Abstract
Objective
Globally 40% of deaths to children under-five occur in the very first month of life with three-quarters of these deaths occurring during the first week of life. The promotion of delivery with a skilled birth attendant (SBA) is being promoted as a strategy to reduce neonatal mortality. This study explored whether SBAs had a protective effect against neonatal mortality in three different regions of the world.
Methods
The analysis pooled data from nine diverse countries for which recent Demographic and Health Survey (DHS) data were available. Multilevel logistic regression was used to understand the influence of skilled delivery on two outcomes – neonatal mortality during the first week of life and during the first day of life. Control variables included age, parity, education, wealth, residence (urban/rural), geographic region (Africa, Asia and Latin America/Caribbean), antenatal care (ANC) and tetanus immunization.
Results
The direction of the effect of skilled delivery on neonatal mortality was dependent on geographic region. While having a SBA at delivery was protective against neonatal mortality in Latin America/Caribbean, in Asia there was only a protective effect for births in the first week of life. In Africa SBAs were associated with higher neonatal mortality for both outcomes, and the same was true for deaths on the first day of life in Asia.
Conclusion
Many women in Africa and Asia deliver at home unless a complication occurs, and thus skilled birth attendants may be seeing more women with complications than their unskilled counterparts. In addition there are issues with the definition of a SBA with many attendants in both Africa and Asia not actually having the needed training and equipment to prevent neonatal mortality. Considerable investment is needed in terms of training and health infrastructure to enable these providers to save the youngest lives.
Keywords: antenatal care, early neonatal mortality, health systems strengthening, scale-up and skilled birth attendant
Introduction
Millennium Development Goal (MDG) 4 aims to reduce under-five mortality by two-thirds from the baseline year 1990 to 2015. Deaths in the first month of life, the neonatal period, account for over 40 percent of all deaths among children under-five years of age (1,2), resulting in a staggering 2.76 million deaths each year (3). The vast majority of these deaths occur in low and middle income countries. Both under-five mortality and late-neonatal mortality have slowly improved in many areas of the world, however there has been little measurable decline for deaths in the first week of life (4,5). Globally three-quarters of neonatal deaths occur during the first week of life, and within the first week of life, the first day of life is a particularly vulnerable period (5–7). In different setting up to half of neonatal deaths occur during the very critical first day of life (8). In order to achieve MDG-4 it is imperative that early neonatal deaths are prevented.
The main causes of neonatal mortality are pre-term birth (35%), intrapartum-related/birth asphyxia (22.5%), sepsis or meningitis (12.5%), congenital abnormalities (10%), pneumonia (10%) tetanus (2.5%), diarrhea (2.5%) and nonspecific causes (5%) (1). Neonatal deaths occur most frequently in the homes of women from the poorest regions of south Asia and sub-Saharan Africa (4, 9, 10). More than half of newborns who die, do so at home (4, 11). Darmstadt et al. estimated that between 41% and 72% of neonatal deaths could be prevented through the universal implementation of 16 simple and cost-effective interventions (12). The promotion of delivery with a skilled birth attendant (SBA) is one strategy to provide several of these interventions. A SBA is defined by the World Health Organization (WHO) as an individual trained to proficiency in the skills needed to manage normal pregnancy, childbirth and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns (13). By providing clean delivery practices, labor surveillance, neonatal resuscitation to address intrapartum-related birth asphyxia and treatment of infections, a properly trained SBA could reduce mortality that occurs during labor, delivery and shortly after birth. Intrapartum-related birth asphyxia and sepsis alone account for 57.5% of neonatal deaths, and intrapartum related birth asphyxia is also a leading cause of stillbirths. Darmstadt et al. estimated great reductions in neonatal mortality for intrapartum-related interventions such as corticosteroids for pre-term labor (40% reduction), caesarian section for breech position (70% reduction), labor surveillance for diagnosis of a complication (40%) and clean delivery practices (58–78%) (12). SBAs can provide pregnancy-related care during antenatal care (ANC) visits, including tetanus immunization, provision of iron/folate, detection and management of pre-existing conditions and monitoring for pre-eclampsia - a condition which if left untreated can lead to intrapartum-related neonatal mortality. SBAs can also promote interventions after birth such as kangaroo care and immediate breastfeeding. They can provide postnatal care (PNC) including pneumonia case management and are a crucial element of the continuum of care approach for mothers, newborns and children.
