Abstract
Objective
This study investigated sexual functioning in persons with obesity and seeking weight loss, and the associations of sexual functioning with relevant demographic and clinical variables as well as quality of life.
Design and Methods
Participants were enrolled in a two-year randomized clinical trial. Participants were obese and had at least two components of metabolic syndrome. Male and female sexual functioning was assessed by the International Index of Erectile Function (IIEF) and the Female Sexual Function Index (FSFI) respectively.
Results
The rate of female sexual dysfunction was 29%. The rate of erectile dysfunction (ED) was 45%. Of the characteristics considered, FSD was associated with age (p=0.002). ED was significantly associated with age and physical functioning (both p <0.01).
Conclusions
A large minority of patients with obesity reported sexual dysfunction. The occurrence of sexual dysfunction was associated with age, but, surprisingly, not weight-related comorbidities. This may be the result of the nature of the study sample or the methods used to administer the questionnaires that assessed sexual functioning.
INTRODUCTION
Many persons with obesity pursue weight loss for the anticipated health benefits. They also seek weight reduction because of its likely effects on quality of life. Numerous studies have suggested that obesity is associated with reduced health-related quality of life (HRQOL), particularly physical limitations, bodily pain, and fatigue (1-5). Other studies have focused more specifically on the deleterious impact of obesity on domains of weight-related quality of life, which encompasses the impact of obesity on health, but also work mobility, self-esteem, interpersonal relationships, body image, and sexual functioning (6).
Two reviews on the specific relationship between obesity and sexual functioning recently have been published (7,8). These reviews suggest that there is a moderate to strong association between obesity and sexual functioning for both genders, although women with obesity appear to report greater difficulties in sexual functioning than men. Yet, there is a strong association between obesity and erectile dysfunction (ED). Additionally, presence of metabolic syndrome appears to be significantly associated with female sexual dysfunction in women with type 2 diabetes (9). Across both genders, the severity of obesity, as well as the presence and treatment of obesity-related comorbidities (e.g. type 2 diabetes and hypertension) appears to be associated with greater impairments in sexual functioning (8).
Relatively few studies have specifically documented the rate of sexual dysfunction in both obese men and women specifically seeking weight reduction. For example, in the Look AHEAD study (10), almost 50% of men with obesity (mean BMI = 35.6 kg/m2) and type 2 diabetes reported mild to moderate degrees of erectile dysfunction, and 24.8% had complete erectile dysfunction. Kadioglu and colleagues (11) reported that 50% of women in an outpatient weight loss clinic reported a sexual dysfunction. Recently, Bond and colleagues (12) reported that 60% of women presenting for bariatric surgery (mean BMI = 45.0 kg/m2) reported a sexual dysfunction.
The present study sought to build upon this growing literature by investigating the rate of sexual dysfunction in a diverse sample of men and women with obesity who presented for weight loss treatment in the context of a research study being conducted in their primary care physicians’ offices. Furthermore, this study sought to identify whether demographic, clinical, and/or quality of life measurements were associated with female sexual dysfunction (FSD) or erectile dysfunction (ED). We hypothesized that participants who were older, heavier, and had a diagnosis of metabolic syndrome, hypertension, and/or diabetes would be more likely to experience sexual dysfunction. In addition, we hypothesized that participants who reported better quality of life would have decreased odds of meeting criteria for FSD or ED.
Methods
Study Design
This study utilized baseline data from a two-year randomized controlled clinical trial titled Practice-Based Opportunities for Weight Reduction at the University of Pennsylvania (POWER-UP), described elsewhere (13,14). Participants were 390 obese men and women who also had at least two components of the metabolic syndrome. The questionnaires used in these analyses were collected during the participants’ baseline visit, which took place between January 2008 and February 2009. The POWER-UP trial was approved by the University of Pennsylvania Institutional Review Board, and informed consent was received from all randomized participants.
Participants
Participants were recruited at six primary care practices which are owned by the University of Pennsylvania Health System. Eligible participants had to be 21 years of age or older, have a BMI of 30 to 50 kg/m2, be established patients in the practice, and have at least two of five criteria for the metabolic syndrome: elevated waist circumference; elevated triglycerides; reduced HDL cholesterol; elevated blood pressure; and elevated fasting glucose (15). Participants were screened over the course of two visits to determine that they met eligibility requirements. Only participants who were willing to complete the Female Sexual Function Index or the International Index of Erectile Function questionnaire at the randomization visit were included in this investigation. Participants were excluded if they were not in a committed relationship, as defined by being married or being in another committed relationship, including a domestic partnership or being engaged.
