1.Introduction
The prevalence of life-threatening injury-related conditions has remained relatively constant, yet the use of computed tomography (CT) for trauma evaluation has increased dramatically in the past 15 years 1. The desire to detect injuries with a near-zero miss rate and the widespread availability of rapid CT have driven this multi-fold increase in CT use and led many trauma centers to the adoption of complete head- to- pelvis CT scanning protocols for blunt trauma evaluation. Proponents of this “pan-scan” approach cite high sensitivity for radiologic injury diagnosis in blunt trauma of the head and cervical spine, while other investigators have shown that this can be a low-yield practice clinically in terms of actual patient care. Few of the injuries detected by CT change patient management, and the clinical significance of these injuries may not warrant the risks and costs associated with CT 1,2. The clinical benefit of CT for blunt trauma, then, remains uncertain.
At least three major problems may be associated with the incremental use of CT in trauma. First, the exposure of potentially harmful ionizing radiation to a disproportionately young patient population may have a true effect on cancer induction risk. Chest CT is among the top three types of imaging in terms of this overall risk 3. Although few physicians recognize the risks of CT-related radiation, recent investigation has determined that it is real and quantifiable 4-8. As many as 2% of cancers in the United States may be attributed to CT radiation and 29,000 future cancers may result from CT scans performed in the year 2007 alone 4-6,8. Second, CT is associated with substantial charges and costs—expenditures for CT imaging exceed $2 billion annually in the United States 6. Lastly, the additional time and resources required to perform, process and interpret potentially unnecessary CT scans is associated with increased time in the emergency department (ED), which may contribute to ED over-crowding and high rates of patients left without being seen 1,9. In a recent national study of ED trauma visits, Korley et al. determined that the mean ED stay was 126 minutes (95% CI, 123-131 minutes) longer when CT or MRI was utilized even when controlling for severity of illness and detected injuries 1. Conversely, the time, cost, and radiation associated with CT scanning may represent a net benefit to patient care if a significant number of clinically important injuries are detected by CT that might have been otherwise missed.
The objective of this study is to determine the added diagnostic utility of chest CT performed after chest x-ray (CXR) in adults presenting to the ED with blunt trauma. Specifically, we sought to determine: 1) the proportion of patients with a normal initial CXR who are subsequently diagnosed with injuries on CT and 2) the clinical significance (major, minor or no clinical significance) of injuries detected on CT, as determined by an expert panel. Determination of the number of significant injuries missed by CXR should help define the value of chest CT in this setting and may establish the need for the development of a decision instrument for selective chest CT scanning in blunt trauma patients.
2. Patients and Methods
2.1 Study Design
We analyzed retrospective data from July 2007 through March 2011. Due to the retrospective data collection, University of California, San Francisco’s Committee on Human Research determined the study was exempt from requiring patient consent.
2.2 Study Setting and Population
The study was conducted at two urban, Level I trauma centers in California, San Francisco General Hospital (SFGH) and Community Regional Medical Center (CRMC) in Fresno. We identified patients from a database of patients enrolled in a study designed to develop a decision instrument for selective CXR imaging in blunt trauma 10,11. Patients were enrolled with the following criteria:
Age >14 years.
Blunt trauma occurring within 24 hours prior to ED presentation.
Received chest imaging, (CXR and/or chest CT) in the ED as a part of their evaluation for trauma. CXRs were performed prior to chest CT, if chest CT was performed.
Enrollment of subjects took place when research assistants were available--daily from 7a.m. to 11 p.m. Research assistants collecting data were blind to final radiologic readings, abstraction of medical records, as well as hypotheses.
2.3 Outcome Determination
Radiologic outcomes were determined using official radiologic reports by board-certified radiologists. Although radiologists were aware that patients were being evaluated for trauma, they were blind to the occurrence of this study. If patients had two CXRs, both readings were considered.