The current definition of a SBA has been critiqued because it does not include an assessment of provider skill. Harvey et al. found provider competence to be low in some areas of maternal and newborn care provision (14). For example, only 46% of providers in the study were competent in the active management of the third stage of labor and only 55% in neonatal resuscitation. In addition cadres of providers varied in their knowledge and skills. In terms of immediate newborn care mean scores were 76.4% for doctors and 67.4% for professional nurses, and for neonatal resuscitation with ambu bag mean scores were 61.6% for doctors and 50.1% for professional nurses. Inadequate obstetric care has been found to be a factor in an audit in Tanzania which found that 66% of neonatal deaths were intrapartum-related and that 80% of deaths occurred to fetuses who were normal birth weight (15). Other studies have found high proportions of neonatal deaths to fetuses that were potentially viable at the beginning of labor (16–18). An evaluation of health worker skills in Pakistan found that all cadres of health workers performed below competency levels for maternal, neonatal and child health knowledge, particularly in neonatal resuscitation and immediate newborn care (19). The current definition of a SBA does not distinguish providers truly skilled to handle complications and those who are not.
The definition of a SBA also does not capture factors associated with the environment in which the providers are working. Inadequate equipment and infrastructure are also barriers in both Africa and Asia. Health facility assessments have shown that in sub-Saharan Africa, only 15% of hospitals are equipped to provide basic neonatal resuscitation (20). A study in Uganda found that less than 15% of facilities had job aids for neonatal resuscitation, and only 16% had a nursery for sick or small babies (21).
This study presents an assessment of whether the presence of a SBA at birth is associated with reduced neonatal mortality using the current definition of a SBA. The objective is to understand how much the promotion of delivery with a skilled birth attendant at their current levels of training and equipment could be expected to reduce neonatal mortality. The study also examines whether associations of skilled birth attendants and neonatal mortality differ by region of the world. This question is important because Africa and Asia generally have weaker health systems and worse health outcomes than Latin America/Caribbean. SBAs must rely on the health facility and more generally the health system in which they work in order to receive training and the necessary supplies to conduct their work.
Methods
Data and sample
This study presents a secondary data analysis which was reviewed and exempted from needing institutional review board (IRB) approval by the University of North Carolina at Chapel Hill. A pooled analysis using Demographic and Health Surveys (DHS) data collected from a diverse set of nine countries was conducted: Bangladesh, Bolivia, Ghana, Haiti, Honduras, Indonesia, Nepal, Uganda, and Zambia. The countries were selected because they had recent data available, represented three different regions of the world and represented diverse levels of socioeconomic development. DHS surveys are nationally representative population-based surveys with large sample sizes (usually between 5,000 and 30,000 households). In all households, women age 15–49 are eligible to participate. The sample is usually based on a stratified two-stage cluster design. The first stage is the sample enumeration area (SEA) or cluster, generally drawn from Census files. In the second stage, within each SEA, a sample of households is selected from an updated list of households. The sample is generally representative at the national level, residence (urban-rural), and regional (departments, states) levels. Women who did not have a live birth within five years prior to the survey were excluded from the analysis. The sample consisted of 53,474 women across the nine countries.
Outcome Variables
The dependent variables were survival status or neonatal mortality on the first day of life and the first week of life for a woman’s most recent live birth.
Skilled Delivery
The key independent variable was whether a woman’s most recent delivery resulting in a live birth was attended by a SBA as defined by the WHO (13). The vast majority of unskilled deliveries occurred in a home environment, and in the Latin American/Caribbean and African countries the vast majority of skilled deliveries occurred in a health facility. In the Asian countries in this sample about 28% of the skilled deliveries occurred in a home environment. Several Asian countries actually promote skilled delivery in either a facility or home environment (when facility delivery is not feasible) (22–24).