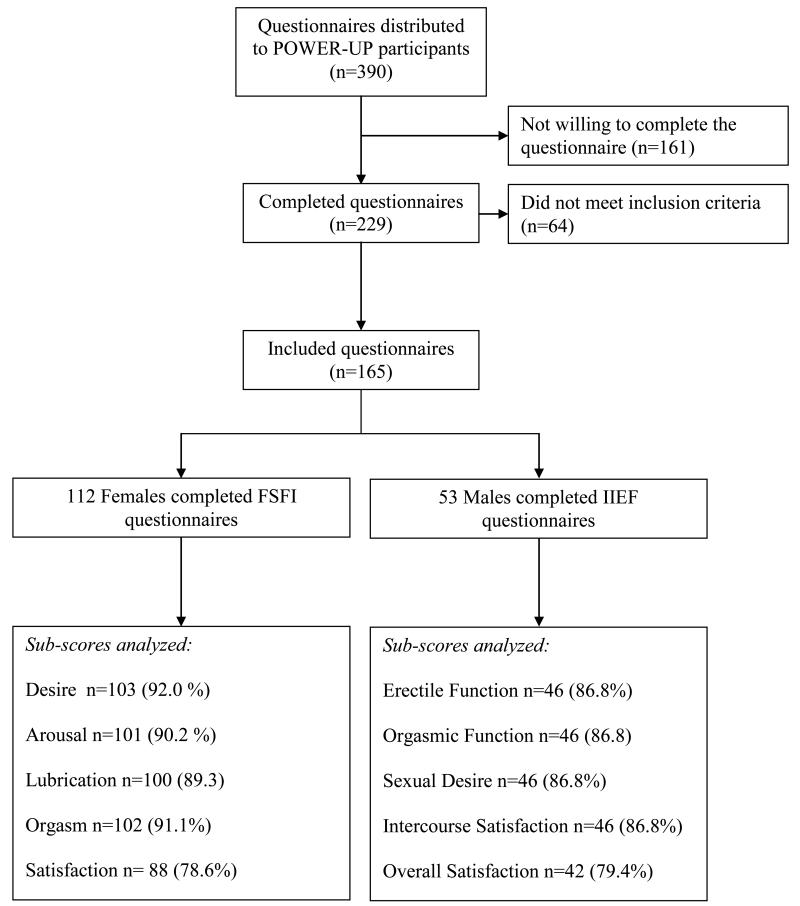
A flow chart of participants in this study is presented in Figure 1. A total of 390 questionnaires were handed out, and 229 were returned to the research staff, a response rate of 58.7%. Of those completed questionnaires, 64 were not included in this study because the participant was not in a committed relationship, yielding an effective response rate of 42.6% (36.0% of potential women and 67.1% of men).
Figure 1.
Flowchart of participant inclusion in the sexual functioning investigation.
Measures
Female Sexual Function Index (FSFI)
The FSFI is a 19-item scale which measures six domains of female sexual functioning: desire (range: 1.2-6); arousal (0-6); lubrication (0-6); orgasm (0-6); satisfaction (0.8-6); and pain (0-6). Higher scores on the questionnaire and subscales indicate better sexual function and less pain (16). Females who score ≤ 5 on the desire subscale are defined as having hypoactive sexual desire disorder (HSDD) (17). In addition, an overall total score that includes all domains and ranges from 2 to 36 can be obtained. A total FSFI score ≤ 26.55 is suggestive of female sexual dysfunction (FSD) (18). Though the desire subscale is used in the calculation for FSD, HSDD is not a subset of FSD or vice versa; a woman can be identified with a diagnosis of HSDD but not a diagnosis of FSD.
International Index of Erectile Function (IIEF)
The IIEF is a 15-item scale that assesses five domains of sexual functioning: erectile function (range: 0-30); orgasmic function (0-10); sexual desire (2-10); intercourse satisfaction (0-15); and overall satisfaction (2-10) (19,20). Lower scores indicate less satisfaction or more sexual dysfunction. Males who score < 26 on the IIEF erectile function subscale are defined as having erectile dysfunction (ED). Erectile dysfunction severity is classified as severe ED (6-10), moderate ED (11-21), mild ED (22-25), and no dysfunction (26-30).
Short Form Health Survey (SF-12)
The SF-12 is a 12 question, shortened version of the 36-item Short-Form Health Survey. Items are divided into two subscales: physical health and mental health (21). Lower scores indicate a lower health-related quality of life. Good evidence of reliability has been demonstrated between the SF-12 and the SF-36 in an obese population (22).
Impact of Weight on Quality of Life-Lite (IWQOL-Lite)
The IWQOL-Lite is a measure specifically designed for use with obese individuals (6). It contains 31 items, with each item beginning with the phrase “Because of my weight.” The measure examines five domains: physical function; self-esteem; sexual life; public distress; and work. Responses to the 31 items are combined to calculate a total score that ranges from 0 to 100; higher scores indicate a better quality of life (23).
EuroQol-5D-3L (EQ-5D)
The EQ-5D is a 5-question descriptive system that measures the following domains: mobility; self-care; usual activities; pain/discomfort; and anxiety/depression (24). Each domain has three levels: 1 = no problems; 2 = some problems; and 3 = severe problems. The answers from each domain are combined to create an index score that ranges from −0.11 to 1.0. Lower EQ-5D index scores indicate lower health status.
Patient Health Questionnaire-8 (PHQ-8)
The PHQ-8 is a shortened version of the Patient Health Questionnaire which was designed to help primary care physicians identify depression in their patients (25, 26). The measure has eight items on which participants rate the frequency with which each item is true for them. Scores on each item range from 0 (not at all) to 3 (nearly every day). A cumulative score ≥15 indicates that the patient may be clinically depressed.
Clinical characteristics
Metabolic syndrome was defined by having three of the following five conditions: systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg or on medication that lowers blood pressure; triglycerides ≥ 150 mg/dl or on medication that lowers triglycerides; waist circumference (≥ 40 inches for men, ≥ 35 inches for women); fasting blood sugar ≥ 100 mg/dl, had a pre-existing diagnosis of diabetes, or taking anti-diabetic medication; or high-density lipoprotein (HDL) (< 40 mg/dl for men, <50 mg/dl for women) (15). Diabetes mellitus was defined by current medication use or fasting glucose ≥ 126 mg/dL. Hypertension was defined by current medication use, systolic blood pressure ≥ 140 mmHg, or diastolic blood pressure ≥ 90 mmHg. Given associations observed in the sexual function literature (8), use of hypertension medication was also considered independently.
Socio-demographics, medication usage and medical history
All participants completed a brief questionnaire for socio-demographic characteristics. Medical history and current medication usage, including phosphodiesterase type 5 inhibitors and antihypertensive medications, were collected via self-report and confirmed by a study physician who reviewed the participants’ medical record.