With regard to clinical significance outcomes, we utilized a method similar to that used by Stiell et al 12. We convened an expert trauma panel consisting of six associate-professor-level or higher emergency physicians and four associate-professor-level or higher trauma surgeons to derive our Radiologic Injury Clinical Significance Scale (RICSS). We generated an inclusive list of chest injuries paired with management changes and interventions, e.g. pneumothorax with chest tube placement. Panel members independently reviewed this list and assigned the following values to each injury/intervention pair: major clinical significance = 2 points, minor clinical significance = 1 point, and no clinical significance = 0 points. Investigator, RMR, collated and calculated the means for these injury pairs, rounding to the first decimal place. Mean scores of 1.5-2.0, 0.5-1.49, and 0-0.49 were deemed to represent major, minor and no clinical significance, respectively (Table 1).
Table 1.
Trauma Panel Consensus of Clinical Significance Classification of Radiologic Injuries
| Radiologic Injury | No Clinical Significance | Minor Clinical Significance | Major Clinical Significance |
|---|---|---|---|
| Mediastinal hematoma | ◆No intervention or observation (outpatient management) |
◆No surgical intervention but observed for > 24hrs |
◆Evacuation or other surgical intervention |
| Hemothorax | ◆No intervention or observation (outpatient management) |
◆No chest tube but observed for > 24 hrs |
◆Thoracotomy or chest tube placement |
| Pneumothorax | ◆No intervention or observation (outpatient management) |
◆No chest tube but observed for >24 hrs |
◆Chest tube placement |
| Pericardial hematoma/effusion |
◆No intervention or observation (outpatient management) |
◆No pericardiocentesis or surgical intervention but observed for > 24 hrs |
◆Pericardiocentesis or other surgical intervention |
| Pneumomediastinum without pneumothorax |
◆No observation (outpatient management) |
◆Observed for > 24 hrs | ¥ |
| Pulmonary contusion | ◆No intervention or observation (outpatient management) |
◆No mechanical ventilation but observed for > 24 hrs |
◆Mechanical ventilation for contusion (not for other e.g… altered mental status) |
| Pulmonary laceration | ◆No intervention or observation (outpatient management) |
◆No surgical intervention but observed for > 24 hrs |
◆Surgical intervention |
| Esophageal injury | ¥ | ◆No surgical intervention but observed for > 24 hrs |
◆Surgical intervention |
| Bronchial injury | ¥ | ◆No surgical intervention but observed for > 24 hrs |
◆Surgical intervention |
| Spinal fractures | ◆No intervention or observation (outpatient management) |
◆No surgery but received in- hospital pain management (IV meds, nerve block) and observed for > 24 hrs ◆No surgery or inpatient pain management (managed on an outpatient basis) but received TLSO |
◆Surgical stabilization/intervention |
| Rib fractures | ¥ | ◆2 or more fractures: received in-hospital pain management (IV meds, epidural/nerve block) or observed for > 24 hrs; ◆2 or more fractures: No in- hospital pain management or observation (managed on an outpatient basis) |
¥ |
| Scapular fracture | ◆No intervention or observation (outpatient management) |
◆No surgery but received in- hospital pain management (IV meds, nerve block) and observed for > 24 hrs |
◆Surgical intervention |
| Sternal fracture | ¥ | ◆No surgery but had in- hospital pain management and observed for > 24 hrs ◆No surgical intervention or in-hospital pain management (managed on an outpatient basis) |
◆Surgical intervention |
| Tracheal injury | ¥ | ◆No surgical intervention but observed for > 24 hrs |
◆Surgical intervention |
| Aortic and/or great vessel injury |
¥ | ¥ | ◆Surgical intervention ◆No surgery but observed for > 24 hrs |
| Ruptured diaphragm | ¥ | ¥ | ◆Surgical intervention |
| Clavicle fracture | ◆No intervention or observation (outpatient management) |
¥ | ¥ |
Abbreviations: CXR, chest x-ray; CT, computed tomography; TLSO, thoracic lumbarsacral orthosis; IV, intravenous.