Control Variables
The control variables were maternal age in years (15–19, 20–24, 25–34, 35–49), parity (one, two to three, and four or more), education (none, primary, secondary or greater), urban or rural residence, wealth quintile (poorest, second poorest, middle, second richest, richest), receipt of tetanus toxoid before or during pregnancy, and four or more ANC visits. The WHO (25) promotes at least four ANC visits, and women who receive ANC are more likely to have skilled deliveries (26). Dummy variables for region (Africa, Asia and Latin America/Caribbean) were also created.
Analysis
Because the data were clustered within countries, the standard assumption of logistic regression that individual respondents are independent across countries and that there is equal variance across countries did not hold. A multilevel regression framework was needed to account for this clustered data structure.
The analysis proceeded in three steps. First, a null or base model was run including only the dependent variable neonatal mortality in the first week (or on the first day) of life to establish the degree of variance at the country level (in order to validate use of a multilevel framework). Next, the key independent variable skilled delivery, plus a region indicator and a skilled delivery by region interaction term, were added to test for significance of the predictor variable and whether the effect varied by region. Finally, all the individual-level demographic control variables were added to the model in order to account for maternal characteristics known to affect neonatal mortality. Mean model-predicted probabilities of neonatal death in the first week and on the first day of life were then plotted by delivery attendant skill and geographic region. All models were estimated with the gllamm command in Stata MP version 12.1.
Results
Table 1 summarizes the pooled survey sample characteristics. Overall, 48% of deliveries were performed by a skilled birth attendant. Nearly two-thirds of respondents reported having the recommended four or more ANC visits, and approximately 85% reported receiving tetanus toxoid either before or during the most recent pregnancy. Most of respondents were aged 25–34 and multiparous, and over a third reported a secondary or higher level of education. The sample included 36% urban respondents and was roughly evenly distributed across the first four household wealth categories with fewer reporting membership in the highest wealth category. About 44% were from Asia, 35% from Latin America/Caribbean and 21% from Africa. Figure 1 shows the percent of skilled delivery by region. This varied from 63% in the Latin American/Caribbean region to 50% in Africa to 35% in Asia.
Table 1.
Sample characteristics: survey-weighted percentages (n = 53,474)
| Characteristic | Percentage |
|---|---|
| Delivery | |
| Skilled birth attendant present | 48.0 |
| Antenatal | |
| Four or more ANC visits | 65.1 |
| Tetanus toxoid before or during pregnancy | 84.8 |
| Demographic | |
| Age (years) | |
| 15–19 | 7.6 |
| 20–24 | 24.9 |
| 25–34 | 46.3 |
| 35–49 | 21.2 |
| Parity | |
| 1 | 28.2 |
| 2–3 | 40.0 |
| ≥ 4 | 31.9 |
| Education | |
| None | 15.4 |
| Primary | 46.7 |
| Secondary+ | 37.9 |
| Residence | |
| Urban | 35.9 |
| Wealth quintile | |
| Lowest | 22.1 |
| Second | 20.4 |
| Middle | 20.4 |
| Fourth | 19.9 |
| Highest | 17.3 |
| Region | |
| Latin America/Caribbean | 35.0 |
| Africa | 21.4 |
| Asia | 43.6 |
Figure 1.