Statistical Analysis
This analysis included 165 participants who, by self-report, were in a committed relationship (to account for regular access to a sexual partner) and completed at least 80% of the items on their gender-specific sexual functioning questionnaire. Participants’ baseline demographic and clinical characteristics were summarized. As is custom in the sexual functioning literature, all analyses were adjusted for age. Logistic regression was used to examine the associations between the binary diagnostic cut points for HSDD, FSD, and ED and the baseline and clinical characteristics. Mean with standard deviation or frequencies with percentages by HSDD, FSD, and ED status and the age adjusted p-value are reported. Ordinary least squares (OLS) regression models were fit to identify participant characteristics that were significantly associated with the subscales of FSFI and the IIEF, adjusted for age. The partial correlations of the demographic, clinical, or QOL characteristic and the age adjusted p-value are reported from each OLS model. All analyses were conducted using SAS, version 9.2. To adjust for multiple comparisons, an alpha level of p≤0.010 was utilized to identify statistically significant findings.
RESULTS
Participants’ Baseline Characteristics
Baseline descriptive characteristics of the 112 women and 53 men who met the criteria for this investigation are included in Table 1. Of the 225 participants not included in the study, 161 did not complete their gender-specific sexual functioning questionnaire, and 64 were not in a committed relationship. In comparison to the 64 participants excluded because they were not in a committed relationship, the 165 participants included in the present analysis had a significantly higher proportion of Caucasians (41% vs 71%, p<0.0001) and had a significantly higher household income (11% vs. 55% household income > $75,000; p<0.0001). Also, there was a lower proportion of Caucasians among included (n=165) as compared to the 161 participants who did not complete the questionnaire (71% of the included vs. 54%, p=0.002), as well as a higher proportion of persons with income greater than $75,000 (55% of the included vs. 28% of those who did not complete questionnaire, p<0.0001). There were no other significant differences between the 165 participants included in the study and those who did not complete the questionnaire or who were not in a committed relationship.
Table 1.
Baseline Demographic and Clinical Characteristics
| Demographic Variable* | Overall (n=165) | Female (n=112) | Male (n=53) |
|---|---|---|---|
| Age | 49.3 (10.5) | 48.1 (10.0) | 51.6 (11.2) |
| Weight | 242.9 (40.8) | 227.7 (33.0) | 275.2 (36.8) |
| BMI | 38.7 (4.8) | 38.5 (4.5) | 39.3 (5.2) |
| Race | |||
| White | 117 (71%) | 76 (68%) | 41 (77%) |
| Black | 44 (27%) | 32 (29%) | 12 (23%) |
| Asian | 2 (1%) | 2 (2%) | 0 (0%) |
| Multiracial | 2 (1%) | 2 (2%) | 0 (0%) |
| Education | |||
| Less than high school | 3 (2%) | 1 (1%) | 2 (4%) |
| High school | 43 (26%) | 31 (28%) | 12 (23%) |
| Some college | 54 (33%) | 41 (37%) | 13 (25%) |
| College or greater | 65 (39%) | 39 (35%) | 26 (49%) |
| Household Income | |||
| <$25,000 | 10 (6%) | 9 (8%) | 1 (2%) |
| $25,000 - <$35,000 | 8 (5%) | 5 (5%) | 3 (6%) |
| $35,000 - <$75,000 | 54 (33%) | 41 (37%) | 13 (25%) |
| > $75,000 | 91 (56%) | 55 (50%) | 36 (68%) |
| Marital Status | |||
| Married | 159 (96%) | 107 (96%) | 52 (98%) |
| Other Partner | 6 (4%) | 5 (4%) | 1 (2%) |
| Metabolic Syndrome (%) | 135 (82%) | 85 (76%) | 50 (94%) |
| Hypertension (%) | 105 (64%) | 65 (58%) | 40 (75%) |
| Diabetes (%) | 28 (17%) | 15 (13%) | 13 (25%) |
Values in the table are mean (SD) or N (column %)
Female Sexual Functioning
Based on the FSFI total score, 29% of women met criteria for FSD. The mean baseline scores on the five FSFI subscales were quite similar, ranging from a mean (SD) of 4.0 (2.5) on the Pain subscale to a 5.1(0.8) on the Satisfaction subscale. Scores on the Lubrication, Orgasm, Arousal, and Desire subscales were 4.2 (2.1), 4.2 (2.0), 4.4 (1.7), and 4.7 (0.9), respectively. Combining the five subscales yielded a baseline mean FSFI total score of 27.2 (7.2), range 7.4-36.0. Based on scores on the Desire subscale, 65% of women met criteria for HSDD.
Male Sexual Functioning
Forty-five percent of men were identified as experiencing ED, based on the erectile function domain score of the IIEF. The mean (SD) of all the IIEF domains, Erectile Function, Orgasmic Function, Sexual Desire, Intercourse Satisfaction, and Overall Satisfaction domains were 22.5 (7.1), 8.5 (2.6), 7.2 (2.1), 9.7 (4.2), and 6.6 (2.5), respectively. Based on the erectile function domain score, five (9%) men reported Severe ED, 15 (28%) had Moderate ED, and four (8%) Mild ED. Twenty-nine men (55%) were free of ED.
Relationship between Sexual Function and Demographic/Clinical Characteristics
As illustrated in Table 2, women with FSD were significantly older than those without FSD (52.7 vs. 46.3 years; p=0.002). Women with HSDD had a significantly lower BMI than women without HSDD (37.7. vs. 40.0 kg/m2; p=0.0008). There were no other statistically significant associations with HSDD or FSD.
Table 2.