: The trauma panel deemed the management of this injury was inappropriate for this category, and classified possible management options in another category of clinical significance.
2.4 CT Techniques and Equipment
At SFGH, blunt trauma chest CT consisted of a CT angiography of the chest, utilizing a GE LightSpeed VCT (64 slice scanner; Chalfont St. Giles, UK) after 2009 and a GE CT Hi-Speed (single slice scanner; Chalfont St. Giles, UK) before 2009. At CRMC Fresno, blunt trauma chest CT included both a non-contrast and contrast CT performed with a GE LightSpeed VSX (64 slice scanner; Chalfont St. Giles, UK).
2.5 Data Abstraction
Data were abstracted from charts in a manner consistent with principles put forth by Gilbert et al 13. Our standardized data collection instrument included age, sex, mechanism of injury, vital signs, intoxication, physical exam findings (chest pain, chest tenderness, visible signs of chest injury, and altered mental status), mortality data, ultrasound data if available, CXR and chest CT results, interventions and admission data. Research assistants who had been trained by our Research Assistants Program recorded demographic data, initial vitals and initial lab reports. Physicians completed historical and physical exam elements. Another set of research assistants, who were blind to prior subject data collected, completed data abstraction from both electronic and paper medical records of final radiologic readings, admission, and interventions from progress notes or discharge summaries. The first author at the primary site trained the lead abstractor, who trained subsequent abstractors. When patients had more than one chest injury, such as multiple rib fractures (of minor clinical significance) and hemothorax with chest tube placement (major clinical significance), they were classified into the most severe category (major clinical significance in this example).
Conflicting or confusing data were presented to the first and last author who made final decisions regarding interpretation. Meetings were held periodically with chart abstractors and by phone to study coordinators at the secondary site. Chart abstractors’ performance was monitored by periodic abstraction of 10% of charts by the lead author for consistency between abstractors. All data of patients with abnormal chest CT was reviewed by two physicians and differences were resolved by consensus.
2.6 Data Analysis
Databases were created in Microsoft Excel (Microsoft Corp., Seattle, WA). We used Stata Corp., version 9.0 to calculate descriptive statistics using proportions and means with interquartile ratios or 95% confidence intervals as appropriate.
3. Results
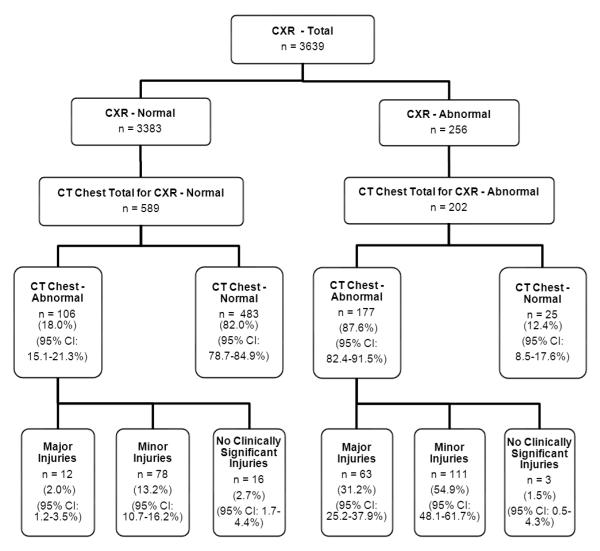
Of 3639 total patients enrolled, 2848 (78.3%) had a CXR alone and 791 (21.7%) received both a CXR and chest CT. Fourteen subjects were excluded from the study because of unavailability of medical records. The demographics of the enrolled patients who had both chest CXR and CT are shown in Table 2. Figure 1 illustrates the final classification of injuries.
Table 2.
