Abstract
Short-chain fatty acids (SCFAs), the end products of fermentation of dietary fibers by the anaerobic intestinal microbiota, have been shown to exert multiple beneficial effects on mammalian energy metabolism. The mechanisms underlying these effects are the subject of intensive research and encompass the complex interplay between diet, gut microbiota, and host energy metabolism. This review summarizes the role of SCFAs in host energy metabolism, starting from the production by the gut microbiota to the uptake by the host and ending with the effects on host metabolism. There are interesting leads on the underlying molecular mechanisms, but there are also many apparently contradictory results. A coherent understanding of the multilevel network in which SCFAs exert their effects is hampered by the lack of quantitative data on actual fluxes of SCFAs and metabolic processes regulated by SCFAs. In this review we address questions that, when answered, will bring us a great step forward in elucidating the role of SCFAs in mammalian energy metabolism.
Keywords: nutritional fiber, bacterial short-chain fatty acid metabolism, short-chain fatty acid fluxes and concentrations
The decrease in physical exercise and increase in energy intake, especially seen in the Western world, disrupts the energy balance in humans and can lead to a complex of symptoms collectively denoted as the metabolic syndrome. The key characteristics of the metabolic syndrome are obesity, loss of glycemic control, dyslipidemia, and hypertension (1). Due to the complex multifactorial etiology of the metabolic syndrome, the exact mechanisms underlying the different comorbidities are not yet completely known. Recently, dietary fibers have raised much interest, as they exert beneficial effects on body weight, food intake, glucose homeostasis, and insulin sensitivity (2–4). Epidemiological studies show an association between a higher fiber intake and a reduced risk of irritable bowel syndrome, inflammatory bowel disease, cardiovascular disease, diabetes, and colon cancer (1).
Humans lack the enzymes to degrade the bulk of dietary fibers. Therefore these nondigestible carbohydrates pass the upper gastrointestinal tract unaffected and are fermented in the cecum and the large intestine by the anaerobic cecal and colonic microbiota. Fermentation results in multiple groups of metabolites [elegantly reviewed by Nicholson et al. (5)] of which short-chain fatty acids (SCFAs) are the major group (6). To the microbial community SCFAs are a necessary waste product, required to balance redox equivalent production in the anaerobic environment of the gut (7). SCFAs are saturated aliphatic organic acids that consist of one to six carbons of which acetate (C2), propionate (C3), and butyrate (C4) are the most abundant (≥95%) (8). Acetate, propionate, and butyrate are present in an approximate molar ratio of 60:20:20 in the colon and stool (9–11). Depending on the diet, the total concentration of SCFAs decreases from 70 to 140 mM in the proximal colon to 20 to 70 mM in the distal colon (12). A unique series of measurements in sudden-death victims (n = 6) showed that the acetate:propionate:butyrate ratio in humans was similar in the proximal and distal regions of the large intestine (11). In the cecum and large intestine, 95% of the produced SCFAs are rapidly absorbed by the colonocytes while the remaining 5% are secreted in the feces (12–15).
In the last few decades, it became apparent that SCFAs might play a key role in the prevention and treatment of the metabolic syndrome, bowel disorders, and certain types of cancer (16–22). In clinical studies SCFA administration positively influenced the treatment of ulcerative colitis, Crohn's disease, and antibiotic-associated diarrhea (10, 23–27). The molecular mechanisms by which SCFAs induce these effects are an active field of research. In this review we will discuss the role of SCFAs in the interplay between diet, gut microbiota, and regulation of host energy metabolism. We will argue that an integrated understanding will require more quantitative data on the SCFA flux across the intestinal wall and the impact this has on host metabolism.
THE DIET
Gut bacteria in the cecum and large intestine produce SCFAs mainly from nondigestible carbohydrates that pass the small intestine unaffected. The different types and amounts of nondigestible carbohydrates that reach the cecum and large intestine depend on the daily intake and type of food. The major components of fiber that pass the upper gut are plant cell-wall polysaccharides, oligosaccharides, and resistant starches (28). The average human diet in Western societies contains approximately 20–25 g fiber/day (29). In diets that are high in fruit and vegetables, the fiber content may reach 60 g/day (30). Fermentation of the carbohydrates reaching the cecum yield 400–600 mmol SCFAs/day, which amounts to a production of SCFAs of 0.24–0.38 kg body weight−1 h−1, equivalent to ∼10% of the human caloric requirements (31).
The amount and type of fiber consumed has dramatic effects on the composition of the intestinal microbiota and consequently on the type and amount of SCFAs produced. For the host, the in vivo SCFA production rates as well as the intestinal SCFA concentrations on different fibers are most relevant. As we discuss in the next sections, information on the cecal SCFA content is available in model organisms, but there is limited information about in vivo production rates. In contrast, in humans measurement of the cecal SCFA concentration is almost impossible and in most cases conclusions about cecal and colonic metabolism are deduced from fecal content and in vitro studies.
Concentrations of SCFAs as a function of diet
In Table 1 we list the effect of fibers on intestinal SCFA concentrations in various studies. Although units and information on dietary composition differ, this overview allows a number of conclusions. In the rat, the addition of fiber resulted in increased cecal SCFA concentrations compared with control diets. The cecal concentrations depend on the type of fiber used but also on the daily fiber intake. There is no linear correlation between fiber intake and SCFA concentration in the cecum (32). Cecal SCFA concentrations increased when 10% of dietary wheat starch was replaced by inulin, but decreased again when fiber content was increased to 20% inulin (Table 1). In contrast to other fibers, inulin shifted the relative production of SCFAs from acetate to propionate and butyrate (32, 33). In pigs, compared with rats a better model for the human gastrointestinal tract, the increase in daily fiber intake is less reflected in the cecal SCFA concentrations (Table 1) (34, 35). However, in studies with pigs, the increase in daily fiber intake per kg body weight is much less compared with the rat studies described above. Indeed, by increasing the daily fiber intake even more, the cecal SCFA concentrations were also increased in pigs (Table 1) (36, 37).
TABLE 1.
Total and molar percentage SCFAs after dietary intervention with various types of fibers in different organisms
| Diet | Daily Fiber Intake (g/day) | Concentration SCFAs | Molar Percentage (Acetate:Propionate:Butyrate) | Reference |
| Rat cecum | ||||
| mmol/L | (76) | |||
| Control | 0 | 41 | 72:14:14 | |
| Cellulose | 1 | 36 | 72:14:14 | |
| Oligofructose | 1 | 50 | 71:10:19 | |
| Fructooligosaccharides | 1 | 61 | 74:9:17 | |
| Xylooligosaccharides | 1 | 46 | 76:11:13 | |
| mmol/L | (32) | |||
| Control | 0 | 85 | 65:23:12 | |
| 5% inulin | 1 | 143 | 45:34:21 | |
| 10% inulin | 2 | 156 | 43:37:20 | |
| 20% inulin | 4 | 107 | 40:34:26 | |
| μ mol/g | (33) | |||
| Control | 0 | 47 | 77:8:15 | |
| Cellulose | 2 | 48 | 83:6:11 | |
| Pectin | 3 | 71 | 84:11:5 | |
| Inulin | 2 | 57 | 63:18:19 | |
| Resistant starch | 5 | 92 | 76:7:17 | |
| Barley hulls | 2 | 62 | 78:5:17 | |
| Pig cecum | ||||
| mmol/L | (34) | |||
| White rice (control) | 20 | 80 | 64:25:11 | |
| Brown rice | 43 | 75 | 66:27:7 | |
| Rice bran | 36 | 68 | 67:25:8 | |
| Rice bran plus rice oil | 43 | 76 | 68:22:10 | |
| mmol/L | (35) | |||
| White rice | 33 | 69 | 68:26:6 | |
| Pan-boiled brown rice | 33 | 63 | 62:32:6 | |
| mmol/L | (37) | |||
| Control | 14 | 70 | 67:22:11 | |
| Wheat bran | 42 | 131 | 60:31:9 | |
| Oat bran | 44 | 92 | 59:32:9 | |
| Baked beans | 45 | 124 | 65:30:5 | |
| mmol/L | (36) | |||
| Control | Not reported | 100 | 73:20:6 | |
| Resistant starch | Not reported | 140 | 73:22:5 | |
In humans the effect of dietary fiber intake has been studied mainly by measuring the SCFA concentrations in feces followed by calculating the total rate of SCFA excretion. Fecal secretion rates for SCFA are in the range of 10–30 mmol/day for diets with high fiber content compared with 5–15 mmol/day for control diets (38–42). In most studies, acetate is the predominant SCFA in the feces, followed by propionate and butyrate. It is important to note that fecal SCFA concentrations do not reflect their concentration and production rate in the intestine as most SCFAs are taken up by the host and therefore fecal SCFA excretion provides little information about actual intestinal SCFA metabolism.
Production fluxes of SCFAs
Because SCFA production is difficult to measure in vivo, most experiments have been done in vitro with intestinal or fecal microbiota as inoculum (Table 2). In vitro fermentation, however, differs from the in vivo situation because: i) during isolation of microbiota the diversity alters dramatically, and ii) products accumulate during fermentation.
TABLE 2.
In vitro SCFA production rates from different organisms
| SCFA Production Rate | ||||||
| Substrate | Inoculum Origin | Acetate | Propionate | Butyrate | Total SCFAs | Reference |
| Pig colon | mmol/L reaction volume/h | (43) | ||||
| Cellulose | 1.7 | 2.5 | 0.8 | 5.0 | ||
| Wheat bran | 5.8 | 4.2 | 3.1 | 13.1 | ||
| Ispaghula husk | 8.3 | 8.3 | 1.0 | 17.6 | ||
| Gum arabic | 5.8 | 5.8 | 0.4 | 12.0 | ||
| Swine ileum | mmol/g substrate/h | (44) | ||||
| Raffinose + stachyose | 0.17 | 0.08 | 0.08 | 0.33 | ||
| Non-oligosaccharides soy solubles | 0.17 | 0.05 | 0.05 | 0.27 | ||
| Soy solubles | 0.12 | 0.02 | 0.03 | 0.17 | ||
| Non-oligosaccharide tGOS | 0.15 | 0.05 | 0.05 | 0.25 | ||
| Transgalactooligosaccharides | 0.07 | 0.02 | 0.02 | 0.10 | ||
| After 6 week adaptation | ||||||
| Raffinose + stachyose | 0.30 | 0.20 | 0.07 | 0.57 | ||
| Non-oligosaccharides soy solubles | 0.17 | 0.07 | 0.03 | 0.25 | ||
| Soy solubles | 0.12 | 0.05 | 0.02 | 0.18 | ||
| Non-oligosaccharide tGOS | 0.18 | 0.13 | 0.03 | 0.35 | ||
| Transgalactooligosaccharides | 0.07 | 0.05 | 0.02 | 0.13 | ||
| Human feces | mmol/L reaction volume/h | (45) | ||||
| Glucose | 21.2 | 5.0 | 2.2 | 28.3 | ||
| Soy oligosaccharide | 12.3 | 6.6 | 5.8 | 24.6 | ||
| Fructooligosaccharide | 15.8 | 5.5 | 2.8 | 24.1 | ||
| Inulin | 13.5 | 7.8 | 5.3 | 26.6 | ||
| Hydrolyzed inulin | 15.1 | 6.4 | 3.9 | 25.4 | ||
| Cellulose | 9.3 | 11.8 | 1.6 | 22.7 | ||
| Powdered cellulose | 7.6 | 8.3 | 3.5 | 19.5 | ||
| Methyl cellulose | 15.3 | 5.8 | 5.0 | 26.2 | ||
| Hydrolyzed guar gum | 13.3 | 11.1 | 7.3 | 31.8 | ||
| Psyllium husk | 8.7 | 8.0 | 7.9 | 24.7 | ||
| Human feces | mmol/g substrate/h | (46) | ||||
| Corn fiber | 0.178 | 0.070 | 0.058 | 0.306 | ||
| Oat bran | 0.546 | 0.187 | 0.125 | 0.858 | ||
| Wheat bran | 0.285 | 0.082 | 0.063 | 0.430 | ||
| Human feces | mmol/L reaction volume/h | (166) | ||||
| Lactulose 2.5 mg/ml | — | — | — | 3.8 | ||
| Lactulose 5.0 mg/ml | — | — | — | 7.5 | ||
| Lactulose 7.5 mg/ml | — | — | — | 10.0 | ||
| Lactulose 10.0 mg/ml | — | — | — | 6.3 | ||
tGOS, transgalactooligosaccharides.