Associations with Hypoactive Sexual Desire Disorder (HSDD), Female Sexual Dysfunction (FSD) and Male Erectile Dysfunction (ED)*
| Females | Males | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No HSDD (n=39) |
HSDD (n=73) |
No FSD (n=80) |
FSD (n=32) |
No ED (n=29) |
ED (n=24) |
||||
| Demographic & Clinical Characteristics | |||||||||
| Mean (SD) or N (%) |
Mean (SD) or N (%) | p-value | Mean (SD) or N (%) |
Mean (SD) or N (%) |
p-value | Mean (SD) or | Mean (SD) or N (%) |
p-value | |
| Age | 47.77 (10.04) | 48.34 (10.06) | 0.77 | 46.34 (9.88) | 52.66 (8.99) | 0.002 | 47.79 (9.80) | 56.29 (11.29) | 0.005 |
| Race | 0.69 | 0.86 | 0.13 | ||||||
| Caucasian | 14 (35.90%) | 22 (30.14%) | 28 (35.00%) | 8 (25.00%) | 3 (10.34%) | 9 (37.50%) | |||
| Non-Caucasian | 25 (64.10%) | 51 (69.86%) | 52 (65.00%) | 24 (75.00%) | 26 (89.66%) | 15 (62.50%) | |||
| Metabolic Syndrome | 0.09 | 0.47 | 0.97 | ||||||
| No | 7 (17.95%) | 20 (27.40%) | 21 (26.25%) | 6 (18.75%) | 3 (10.34%) | 0 (0.00%) | |||
| Yes | 32 (82.05%) | 53 (72.60%) | 59 (73.75%) | 26 (81.25%) | 26 (89.66%) | 24 (100.00%) | |||
| Hypertension | 0.73 | 0.91 | 0.80 | ||||||
| No | 16 (41.03%) | 31 (42.47%) | 35 (43.75%) | 12 (37.50%) | 9 (31.03%) | 4 (16.67%) | |||
| Yes | 23 (58.97%) | 42 (57.53%) | 45 (56.25%) | 20 (62.50%) | 20 (68.97%) | 20 (83.33%) | |||
| Hypertension Medications |
0.80 | 0.03 | 0.55 | ||||||
| No | 34 (87.18%) | 61 (83.56%) | 73 (91.25%) | 22 (68.75%) | 23 (79.31%) | 17 (70.83%) | |||
| Yes | 5 (12.82%) | 12 (16.44%) | 7 (8.75%) | 10 (31.25%) | 6 (20.69%) | 7 (29.17%) | |||
| Erectile Dysfunction Medications | 0.62 | ||||||||
| No | 28 (96.55%) | 21 (87.50%) | |||||||
| Yes | 1 (3.45%) | 3 (12.50%) | |||||||
| Diabetes | 0.17 | 0.71 | 0.45 | ||||||
| No | 31 (79.49%) | 66 (90.41%) | 69 (86.25%) | 28 (87.50%) | 24 (82.76%) | 16 (66.67%) | |||
| Yes | 8 (20.51%) | 7 (9.59%) | 11 (13.75%) | 4 (12.50%) | 5 (17.24%) | 8 (33.33%) | |||
| BMI (baseline) | 39.98 (4.56) | 37.67 (4.34) | 0.0008 | 38.78 (4.36) | 0.12 | 37.70 (4.92) | 38.90 (5.56) | 39.70 (4.80) | 0.15 |
| Quality of Life Measures | |||||||||
| IWQOL-Lite (total) | 60.78 (20.20) | 69.02 (13.88) | 0.004 | 67.78 (17.59) | 62.08 (13.82) | 0.23 | 78.78 (15.35) | 66.77 (18.85) | 0.02 |
| EQ-5D (index) | 0.83 (0.15) | 0.85 (0.11) | 0.87 | 0.86 (0.13) | 0.81 (0.14) | 0.03 | 0.91 (0.11) | 0.83 (0.10) | 0.012 |
| SF-12 | |||||||||
| Physical | 41.88 (9.82) | 44.77 (9.98) | 0.31 | 4.03 (10.03) | 43.01 (9.96) | 0.38 | 47.61 (7.89) | 41.00 (11.28) | 0.005 |
| Functioning | |||||||||
| Mental Health | 48.57 (9.58) | 47.95 (11.09) | 0.60 | 48.42 (10.56) | 47.58 (10.57) | 0.55 | 51.89 (8.70) | 50.53 (7.66) | 0.54 |
| PHQ-8 | 6.63 (5.10) | 5.71 (4.29) | 0.11 | 5.99 (4.77) | 6.13 (4.15) | 0.88 | 4.62 (4.42) | 5.92 (4.60) | 0.15 |
p-values are based on Logistic Regression, adjusted for age
Regardless of whether a woman met diagnostic criteria for a specific disorder, age was significantly associated with the lubrication and pain domains, as well as the total score on the FSFI (Table 3). Those who reported use of hypertension medications had significantly poorer sexual functioning on the arousal and pain domains and total score of FSFI in comparison to those not utilizing hypertension medications (all p≤0.010). There were no other statistically significant associations of demographic or baseline clinical characteristics with FSFI domains and total score (Table 3).
Table 3.