Demographics of patients with CT Chest
| Demographics, Clinical Characteristics, and Mechanism of Injury |
CXR and Chest CT No., (%) |
|---|---|
| Mean age (IQR)* | 46.6 (30 – 60y) |
| Male | 518 (65.6) |
| Mechanism of blunt trauma Motor vehicle accident |
378 (47.8) |
| Fall (not from standing) | 118 (14.9) |
| Pedestrian struck by motorized moving vehicle | 103 (13.0) |
| Motorcycle accident | 73 (9.2) |
| Other trauma | 46 (5.8) |
| Fall from standing | 27 (3.4) |
| Bicycle accident | 24 (3.0) |
| Struck by blunt object(s) | 12 (1.5) |
| Struck by fists or kicked | 14 (1.8) |
| Unknown | 16 (2.0) |
| Injury Severity Score Mean (SD) ** | 18.5 (11.2) |
| Admitted for >24 hours | 574 (72.6) |
Abbreviations: No., number; IQR, interquartile ratio; SD, standard deviation
Injury severity scores (ISS), when available, were retrospectively abstracted from a trauma database of admitted patients at the primary hospital site.
Figure 1.
Total enrolled patients, radiographic studies, results, and patient’s ultimate classification of their highest level of radiologic injury by clinical significance.
3.1 Outcome by Radiologic Injury
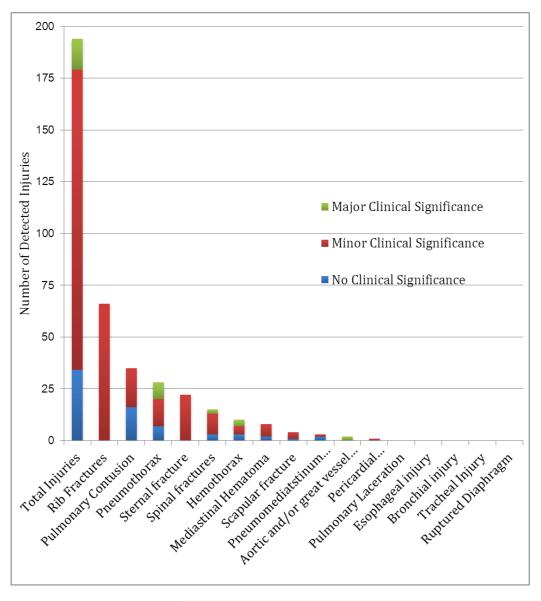
Radiologic injuries were defined by final radiologic reports as any of the following injuries in the first column, listed in Table 1. Of the 589 patients who had a chest CT after a normal CXR, 483 [82.0% (95% CI: 78.7-84.9%)] had CTs that were also read as normal and 106 [18.0% (95% CI: 15.1-21.3%)] had CTs that diagnosed injuries, primarily rib fractures, pulmonary contusions and incidental pneumothorax. In patients with a CXR suggesting injury, the majority had injuries confirmed by chest CT, including multiple rib fractures, pneumothorax, hemothorax, and pulmonary contusion.
3.2 Outcome by Clinical Significance
Table 1 shows the results of our a priori expert panel classification (RICSS). Of the 589 patients with a normal CXR, chest CT led to an injury diagnosis of major clinical significance in 12 [2.0% (95% CI: 1.2-3.5%)], minor significance in 78 [13.2% (95% CI: 10.7-16.2%)], and clinically insignificant in 16 [2.7% (95% CI (1.7-4.4%)] cases. Table 3 lists the injuries undetected on CXR but diagnosed by CT according to clinical significance, and Figure 2 is a graphical depiction of these injuries.
Table 3.