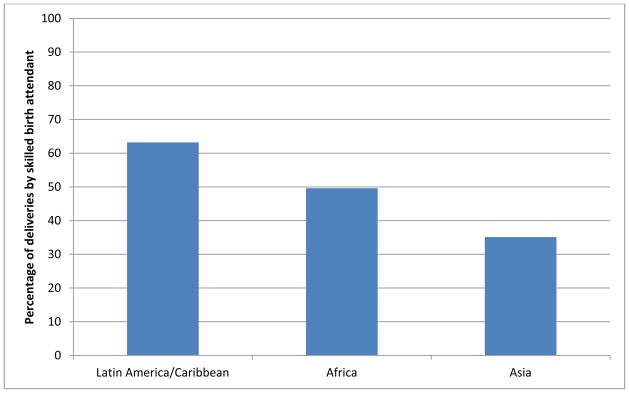
Percent of deliveries by a Skilled Birth Attendant by Region
Table 2 shows that overall there were approximately 12.4 neonatal deaths per 1,000 births or approximately 642 deaths in the first week of life, of which nearly 8 per 1,000 or 408 occurred on the first day of life, with slightly more occurring in the presence of unskilled versus skilled delivery attendants. This differential mortality by skilled delivery was much more prominent in Latin America/Caribbean compared to Asia, and in Africa the relationship between skilled delivery attendance and mortality was reversed. In Africa neonatal mortality was higher in the presence of a SBA. Low and high parity tended to be associated with higher mortality, with no difference by skilled versus unskilled delivery. Similarly, having four or more ANC visits and tetanus toxoid before or during pregnancy were protective.
Table 2.
Survey-weighted neonatal mortality rate (per 1,000) within the first week and on the first day of life, by maternal characteristics and skill of delivery attendant (n = 53,474)
| Characteristic | Skill of Delivery Attendant | Neonatal death rate (per 1,000)
|
|
|---|---|---|---|
| 7 days | 1 day | ||
| Overall | Unskilled | 12.73 | 7.97 |
| Skilled | 11.97 | 7.75 | |
| Region | |||
| Latin America/Caribbean | Unskilled | 16.05 | 9.15 |
| Skilled | 9.20 | 5.33 | |
| Africa | Unskilled | 13.02 | 6.24 |
| Skilled | 19.33 | 13.01 | |
| Asia | Unskilled | 11.11 | 8.09 |
| Skilled | 10.90 | 7.60 | |
| Parity | |||
| 1 | Unskilled | 12.94 | 8.42 |
| Skilled | 12.98 | 8.78 | |
| 2–3 | Unskilled | 10.17 | 6.06 |
| Skilled | 9.18 | 4.99 | |
| ≥ 4 | Unskilled | 15.25 | 9.67 |
| Skilled | 15.12 | 10.80 | |
| ANC visits | |||
| < 4 | Unskilled | 17.21 | 10.75 |
| Skilled | 18.76 | 11.37 | |
| ≥ 4 | Unskilled | 8.48 | 5.32 |
| Skilled | 10.29 | 6.85 | |
| Tetanus toxoid before or during pregnancy | |||
| no | Unskilled | 19.24 | 12.35 |
| Skilled | 12.11 | 7.42 | |
| yes | Unskilled | 11.17 | 6.92 |
| Skilled | 11.96 | 7.79 | |
Table 3 shows the multilevel logistic modeling results for the two outcomes. Compared to unskilled in Latin America/Caribbean, skilled delivery was associated with a 51% increase (OR=1.51) in the probability of death during the first week of life and an 84% increase (OR=1.84) in the probability of death on the first day of life in Africa, controlling for other factors. Compared to unskilled in Latin America/Caribbean there was a 2% reduction (OR=0.98) in the probability of death during the first week of life and a 32% increase (OR=1.32) in the probability of death on the first day of life in Asia, controlling for other factors. As expected, there was a significant protective effect for four or more ANC visits on neonatal mortality during the first week of life (OR = 0.65, 95% CI: 0.47–0.89) and the first day of life (OR = 0.71, 95% CI: 0.52–0.98), or approximately 29% to 35% fewer deaths. Tetanus immunization was not significantly associated with either outcome.
Table 3.