Using microbiota obtained from pig intestine, studies showed pronounced differences in SCFA production rates from different fibers (Table 2) (43, 44). In addition, in vitro SCFA production by inocula derived from swine ileum were higher when the swine were put on galactooligosaccharide diets for 6 weeks compared with production rates before adaptation (Table 2) (44). Studies using human feces as inoculum show less pronounced effects of fiber type (45, 46). It is unclear if this is due to the type of fiber or the origin of the microbiota. Titration with lactulose yielded an optimum SCFA production rate at 7.5 mg/ml (Table 2), reminiscent of the in vivo effect of inulin supply on the cecal SCFA concentrations (Table 1).
As far as we know, Bergman et al. (47) performed the most accurate in vivo determination of SCFA production rates. In three separate experiments they infused radiolabeled acetate, propionate, or butyrate into the rumen of continuously dried grass-fed sheep. Combining the data of the radioactivity of the SCFAs in the rumen they found production rates of 2.9, 0.8, and 0.5 mmol kg body weight−1 h−1 for acetate, propionate, and butyrate, respectively. These values cannot be translated to humans, because fiber fermentation in ruminants has a more prominent role than it has in nonruminants (31), yet this methodology is well-suited to be applied more widely in laboratory animals. Alternative techniques to measure intestinal SCFA fluxes are indirect and subject to controversy. In these studies isotope dilution of intravenously infused 13C-labeled SCFAs was monitored (48, 49). The obtained values reflect the rate of appearance of SCFAs in the peripheral circulation after first-pass extraction by the splanchnic bed, and thereby underestimate SCFA production by gut microbiota. Pouteau et al. (48) performed whole-body stable-isotope-dilution studies in fasted humans before and after giving them 20 g of pure lactulose. From the difference in whole-body production between both situations, they estimated the colonic acetate production rate to be 0.2 mmol kg body weight−1 h−1. Isotope studies in children, who are unable to metabolize propionate due to a nonfunctional propionyl-CoA carboxylase, showed that gut microbiota produce approximately 0.05 mmol kg body weight−1 h−1 propionate (50). This estimated propionate production rate is 4-fold lower than the reported acetate production rate. Although we are aware that these studies cannot be compared directly, we note that this ratio is similar to the average acetate:propionate ratio in cecal concentration (Table 1).
THE PRODUCTION OF SCFAs BY GUT MICROBIOTA
Changes in dietary fibers drive changes in the composition of gut microbiota. Although diet is a major determinant of the colonic microbiome, the host genetic background and the colonic milieu also exert a strong influence on the microbial composition in the large intestine (51–54). The microbial activity in turn also affects the colonic milieu. Together, this causes a strong variation of the microbial population between individuals. In this section we will discuss this variation, the mechanisms of microbial SCFA production, and the interaction between microbial composition, microbial SCFA production, and the colonic milieu.
The composition of gut microbiota
Infants are born without gut microbiota, but rapidly after birth the infant's gut is conventionalized by bacteria coming from the mother and the surrounding environment. The composition of the microbiota stays unstable until the age of approximately 3–4 years, when it becomes mature. Colonization of the gut has two major benefits. First, the microbiota educate the immune system and increase the tolerance to microbial immunodeterminants (55). Second, the microbiota act as a metabolic organ that can break down otherwise indigestible food components, degrade potentially toxic food compounds like oxalate, and synthesize certain vitamins and amino acids (55). Each individual has a unique microbiome of which the composition is influenced by the host genotype and physiology, the colonization history, environmental factors, food, and drugs (e.g., antibiotics) (56). A recent metabolic reconstruction based on the data of the Human Microbiome Consortium clearly showed, however, that metabolic functionality was rather constant over a group of studied individuals because many biochemical pathways are redundant between alternative members of the microbiome (57).
Bacteria constitute, with 1014 citizens, the most dominant and most diverse group of microorganisms present in the human colon. Based on variation in 16S rRNA genes, it was assessed that there may be between 500 and 1,000 different species present, which belong to more than 70 genera (55). The three phyla Bacteroidetes (gram-negative), Firmicutes (gram-positive), and Actinobacteria (gram-positive) are the most abundant in the intestine. The Bacteroidetes phylum mainly produces acetate and propionate, whereas the Firmicutes phylum has butyrate as its primary metabolic end product (58). Most bacterial activity occurs in the proximal colon where substrate availability is highest. Toward the distal colon, the availability of substrate declines and the extraction of free water reduces diffusion of substrates and microbial products. This makes the proximal part of the colon the principal site of fermentation. Particularly, nondigestible carbohydrates are fermented in the proximal colon by saccharolytic bacteria, mainly primary fermenters like Bacteroidetes. This fermentation results in SCFAs together with the gases CO2 and H2 (12). The Bacteroidetes are part of a community, stabilized by mutual cross-feeding, where other members of the community consume these gasses. For instance, Archaea produce CH4 from CO2 and H2, while acetogens convert CO2 into acetate.
Nitrogen is essential for bacterial growth, and the hydrolysis of host-derived urea to NH3 is a major nitrogen source. Almost 50% of the urea produced by the host is hydrolyzed in the lumen of the large intestine (59). Fermentation of bacterial proteins and amino acids derived from primary fermenters like Bacteroidetes occurs in the more distal part of the colon by secondary fermenters: the proteolytic bacteria. Degradation of proteins and amino acids results in branched-chain fatty acids, accompanied by potentially toxic metabolites such as amines, phenolic compounds, and volatile sulfur compounds (60).
The bacterial pathways of anaerobic SCFA production
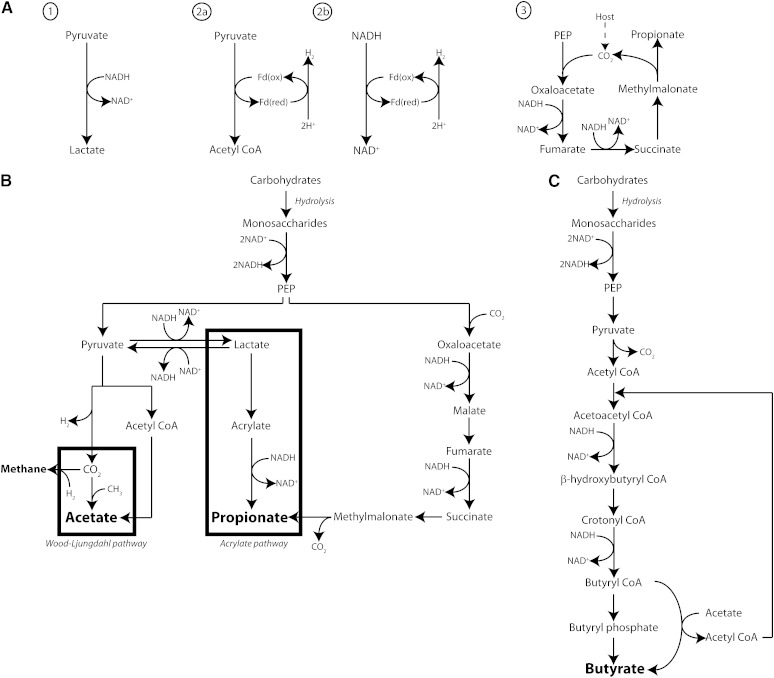
The microbiota hydrolyze nondigestible carbohydrates into oligosaccharides and then monosaccharides, which they ferment in the anaerobic environment of the gut. Major bacterial metabolic routes are the Embden-Meyerhof-Parnas pathway (glycolysis, for six-carbon sugars) and the pentose-phosphate pathway (for five-carbon sugars), which convert monosaccharides into phosphoenolpyruvate (PEP) (61). Subsequently, PEP is converted into fermentation products such as organic acids or alcohols.
At the level of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) the electron carrier NADH is formed. Anaerobically, there are three types of pathways to get rid of excess reducing equivalents (Fig. 1A). The first is the classical fermentation pathway where pyruvate is reduced to lactate or ethanol, thereby oxidizing NADH. Second, many primary fermenters sink their excess of reducing equivalents into molecular H2 (62). Two major routes are used to generate H2: 1) an exergonic (ΔGo′ < 0) route via pyruvate:ferredoxin oxidoreductase and ferredoxin hydrogenase; and 2) an endergonic (ΔGo′ > 0) route via NADH:ferredoxin oxidoreductase and ferredoxin hydrogenase. The latter proceeds only at a low H2 pressure in the lumen of the large intestine. Consequently, H2-consuming bacteria drive the metabolism of primary fermenters by depleting H2 (58). The third type of pathway is a primitive anaerobic electron transport chain (63, 64). It starts with the carboxylation of PEP and the resulting oxaloacetate is reduced to fumarate. Subsequently fumarate accepts electrons from NADH via a simple electron-transfer chain between NADH and fumarate. Two enzymes constitute this chain: NADH dehydrogenase and fumarate reductase. Protons are transported across the cell membrane by the NADH dehydrogenase, which are then used for chemiosmotic ATP synthesis. When the partial pressure of CO2 is low, succinate, the product of fumarate reductase, is converted into methylmalonate, which is cleaved into propionate and CO2. The latter can be recycled into PEP via carboxylation to form oxaloacetate.
Fig. 1.
Schematic overview of the three pathways that gut microbes use to get rid of excess reducing equivalents A: Pyruvate reduced to lactate thereby reducing NADH (1), pyruvate:ferredoxin oxidoreductase and hydrogenase (2a) or NADH:ferredoxin oxidoreductase and hydrogenase to sink reducing equivalents into molecular H2 (2b), and primitive anaerobic electron transport chain for reducing NADH (3). B, C: Schematic overview of the production of acetate, propionate, and butyrate from carbohydrates. B: Acetate is either formed directly from acetyl CoA or via the Wood-Ljungdahl pathway using formate. Propionate can be formed from PEP through the succinate decarboxylation pathway or through the acrylate pathway in which lactate is reduced to propionate. C: Condensation of two molecules of acetyl CoA results in butyrate by the enzyme butyrate-kinase or by utilizing exogenously derived acetate using the enzyme butyryl-CoA:acetate-CoA-transferase.
Major end products of the described fermentation pathways are the SCFAs. A major part of pyruvate is converted to acetyl-CoA with the concomitant formation of H2 and CO2. Acetate is either formed by hydrolysis of acetyl-CoA or from CO2 via the Wood-Ljungdahl pathway (Fig. 1B), in which CO2 is reduced to CO and converted with a methyl group and CoASH to acetyl-CoA (65, 66). Propionate can be formed via the primitive electron transfer chain using PEP as described above or by the reduction of lactate to propionate, the latter being called the acrylate pathway (61). Both pathways reduce additional NADH compared with the fermentation to lactate (Fig. 1B). Formation of butyrate starts from condensation of two molecules of acetyl-CoA and subsequent reduction to butyryl-CoA (Fig. 1C). Lactate-utilizing bacteria can produce butyrate by first producing acetyl-CoA from lactate (67). In the so-called classical pathway the enzymes phosphotransbutyrylase and butyrate kinase convert butyryl-CoA to butyrate and CoASH with the concomitant formation of ATP (68). However, recently an alternative pathway was discovered in which butyryl-CoA is converted by butyryl-CoA:acetate CoA-transferase to butyrate (69). The conversion utilizes exogenously derived acetate and generates butyrate and acetyl-CoA. This finding was supported by labeling studies, which showed that there was cross-feeding between acetate-producing and butyrate-producing bacteria (70, 71). The alternative pathway appears to dominate over the classical pathway in human gut microbiota (69).
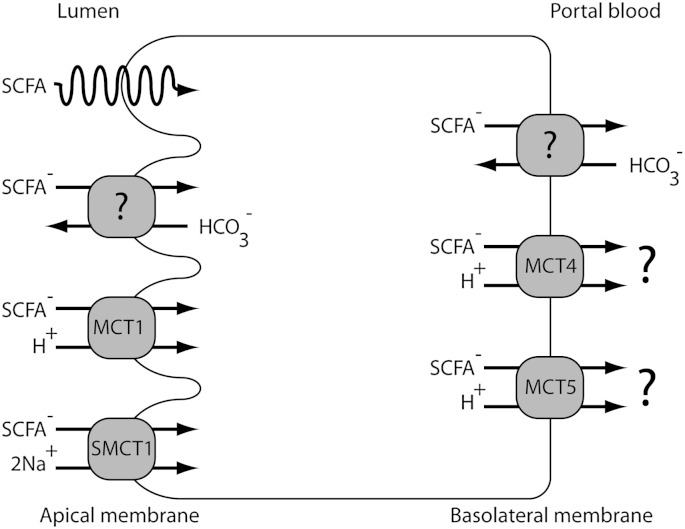
For the production of SCFAs, it is important that the gut microbiota work as a community, but also that the gut microbiota have symbiotic associations with the host. The molecular H2 that is produced during acetate formation must be used by other bacteria in the community to avoid accumulation of H2 which would inhibit the ability of primary fermenters to oxidize NADH. The CO2 that is needed in the primitive electron transfer chain is partly provided by the host. Humans produce on average about 0.7 kg of CO2 per day (72). Part of that production is excreted into the lumen of the gut as HCO3− in exchange for SCFA anions (see below and Fig. 2). Most likely this is an important pH regulatory mechanism because protons in the lumen of the gut, formed during the production of SCFAs, are neutralized by bicarbonate under the formation of CO2.