Detailed classification of injuries detected on chest CT when CXR is normal. A single patient could have multiple injuries.
| Missed on | Major Clinical | Minor Clinical | No Clinical | |
|---|---|---|---|---|
| Injury | CXR | Significance | Significance | Significance |
| Rib fractures | 66 | 0 | 66 | 0 |
| Sternal fracture | 22 | 0 | 22 | 0 |
| Pulmonary contusion | 35 | 0 | 19 | 16 |
| Pneumothorax | 28 | 8 | 13 | 7 |
| Spinal fractures | 15 | 2 | 10 | 3 |
| Hemothorax | 10 | 3 | 4 | 3 |
| Mediastinal hematoma | 8 | 0 | 6 | 2 |
| Scapular fracture | 4 | 0 | 3 | 1 |
| Pneumomediatstinum without pneumothorax |
3 | 0 | 1 | 2 |
| Aortic and/or great vessel injury |
2 | 2 | 0 | 0 |
| Pericardial hematoma/effusion |
1 | 0 | 1 | 0 |
| Pulmonary laceration | 0 | 0 | 0 | 0 |
| Esophageal injury | 0 | 0 | 0 | 0 |
| Bronchial injury | 0 | 0 | 0 | 0 |
| Tracheal injur | 0 | 0 | 0 | 0 |
| Ruptured diaphragm | 0 | 0 | 0 | 0 |
| Total of missed injuries | 194 | 15 | 145 | 34 |
Figure 2.
Plain radiograph missed injuries, classified by clinical significance of observed major, minor injuries, and no clinical significance. N=194
Of the 202 patients with a CXR suggesting traumatic injury, chest CT confirmed radiologic injury in 177 [87.6% (95% CI: 82.4-91.5%)] patients and ruled out radiologic injury in 25 patients [12.4% (95% CI: 8.5-17.6%)]. In the 177 patients with radiologic injury on CXR and CT, major injury was seen in 63 [31.2% (95% CI: 25.2-37.9%)], minor injury in 111 [54.9% (95% CI: 48.1-61.7%)], and clinically insignificant injury in 3 [1.5% (95% CI: 0.5-4.3%)] of cases. The calculated kappa was 0.94, indicating extremely high inter-abstractor agreement.
4. Discussion
In this study of adult victims of blunt trauma, we found that 18.1% of patients who were evaluated by both CXR and chest CT were diagnosed with radiologic injuries detected by CT but missed by CXR. The majority of injuries detected by CT alone, however, were clinically minor or insignificant, resulting in little or no change in management. Thus, in the setting of a normal CXR, chest CT was a relatively low yield test. In those patients who had CXR suggesting injury, chest CT confirmed injury in the vast majority of cases, and nearly a third were clinically major injuries. CT ruled out injury in approximately 12% of these abnormal CXR cases.
At most institutions, standard blunt trauma imaging protocols begin with plain radiography. Because of the increased availability and rapidity of CT scans, CT imaging has replaced plain x-rays as the first step in some institutions. Advocates of routine CT scanning cite much greater sensitivity of CT for injuries 14,15. However, several studies of head and cervical CT scanning have shown that this increased sensitivity of injury detection does not necessarily translate to the detection of injuries that require an intervention, and no study has demonstrated improved outcomes with routine CT in blunt trauma 1,2,16. We similarly found that CT detected more injuries than CXR, but at a cost of many additional negative CT scans in patients with a normal CXR. The CXR was abnormal in 63 of 75 (84%) patients with major thoracic injury. The challenge is to develop a rational approach to selective utilization of chest CT to detect the major injuries missed by CXR while minimizing CT scans in patients without injury.
In smaller studies, other investigators have examined the utility of CXR and chest CT in blunt trauma patents. Barrios et al. found that patients with a normal screening CXR were much less likely to have an abnormal subsequent chest CT compared to those with initial abnormal CXR (25% vs 81%). Only 9 of 143 patients with a normal CXR had a change in management via chest CT imaging 17. Traub et al. also showed that chest CT was diagnostically more sensitive than CXR in blunt trauma patients but found that only 19% (27/141) of their patients had a subsequent investigation and/or intervention due to the chest CT 14.