Parameter estimatesa (odds ratio) for multilevel weighted logistic regression models of death in first week and death on the first day of life by skilled delivery attendance, controlling for maternal antenatal and demographic characteristics (N=53,474)
| Death in first weekb OR (95% CI) | Death on first dayb OR (95% CI) | |
|---|---|---|
| Explanatory variables | ||
| Fixed effects | ||
| Delivery attendants’ skills | ||
| Unskilled | 1.00 | 1.00 |
| Skilled | 0.70 (0.46,1.07) | 0.71 (0.36,1.41) |
| Geographic region | ||
| Latin America/Caribbean | 1.00 | 1.00 |
| Africa | 0.87 (0.53,1.45) | 0.72 (0.36,1.42) |
| Asia | 0.79 (0.46,1.38) | 1.06 (0.50,2.26) |
| Delivery by region interaction | ||
| Skilled in Africa | 2.49 (1.42,4.36)** | 3.61 (1.52,8.52)** |
| Skilled in Asia | 1.78 (1.08,2.94)* | 1.76 (0.85,3.65)** |
| Antenatal care | ||
| Tetanus toxoid before/during pregnancy | ||
| No | 1.00 | 1.00 |
| Yes | 0.70 (0.47,1.05) | 0.70 (0.44,1.11) |
| Antenatal visits | ||
| <4 | 1.00 | 1.00 |
| ≥4 | 0.65 (0.47,0.89)** | 0.71 (0.52,0.98)* |
| Random effects | ||
| Country-level variance (SE)c | 0.81 (0.75,0.88)*** | 0.83 (0.75,0.91)*** |
| Log likelihood | −3381.15 | −2325.73 |
| AIC | 6778.3 | 4667.45 |
| Log likelihood Ratio Test (χ2)d | 46.25*** | 54.37*** |
Parameters for predictors (fixed effects) are reported as odds ratio; for random effects, the parameter is the variance
Full model including all demographic control variables: age, parity, education, residence (urban/rural), and wealth quintile.
Significance of random effects evaluated by comparing model with a similar one in which random effects have been constrained to be zero.
Compared to null model with no covariates
p<0.05
p<0.01
p<0.001
The mean model-predicted probabilities of death on the first day and during the first week of life by birth attendant skill level and region are plotted in Figure 2, showing graphically the results discussed above.
Figure 2.
Mean (SD) model-predicted probabilities of neonatal death in the first week and on the first day of life, by delivery attendant skill and region
Conclusion
Three quarters of the estimated 2.76 million child deaths during the first month of life (1, 2) occur in the first week of life with the first day of life being a particularly vulnerable period. (5–8). SBAs performing deliveries in a health facility are a crucial element of a continuum of care approach for mothers and newborns. Properly trained birth attendants have the potential to reduce neonatal mortality through the implementation of relatively simple and cost-effective interventions (27, 28).
Skilled delivery was not associated with reduced neonatal mortality overall, but interaction effects with geographic region were significant. Skilled delivery was protective against neonatal mortality in Latin America/Caribbean which overall has a stronger health infrastructure than both Africa and Asia. Higher proportions of women deliver with a SBA in the Latin American/Caribbean region whereas in some settings in Asia and Africa, women with complications are more likely to seek skilled delivery than those without complications (29–34). In these settings many women have a preference for home births for a variety of reasons and may only present to a facility when a complication has progressed. Unfortunately the DHS data does not capture any information on reported complications.
In addition studies have shown that existing coverage of the simple interventions needed to prevent neonatal morality are low in Asia and Africa (35, 20). Few of these countries have been able to implement the 16 recommended interventions, with the exception of tetanus immunization, at scale (35). Facilities frequently fall short in providing essential newborn care (ENC), which is a set of basic preventive measures including clean delivery, temperature maintenance, eye and cord care and breastfeeding. ENC also includes early detection and treatment of danger signs such as for birth asphyxia and infections. Facilities in these regions are also not keeping pace with the increase in facility-based deliveries (36, 37). Zimba et al (2012) found that while Malawi has increased the percent of skilled deliveries, the majority of women and newborns with complications still lack access to essential services (37). Ali et al. (2005) found the met need for Emergency Obstetric Care (EmOC) was only 9% in Pakistan [38]. A key next step is for countries to focus on and document scale-up so that progress can be measured (39).
As mentioned earlier inadequate equipment and quality of care are also barriers in both Africa and Asia (14). The current definition of a SBA does not encompass these factors. While it seems many countries in Africa and Asia are increasing the percent of deliveries that are skilled, many of the individuals who are labeled as skilled do not have the necessary competence or equipment to handle maternal and newborn complications. Based on the high mortality on the first day of life, training on intrapartum-related interventions is particularly pressing.