Fig. 2.
Schematic overview of the proposed transport mechanisms of SCFAs in colonocytes. Across the apical membrane the major part of SCFAs is transported in the dissociated form by an HCO3− exchanger of unknown identity (?) or by one of the known symporters, MCT1 or SMCT1. A small part may be transported via passive diffusion (spiral). The part of SCFAs that is not oxidized by the colonocytes is transported across the basolateral membrane. The basolateral transport can be mediated by an unknown HCO3− exchanger, MCT4, or MCT5.
Although much is known about the biochemistry of the conversion of carbohydrates into SCFAs by the bacteria composing the microbial community, there is a paucity of data on the production rates of SCFAs by the gut microbial community as a whole. This is largely due to the inability to sample the large intestine of man. Therefore, and as discussed in the previous section, the supply rate of SCFAs to the host remains enigmatic. There is a pressing need for measurement of true production rates of SCFAs, and the degree by which specific carbohydrates and microbiota influence the mass and composition of SCFAs.
The mutual relationship between microbial composition, microbial SCFA production, and the colonic milieu
The diet and the intestinal milieu interact in a complex way with the bacterial population in the gut. Fibers that lead to high amounts of SCFAs, lower the pH in the colon, which in turn affects the composition of the colonic microbiota and thereby the SCFA production.
Because most SCFAs are absorbed by the host in exchange for bicarbonate, the luminal pH is the result of the microbial SCFA production and the neutralizing capacity of bicarbonate. As the concentration of SCFAs decline from the proximal to the distal colon, the pH increases from cecum to rectum (11, 73–75). The drop in pH from the ileum to the cecum due to the higher SCFA concentrations has two effects. First, both in vitro and animal studies show that lower pH values change gut microbiota composition and second, it prevents overgrowth by pH-sensitive pathogenic bacteria like Enterobacteriaceae and Clostridia (51, 52, 54). Studies of human fecal microbial communities showed that at pH 5.5 the butyrate-producing bacteria such as Roseburia spp. and Faecalibacterium prausnitzii, both belonging to the Firmicutes phylum, comprised 20% of the total population (53). When fermentable dietary fibers become limiting in the more distal parts of the large intestine, the luminal pH increases to 6.5, the butyrate-producing bacteria almost completely disappear, and the acetate- and propionate-producing Bacteroides-related bacteria become dominant (53).
The interplay between diet, gut microbiota, and SCFA production was also found in rats fed different fibers. The cecum content differed in SCFA concentration, pH, and microbiota composition in the different fiber groups (76). After 14 days of diet, the rats fed oligosaccharide-containing diets showed higher cecal SCFA pools while pH was lower compared with control or cellulose diets. The oligosaccharide-containing diets resulted also in altered microbiota compositions as cecal bifidobacteria and total amounts of anaerobes were higher, whereas total aerobes were lower compared with rats fed the control diet. In addition, in vitro SCFA production rates from swine ileum were higher when the swine were put on galactooligosaccharide diets for 6 weeks compared with production rates before adaptation (Table 2) (44). Microbiota analysis showed that fecal bifidobacteria and lactobacilli were increased after adaptation. The changes in the intestinal lumen pH also affects the transport of SCFAs from the lumen to the colonocytes (8), which we will discuss more extensively below in the section about SCFA metabolism by the host.
THE EFFECTS OF SCFAs ON HOST METABOLISM
SCFAs produced by the microbiota in the cecum and the colon can be found in hepatic, portal, and peripheral blood (11, 77). These SCFAs affect lipid, glucose, and cholesterol metabolism in various tissues (17, 78–80). These results indicate that SCFAs are transported from the intestinal lumen into the blood compartment of the host and are taken up by organs where they act as substrates or signal molecules. SCFA transport has been studied mostly in colonocytes, the first host cells that take up SCFAs and which depend largely on butyrate for their energy supply (10). SCFA receptors constitute a new and rapidly growing field of research as more functions of these receptors are discovered (81–83). In this section we will discuss the transport and metabolism of SCFAs by the host as well as their regulatory role in energy metabolism of the host.
Transport of SCFAs across host cell membranes
Most SCFA transport studies have been performed in colonocytes, which form the cecal and colonic epithelium and are exposed to the highest SCFA concentrations. SCFAs are transported across the apical and the basolateral membranes of colonocytes (Fig. 2). For the apical uptake of SCFAs two mechanisms have been proposed, namely passive diffusion of undissociated SCFAs and active transport of dissociated SCFA anions mediated by a number of different transporters. With a pKa of ∼4.8 and a luminal pH around 6.0 (pH 5.5–6.5), only a very small part of the SCFAs is present in the undissociated form (84). Thus it is unlikely that passive diffusion of the undissociated form plays a major role.
Three mechanisms have been described for the transport of the SCFA anions across the apical membrane of the epithelial cells lining the gut. The first type of transporter couples the import of SCFA anions to HCO3− secretion into the intestinal lumen (Fig. 2). Conclusive evidence for the existence of SCFA-HCO3− exchange was obtained from vesicle studies in which it was shown that SCFA-HCO3− exchange was independent of Cl−-HCO3− exchange and Na+ transport (85–88). The identity of the transporter, however, remains unknown. Second, members of the family of monocarboxylate transporters (MCTs) catalyze SCFA anion cotransport with cations (85, 89). MCT1 (SLC16A1) was found in the apical membranes of enterocytes, and it transports SCFAs in an H+-dependent electroneutral manner, but it can also transport lactate and pyruvate (Fig. 2) (90). Finally, the electrogenic sodium-dependent monocarboxylate transporter (SMCT)1 (SLC5A8) is expressed along the entire length of the large intestine and is located in the apical membrane (91). SCFA anion transport by SMCT1 is coupled to Na+ transport in a 1:2 stoichiometry and stimulates Cl− and water absorption (Fig. 2) (92). SMCT1 transports butyrate faster than propionate and acetate. Recently, it was shown that SCFA anion transport by MCT dominates over transport by SMCT1 (93). An increased transport of SCFA anions across the apical membrane enhances the activity and expression of NHE3, an apical Na+/H+ exchanger, and thereby stimulates sodium and water absorption as well as deacidification of the cell (94).
The part of SCFAs that is not consumed by the colonocytes is transported across the basolateral membrane. SCFA anion transport across the basolateral membrane is probably mediated via the SCFA−-HCO3− antiport and the cation-SCFA anion symport (Fig. 2). The basolateral SCFA−-HCO3− antiporter is distinct from the apical SCFA−-HCO3− antiporter as indicated by their different Km values for butyrate, which are 1.5 mM and 17.5 mM for the apical and the basolateral exchanger, respectively (87, 95). Immunoblotting revealed that MCT4 (SLC16A3) and MCT5 (SLC16A4) were localized to the basolateral membrane (96). MCT4 transports SCFA anions in an H+-dependent electroneutral manner, but has a lower substrate affinity compared with MCT1 (97). Whether MCT5 is capable of transporting SCFAs is not known, as MCT5 has not been functionally characterized yet. Because the intracellular pH is higher than the pH in the intestinal lumen, all intracellular SCFAs are present in the dissociated form, implying that transport at the basolateral side should be via transporters only because no diffusion can occur.
The transporters for the uptake of SCFAs from the blood into the tissues remain largely unknown. Recently, the organic anion transporters OAT2 and OAT7 were found to transport propionate and butyrate, respectively, across the sinusoidal membrane of hepatocytes (98, 99). For a better understanding of the role of SCFAs in various tissues, the uptake by the different organs should be investigated further.
SCFAs as a source of energy
When taken up, a large part of the SCFAs is used as a source of energy. In humans, SCFAs provide ∼10% of the daily caloric requirements (31). CO2 production measurements in isolated colonocytes showed that colonocytes derive 60–70% of their energy supply from SCFA oxidation (100). The general idea is that colonocytes prefer butyrate to acetate and propionate, and oxidize it to ketone bodies and CO2 (100). This is based on the relatively high affinity of the colonocytes for butyrate. However, isolated colonocytes from humans and rats showed a maximum flux of 0.6, 0.2, and 0.4 μmol/min/g cell weight and a K0.5 of approximately 0.6, 0.4, and 0.1 mM for acetate, propionate, and butyrate, respectively (101, 102). This indicates that under physiological conditions, with a relative high colonic concentration of acetate compared with butyrate, acetate is at least as important as butyrate for the energy supply in colonocytes. In sudden death victims (n = 6), molar fractions of SCFAs in the hepatic portal vein were found to be 69:23:8 for acetate:propionate:butyrate, as compared with 57:22:21 in the large intestine (11). This is generally attributed to consumption of a large part of butyrate by colonocytes. Donohoe et al. (18) showed that colonocytes of germ-free mice exhibit a deficit in mitochondrial respiration and undergo autophagy. By introducing the butyrate-producing strain Butyrivibrio fibrisolvens into germ-free mice or by adding butyrate to isolated colonocytes of germ-free mice, they rescued the colonocytes from both the deficit in mitochondrial respiration and from autophagy. In the presence of an inhibitor for fatty acid oxidation, butyrate was unable to suppress autophagy. From this it was concluded that the rescue was due to butyrate acting as an energy source rather than as a regulator.
Exogenous acetate formed by colonic bacterial fermentation enters the blood compartment and is mixed with endogenous acetate released by tissues and organs (103, 104). Up to 70% of the acetate is taken up by the liver (105), where it is not only used as an energy source, but is also used as a substrate for the synthesis of cholesterol and long-chain fatty acids and as a cosubstrate for glutamine and glutamate synthesis. Other tissues including heart, adipose tissue, kidney, and muscle metabolize the remainder of acetate (104).
To prevent high SCFA concentrations in blood, the liver clears the major part of propionate and butyrate from the portal circulation (105). Propionate acts as a precursor for gluconeogenesis in the liver (6). In ruminants, with isotope dilution techniques, the contribution of propionate to glucose synthesis was calculated to vary between 45 and 60% (106). It is unclear if this is similar in nonruminants, because ruminants depend on SCFAs for 80% of their maintenance energy (31). After conversion of propionate into propionyl-CoA by propanoate:CoA ligase (AMP-forming), propionyl-CoA is converted to succinyl-CoA in three consecutive steps catalyzed by propionyl-CoA carboxylase, methylmalonyl-CoA epimerase, and methylmalonyl-CoA mutase. Succinyl-CoA enters the tricarboxylic acid (TCA) cycle and is converted to oxaloacetate, the precursor of gluconeogenesis (107). In humans the extent to which propionate contributes to energy metabolism is unknown due to the lack of data on true production rates of propionate. Concentrations of propionate in portal blood and hepatic venous blood suggest that around 30% of propionate is taken up by the liver (11, 105). Peripheral tissues take up the remainder of propionate because peripheral venous blood levels were 23% lower compared with hepatic venous blood levels. In another study it was estimated that humans use 50% of the propionate as a substrate for hepatic gluconeogenesis (108). The general view is that the liver clears a large fraction of propionate from the portal circulation, but absolute values are still unknown.
As discussed above, the major part of butyrate is used as fuel for colonocytes. The remainder is mostly oxidized by hepatocytes, which prevents toxic systemic concentrations (107).
Receptors of SCFAs
Next to the role as substrates, SCFA concentrations are also sensed by specific G protein-coupled receptors (GPRs), which are involved in the regulation of lipid and glucose metabolism. GPR41 and GPR43 were identified as SCFA receptors (109, 110), and two other GPRs of the same subfamily, GPR40 and GPR42, were found to be receptors for medium- and long-chain fatty acids and an open reading frame pseudogene of GPR41, respectively (81). After the discovery of the SCFA receptors, GPR41 was renamed free fatty acid receptor (Ffar)3 and GPR43 became Ffar2. Ffar2 and Ffar3 only share 33% amino acid identity and they differ in affinity for SCFAs, tissue distribution, and physiological roles. The distinct chain length:activity relationship for Ffar2 is acetate = propionate > butyrate, and for Ffar3, butyrate = propionate > acetate (109, 110). The two receptors have distinct G protein-coupling specificities: Ffar2 couples to both pertussis toxin-sensitive (Gi/o) and -insensitive (Gq) G proteins and Ffar3 only to Gi/o proteins (109, 110). Nilsson et al. (111) showed by a [Ca2+] mobilization assay in the presence of pertussis toxin that Ffar2 signals approximately for 70% through the Gi/o pathway.