In a resource-constrained system, the costs, time and radiation risk of chest CT cannot be ignored. The charge for the performance and interpretation of trauma chest CT at our institution is $2,875. In the year 2007 alone, more than 70 million chest CTs were performed 18. While radiation dosage has not yet been directly correlated to cancer, numerous studies have extrapolated the cancer risks from the aftermaths of the atomic bomb and Chernoble. In CT coronary angiography studies, Einstein et al. estimated a lifetime attributable risk of cancer in a 20-year-old woman from a single CT scan to be 0.70%, whereas Horowitz et al. estimated a relative risk of 1.4% to 2.6% for breast cancer and 2.4% to 3.8% for lung cancer in 25-year-old 19,20. The women cancer-induced mortality risk has been estimated to be as high as 12.5 deaths per 10,000 CTs 21. Thus, the risks of cancer must be considered against the added benefit of chest CT .
4.1 Limitations
There are no standard accepted definitions of clinically significant changes in management, and practitioners may disagree with our expert panel classification. To address this potential disagreement, we have included analyses that reflect a full range of interpretations of clinical significance. Because some of our data were collected retrospectively, the true reasons for certain interventions may have been misinterpreted. For example, a patient may have been admitted and observed for concomitant head injuries or a patient may have been intubated for altered mental status rather than for their chest injury. Because not all patients had a chest CT, it is not possible to calculate the true sensitivity and specificity of these imaging modalities.
5. Conclusions
Overall, our findings indicate that if chest imaging is indicated in a blunt trauma patient, it should begin with a CXR. In patients with an abnormal CXR, chest CT is a high yield test, and reveals many significant injuries. Those patients who have a normal CXR present a more difficult decision. Routine chest CT detects additional injuries, but most are minor. A decision instrument that would assist the clinician in selective chest CT utilization in this group is warranted. Such a guideline might include clinical features and CXR results to separate blunt trauma victims into high risk for clinical injury (benefit from chest CT) and low risk for clinical injury (no need for CT) groups. Given that there may be substantial inter-specialty disagreement as to what injuries are important to detect, consensus expert panels like the one we convened would be crucial to the development of an acceptable guideline 22. Nevertheless, by determining the subset of patients who are unlikely to have a clinically significant injury, it may be possible to safely reduce CT utilization in this patient population.
In summary, we found that in blunt trauma patients, chest CT after a normal CXR rarely detected a clinically significant injury. Although many injuries were found, the large majority were clinically minor or insignificant, resulting in no change in management. Development of a decision instrument to detect important, occult injuries, while minimizing the cost, time, and radiation of CT is warranted.
Acknowledgments
Phillip Hong, BA, Gabriel Prager, BS, and Matthew Cuenot, BS for assistance with data collection and entry.
Footnotes
Conflicts of interest and source of funding: Bory Kea received a grant UCSF Clinical and Translational Science Institute Resident Research Grant. For the remaining authors, no conflicts were declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bory Kea, Department of Emergency Medicine, UCSF School of Medicine, San Francisco General Hospital, San Francisco, CA borykea@gmail.com.
Ruwan Gamarallage, Department of Emergency Medicine, UCSF School of Medicine, San Francisco General Hospital, San Francisco, CA ruwangamage@gmail.com.
Hemamalini Vairamuthu, Department of Emergency Medicine, UCSF School of Medicine, San Francisco General Hospital, San Francisco, CA hemavairamuthu@yahoo.com.
Jonathan Fortman, Department of Emergency Medicine, UCSF School of Medicine, San Francisco General Hospital, San Francisco, CA Jonathan.Fortman@emergency.ucsf.edu.
Kevin Lunney, Department of Emergency Medicine, UCSF School of Medicine-Fresno, Fresno Regional Community Medical Center, Fresno, CA KLunney@fresno.ucsf.edu.
Gregory W. Hendey, Department of Emergency Medicine, UCSF School of Medicine-Fresno, Fresno Regional Community Medical Center, Fresno, CA GHendey@fresno.ucsf.edu.