In this analysis four or more ANC visits was significantly associated with reduced neonatal mortality on both the first day and first week of life. ANC is a means of providing women with counseling, vitamins and treatment and detection of pre-existing conditions which may have a negative impact on birth outcomes. ANC is also a means to connect women to the health system, and women who use ANC are more likely to have a skilled delivery (26). Receipt of the tetanus toxoid immunization was negatively associated with neonatal mortality on both the first day and first week of life, but these associations were not significant. Eighty-five percent of women in the study had received the tetanus toxoid vaccine, and globally there have been reductions in the number of deaths due to neonatal tetanus (35).
Limitations of this analysis include omitted variables. Many women who deliver at home do not know their child’s birth weight, and low birth weight is a strong predictor for neonatal mortality. Likewise the DHS does not include measures for gestational age and whether the mother experienced a complication. PNC could not be studied because of left censoring of the data. The DHS records newborns who died within minutes and those who died after 23 hours the same way. These deaths are recorded as occurring on day one so determining which newborns died before they were eligible for PNC was not possible.
The promotion of skilled delivery is an essential strategy to reduce both maternal and neonatal mortality. Though simple and low cost interventions are available to prevent a large proportion of neonatal deaths, they are not reaching the poorest women and children in Africa and Asia. Sufficient investment must be made in these regions to ensure that interventions are implemented at scale and at sufficient quality to ensure an impact on neonatal mortality. The cost of scale-up will be higher in countries with higher neonatal mortality than those with lower neonatal mortality. The overall cost of scale-up encompasses the costs to implement the 16 interventions themselves and the costs associated with health systems strengthening (28). When working in a relatively strong health system skilled SBAs can reduce neonatal mortality as demonstrated by their protective effect in Latin America/Caribbean. Significant commitment to improving the competency of providers in Africa and Asia is needed to enable them to save our youngest citizens. Revisions to our current definition of a SBA should be considered.
Acknowledgments
This study was funded by the United States Agency for International Development (USAID) through a cooperative agreement (GHA-A-00-08-00003-00) with MEASURE Evaluation. The views expressed in this paper do not necessarily reflect those of USAID. This work was also supported in part by an R24 Center Grant to the Carolina Population Center at the University of North Carolina at Chapel Hill. The authors would like to thank Lily Kak, Lisa Maniscalco and Allisyn Moran for comments on earlier drafts of the paper, and Erica Haney for assistance with the literature review.
References
- 1.Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Development Program (UNDP) The Path to Achieving the Millennium Development Goals: A Synthesis of MDG Evidence from Around the World. New York: UNDP; 2010. [Google Scholar]
- 3.UNICEF. Committing to Child Survival: A Promised Renewed. UNICEF; New York: 2012. [Google Scholar]
- 4.Lawn JE, Kerber K, Enweronu-Laryea C, et al. Newborn survival in low resource settings-are we delivering? Bjog-Int J Obstet Gy. 2009;116:49–59. doi: 10.1111/j.1471-0528.2009.02328.x. [DOI] [PubMed] [Google Scholar]
- 5.Saving Newborn Lives. The State of the World’s Newborns: A Report from Saving Newborn Lives. Washington, D.C: Save the Children; 2001. [Google Scholar]