The highest mRNA expression of Ffar2 was found in immune cells such as monocytes, B-lymphocytes, and polymorphonuclear cells (109–111). In addition, considerable mRNA expression was found in white and brown adipose tissue, bone marrow, spleen, pancreas, and large intestine (112). Ffar3 has a more widespread expression pattern than Ffar2, with the highest expression in adipose tissue. High mRNA expression was also found in the spleen, pancreas, lymph nodes, bone marrow, and polymorphonuclear cells (109–111). It is not known whether Ffar2 and Ffar3 reside on apical or basolateral membranes.
As discussed below, SCFA-Ffar pathways turn out to be involved in regulation of lipid and glucose metabolism (113–120).
Regulation of fatty acid metabolism by SCFAs
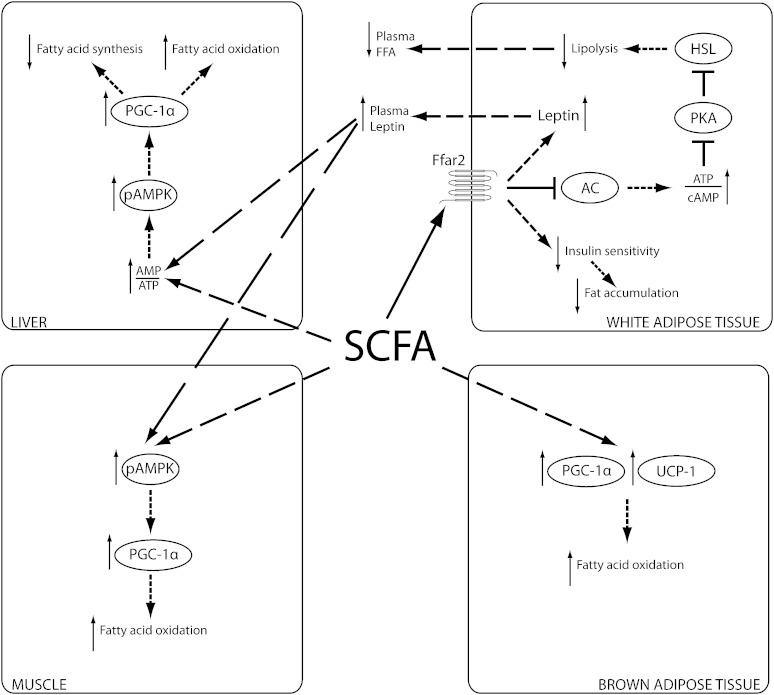
SCFAs regulate the balance between fatty acid synthesis, fatty acid oxidation, and lipolysis in the body. Fatty acid oxidation is activated by SCFAs, while de novo synthesis and lipolysis are inhibited. The net result is a reduction of the concentrations of free fatty acids in plasma (114) and a decrease in body weight (17, 121–124). In this section we discuss the signaling pathways that mediate this regulation. Besides the receptors Ffar2 and Ffar3 that we discussed above, AMP-activated protein kinase (AMPK) plays an important role in this regulation, as summarized in Fig. 3.
Fig. 3.
Schematic overview of the proposed mechanisms by which SCFAs increase fatty acid oxidation in liver, muscle, and brown adipose tissue. In muscle and liver, SCFAs phosphorylate and activate AMPK (pAMPK) directly by increasing the AMP/ATP ratio and indirectly via the Ffar2-leptin pathway in white adipose tissue. In white adipose tissue, SCFAs decrease insulin sensitivity via Ffar2 and thereby decrease fat storage. In addition, binding of SCFAs to Ffar2 leads to the release of the Gi/o protein, the subsequent inhibition of adenylate cyclase (AC), and an increase of the ATP/cAMP ratio. This, in turn, leads to the inhibition of PKA and the subsequent inhibition of HSL, leading to a decreased lipolysis and reduced plasma free fatty acids.
SCFAs have been shown to increase the AMPK activity in liver and muscle tissue (17, 121, 125). Activation of AMPK triggers peroxisome proliferator-activated receptor gamma coactivator (PGC)-1α expression, which is known to control the transcriptional activity of several transcription factors such as peroxisome proliferator-activated receptor (PPAR)α, PPARδ, PPARγ, liver X receptor (LXR), and farnesoid X receptor (FXR), all important in regulation of cholesterol, lipid, and glucose metabolism (126, 127). As a consequence, fatty acid oxidation is enhanced in both tissues and de novo fatty acid synthesis in the liver is decreased. In addition, SCFAs have been shown to increase protein expression of PGC-1α and uncoupling protein (UCP)-1 in brown adipose tissue, thereby increasing thermogenesis and fatty acid oxidation (17). If AMPK is involved in this effect of SCFAs, however, is still unknown. SCFAs activate AMPK either directly by increasing the AMP/ATP ratio or indirectly via the Ffar2-leptin pathway. In vitro studies showed that SCFAs increased the AMP/ATP ratio and AMPK activity in both muscle and liver cells in a leptin-independent manner (17, 123), but the mechanism is still unknown. In vitro and in vivo experiments showed that SCFAs increase leptin expression via a Ffar2-dependent pathway (113, 118, 119). Leptin, an adipokine that regulates energy expenditure and food intake, stimulates fatty acid oxidation by increasing the AMP/ATP ratio and AMPK activity in liver and muscle tissue (128, 129). To what extent the AMPK-activated effect of SCFAs in vivo is regulated via leptin or via the leptin-independent mechanism is still unknown.
Hepatic fatty acid lipolysis seems to be unaffected by SCFAs, but lipolysis in adipose tissue is strongly reduced by SCFAs (113, 114, 121, 130). In isolated adipocytes, acetate and propionate were found to inhibit lipolysis via Ffar2 activation (113, 114). A reduction of lipolysis is consistent with data from human studies where intravenous administration of acetate and propionate reduced plasma free fatty acids and glycerol (131, 132). Ffar2 mediated inhibition of lipolysis is most likely through inactivation of the hormone-sensitive lipase (HSL), which hydrolyzes triglycerides and is one of the key molecules controlling lipolysis in adipose tissue (133). Binding of SCFAs to Ffar2 leads to the dissociation and thereby the activation of the Gi/o protein. The Gi/o protein inhibits adenylate cyclase and thereby reduces the production of cAMP from ATP, which subsequently decreases the activity of protein kinase A (PKA) (134). A decrease of PKA activity leads to dephosphorylation and deactivation of HSL in adipose tissue (133). Consistently, administration of high resistant starch to humans resulted in higher plasma SCFA concentrations and lower HSL activity in adipose tissue (130).
Ffar2 also plays an important role in storage of fat in white adipose tissue as shown recently by Kimura et al. (135). Ffar2-deficient mice are obese on a normal diet, whereas mice overexpressing Ffar2 specifically in adipose tissue are protected against dietary-induced obesity. The authors concluded that SCFA activation of adipose-specific Ffar2 suppresses insulin signaling by inhibition of Akt phosphorylation, which inhibits fat storage in adipose tissue and promotes the metabolism of lipids and glucose in other tissues. Indeed, liver triglycerides were decreased and mRNA levels of genes involved in fatty acid oxidation in muscle tissue were increased in mice overexpressing adipose-specific Ffar2 compared with wild-type controls. In addition, total body energy expenditure was also increased together with a decreased respiratory exchange ratio value, indicating increased fatty acid oxidation. Unfortunately, no data was provided on the AMP/ATP ratio, AMPK activity, and actual organ-specific fatty acid oxidation fluxes. Surprisingly, plasma leptin levels in adult mice overexpressing adipose-specific Ffar2 were lower than in wild-type mice. Although SCFAs have been shown to increase leptin expression via a Ffar2-dependent pathway, it is possible that the decreased leptin levels are simply a result of decreased adipose tissue (136).
In conclusion, it has been shown convincingly that the prevention of dietary-induced obesity by SCFAs can be attributed to an increase of fatty acid oxidation in multiple tissues and a decrease of fat storage in white adipose tissue. However, our understanding of the molecular mechanisms is still incomplete.
Regulation of glucose metabolism by SCFAs
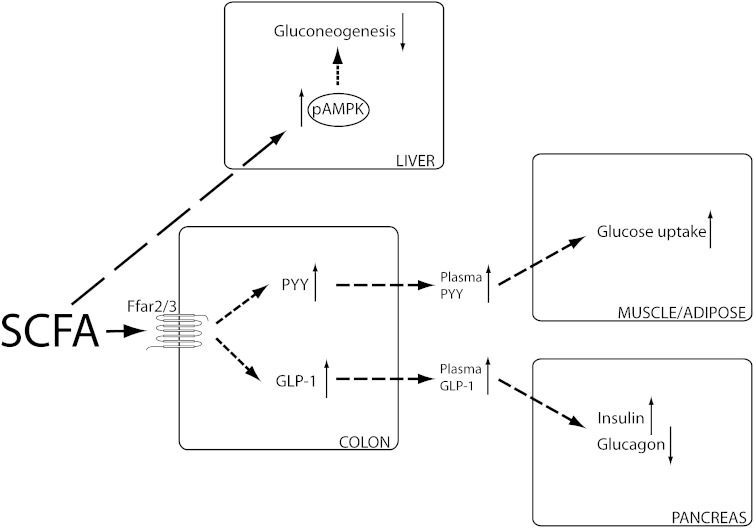
The scarce data available on the effect of SCFAs on glucose metabolism reveal a decrease of plasma glucose levels possibly via multiple mechanisms. The plasma glucose level is determined by uptake via the food, gluconeogenesis, and uptake by multiple organs. Again, the Ffars and AMPK are involved in transduction of the effects of SCFAs (Fig. 4). In addition, the gut hormones peptide YY (PYY) and glucagon-like peptide-1 (GLP-1) play an important role in the communication between tissues.
Fig. 4.
Schematic overview of the proposed mechanisms by which SCFAs effect glucose metabolism. In the colon SCFAs can increase PYY and GLP-1 expression via Ffar2 and Ffar3. PYY has been shown to increase glucose uptake in muscle and adipose tissue, whereas GLP-1 increases insulin and decreases glucagon production in the pancreas. In addition, SCFAs have been shown to decrease hepatic gluconeogenesis by increasing the AMPK phosphorylation and activity.
Oral administration of acetate and propionate reduced glycemia in diabetic hyperglycemic KK-A(y) mice and normal rats (137, 138). There is indirect evidence for a reduced gluconeogenesis by the liver. Activation of the hepatic AMPK pathway decreased gene expression of the gluconeogenic enzymes glucose 6-phosphatase (G6Pase) and phosphoenolpyruvate carboxykinase (PEPCK). Unfortunately, the gluconeogenic flux was not measured, but fasting plasma glucose and insulin levels were decreased together with an increased glucose tolerance (137).
SCFAs may also affect plasma glucose levels by increasing the gut hormones PYY and GLP-1 via activation of the receptors Ffar2 and Ffar3. PYY is known as a satiety hormone, but it also reinforces the insulin action on glucose disposal in muscle and adipose tissue (139–141). In human and rat colon samples, the SCFA receptors Ffar2 and Ffar3 colocalize with enteroendocrine L cells containing PYY (142–144). In addition, Ffar2 and Ffar3 knockout mice showed reduced colonic PYY expression and whole-body glucose tolerance (145). Intracolonic infusions of SCFAs in rats and pigs increased blood concentrations of PYY, but unfortunately no data on glucose metabolism was reported (146, 147). GLP-1 indirectly regulates blood glucose levels by increasing the secretion of insulin and decreasing the secretion of glucagon by the pancreas (148). Intracolonic infusions of SCFAs and intake of fibers both increased plasma GLP-1 concentrations and glucose uptake by adipose tissue (147, 149–151). In addition, mice lacking Ffar2 or Ffar3 exhibited reduced SCFA-triggered GLP-1 secretion in vitro and in vivo, and a parallel impairment of glucose tolerance (145).
In summary, SCFAs seem to beneficially affect glucose metabolism by normalizing plasma glucose levels and increasing glucose handling. To what extent these effects occur directly via a hepatic AMPK regulation pathway, or indirectly via the gut derived hormones PYY and GLP-1, is not clear.
Regulation of cholesterol metabolism by SCFAs
SCFAs have been shown to reduce plasma concentrations of cholesterol in rodents and humans (78, 79, 124). Cholesterol is synthesized from its precursor unit, acetyl-CoA, via a complex metabolic pathway in which 3-hydroxy-3-methylglutaryl-CoA reductase is the rate-limiting enzyme (152).