Robert M. Rodriguez, Department of Emergency Medicine, UCSF School of Medicine, San Francisco General Hospital, San Francisco, CA Robert.Rodriguez@emergency.ucsf.edu.
REFERENCES
- 1.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA : the journal of the American Medical Association. 2010;304:1465–71. doi: 10.1001/jama.2010.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atzema C, Mower WR, Hoffman JR, et al. Defining “therapeutically inconsequential” head computed tomographic findings in patients with blunt head trauma. Annals of emergency medicine. 2004;44:47–56. doi: 10.1016/j.annemergmed.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 3.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Archives of internal medicine. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071–7. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brenner DJ, Hall EJ. Risk of cancer from diagnostic X-rays. Lancet. 2004;363:2192. doi: 10.1016/S0140-6736(04)16519-7. author reply -3. [DOI] [PubMed] [Google Scholar]
- 6.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361:849–57. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231:393–8. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]
- 8.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center for Disease Control and Prevention NCfHS . National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary: Center for Disease Control and Prevention. National Center for Health Statistics; May 26, 2005. 2005. Report No.: 358. [Google Scholar]
- 10.Rodriguez RM, Hendey GW, Mower W, et al. Derivation of a Decision Instrument for Selective Chest Radiography in Blunt Trauma. J Trauma. 2010 doi: 10.1097/TA.0b013e3181f2ac9d. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez RM, Hendey GW, Marek G, Dery RA, Bjoring A. A pilot study to derive clinical variables for selective chest radiography in blunt trauma patients. Ann Emerg Med. 2006;47:415–8. doi: 10.1016/j.annemergmed.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391–6. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27:305–8. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 14.Traub M, Stevenson M, McEvoy S, et al. The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury. 2007;38:43–7. doi: 10.1016/j.injury.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Tillou A, Gupta M, Baraff LJ, et al. Is the use of pan-computed tomography for blunt trauma justified? A prospective evaluation. J Trauma. 2009;67:779–87. doi: 10.1097/TA.0b013e3181b5f2eb. [DOI] [PubMed] [Google Scholar]
- 16.Barrios C, Malinoski D, Dolich M, Lekawa M, Hoyt D, Cinat M. Utility of thoracic computed tomography after blunt trauma: when is chest radiograph enough? The American surgeon. 2009;75:966–9. [PubMed] [Google Scholar]
- 17.Barrios C, Malinoski D, Dolich M, Lekawa M, Hoyt D, Cinat M. Utility of thoracic computed tomography after blunt trauma: when is chest radiograph enough? Am Surg. 2009;75:966–9. [PubMed] [Google Scholar]
- 18.Sarma A, Heilbrun ME, Conner KE, Stevens SM, Woller SC, Elliott CG. Radiation and Chest CT Scan Examinations: What Do We Know? Chest. 2012;142:750–60. doi: 10.1378/chest.11-2863. [DOI] [PubMed] [Google Scholar]
- 19.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA : the journal of the American Medical Association. 2007;298:317–23. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 20.Hurwitz LM, Reiman RE, Yoshizumi TT, et al. Radiation dose from contemporary cardiothoracic multidetector CT protocols with an anthropomorphic female phantom: implications for cancer induction. Radiology. 2007;245:742–50. doi: 10.1148/radiol.2453062046. [DOI] [PubMed] [Google Scholar]
- 21.Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology. 2004;230:619–28. doi: 10.1148/radiol.2303021726. [DOI] [PubMed] [Google Scholar]
- 22.Gupta M, Schriger DL, Hiatt JR, et al. Selective use of computed tomography compared with routine whole body imaging in patients with blunt trauma. Annals of emergency medicine. 2011;58:407–16. e15. doi: 10.1016/j.annemergmed.2011.06.003. [DOI] [PubMed] [Google Scholar]