Associations with the FSFI Domains and Total Score with Baseline Characteristics and Quality of Life Variables*
| Baseline Characteristics | FSFI Desire | FSFI Arousal | FSFI Lubrication | FSFI Orgasm | FSFI Satisfaction | FSFI Pain | FSFI Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* |
p- value |
Correlation (r) Mean(SD)* | p- value |
|
| Race | 0.04 | 0.66 | 0.09 | 0.34 | 0.37 | 0.17 | 0.06 | 0.54 | 0.14 | 0.14 | 0.12 | 0.19 | 0.11 | 0.25 |
| Caucasian | 4.75 (0.83) | 4.71 (1.14) | 4.88 (1.47) | 4.60 (1.41) | 5.29 (0.71) | 4.77 (1.92) | 29.00 (5.29) | |||||||
| Non-Caucasian | 4.72 (0.89) | 4.40 (1.81) | 4.11 (2.13) | 4.28 (2.07) | 4.98 (0.87) | 3.83 (2.59) | 26.33 (7.88) | |||||||
| Metabolic Syndrome | 0.08 | 0.40 | 0.02 | 0.80 | 0.06 | 0.52 | 0.04 | 0.65 | 0.08 | 0.42 | 0.08 | 0.36 | 0.04 | 0.64 |
| No | 4.69 (0.71) | 4.54 (1.45) | 4.93 (1.61) | 4.67 (1.56) | 5.05 (0.74) | 4.70 (2.10) | 28.58 (6.32) | |||||||
| Yes | 4.74 (0.92) | 4.49 (1.69) | 4.18 (2.04) | 4.29 (1.98) | 5.09 (0.86) | 3.95 (2.51) | 26.74 (7.48) | |||||||
| Hypertension | 0.04 | 0.67 | 0.06 | 0.49 | 0.03 | 0.72 | 0.06 | 0.50 | 0.02 | 0.85 | 0.02 | 0.82 | 0.05 | 0.56 |
| No | 4.70 (0.88) | 4.39 (1.76) | 4.50 (1.97) | 4.54 (1.78) | 5.11 (0.83) | 4.31 (2.33) | 27.54 (7.39) | |||||||
| Yes | 4.75 (0.87) | 4.58 (1.53) | 4.26 (1.97) | 4.27 (1.96) | 5.06 (0.84) | 4.00 (2.51) | 26.93 (7.16) | |||||||
| Hypertension Medications | 0.06 | 0.48 | 0.24 | 0.007 | 0.14 | 0.09 | 0.20 | 0.02 | 0.17 | 0.07 | 0.25 | 0.004 | 0.26 | 0.004 |
| No | 4.72 (0.88) | 4.69 (1.38) | 4.55 (1.82) | 4.59 (1.74) | 5.15 (0.81) | 4.43 (2.24) | 28.14 (6.44) | |||||||
| Yes | 4.76 (0.86) | 3.42 (2.40) | 3.28 (2.42) | 3.25 (2.27) | 4.68 (0.85) | 2.45 (2.79) | 21.85 (9.13) | |||||||
| Diabetes | 0.13 | 0.15 | 0.06 | 0.51 | 0.003 | 0.97 | 0.03 | 0.75 | 0.02 | 0.83 | 0.0001 | 0.99 | 0.03 | 0.76 |
| No | 4.68 (0.86) | 4.48 (1.65) | 4.35 (2.00) | 4.38 (1.89) | 5.09 (0.83) | 4.11 (2.46) | 27.09 (7.33) | |||||||
| Yes | 5.04 (0.93) | 4.62 (1.53) | 4.40 (1.76) | 4.43 (1.93) | 5.04 (0.85) | 4.29 (2.28) | 27.82 (6.76) | |||||||
| Age | −0.01 | 0.95 | −0.09 | 0.33 | −0.35 | 0.0002 | −0.17 | 0.08 | −0.15 | 0.11 | −0.29 | 0.002 | −0.28 | 0.003 |
| BMI (baseline) | 0.17 | 0.07 | −0.07 | 0.46 | 0.02 | 0.81 | −0.07 | 0.49 | −0.16 | 0.09 | 0.06 | 0.51 | −0.004 | 0.96 |
| IWQOL-Lite (total) | −0.25 | 0.009 | 0.12 | 0.21 | 0.17 | 0.08 | 0.16 | 0.09 | 0.29 | 0.002 | 0.09 | 0.36 | 0.15 | 0.12 |
| EQ-5D (index) | −0.04 | 0.66 | −0.05 | 0.64 | 0.06 | 0.56 | 0.10 | 0.30 | 0.10 | 0.34 | 0.13 | 0.19 | 0.08 | 0.41 |
| SF-12 | ||||||||||||||
| Physical Functioning | −0.06 | 0.52 | 0.13 | 0.18 | 0.06 | 0.54 | 0.10 | 0.30 | 0.10 | 0.29 | −0.002 | 0.98 | 0.08 | 0.43 |
| Mental Health | −0.10 | 0.31 | −0.02 | 0.83 | 0.17 | 0.07 | 0.13 | 0.17 | 0.002 | 0.99 | 0.19 | 0.05 | 0.13 | 0.19 |
| PHQ-8 | 0.11 | 0.25 | 0.03 | 0.76 | −0.06 | 0.51 | −0.02 | 0.84 | −0.10 | 0.31 | −0.09 | 0.37 | −0.04 | 0.67 |
Mean(SD) for Categorical Variables; partial correlation and p-values adjusted for age.
Men with ED were significantly older (56 years) than those without ED (48) (p=0.005; Table 2). In men, and regardless of the presence of ED, there was a significant association between age and the erectile function and orgasmic function domains on the IIEF (all p≤0.010; Table 4). There were no other statistically significant associations of baseline demographic and clinical characteristics with the IIEF domain scores (Table 4).
Table 4.