In vitro studies showed that propionate lowered cholesterol synthesis rate by decreasing the enzyme activity of hepatic 3-hydroxy-3-methylglutaryl-CoA synthase (HMGCS) and 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) (152, 153). In addition, in vivo experiments using 3H2O as a tracer showed that total cholesterol synthesis rate was decreased in rat livers upon addition of dietary propionate (154, 155). The role of acetate in cholesterol homeostasis has received less attention, but Fushimi et al. (78) showed that serum cholesterol levels are affected by acetate. Rats receiving a diet containing 1% (w/w) cholesterol showed significantly less increased serum cholesterol levels when the diet was supplemented with 0.3% (w/w) acetate. In the liver, the protein concentration of HMGCS was reduced and the mRNA level of cholesterol 7α-hydroxylase (CYP7A1) was increased upon addition of acetate. CYP7A1 is involved in the conversion of cholesterol to bile acid, and acts as a sink for cholesterol. In line with this observation, acetate supplementation decreased hypercholesterolemia in humans (124).
Because AMPK activation has also been reported to inhibit HMGCR activity and reduce cholesterol levels in isolated rat hepatocytes (156–158), it is not unlikely that the cholesterol-lowering effects described are mediated through AMPK activation by SCFAs, just like the effects of SCFAs on fatty acid and glucose metabolism.
THE INTERPLAY BETWEEN GUT MICROBIOTA, SCFA CONCENTRATIONS, AND HOST ENERGY METABOLISM
The complexity of the interactions between gut microbiota, SCFA concentrations, and host energy metabolism is illustrated by contradictory reports in obese and germ-free subjects. Dietary administration of SCFAs protected mice from diet-induced obesity and insulin resistance (17, 121, 122). Yet, genetically obese ob/ob mice and obese human subjects have increased amounts of cecal and fecal SCFAs (159–161). It is unclear whether the beneficial effect of SCFAs is somehow compromised in obese subjects, or whether the effect is simply not strong enough to compensate for an adverse diet or genetic predisposition.
Another puzzling result is that despite very low SCFA levels, germ-free mice and rats are protected from diet-induced obesity (162, 163). In this respect it is important to note that the type of microbiota is of key importance. A conventionalization study of adult germ-free mice with microbiota from obese mice (ob/ob) exhibited a significantly greater percentage increase in total body fat than colonization with microbiota from lean (+/+) donors (159). The obese animals in this study showed a 50% reduction in relative abundance of the Bacteroidetes (i.e., acetate and propionate producers), whereas the Firmicutes (i.e., butyrate producers) were proportionally increased compared with the lean counterparts. Comparative metagenomic analysis predicted that the microbiota from ob/ob mice had an increased fermentation capacity, which was also shown in increased cecal concentrations of SCFAs. From this, it was hypothesized that the efficiency of energy harvesting from the diet is increased by a change in gut microbiota, which then might lead to obesity. To test this hypothesis, Murphy et al. (160) fed wild-type mice and ob/ob mice either a high-fat or a low-fat diet and investigated the relationship between the microbial composition and energy harvesting capacity (deduced from the cecal SCFA concentrations). The decrease of Bacteroidetes and the increase of Firmicutes were confirmed, but they did not see a direct association between changes in the microbiota and markers of energy harvesting. This and other studies are, however, limited by a lack of flux data. A priori, there is no reason why cecal SCFA concentrations reflect the SCFA flux to the host and thereby the additional energy harvest.
In humans the distinct relation between the Firmicutes:Bacteroidetes ratio and obesity is less clear. Multiple studies found a higher Firmicutes:Bacteroidetes ratio and an increased amount of SCFAs in the stool samples of obese people compared with lean people (159, 164, 165). In contrast, Schwiertz et al. (161) found no changes in Firmicutes but an increase in Bacteroidetes in obese humans compared with lean humans. In agreement with earlier studies, the latter also reported an increase in total fecal SCFA concentrations in obese humans.
OUTLOOK
SCFAs have unambiguously been shown to exert multiple beneficial effects on various aspects of mammalian energy metabolism. An ever increasing detail in our understanding of the underlying molecular mechanisms, however, does not yet allow us to understand paradoxical results in physiological studies. Partly this is caused by the lack of human data, because not all results obtained in rodents can be directly translated to humans. More fundamentally, the field is severely hampered by the lack of data on actual fluxes of SCFAs and metabolic processes regulated by SCFAs. Most studies report concentrations of metabolites (fatty acids, glucose, cholesterol, etc.) or transcript levels, but these do not necessarily reflect flux changes. A number of questions need to be addressed: 1) What are the in vivo SCFA production and uptake fluxes under different conditions (i.e., with different fibers, with different microbiota, or in different disease models)? 2) How do these SCFAs then affect glucose and lipid fluxes via their dual role as substrates and regulators? 3) Can we quantify the role of different tissues and hormones? 4) Does the demand of the host for specific SCFAs drive a change in microbial metabolism? 5) At which timescales are different, apparently contradictory effects working?
A quantitative and time-resolved approach to these questions should bring us a great step forward to elucidate the role of SCFAs in mammalian energy metabolism.
Footnotes
Abbreviations:
- AMPK
- AMP-activated protein kinase
- Ffar
- free fatty acid receptor
- GLP-1
- glucagon-like peptide-1
- GPR
- G protein-coupled receptor
- HSL
- hormone-sensitive lipase
- MCT
- monocarboxylate transporter
- PEP
- phosphoenolpyruvate
- PGC
- peroxisome proliferator-activated receptor gamma coactivator
- PKA
- protein kinase A
- PPAR
- peroxisome proliferator-activated receptor
- PYY
- peptide YY
- SCFA
- short-chain fatty acid
- SMCT
- sodium-dependent monocarboxylate transporter
This work was funded by the Netherlands Genomics Initiative via the Netherlands Consortium for Systems Biology.
REFERENCES
- 1.Galisteo M., Duarte J., Zarzuelo A. 2008. Effects of dietary fibers on disturbances clustered in the metabolic syndrome. J. Nutr. Biochem. 19: 71–84. [DOI] [PubMed] [Google Scholar]
- 2.Venn B. J., Mann J. I. 2004. Cereal grains, legumes and diabetes. Eur. J. Clin. Nutr. 58: 1443–1461. [DOI] [PubMed] [Google Scholar]
- 3.Delzenne N. M., Cani P. D. 2005. A place for dietary fibre in the management of the metabolic syndrome. Curr. Opin. Clin. Nutr. Metab. Care. 8: 636–640. [DOI] [PubMed] [Google Scholar]
- 4.Marlett J. A., McBurney M. I., Slavin J. L. 2002. Position of the American Dietetic Association: health implications of dietary fiber. J. Am. Diet. Assoc. 102: 993–1000. [DOI] [PubMed] [Google Scholar]
- 5.Nicholson J. K., Holmes E., Kinross J., Burcelin R., Gibson G., Jia W., Pettersson S. 2012. Host-gut microbiota metabolic interactions. Science. 336: 1262–1267. [DOI] [PubMed] [Google Scholar]
- 6.Roy C. C., Kien C. L., Bouthillier L., Levy E. 2006. Short-chain fatty acids: ready for prime time? Nutr. Clin. Pract. 21: 351–366. [DOI] [PubMed] [Google Scholar]
- 7.van Hoek M. J., Merks R. M. 2012. Redox balance is key to explaining full vs. partial switching to low-yield metabolism. BMC Syst. Biol. 6: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook S. I., Sellin J. H. 1998. Review article: short chain fatty acids in health and disease. Aliment. Pharmacol. Ther. 12: 499–507. [DOI] [PubMed] [Google Scholar]
- 9.Hijova E., Chmelarova A. 2007. Short chain fatty acids and colonic health. Bratisl. Lek. Listy. 108: 354–358. [PubMed] [Google Scholar]
- 10.Binder H. J. 2010. Role of colonic short-chain fatty acid transport in diarrhea. Annu. Rev. Physiol. 72: 297–313. [DOI] [PubMed] [Google Scholar]
- 11.Cummings J. H., Pomare E. W., Branch W. J., Naylor C. P., Macfarlane G. T. 1987. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut. 28: 1221–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Topping D. L., Clifton P. M. 2001. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol. Rev. 81: 1031–1064. [DOI] [PubMed] [Google Scholar]
- 13.Ruppin H., Bar-Meir S., Soergel K. H., Wood C. M., Schmitt M. G. J. 1980. Absorption of short-chain fatty acids by the colon. Gastroenterology. 78: 1500–1507. [PubMed] [Google Scholar]
- 14.Dawson A. M., Holdsworth C. D., Webb J. 1964. Absorption of short chain fatty acids in man. Proc. Soc. Exp. Biol. Med. 117: 97–100. [DOI] [PubMed] [Google Scholar]
- 15.Rechkemmer G., Rönnau K., Engelhardt W. V. 1988. Fermentation of polysaccharides and absorption of short chain fatty acids in the mammalian hindgut. Comp. Biochem. Physiol. A. 90: 563–568. [DOI] [PubMed] [Google Scholar]
- 16.Hu G. X., Chen G. R., Xu H., Ge R. S., Lin J. 2010. Activation of the AMP activated protein kinase by short-chain fatty acids is the main mechanism underlying the beneficial effect of a high fiber diet on the metabolic syndrome. Med. Hypotheses. 74: 123–126. [DOI] [PubMed] [Google Scholar]
- 17.Gao Z., Yin J., Zhang J., Ward R. E., Martin R. J., Lefevre M., Cefalu W. T., Ye J. 2009. Butyrate improves insulin sensitivity and increases energy expenditure in mice. Diabetes. 58: 1509–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donohoe D. R., Garge N., Zhang X., Sun W., O'Connell T. M., Bunger M. K., Bultman S. J. 2011. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 13: 517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blouin J. M., Penot G., Collinet M., Nacfer M., Forest C., Laurent-Puig P., Coumoul X., Barouki R., Benelli C., Bortoli S. 2011. Butyrate elicits a metabolic switch in human colon cancer cells by targeting the pyruvate dehydrogenase complex. Int. J. Cancer. 128: 2591–2601. [DOI] [PubMed] [Google Scholar]
- 20.Scharlau D., Borowicki A., Habermann N., Hofmann T., Klenow S., Miene C., Munjal U., Stein K., Glei M. 2009. Mechanisms of primary cancer prevention by butyrate and other products formed during gut flora-mediated fermentation of dietary fibre. Mutat. Res. 682: 39–53. [DOI] [PubMed] [Google Scholar]
- 21.Tang Y., Chen Y., Jiang H., Robbins G. T., Nie D. 2011. G-protein-coupled receptor for short-chain fatty acids suppresses colon cancer. Int. J. Cancer. 128: 847–856. [DOI] [PubMed] [Google Scholar]
- 22.Hamer H. M., Jonkers D., Venema K., Vanhoutvin S., Troost F. J., Brummer R. J. 2008. Review article: the role of butyrate on colonic function. Aliment. Pharmacol. Ther. 27: 104–119. [DOI] [PubMed] [Google Scholar]
- 23.Harig J. M., Soergel K. H., Komorowski R. A., Wood C. M. 1989. Treatment of diversion colitis with short-chain-fatty acid irrigation. N. Engl. J. Med. 320: 23–28. [DOI] [PubMed] [Google Scholar]