- 6.Edmond KM, Quigley MA, Zandoh C, et al. Aetiology of stillbirths and neonatal deaths in rural Ghana: implications for health programming in developing countries. Paediatr Perinat Ep. 2008;22(5):430–437. doi: 10.1111/j.1365-3016.2008.00961.x. [DOI] [PubMed] [Google Scholar]
- 7.Lawn JE, Tinker A, Munjanja SP. Where is maternal and child health now? Lancet. 2006;368(9546):1474–7. doi: 10.1016/S0140-6736(06)69387-2. [DOI] [PubMed] [Google Scholar]
- 8.Lawn JE, Cousens S, Zupan J for the Lancet Neonatal Survival Steering Committee. 4 Million Neonatal Deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 9.Bryce J, Daelmans B, Dwivedi A, et al. Countdown to 2015 for maternal, newborn, and child survival: the 2008 report on tracking coverage of interventions. Lancet. 2008;371(9620):1247–58. doi: 10.1016/S0140-6736(08)60559-0. [DOI] [PubMed] [Google Scholar]
- 10.Rohde J, Cousens S, Chopra M, et al. Alma-Ata: Rebirth and revision 4 – 30 years after Alma-Ata: has primary health care worked in countries? Lancet. 2008;372(9642):950–61. doi: 10.1016/S0140-6736(08)61405-1. [DOI] [PubMed] [Google Scholar]
- 11.Nair N, Tripathy P, Prost A, et al. Improving Newborn Survival in Low-Income Countries: Community-Based Approaches and Lessons from South Asia. Plos Med. 2010;7(4) doi: 10.1371/journal.pmed.1000246. ARTN e1000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darmstadt GL, Bhutta ZA, Cousens S, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365(9463):977–88. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 13.WHO. [Accessed February 22, 2013];Births Attended by skilled health personnel (percentage) 2013 http://www.who.int/healthinfo/statistics/indbirthswithskilledhealthpersonnel/en/
- 14.Harvey S, Blandon Y, McCaw-Binn A, et al. Are skilled birth attendants really skilled? A measurement method, some disturbing results and a potential way forward. Bulletin of the World Health Organization. 2007;85:783–790. doi: 10.2471/BLT.06.038455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mbaruku G, van Roosmalen J, Kimondo I, et al. Perinatal audit using the 3-delays model in western Tanzania. Int J Gynecol Obstet. 2009;106(1):85–8. doi: 10.1016/j.ijgo.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Chalumeau M, Bouvier-Colle MH, Breart G. Can clinical risk factors for late stillbirth in West Africa be detected during antenatal care or only during labour? Int J Epidemiol. 2002;31(3):661–8. doi: 10.1093/ije/31.3.661. [DOI] [PubMed] [Google Scholar]
- 17.Taha TE, Gray RH, Abdelwahab MM, et al. Levels and Determinants of Perinatal-Mortality in Central Sudan. Int J Gynecol Obstet. 1994;45(2):109–15. doi: 10.1016/0020-7292(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 18.Weiner R, Ronsmans C, Dorman E, et al. Labour complications remain the most important risk factors for perinatal mortality in rural Kenya. B World Health Organ. 2003;81(8):561–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Ariff S, Soofi S, Sadik K, et al. Evaluation of health workforce competence in maternal and neonatal issues in public health sector of Pakistan: an Assessment of their training. BMC Health Services Research. 2010;10(319) doi: 10.1186/1472-6963-10-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wall SN, Lee ACC, Carlo W, et al. Reducing Intrapartum-Related Neonatal Deaths in Low- and Middle-Income Countries-What Works? Semin Perinatol. 2010;34(6):395–407. doi: 10.1053/j.semperi.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Mbonye AK, Sentongo M, Mukasa GK, et al. Newborn survival in Uganda: a decade of change and future implications. Health Policy Plann. 2012;27:104–17. doi: 10.1093/heapol/czs045. [DOI] [PubMed] [Google Scholar]
- 22.Blum LS, Sharmin T, Ronsmans C. Attending Home Vs. Clinic-Based Deliveries: Perspectives of Skilled Birth Attendants in Matlab, Bangladesh. Reproductive Health Matters. 2006;14(27):51–60. doi: 10.1016/S0968-8080(06)27234-3. [DOI] [PubMed] [Google Scholar]