Associations with the IIEF Domains with Baseline Characteristics and Quality of Life Variables*
| Baseline Characteristics | IIEF Erectile Function | IIEF Orgasmic Function | IIEF Sexual Desire | IIEF Intercourse Satisfaction | IIEF Overall Satisfaction | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Correlation (r) Mean(SD)* |
p-value | Correlation (r) Mean(SD)* |
p-value | Correlation (r) Mean(SD)* |
p-value | Correlation (r) Mean(SD)* |
p-value | Correlation (r) Mean(SD)* |
p-value | |
| Race | 0.14 | 0.30 | 0.01 | 0.92 | 0.19 | 0.16 | 0.06 | 0.67 | 0.07 | 0.63 |
| Caucasian | 19.58 (6.20) | 7.92 (1.88) | 6.17 (1.95) | 8.83 (4.09) | 6.17 (2.82) | |||||
| Non-Caucasian | 23.29 (7.14) | 8.71 (2.76) | 7.46 (2.11) | 9.95 (4.24) | 6.68 (2.36) | |||||
| Metabolic Syndrome | 0.13 | 0.32 | 0.07 | 0.57 | 0.01 | 0.93 | 0.02 | 0.86 | 0.03 | 0.83 |
| No | 27.67 (0.58) | 10.00 (0.00) | 7.67 (2.31) | 10.67 (4.93) | 7.00 (4.36) | |||||
| Yes | 22.14 (7.15) | 8.44 (2.64) | 7.14 (2.14) | 9.64 (4.20) | 6.54 (2.37) | |||||
| Hypertension | 0.12 | 0.38 | 0.15 | 0.22 | 0.02 | 0.91 | 0.22 | 0.11 | 0.15 | 0.30 |
| No | 23.00 (7.56) | 8.77 (2.98) | 7.69 (1.60) | 8.92 (4.73) | 6.15 (2.82) | |||||
| Yes | 22.28 (6.98) | 8.45 (2.49) | 7.00 (2.26) | 9.95 (4.04) | 6.70 (2.34) | |||||
| Hypertension Medications | 0.08 | 0.56 | 0.05 | 0.66 | 0.07 | 0.62 | 0.06 | 0.66 | 0.10 | 0.46 |
| No | 22.95 (6.52) | 8.70 (2.45) | 7.30 (2.10) | 9.63 (4.33) | 6.73 (2.52) | |||||
| Yes | 20.92 (8.63) | 8.00 (3.03) | 6.77 (2.24) | 9.92 (3.90) | 6.08 (2.25) | |||||
| Erectile Dysfunction Medications | 0.11 | 0.42 | 0.03 | 0.82 | 0.04 | 0.78 | 0.03 | 0.81 | 0.20 | 0.16 |
| No | 22.88 (6.55) | 8.61 (2.37) | 7.20 (2.08) | 9.82 (4.10) | 6.71 (2.42) | |||||
| Yes | 17.25 (11.73) | 7.50 (5.00) | 6.75 (2.99) | 8.25 (5.74) | 4.75 (2.50) | |||||
| Diabetes | 0.17 | 0.19 | 0.12 | 0.33 | 0.09 | 0.52 | 0.23 | 0.10 | 0.01 | 0.97 |
| No | 23.33 (6.57) | 8.80 (2.47) | 7.33 (1.91) | 10.30 (3.90) | 6.58 (2.42) | |||||
| Yes | 19.77 (8.07) | 7.69 (2.87) | 6.69 (2.72) | 7.85 (4.69) | 6.54 (2.67) | |||||
| Age | −0.37 | 0.007 | −0.47 | 0.0003 | −0.31 | 0.02 | −0.23 | 0.10 | −0.09 | 0.52 |
| BMI (baseline) | −0.05 | 0.70 | −0.06 | 0.70 | −0.22 | 0.12 | −0.11 | 0.44 | −0.04 | 0.76 |
| IWQOL-Lite (total) | 0.34 | 0.015 | 0.15 | 0.29 | 0.50 | 0.0002 | 0.27 | 0.05 | 0.32 | 0.02 |
| EQ-5D (index) | 0.35 | 0.02 | 0.25 | 0.09 | 0.29 | 0.05 | 0.30 | 0.04 | 0.40 | 0.005 |
| SF-12 | ||||||||||
| Physical Functioning | 0.39 | 0.005 | 0.17 | 0.24 | 0.33 | 0.02 | 0.27 | 0.05 | 0.26 | 0.06 |
| Mental Health | 0.17 | 0.23 | 0.07 | 0.62 | 0.34 | 0.015 | 0.30 | 0.03 | 0.44 | 0.001 |
| PHQ-8 | −0.25 | 0.07 | −0.03 | 0.84 | −0.36 | 0.008 | −0.34 | 0.013 | −0.47 | 0.0004 |
Mean(SD) for Categorical Variables; partial correlation and p-values adjusted for age.
Relationship of Sexual Functioning with Quality of Life and Depressive Symptoms
We also examined the relationship between the FSFI and IIEF and health- and weight-related quality of life (Table 2). Women with HSDD reported a better quality of life based on higher scores on the IWQOL-Lite total score than those who were not experiencing HSDD (69.0 vs. 60.8; p=0.004). Among all women, and as expected, the desire, lubrication, orgasm, and satisfaction domains of FSFI were positively correlated with the IWQOL-Lite total score (Table 3). In addition, the orgasm and pain domains of FSFI were positively correlated with the EQ-5D and the lubrication and pain domains were positively associated with mental health (SF-12). There were no other significant associations between the domains or total scores of the FSFI and QOL measures (Table 3).
In men, scores on SF-12’s Physical Health were significantly lower, indicating poorer QOL for men with ED (Table 2). Furthermore, all of the quality of life measures, including depression (PHQ-8), were positively correlated with at least one domain of the IIEF (Table 4).
DISCUSSION
In this sample, 29% of the women met the criteria for FSD and 45% of men had ED. Age (older) was the only variable of interest associated with FSD, which was surprising as we hypothesized additional variables would be significantly associated. In men, older age and poorer non-weight-related quality of life (physical functioning of SF-12) were both significantly related to ED.