- 24.Breuer R. I., Buto S. K., Christ M. L., Bean J., Vernia P., Paoluzi P., Di Paolo M. C., Caprilli R. 1991. Rectal irrigation with short-chain fatty acids for distal ulcerative colitis. Preliminary report. Dig. Dis. Sci. 36: 185–187. [DOI] [PubMed] [Google Scholar]
- 25.Vernia P., Marcheggiano A., Caprilli R., Frieri G., Corrao G., Valpiani D., Di Paolo M. C., Paoluzi P., Torsoli A. 1995. Short-chain fatty acid topical treatment in distal ulcerative colitis. Aliment. Pharmacol. Ther. 9: 309–313. [DOI] [PubMed] [Google Scholar]
- 26.Scheppach W. 1996. Treatment of distal ulcerative colitis with short-chain fatty acid enemas. A placebo-controlled trial. German-Austrian SCFA Study Group. Dig. Dis. Sci. 41: 2254–2259. [DOI] [PubMed] [Google Scholar]
- 27.Di Sabatino A., Morera R., Ciccocioppo R., Cazzola P., Gotti S., Tinozzi F. P., Tinozzi S., Corazza G. R. 2005. Oral butyrate for mildly to moderately active Crohn's disease. Aliment. Pharmacol. Ther. 22: 789–794. [DOI] [PubMed] [Google Scholar]
- 28.Flint H. J., Bayer E. A., Rincon M. T., Lamed R., White B. A. 2008. Polysaccharide utilization by gut bacteria potential for new insights from genomic analysis. Nat. Rev. Microbiol. 6: 121–131. [DOI] [PubMed] [Google Scholar]
- 29.Bingham S. A., Day N. E., Luben R., Ferrari P., Slimani N., Norat T., Clavel-Chapelon F., Kesse E., Nieters A., Boeing H., et al. ; European Prospective Investigation into Cancer and Nutrition. 2003. Dietary fibre in food and protection against colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC): an observational study. Lancet. 361: 1496–1501. [DOI] [PubMed] [Google Scholar]
- 30.Musso G., Gambino R., Cassader M. 2011. Interactions between gut microbiota and host metabolism predisposing to obesity and diabetes. Annu. Rev. Med. 62: 361–380. [DOI] [PubMed] [Google Scholar]
- 31.Bergman E. N. 1990. Energy contributions of volatile fatty acids from the gastrointestinal tract in various species. Physiol. Rev. 70: 567–590. [DOI] [PubMed] [Google Scholar]
- 32.Levrat M. A., Rémésy C., Demigné C. 1991. High propionic acid fermentations and mineral accumulation in the cecum of rats adapted to different levels of inulin. J. Nutr. 121: 1730–1737. [DOI] [PubMed] [Google Scholar]
- 33.Hedemann M. S., Theil P. K., Bach Knudsen K. E. 2009. The thickness of the intestinal mucous layer in the colon of rats fed various sources of non-digestible carbohydrates. Br. J. Nutr. 102: 117–125. [DOI] [PubMed] [Google Scholar]
- 34.Marsono Y., Illman R. J., Clarke J. M., Trimble R. P., Topping D. L. 1993. Plasma lipids and large bowel volatile fatty acids in pigs fed on white rice, brown rice and rice bran. Br. J. Nutr. 70: 503–513. [DOI] [PubMed] [Google Scholar]
- 35.Bird A. R., Hayakawa T., Marsono Y., Gooden J. M., Record I. R., Correll R. L., Topping D. L. 2000. Coarse brown rice increases fecal and large bowel short-chain fatty acids and starch but lowers calcium in the large bowel of pigs. J. Nutr. 130: 1780–1787. [DOI] [PubMed] [Google Scholar]
- 36.Haenen D., Zhang J., Souza da Silva C., Bosch G., van der Meer I. M., van Arkel J., van den Borne J. J., Pérez Gutiérrez O., Smidt H., Kemp B., et al. 2013. A diet high in resistant starch modulates microbiota composition, SCFA concentrations, and gene expression in pig intestine. J. Nutr. 143: 274–283. [DOI] [PubMed] [Google Scholar]
- 37.Topping D. L., Illman R. J., Clarke J. M., Trimble R. P., Jackson K. A., Marsono Y. 1993. Dietary fat and fiber alter large bowel and portal venous volatile fatty acids and plasma cholesterol but not biliary steroids in pigs. J. Nutr. 123: 133–143. [DOI] [PubMed] [Google Scholar]
- 38.Cummings J. H., Beatty E. R., Kingman S. M., Bingham S. A., Englyst H. N. 1996. Digestion and physiological properties of resistant starch in the human large bowel. Br. J. Nutr. 75: 733–747. [DOI] [PubMed] [Google Scholar]
- 39.van Munster I. P., Tangerman A., Nagengast F. M. 1994. Effect of resistant starch on colonic fermentation, bile acid metabolism, and mucosal proliferation. Dig. Dis. Sci. 39: 834–842. [DOI] [PubMed] [Google Scholar]
- 40.Holt P. R., Atillasoy E., Lindenbaum J., Ho S. B., Lupton J. R., McMahon D., Moss S. F. 1996. Effects of acarbose on fecal nutrients, colonic pH, and short-chain fatty acids and rectal proliferative indices. Metabolism. 45: 1179–1187. [DOI] [PubMed] [Google Scholar]
- 41.Fleming S. E., O'Donnell A. U., Perman J. A. 1985. Influence of frequent and long-term bean consumption on colonic function and fermentation. Am. J. Clin. Nutr. 41: 909–918. [DOI] [PubMed] [Google Scholar]
- 42.Jenkins D. J. A., Vuksan V., Kendall C. W. C., Wursch P., Jeffcoat R., Waring S., Mehling C. C., Vidgen E., Augustin L. S. A., Wong E. 1998. Physiological effects of resistant starches on fecal bulk, short chain fatty acids, blood lipids and glycemic index. J. Am. Coll. Nutr. 17: 609–616. [DOI] [PubMed] [Google Scholar]
- 43.Holtug K., Rasmussen H. S., Mortensen P. B. 1992. An in vitro study of short-chain fatty acid concentrations, production and absorption in pig (Sus scrofa) colon. Comp. Biochem. Physiol. Comp. Physiol. 103: 189–197. [DOI] [PubMed] [Google Scholar]
- 44.Smiricky-Tjardes M. R., Grieshop C. M., Flickinger E. A., Bauer L. L., Fahey G. C. 2003. Dietary galactooligosaccharides affect ileal and total-tract nutrient digestibility, ileal and fecal bacterial concentrations, and ileal fermentative characteristics of growing pigs. J. Anim. Sci. 81: 2535–2545. [DOI] [PubMed] [Google Scholar]
- 45.Velázquez M., Davies C., Marett R., Slavin J. L., Feirtag J. M. 2000. Effect of oligosaccharides and fibre substitutes on short-chain fatty acid production by human faecal microflora. Anaerobe. 6: 87–92. [Google Scholar]
- 46.Bourquin L. D., Titgemeyer E. C., Garleb K. A., Fahey G. C. 1992. Short-chain fatty acid production and fiber degradation by human colonic bacteria: effects of substrate and cell wall fractionation procedures. J. Nutr. 122: 1508–1520. [DOI] [PubMed] [Google Scholar]
- 47.Bergman E. N., Reid R. S., Murray M. G., Brockway J. M., Whitelaw F. G. 1965. Interconversions and production of volatile fatty acids in the sheep rumen. Biochem. J. 97: 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pouteau E., Vahedi K., Messing B., Flourie B., Nguyen P., Darmaun D., Krempf M. 1998. Production rate of acetate during colonic fermentation of lactulose: a stable-isotope study in humans. Am. J. Clin. Nutr. 68: 1276–1283. [DOI] [PubMed] [Google Scholar]
- 49.Pouteau E., Nguyen P., Ballevre O., Krempf M. 2003. Production rates and metabolism of short-chain fatty acids in the colon and whole body using stable isotopes. Proc. Nutr. Soc. 62: 87–93. [DOI] [PubMed] [Google Scholar]
- 50.Thompson G. N., Walter J. H., Bresson J. L., Ford G. C., Lyonnet S. L., Chalmers R. A., Saudubray J. M., Leonard J. V., Halliday D. 1990. Sources of propionate in inborn errors of propionate metabolism. Metabolism. 39: 1133–1137. [DOI] [PubMed] [Google Scholar]
- 51.Cherrington C. A., Hinton M., Pearson G. R., Chopra I. 1991. Short-chain organic acids at ph 5.0 kill Escherichia coli and Salmonella spp. without causing membrane perturbation. J. Appl. Bacteriol. 70: 161–165. [DOI] [PubMed] [Google Scholar]
- 52.Prohászka L., Jayarao B. M., Fábián A., Kovács S. 1990. The role of intestinal volatile fatty acids in the Salmonella shedding of pigs. Zentralbl. Veterinarmed. B. 37: 570–574. [DOI] [PubMed] [Google Scholar]
- 53.Walker A. W., Duncan S. H., McWilliam Leitch E. C., Child M. W., Flint H. J. 2005. pH and peptide supply can radically alter bacterial populations and short-chain fatty acid ratios within microbial communities from the human colon. Appl. Environ. Microbiol. 71: 3692–3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duncan S. H., Louis P., Thomson J. M., Flint H. J. 2009. The role of pH in determining the species composition of the human colonic microbiota. Environ. Microbiol. 11: 2112–2122. [DOI] [PubMed] [Google Scholar]
- 55.Xu J., Gordon J. I. 2003. Honor thy symbionts. Proc. Natl. Acad. Sci. USA. 100: 10452–10459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zoetendal E. G., Akkermans A. D. L., Akkermans-van Vliet W. M., de Visser J. A. G. M., de Vos W. M. 2001. The host genotype affects the bacterial community in the human gastrointestinal tract. Microb. Ecol. Health Dis. 13: 129–134. [Google Scholar]
- 57.Abubucker S., Segata N., Goll J., Schubert A. M., Izard J. 2012. Metabolic reconstruction for metagenomic data and its application to the human microbiome. PLOS Comput. Biol. 8: e1002358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Macfarlane S., Macfarlane G. T. 2003. Regulation of short-chain fatty acid production. Proc. Nutr. Soc. 62: 67–72. [DOI] [PubMed] [Google Scholar]
- 59.Veeneman J. M., Kingma H. A., Stellaard F., de Jong P. E., Reijngoud D., Huisman R. M. 2004. Comparison of amino acid oxidation and urea metabolism in haemodialysis patients during fasting and meal intake. Nephrol. Dial. Transplant. 19: 1533–1541. [DOI] [PubMed] [Google Scholar]
- 60.Millet S., Van Oeckel M. J., Aluwé M., Delezie E., De Brabander D. L. 2010. Prediction of in vivo short-chain fatty acid production in hindgut fermenting mammals: problems and pitfalls. Crit. Rev. Food Sci. Nutr. 50: 605–619. [DOI] [PubMed] [Google Scholar]
- 61.Miller T. L., Wolin M. J. 1996. Pathways of acetate, propionate, and butyrate formation by the human fecal microbial flora. Appl. Environ. Microbiol. 62: 1589–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fischbach M. A., Sonnenburg J. L. 2011. Eating for two: how metabolism establishes interspecies interactions in the gut. Cell Host Microbe. 10: 336–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Macy J. M., Ljungdahl L. G., Gottschalk G. 1978. Pathway of succinate and propionate formation in Bacteroides fragilis. J. Bacteriol. 134: 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Macy J. M., Probst I. 1979. The biology of gastrointestinal bacteroides. Annu. Rev. Microbiol. 33: 561–594. [DOI] [PubMed] [Google Scholar]
- 65.Pryde S. E., Duncan S. H., Hold G. L., Stewart C. S., Flint H. J. 2002. The microbiology of butyrate formation in the human colon. FEMS Microbiol. Lett. 217: 133–139. [DOI] [PubMed] [Google Scholar]
- 66.Ragsdale S. W., Pierce E. 2008. Acetogenesis and the Wood-Ljungdahl pathway of CO(2) fixation. Biochim. Biophys. Acta. 1784: 1873–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Duncan S. H., Louis P., Flint H. J. 2004. Lactate-utilizing bacteria, isolated from human feces, that produce butyrate as a major fermentation product. Appl. Environ. Microbiol. 70: 5810–5817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Louis P., Flint H. J. 2009. Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiol. Lett. 294: 1–8. [DOI] [PubMed] [Google Scholar]
- 69.Duncan S. H., Barcenilla A., Stewart C. S., Pryde S. E., Flint H. J. 2002. Acetate Utilization and butyryl coenzyme A (CoA):acetate-CoA transferase in butyrate-producing bacteria from the human large intestine. Appl. Environ. Microbiol. 68: 5186–5190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Venema K. 2010. Role of gut microbiota in the control of energy and carbohydrate metabolism. Curr. Opin. Clin. Nutr. Metab. Care. 13: 432–438. [DOI] [PubMed] [Google Scholar]
