion among the Chicago MACS-CCS cohort, 1984 to 1992. A case-control study. Sex Transm Dis 23: 453–460. [DOI] [PubMed] [Google Scholar]
- 26. Heath J, Lanoye A, Maisto SA (2012) The role of alcohol and substance use in risky sexual behavior among older men who have sex with men: a review and critique of the current literature. AIDS Behav 16: 578–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kippax S, Campbell D, Van de Ven P, Crawford J, Prestage G, et al. (1998) Cultures of sexual adventurism as markers of HIV seroconversion: a case control study in a cohort of Sydney gay men. AIDS Care 10: 677–688. [DOI] [PubMed] [Google Scholar]
- 28. Leobon A, Velter A, Engler K, Drouin MC, Otis J (2011) A relative profile of HIV-negative users of French websites for men seeking men and predictors of their regular risk taking: a comparison with HIV-positive users. AIDS Care 23: 25–34. [DOI] [PubMed] [Google Scholar]
- 29. Wasserheit JN (1992) Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis 19: 61–77. [PubMed] [Google Scholar]
- 30. Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, et al. (2005) Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health 82: 312–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marks G, Crepaz N, Senterfitt JW, Janssen RS (2005) Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr 39: 446–453. [DOI] [PubMed] [Google Scholar]
- 32. Silva-Santisteban A, Raymond HF, Salazar X, Villayzan J, Leon S, et al. (2012) Understanding the HIV/AIDS epidemic in transgender women of Lima, Peru: results from a sero-epidemiologic study using respondent driven sampling. AIDS Behav 16: 872–881. [DOI] [PubMed] [Google Scholar]
- 33. Luchters S, Geibel S, Syengo M, Lango D, King'ola N, et al. (2011) Use of AUDIT, and measures of drinking frequency and patterns to detect associations between alcohol and sexual behaviour in male sex workers in Kenya. BMC Public Health 11: 384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, et al. (2011) HIV risk, prevention, and testing behaviors among men who have sex with men – National HIV Behavioral Surveillance System, 21 U.S. cities, United States, 2008. MMWR Surveill Summ 60: 1–34. [PubMed] [Google Scholar]
- 35. Pappas MK, Halkitis PN (2011) Sexual risk taking and club drug use across three age cohorts of HIV-positive gay and bisexual men in New York City. AIDS Care 23: 1410–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jacob ST, Baeten JM, Hughes JP, Peinado J, Wang J, et al. (2011) A post-trial assessment of factors influencing study drug adherence in a randomized biomedical HIV-1 prevention trial. AIDS Behav 15: 897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Blankenship KM, Bray SJ, Merson MH (2000) Structural interventions in public health. AIDS 14: S11–S21. [DOI] [PubMed] [Google Scholar]
- 38. Koblin B, Chesney M, Coates T (2004) Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet 364: 41–50. [DOI] [PubMed] [Google Scholar]
- 39. Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, et al. (2006) Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 295: 2003–2017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Correlates of HIV-related risk behaviors associated with HIV transmission.
(DOCX)