Less than one third of the women in this study reported a sexual dysfunction based on all 6 domains of the FSFI (i.e. FSD). This is less than the rate found in at least one study of the general population (43%;16), a study of women in an outpatient weight loss clinic (50%;11) and women who presented for bariatric surgery (60%;12). One possible explanation for the differences is that our analysis was limited to women who reported they were married or in a committed relationship. This is in contrast, for example, with the study by Rosen and colleagues (16) who included married, divorced, and single women, some of whom may not have had regular access to a sexual partner. The lower rate of FSD in our study versus that of Bond and colleagues (12) may be associated with BMI differences. The mean BMI in the Bond et al. study was 46.1 ± 7.6 kg/m2, significantly larger than the mean BMI of women enrolled in this study (38.5 ± 4.5 kg/m2). Other studies have found that BMI is associated with impairments in health-related quality of life (1). It has also been associated with lower levels of weight-related quality of life, as assessed by the IWQOL-Lite, which includes a subscale that specifically assesses sexual functioning as related to body weight. In our study, FSD was not significantly associated with IWQOL-Lite. Another possible explanation for our differences in FSD rates could be related to the voluntary process for answering the IIEF or FSFI questionnaires in the larger POWER-UP study; it is possible that those who choose not to complete the questionnaire have higher rates of dysfunction but did not feel comfortable reporting it.
Although only 29% of women met criteria for FSD, which considers all 6 domains (including desire) of FSFI, 65% met criteria for HSDD, which is based only on the desire subscale. Despite the fact that only older age was significantly associated with FSD, BMI and weight-related quality of life were significantly associated with HSDD. As noted above, although the desire subscale of the FSFI is used in the calculation of FSD, the diagnostic cutoff for HSDD is not a subset of FSD or vice versa. Thus, differences are not surprising. In this study, the direction of the association between hypoactive sexual desire with BMI and weight-related quality of life is surprising; those with HSDD had lower BMI and better weight-related quality of life than those who did not meet criteria for HSDD. Sexual desire is unquestionably related to a range of cognitive, behavioral and physical factors. The present finding suggests that the relationship to body weight may be less strong than previously thought.
Less than half (45.2%) of men with obesity were found to suffer from some form of ED. This is substantially less than the 74.6% of men enrolled in the Look AHEAD trial (10), which investigated a similar weight loss intervention in men with type 2 diabetes. The differences in these results could be explained by the presence of diabetes in the Look AHEAD trial, or by differences in age. Men in the current study were younger than those in the Look AHEAD trial [52.0 (11.0) v. 60.5 (6.5)]. Within the current study, ED was associated with increasing age as well.
Intuitively, the difference between the present study and the Look AHEAD sample could be understood to be a function of diabetes status. Diabetes mellitus is widely acknowledged to be the single most common cause of erectile dysfunction. (7,8) Approximately 50% of men with diabetes develop erectile problems during the course of their disease and diabetes is present in approximately 25%-30% of all men presenting for sexual dysfunction treatment (27,28). However, in the present study, there was not a significant difference in the rate of ED in men with and without diabetes.
The relationship between sexual function and quality of life differed between males and females. None of the quality of life measures were associated with FSD; however, there were significant associations between poorer SF-12 Physical Functioning and ED. Further examination of the IWQOL-Lite subscales revealed that FSD was associated with the sexual life subscale (p=0.0005) but there was no association with any of the other subscales (physical function, self-esteem, public distress, work: all p>0.11). However for men, erectile dysfunction was associated with all IWQOL-Lite subscales (p<0.01), except for the self-esteem subscale (p=0.39). Further research is needed to tease out these differences between men and women in the association of sexual functioning and other quality of life measures. One speculation is the ubiquitous nature of advertisements for ED, which typically depict erectile functioning as an important aspect of quality of life. In the absence of similar medications for sexual functioning for women, it may be that women do not associate sexual functioning with quality of life in the same manner as men do.
The present study provides additional information on the sexual function of obese men and women who seek weight loss. However, the study also had a number of limitations. The greatest limitation may have been the differences between our sample and the larger POWER-UP trial. The manner in which we distributed and received the questionnaires may have contributed to this. POWER-UP participants were given the sexual functioning questionnaires before the onset of treatment and with a cover letter which stated: “The following questionnaire contains questions about your past physical and sexual experiences. Some of the questions are rather personal in nature and some of you may be somewhat uncomfortable answering them. While we would like you to complete all of the questions so that we are able to collect more information concerning this sensitive topic, if you find these questions too personal, please skip the next questionnaire.” Thus, completion was not required which likely had a detrimental impact on our response rate. In addition, participants returned the questionnaires directly to the research coordinator. Directly handing a questionnaire which includes very personal and sensitive information to another person also may have led some individuals not to participate. Taken together, these factors contributed to an effective response rate of 42.6% for the questionnaires, which is a great limitation of the present study.
In contrast, in the Look AHEAD study, sexual function was a primary outcome, participants received compensation specifically for completing the sexual function measures, and they returned them to the investigators in a sealed envelope. In addition, Look AHEAD investigators limited their sample to those that were sexually active within the last 6 months or in a committed relationship. All POWER-UP participants were asked to complete the questionnaire; however, only those in committed relationships were included in this analysis. Also, as discussed, all Look AHEAD participants had diabetes. These methodological differences may explain the different findings in this study and the Look AHEAD sexual functioning study.