- 71.Duncan S. H., Holtrop G., Lobley G. E., Calder A. G., Stewart C. S., Flint H. J. 2004. Contribution of acetate to butyrate formation by human faecal bacteria. Br. J. Nutr. 91: 915–923. [DOI] [PubMed] [Google Scholar]
- 72.el-Khoury A. E., Sánchez M., Fukagawa N. K., Gleason R. E., Young V. R. 1994. Similar 24-h pattern and rate of carbon dioxide production, by indirect calorimetry vs. stable isotope dilution, in healthy adults under standardized metabolic conditions. J. Nutr. 124: 1615–1627. [DOI] [PubMed] [Google Scholar]
- 73.Annison G., Illman R. J., Topping D. L. 2003. Acetylated, propionylated or butyrylated starches raise large bowel short-chain fatty acids preferentially when fed to rats. J. Nutr. 133: 3523–3528. [DOI] [PubMed] [Google Scholar]
- 74.Jacobs L. R., Lupton J. R. 1986. Relationship between colonic luminal pH, cell proliferation, and colon carcinogenesis in 1,2-dimethylhydrazine treated rats fed high fiber diets. Cancer Res. 46: 1727–1734. [PubMed] [Google Scholar]
- 75.Ward F. W., Coates M. E. 1987. Gastrointestinal pH measurement in rats: influence of the microbial flora, diet and fasting. Lab. Anim. 21: 216–222. [DOI] [PubMed] [Google Scholar]
- 76.Campbell J. M., Fahey G. C., Wolf B. W. 1997. Selected indigestible oligosaccharides affect large bowel mass, cecal and fecal short-chain fatty acids, pH and microflora in rats. J. Nutr. 127: 130–136. [DOI] [PubMed] [Google Scholar]
- 77.Murase M., Kimura Y., Nagata Y. 1995. Determination of portal short-chain fatty acids in rats fed various dietary fibers by capillary gas chromatography. J. Chromatogr. B Biomed. Appl. 664: 415–420. [DOI] [PubMed] [Google Scholar]
- 78.Fushimi T., Suruga K., Oshima Y., Fukiharu M., Tsukamoto Y., Goda T. 2006. Dietary acetic acid reduces serum cholesterol and triacylglycerols in rats fed a cholesterol-rich diet. Br. J. Nutr. 95: 916–924. [DOI] [PubMed] [Google Scholar]
- 79.Demigné C., Morand C., Levrat M. A., Besson C., Moundras C., Rémésy C. 1995. Effect of propionate on fatty acid and cholesterol synthesis and on acetate metabolism in isolated rat hepatocytes. Br. J. Nutr. 74: 209–219. [DOI] [PubMed] [Google Scholar]
- 80.Todesco T., Rao A. V., Bosello O., Jenkins D. J. 1991. Propionate lowers blood glucose and alters lipid metabolism in healthy subjects. Am. J. Clin. Nutr. 54: 860–865. [DOI] [PubMed] [Google Scholar]
- 81.Stoddart L. A., Smith N. J., Milligan G. 2008. International Union of Pharmacology. LXXI. Free fatty acid receptors FFA1, -2, and -3: pharmacology and pathophysiological functions. Pharmacol. Rev. 60: 405–417. [DOI] [PubMed] [Google Scholar]
- 82.Ulven T. 2012. Short-chain free fatty acid receptors FFA2/GPR43 and FFA3/GPR41 as new potential therapeutic targets. Front. Endocrinol. (Lausanne). 3: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tazoe H., Otomo Y., Kaji I., Tanaka R., Karaki S. I., Kuwahara A. 2008. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J. Physiol. Pharmacol. 59: 251–262. [PubMed] [Google Scholar]
- 84.Sellin J. H. 1999. SCFAs: the enigma of weak electrolyte transport in the colon. News Physiol. Sci. 14: 58–64. [DOI] [PubMed] [Google Scholar]
- 85.Vidyasagar S., Barmeyer C., Geibel J., Binder H. J., Rajendran V. M. 2005. Role of short-chain fatty acids in colonic HCO(3) secretion. Am. J. Physiol. Gastrointest. Liver Physiol. 288: G1217–G1226. [DOI] [PubMed] [Google Scholar]
- 86.Mascolo N., Rajendran V. M., Binder H. J. 1991. Mechanism of short-chain fatty acid uptake by apical membrane vesicles of rat distal colon. Gastroenterology. 101: 331–338. [DOI] [PubMed] [Google Scholar]
- 87.Harig J. M., Ng E. K., Dudeja P. K., Brasitus T. A., Ramaswamy K. 1996. Transport of n-butyrate into human colonic luminal membrane vesicles. Am. J. Physiol. 271: G415–G422. [DOI] [PubMed] [Google Scholar]
- 88.Harig J. M., Soergel K. H., Barry J. A., Ramaswamy K. 1991. Transport of propionate by human ileal brush-border membrane vesicles. Am. J. Physiol. 260: G776–G782. [DOI] [PubMed] [Google Scholar]
- 89.Hadjiagapiou C., Schmidt L., Dudeja P. K., Layden T. J., Ramaswamy K. 2000. Mechanism(s) of butyrate transport in Caco-2 cells: role of monocarboxylate transporter 1. Am. J. Physiol. Gastrointest. Liver Physiol. 279: G775–G780. [DOI] [PubMed] [Google Scholar]
- 90.Teramae H., Yoshikawa T., Inoue R., Ushida K., Takebe K., Nio-Kobayashi J., Iwanaga T. 2010. The cellular expression of SMCT2 and its comparison with other transporters for monocarboxylates in the mouse digestive tract. Biomed. Res. 31: 239–249. [DOI] [PubMed] [Google Scholar]
- 91.Takebe K., Nio J., Morimatsu M., Karaki S., Kuwahara A., Kato I., Iwanaga T. 2005. Histochemical demonstration of a Na(+)-coupled transporter for short-chain fatty acids (slc5a8) in the intestine and kidney of the mouse. Biomed. Res. 26: 213–221. [DOI] [PubMed] [Google Scholar]
- 92.Gupta N., Martin P. M., Prasad P. D., Ganapathy V. 2006. SLC5A8 (SMCT1)-mediated transport of butyrate forms the basis for the tumor suppressive function of the transporter. Life Sci. 78: 2419–2425. [DOI] [PubMed] [Google Scholar]
- 93.Gonçalves P., Araújo J. R., Martel F. 2011. Characterization of butyrate uptake by nontransformed intestinal epithelial cell lines. J. Membr. Biol. 240: 35–46. [DOI] [PubMed] [Google Scholar]
- 94.Musch M. W., Bookstein C., Xie Y., Sellin J. H., Chang E. B. 2001. SCFA increase intestinal Na absorption by induction of NHE3 in rat colon and human intestinal C2/bbe cells. Am. J. Physiol. Gastrointest. Liver Physiol. 280: G687–G693. [DOI] [PubMed] [Google Scholar]
- 95.Tyagi S., Venugopalakrishnan J., Ramaswamy K., Dudeja P. K. 2002. Mechanism of n-butyrate uptake in the human proximal colonic basolateral membranes. Am. J. Physiol. Gastrointest. Liver Physiol. 282: G676–G682. [DOI] [PubMed] [Google Scholar]
- 96.Gill R. K., Saksena S., Alrefai W. A., Sarwar Z., Goldstein J. L., Carroll R. E., Ramaswamy K., Dudeja P. K. 2005. Expression and membrane localization of MCT isoforms along the length of the human intestine. Am. J. Physiol. Cell Physiol. 289: C846–C852. [DOI] [PubMed] [Google Scholar]
- 97.Halestrap A. P., Meredith D. 2004. The SLC16 gene family-from monocarboxylate transporters (MCTs) to aromatic amino acid transporters and beyond. Pflugers Arch. 447: 619–628. [DOI] [PubMed] [Google Scholar]
- 98.Islam R., Anzai N., Ahmed N., Ellapan B., Jin C. J., Srivastava S., Miura D., Fukutomi T., Kanai Y., Endou H. 2008. Mouse organic anion transporter 2 (mOat2) mediates the transport of short chain fatty acid propionate. J. Pharmacol. Sci. 106: 525–528. [DOI] [PubMed] [Google Scholar]
- 99.Shin H. J., Anzai N., Enomoto A., He X., Kim D. K., Endou H., Kanai Y. 2007. Novel liver-specific organic anion transporter OAT7 that operates the exchange of sulfate conjugates for short chain fatty acid butyrate. Hepatology. 45: 1046–1055. [DOI] [PubMed] [Google Scholar]
- 100.Roediger W. E. 1982. Utilization of nutrients by isolated epithelial cells of the rat colon. Gastroenterology. 83: 424–429. [PubMed] [Google Scholar]
- 101.Clausen M. R., Mortensen P. B. 1995. Kinetic studies on colonocyte metabolism of short chain fatty acids and glucose in ulcerative colitis. Gut. 37: 684–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jørgensen J. R., Clausen M. R., Mortensen P. B. 1997. Oxidation of short and medium chain C2-C8 fatty acids in Sprague-Dawley rat colonocytes. Gut. 40: 400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ballard F. J. 1972. Supply and utilization of acetate in mammals. Am. J. Clin. Nutr. 25: 773–779. [DOI] [PubMed] [Google Scholar]
- 104.Knowles S. E., Jarrett I. G., Filsell O. H., Ballard F. J. 1974. Production and utilization of acetate in mammals. Biochem. J. 142: 401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bloemen J. G., Venema K., van de Poll M. C., Olde Damink S. W., Buurman W. A., Dejong C. H. 2009. Short chain fatty acids exchange across the gut and liver in humans measured at surgery. Clin. Nutr. 28: 657–661. [DOI] [PubMed] [Google Scholar]
- 106.Wiltrout D. W., Satter L. D. 1972. Contribution of propionate to glucose synthesis in the lactating and nonlactating cow. J. Dairy Sci. 55: 307–317. [DOI] [PubMed] [Google Scholar]
- 107.Bloemen J. G., Olde Damink S. W. M., Venema K., Buurman W. A., Jalan R., Dejong C. H. C. 2010. Short chain fatty acids exchange: is the cirrhotic, dysfunctional liver still able to clear them? Clin. Nutr. 29: 365–369. [DOI] [PubMed] [Google Scholar]
- 108.Reilly K. J., Rombeau J. L. 1993. Metabolism and potential clinical applications of short-chain fatty acids. Clin. Nutr. 12 (Suppl. 1): S97–S105. [Google Scholar]
- 109.Brown A. J., Goldsworthy S. M., Barnes A. A., Eilert M. M., Tcheang L., Daniels D., Muir A. I., Wigglesworth M. J., Kinghorn I., Fraser N. J., et al. 2003. The orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J. Biol. Chem. 278: 11312–11319. [DOI] [PubMed] [Google Scholar]
- 110.Le Poul E., Loison C., Struyf S., Springael J. Y., Lannoy V., Decobecq M. E., Brezillon S., Dupriez V., Vassart G., Van Damme J., et al. 2003. Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J. Biol. Chem. 278: 25481–25489. [DOI] [PubMed] [Google Scholar]
- 111.Nilsson N. E., Kotarsky K., Owman C., Olde B. 2003. Identification of a free fatty acid receptor, FFA2R, expressed on leukocytes and activated by short-chain fatty acids. Biochem. Biophys. Res. Commun. 303: 1047–1052. [DOI] [PubMed] [Google Scholar]
- 112.Regard J. B., Sato I. T., Coughlin S. R. 2008. Anatomical profiling of G protein-coupled receptor expression. Cell. 135: 561–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hong Y. H., Nishimura Y., Hishikawa D., Tsuzuki H., Miyahara H., Gotoh C., Choi K. C., Feng D. D., Chen C., Lee H., et al. 2005. Acetate and propionate short chain fatty acids stimulate adipogenesis via GPCR43. Endocrinology. 146: 5092–5099. [DOI] [PubMed] [Google Scholar]
- 114.Ge H., Li X., Weiszmann J., Wang P., Baribault H., Chen J., Tian H., Li Y. 2008. Activation of G protein-coupled receptor 43 in adipocytes leads to inhibition of lipolysis and suppression of plasma free fatty acids. Endocrinology. 149: 4519–4526. [DOI] [PubMed] [Google Scholar]
- 115.Samuel B. S., Shaito A., Motoike T., Rey F. E., Backhed F., Manchester J. K., Hammer R. E., Williams S. C., Crowley J., Yanagisawa M., et al. 2008. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc. Natl. Acad. Sci. USA. 105: 16767–16772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sleeth M. L., Thompson E. L., Ford H. E., Zac-Varghese S. E. K., Frost G. 2010. Free fatty acid receptor 2 and nutrient sensing a proposed role for fibre, fermentable carbohydrates and short-chain fatty acids in appetite regulation. Nutr. Res. Rev. 23: 135–145. [DOI] [PubMed] [Google Scholar]
- 117.Bjursell M., Admyre T., Goransson M., Marley A. E., Smith D. M., Oscarsson J., Bohlooly-Y M. 2011. Improved glucose control and reduced body fat mass in free fatty acid receptor 2-deficient mice fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 300: E211–E220. [DOI] [PubMed] [Google Scholar]