- 23.Huque ZA, Leppard M, Mavalankar D, et al. Safe motherhood programmes in Bangladesh. In: Berer M, Ravindra TKS, editors. Safe Motherhood Initiatives: Critical Issues. London: Reproductive Health Matters; 1999. pp. 53–61. [Google Scholar]
- 24.Geefhuysen CJ. Safe Motherhood in Indonesia: A task for the next century. In: Berer M, Ravindra TKS, editors. Safe Motherhood Initatives. Critical Issues. London: Reproductive Healh Matters; 1999. pp. 62–72. [Google Scholar]
- 25.WHO/UNFA/UNICEF. Reduction of Maternal Mortality. Geneva: Author; 1999. [Google Scholar]
- 26.Stanton C, Blanc A, Croft T, Choi Y. Skilled Care at Birth in the Developing World: Progress to Date and Strategies for Expanding Coverage. J Biosoc Sci. 2007;39:109–120. doi: 10.1017/S0021932006001271. [DOI] [PubMed] [Google Scholar]
- 27.Adam T, Lim SS, Mehta S, et al. Achieving the millennium development goals for health - Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. Brit Med J. 2005;331(7525):1107–10. doi: 10.1136/bmj.331.7525.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darmstadt GL, Walker N, Lawn JE, et al. Saving newborn lives in Asia and Africa: cost and impact of phased scale-up of interventions within the continuum of care. Health Policy Plann. 2008;23(2):101–17. doi: 10.1093/heapol/czn001. [DOI] [PubMed] [Google Scholar]
- 29.Izugbara C, Karbiru C, Zulu E. Urban Poor Kenyan Women and Hospital-Based Delivery. Public Health Reports. 2009 Jul-Aug;124(4):585–589. doi: 10.1177/003335490912400416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edmond KM, Quigley MA, Zandoh C, Danso S, Hurt C, Owusu Agyei S, Kirkwood BR. Aetiology of stillbirths and neonatal deaths in rural Ghana: implications for health programming in developing countries. Paediatric Perinatal Epidemiology. 2008 Sep;22(5):430–7. doi: 10.1111/j.1365-3016.2008.00961.x. [DOI] [PubMed] [Google Scholar]
- 31.Afsana K, Rashid SF. The challenges of meeting rural Bangladeshi women’s needs in delivery care. Reproductive Health Matters. 2001 Nov;9(18):79–89. doi: 10.1016/s0968-8080(01)90094-1. [DOI] [PubMed] [Google Scholar]
- 32.Bazant E. Doctoral Dissertation. Baltimore, MD: Bloomberg School of Public Health, Johns Hopkins University; 2008. Women’s Place of Delivery and Experience of Quality in Delivery Car: A Quantitative and Qualitative Study in Nairobi’s Informal Settlements. [Google Scholar]
- 33.Paul BK, Rumsey DJ. Utilization of health facilities and trained birth attendants for childbirth in rural Bangladesh: an empirical study. Social Science in Medicine. 2002 Jun;54(12):1755–65. doi: 10.1016/s0277-9536(01)00148-4. [DOI] [PubMed] [Google Scholar]
- 34.Walraven GE, Mkanje RJ, van Roosmalen J, van Dongen PW, Dolmans WM. Comparison of Perintal Outcomes in Rural Tanzania. [PubMed] [Google Scholar]
- 35.Lawn JE, Kinney MV, Black RE, et al. Newborn survival: a multi-country analysis of a decade of change. Health Policy Plann. 2012;27:6–28. doi: 10.1093/heapol/czs053. [DOI] [PubMed] [Google Scholar]
- 36.Waiswa P, Kalter HD, Jakob R, et al. Increased use of social autopsy is needed to improve maternal, neonatal and child health programmes in low-income countries. B World Health Organ. 2012;90(6):403. doi: 10.2471/Blt.12.105718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zimba E, Kinney MV, Kachale F, et al. Newborn survival in Malawi: a decade of change and future implications. Health Policy Plann. 2012;27:88–103. doi: 10.1093/heapol/czs043. [DOI] [PubMed] [Google Scholar]
- 38.Ali M, Ahmed K, Kuroiwa C. Emergency Obstetric Care in Punjab, Pakistan: improvement needed. Eur J Contracept Reprod Health Care. 2008;13(2):201–7. doi: 10.1080/13625180701877712. [DOI] [PubMed] [Google Scholar]
- 39.Moran A, Kerber K, Pfitzer A, et al. Benchmarks to measure readiness to integrate and scale up newborn survial interventions. Health Policy and Planning. 2012;27:iii29–iii39. doi: 10.1093/heapol/czs046. [DOI] [PubMed] [Google Scholar]