The present study provides important and new information as well as some insight into the relationship between sexual functioning and quality of life in obese patients. The findings also suggest avenues for future research. Given the negative association between BMI and sexual functioning, studies should continue to investigate how weight change affects sexual function and, in turn, quality of life. Intuitively, weight loss would be anticipated to contribute to improvements in sexual functioning. However, changes in the comorbidities associated with obesity, including type 2 diabetes and hypertension, may moderate this relationship. Similarly, discontinuation of the medications that are used to treat those conditions may improve sexual functioning in men and women independent of body weight. The potential impact of these weight-related comorbidities, and the medications used to treat them, need to be thoughtfully evaluated in studies that will look at the impact of weight loss on sexual functioning.
Footnotes
DISCLOSURE
Dr. David B. Sarwer discloses that he has consulting relationships with Allergan, Baronova, Enteromedics, Ethicon Endo-Surgery, and Galderma. Sheri Volger is currently affiliated with Pfizer. Dr. Thomas A. Wadden discloses that he has relationships with Novo Nordisk, Orexigen, Vivus, Nutrisystem, Guilford Press, and the Cardiometabolic Support Network.
REFERENCES
- 1.Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev. 2001;2:173–82. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Moriarty DG, Zack MM, Mokdad AH, Chapman DP. Self-reported body mass index and health-related quality of life: findings from the behavioral risk factor surveillance system. Obes Res. 2001;9:21–31. doi: 10.1038/oby.2001.4. [DOI] [PubMed] [Google Scholar]
- 3.Hassan MK, Joshi AV, Madhavan SS, Amonkar MM. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes. 2003;27:1227–1232. doi: 10.1038/sj.ijo.0802396. [DOI] [PubMed] [Google Scholar]
- 4.Heo M, Allison DB, Faith MS, Zhu S, Fontaine KR. Obesity and quality of life: mediating effects of pain and comorbidities. Obes Res. 2003;11:209–216. doi: 10.1038/oby.2003.33. [DOI] [PubMed] [Google Scholar]
- 5.Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10:748–756. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- 6.Kolotkin RL, Crosby RD, Kosloski KD, Williams RG. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9:102–111. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 7.Kolotkin RL, Zunker C, Ostbye T. [Accessed November 7, 2012];Sexual functioning and obesity: a review [published online ahead of print May 17 2012] Obesity. 2012 http://www.nature.com/oby/journal/vaop/ncurrent/full/oby2012104a.html.
- 8.Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life and sexual function. Obes Surg. 2012;22:668–76. doi: 10.1007/s11695-012-0588-1. [DOI] [PubMed] [Google Scholar]
- 9.Esposito K, Maiorino MI, Bellastella G, et al. Determinants of female sexual dysfunction in type 2 diabetes. Int J Impot Res. 2010;22:179–84. doi: 10.1038/ijir.2010.6. [DOI] [PubMed] [Google Scholar]
- 10.Rosen RC, Wing RR, Schneider S, et al. Erectile dysfunction in type 2 diabetic men: relationship to exercise fitness and cardiovascular risk factors in the Look AHEAD trial. J Sex Med. 2009;6:1414–1422. doi: 10.1111/j.1743-6109.2008.01209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kadioglu P, Yetkin DO, Sanli O, et al. Obesity might not be a risk factor for normal sexual dysfunction. BJUI. 2009;106:1357–1361. doi: 10.1111/j.1464-410X.2010.09348.x. [DOI] [PubMed] [Google Scholar]
- 12.Bond DS, Vithiananthan S, Leahey TM, et al. Prevalence and degree of sexual dysfunction in a sample of women seeking bariatric surgery. Surg Obes Relat Dis. 2009;5:698–704. doi: 10.1016/j.soard.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, Kumanyika S, Schmitz KH, Diewald LK, Barg R, Chittams J, Moore RH. A two-year randomized trial of obesity treatment in primary care practice. New England Journal of Medicine. 2011 Nov;365(21):1969–79. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeh HC, Clark JM, Emmons KE, et al. Independent but coordinated trials: insights from the practice-based opportunities for weight reduction trials collaborative research group. Clinical Trials. 2010;7:322–332. doi: 10.1177/1740774510374213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Expert Panel on Detection and Treatment of High Blood Cholesterol in Adults Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 16.Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 17.Gerstenberger EP, Rosen RC, Brewer JV, et al. Sexual Desire and the Female Sexual Function Index (FSFI): A Sexual Desire Cutpoint for Clinical Interpretation of the FSFI in Women with and without Hypoactive Sexual Desire Disorder. J Sex Med. 2010;7:3096–3103. doi: 10.1111/j.1743-6109.2010.01871.x. [DOI] [PubMed] [Google Scholar]
- 18.Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 19.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 20.Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Adult Urology. 1999;54:346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Wee CC, Davis RB, Hamel MB. Comparing the SF-12 and SF-36 health status questionnaires in patients with and without obesity. Health Qual Life Outcomes. 2008:6. doi: 10.1186/1477-7525-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kolotkin RL, Norquist JM, Crosby RD, et al. One-year health-related quality of life outcomes in weight loss trial participants: comparison of three measures. Health Qual Life Outcomes. 2009;7:53. doi: 10.1186/1477-7525-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheung K, Oemar M, Oppe M, Rabin R. EQ-5D User Guide. 2009 Retrieved from www.euroqol.org.
- 25.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–521. 32. [Google Scholar]
- 26.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affective Disord. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 27.Hakim LS, Goldstein I. Diabetic sexual dysfunction. Endocrinol Metab Clin North Am. 1996;25:379–394. doi: 10.1016/s0889-8529(05)70329-7. [DOI] [PubMed] [Google Scholar]
- 28.McCullough DK, Campbell IW, Wu FC. The prevalence of diabetic impotence. Diabetologia. 1980;18:279–283. doi: 10.1007/BF00251005. [DOI] [PubMed] [Google Scholar]