- 118.Zaibi M. S., Stocker C. J., O'Dowd J., Davies A., Bellahcene M., Cawthorne M. A., Brown A. J. H., Smith D. M., Arch J. R. S. 2010. Roles of GPR41 and GPR43 in leptin secretory responses of murine adipocytes to short chain fatty acids. FEBS Lett. 584: 2381–2386. [DOI] [PubMed] [Google Scholar]
- 119.Xiong Y., Miyamoto N., Shibata K., Valasek M. A., Motoike T., Kedzierski R. M., Yanagisawa M. 2004. Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proc. Natl. Acad. Sci. USA. 101: 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Covington D. K., Briscoe C. A., Brown A. J., Jayawickreme C. K. 2006. The G-protein-coupled receptor 40 family (GPR40-GPR43) and its role in nutrient sensing. Biochem. Soc. Trans. 34: 770–773. [DOI] [PubMed] [Google Scholar]
- 121.Yamashita H., Fujisawa K., Ito E., Idei S., Kawaguchi N., Kimoto M., Hiemori M., Tsuji H. 2007. Improvement of obesity and glucose tolerance by acetate in type 2 diabetic Otsuka Long-Evans Tokushima fatty (OLETF) rats. Biosci. Biotechnol. Biochem. 71: 1236–1243. [DOI] [PubMed] [Google Scholar]
- 122.Lin H. V., Frassetto A., Kowalik E. J. J., Nawrocki A. R., Lu M. M., Kosinski J. R., Hubert J. A., Szeto D., Yao X., Forrest G., et al. 2012. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS ONE. 7: e35240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kondo T., Kishi M., Fushimi T., Kaga T. 2009. Acetic acid upregulates the expression of genes for fatty acid oxidation enzymes in liver to suppress body fat accumulation. J. Agric. Food Chem. 57: 5982–5986. [DOI] [PubMed] [Google Scholar]
- 124.Kondo T., Kishi M., Fushimi T., Ugajin S., Kaga T. 2009. Vinegar intake reduces body weight, body fat mass, and serum triglyceride levels in obese Japanese subjects. Biosci. Biotechnol. Biochem. 73: 1837–1843. [DOI] [PubMed] [Google Scholar]
- 125.Zydowo M. M., Smolen´ski R. T., Swierczyn´ski J. 1993. Acetate-induced changes of adenine nucleotide levels in rat liver. Metabolism. 42: 644–648. [DOI] [PubMed] [Google Scholar]
- 126.Lin J., Handschin C., Spiegelman B. M. 2005. Metabolic control through the PGC-1 family of transcription coactivators. Cell Metab. 1: 361–370. [DOI] [PubMed] [Google Scholar]
- 127.Jäger S., Handschin C., St.-Pierre J., Spiegelman B. M. 2007. AMP-activated protein kinase (AMPK) action in skeletal muscle via direct phosphorylation of PGC-1α. Proc. Natl. Acad. Sci. USA. 104: 12017–12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Minokoshi Y., Kim Y. B., Peroni O. D., Fryer L. G., Müller C., Carling D., Kahn B. B. 2002. Leptin stimulates fatty-acid oxidation by activating AMP-activated protein kinase. Nature. 415: 339–343. [DOI] [PubMed] [Google Scholar]
- 129.Yu X., McCorkle S., Wang M., Lee Y., Li J., Saha A. K., Unger R. H., Ruderman N. B. 2004. Leptinomimetic effects of the AMP kinase activator AICAR in leptin-resistant rats: prevention of diabetes and ectopic lipid deposition. Diabetologia. 47: 2012–2021. [DOI] [PubMed] [Google Scholar]
- 130.Robertson M. D., Bickerton A. S., Dennis A. L., Vidal H., Frayn K. N. 2005. Insulin-sensitizing effects of dietary resistant starch and effects on skeletal muscle and adipose tissue metabolism. Am. J. Clin. Nutr. 82: 559–567. [DOI] [PubMed] [Google Scholar]
- 131.Suokas A., Kupari M., Heikkilä J., Lindros K., Ylikahri R. 1988. Acute cardiovascular and metabolic effects of acetate in men. Alcohol. Clin. Exp. Res. 12: 52–58. [DOI] [PubMed] [Google Scholar]
- 132.Al-Lahham S. H., Peppelenbosch M. P., Roelofsen H., Vonk R. J., Venema K. 2010. Biological effects of propionic acid in humans; metabolism, potential applications and underlying mechanisms. Biochim. Biophys. Acta. 1801: 1175–1183. [DOI] [PubMed] [Google Scholar]
- 133.Carmen G. Y., Víctor S. M. 2006. Signalling mechanisms regulating lipolysis. Cell. Signal. 18: 401–408. [DOI] [PubMed] [Google Scholar]
- 134.Houslay M. D., Milligan G. 1997. Tailoring cAMP-signalling responses through isoform multiplicity. Trends Biochem. Sci. 22: 217–224. [DOI] [PubMed] [Google Scholar]
- 135.Kimura I., Ozawa K., Inoue D., Imamura T., Kimura K., Maeda T., Terasawa K., Kashihara D., Hirano K., Tani T., et al. 2013. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43. Nat. Commun. 4: 1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Friedman J. M., Halaas J. L. 1998. Leptin and the regulation of body weight in mammals. Nature. 395: 763–770. [DOI] [PubMed] [Google Scholar]
- 137.Sakakibara S., Yamauchi T., Oshima Y., Tsukamoto Y., Kadowaki T. 2006. Acetic acid activates hepatic AMPK and reduces hyperglycemia in diabetic KK-A(y) mice. Biochem. Biophys. Res. Commun. 344: 597–604. [DOI] [PubMed] [Google Scholar]
- 138.Boillot J., Alamowitch C., Berger A. M., Luo J., Bruzzo F., Bornet F. R., Slama G. 1995. Effects of dietary propionate on hepatic glucose production, whole-body glucose utilization, carbohydrate and lipid metabolism in normal rats. Br. J. Nutr. 73: 241–251. [DOI] [PubMed] [Google Scholar]
- 139.Batterham R. L., Cowley M. A., Small C. J., Herzog H., Cohen M. A., Dakin C. L., Wren A. M., Brynes A. E., Low M. J., Ghatei M. A., et al. 2002. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 418: 650–654. [DOI] [PubMed] [Google Scholar]
- 140.van den Hoek A. M., Heijboer A. C., Corssmit E. P. M., Voshol P. J., Romijn J. A., Havekes L. M., Pijl H. 2004. PYY3-36 reinforces insulin action on glucose disposal in mice fed a high-fat diet. Diabetes. 53: 1949–1952. [DOI] [PubMed] [Google Scholar]
- 141.Boey D., Lin S., Karl T., Baldock P., Lee N., Enriquez R., Couzens M., Slack K., Dallmann R., Sainsbury A., et al. 2006. Peptide YY ablation in mice leads to the development of hyperinsulinaemia and obesity. Diabetologia. 49: 1360–1370. [DOI] [PubMed] [Google Scholar]
- 142.Karaki S., Tazoe H., Hayashi H., Kashiwabara H., Tooyama K., Suzuki Y., Kuwahara A. 2008. Expression of the short-chain fatty acid receptor, GPR43, in the human colon. J. Mol. Histol. 39: 135–142. [DOI] [PubMed] [Google Scholar]
- 143.Karaki S., Mitsui R., Hayashi H., Kato I., Sugiya H., Iwanaga T., Furness J. B., Kuwahara A. 2006. Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res. 324: 353–360. [DOI] [PubMed] [Google Scholar]
- 144.Tazoe H., Otomo Y., Karaki S., Kato I., Fukami Y., Terasaki M., Kuwahara A. 2009. Expression of short-chain fatty acid receptor in the human colon. Biomed Res. 30: 149–156. [DOI] [PubMed] [Google Scholar]
- 145.Tolhurst G., Heffron H., Lam Y. S., Parker H. E., Habib A. M., Diakogiannaki E., Cameron J., Grosse J., Reimann F., Gribble F. M. 2012. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein–coupled receptor FFAR2. Diabetes. 61: 364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cherbut C., Ferrier L., Rozé C., Anini Y., Blottière H., Lecannu G., Galmiche J. 1998. Short-chain fatty acids modify colonic motility through nerves and polypeptide YY release in the rat. Am. J. Physiol. 275: G1415–G1422. [DOI] [PubMed] [Google Scholar]
- 147.Cuche G., Cuber J. C., Malbert C. H. 2000. Ileal short-chain fatty acids inhibit gastric motility by a humoral pathway. Am. J. Physiol. Gastrointest. Liver Physiol. 279: G925–G930. [DOI] [PubMed] [Google Scholar]
- 148.Barrera J. G., Sandoval D. A., D'Alessio D. A., Seele R. J. 2011. GLP-1 and energy balance: an integrated model of short-term and long-term control. Nat. Rev. Endocrinol. 7: 507–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhou J., Martin R. J., Tulley R. T., Raggio A. M., McCutcheon K. L., Shen L., Danna S. C., Tripathy S., Hegsted M., Keenan M. J. 2008. Dietary resistant starch upregulates total GLP-1 and PYY in a sustained day-long manner through fermentation in rodents. Am. J. Physiol. Endocrinol. Metab. 295: E1160–E1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hooda S., Matte J. J., Vasanthan T., Zijlstra R. T. 2010. Dietary oat beta-glucan reduces peak net glucose flux and insulin production and modulates plasma incretin in portal-vein catheterized grower pigs. J. Nutr. 140: 1564–1569. [DOI] [PubMed] [Google Scholar]
- 151.Freeland K. R., Wolever T. M. 2010. Acute effects of intravenous and rectal acetate on glucagon-like peptide-1, peptide YY, ghrelin, adiponectin and tumour necrosis factor-alpha. Br. J. Nutr. 103: 460–466. [DOI] [PubMed] [Google Scholar]
- 152.Rodwell V. W., Nordstrom J. L., Mitschelen J. J. 1976. Regulation of HMG-CoA reductase. Adv. Lipid Res. 14: 1–74. [DOI] [PubMed] [Google Scholar]
- 153.Bush R. S., Milligan L. P. 1971. Study of the mechanism of inhibition of ketogenesis by propionate in bovine liver. Can. J. Anim. Sci. 51: 121–127. [Google Scholar]
- 154.Wright R. S., Anderson J. W., Bridges S. R. 1990. Propionate inhibits hepatocyte lipid synthesis. Proc. Soc. Exp. Biol. Med. 195: 26–29. [DOI] [PubMed] [Google Scholar]
- 155.Hara H., Haga S., Aoyama Y., Kiriyama S. 1999. Short-chain fatty acids suppress cholesterol synthesis in rat liver and intestine. J. Nutr. 129: 942–948. [DOI] [PubMed] [Google Scholar]
- 156.Carling D., Clarke P. R., Zammit V. A., Hardie D. G. 1989. Purification and characterization of the AMP-activated protein kinase. Eur. J. Biochem. 186: 129–136. [DOI] [PubMed] [Google Scholar]
- 157.Corton J. M., Gillespie J. G., Hardie D. G. 1994. Role of the AMP-activated protein kinase in the cellular stress response. Curr. Biol. 4: 315–324. [DOI] [PubMed] [Google Scholar]
- 158.Henin N., Vincent M. F., Gruber H. E., Van den Berghe G. 1995. Inhibition of fatty acid and cholesterol synthesis by stimulation of AMP-activated protein kinase. FASEB J. 9: 541–546. [DOI] [PubMed] [Google Scholar]
- 159.Turnbaugh P. J., Ley R. E., Mahowald M. A., Magrini V., Mardis E. R., Gordon J. I. 2006. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 444: 1027–1031. [DOI] [PubMed] [Google Scholar]
- 160.Murphy E. F., Cotter P. D., Healy S., Marques T. M., O'Sullivan O., Fouhy F., Clarke S. F., O'Toole P. W., Quigley E. M., Stanton C., et al. 2010. Composition and energy harvesting capacity of the gut microbiota: relationship to diet, obesity and time in mouse models. Gut. 59: 1635–1642. [DOI] [PubMed] [Google Scholar]
- 161.Schwiertz A., Taras D., Schäfer K., Beijer S., Bos N. A., Donus C., Hardt P. D. 2010. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring). 18: 190–195. [DOI] [PubMed] [Google Scholar]
- 162.Bäckhed F., Manchester J. K., Semenkovich C. F., Gordon J. I. 2007. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc. Natl. Acad. Sci. USA. 104: 979–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Høverstad T., Midtvedt T. 1986. Short-chain fatty acids in germfree mice and rats. J. Nutr. 116: 1772–1776. [DOI] [PubMed] [Google Scholar]
- 164.Ley R. E., Ãckhed F. B., Turnbaugh P., Lozupone C. A., Knight R. D., Gordon J. I. 2005. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 102: 11070–11075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ley R. E., Turnbaugh P. J., Klein S., Gordon J. I. 2006. Microbial ecology: human gut microbes associated with obesity. Nature. 444: 1022–1023. [DOI] [PubMed] [Google Scholar]
- 166.Khan K. M., Edwards C. A. 2002. Effect of substrate concentration on short chain fatty acid production in in vitro cultures of human faeces. Microb Ecol Health Dis. 14: 160–164. [Google Scholar]