Abstract
Outcomes research, which investigates the outcomes of health care practices, is intended to provide scientific evidence for clinical decision making and health care. This paper elucidates the goal and domains of outcomes research. Also it shows the potential and promise of outcomes research to provide a methodology to uncover what to do and how to do it, and enable the health care profession to achieve the right care, for the right patient, at the right time, the first time, every time, nothing more, and nothing less.
1. Clinical case
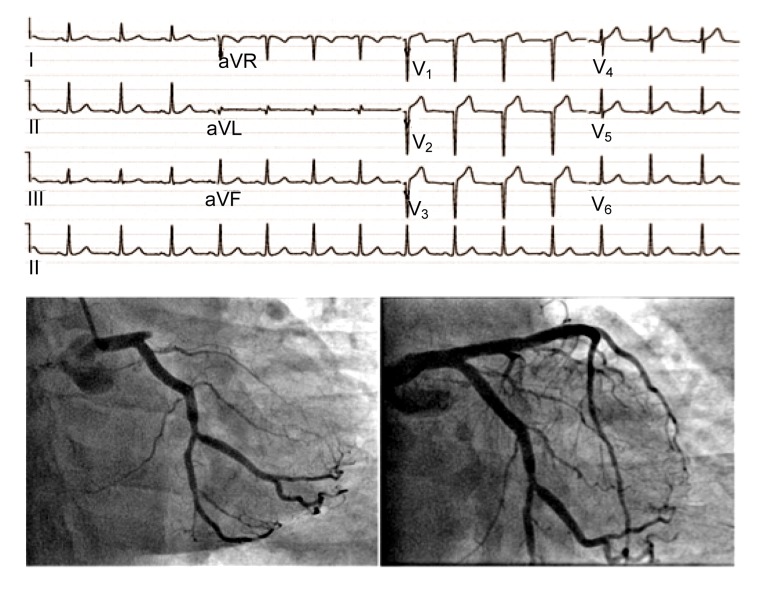
A 56 year-old male smoker presented to a hospital emergency department, having suffered 3 h of severe chest pain. Physical exam showed a heart rate of 90 beats/min, blood pressure of 90/60 mmHg, and bibasilar rales. An electrocardiogram performed within 10 min of arrival demonstrated a 2-mm ST-elevation in leads V1–V4 (Fig. 1). The patient was treated with 325 mg of aspirin, 600 mg of clopidogrel, and 4 000 U of heparin, and underwent primary percutaneous coronary intervention using right radial artery access. Following aspiration thrombectomy, a drug-eluting stent was placed in the left anterior descending artery, restoring normal blood flow. The door-to-balloon time was 70 min. Echocardiography showed a preserved left ventricular ejection fraction of 60% with only mild anterior-apical hypokinesis. He was started on 50 mg of metoprolol twice daily, 40 mg of atorvastatin daily, 81 mg of aspirin daily, and 75 mg of clopidogrel daily, and discharged from hospital on Day 3. Was this high-quality patient care?
Fig. 1.
Clinical case of electrocardiogram and angiogram
The care provided in the emergency department, cardiac catheterization lab, and coronary care unit was appropriate and excellent. However, despite rapid diagnosis and treatment for this patient with ST-elevation myocardial infarction, what were the long-term patient outcomes at 30 d, 6 months, and 1 year? While long-term survival free from recurrent major adverse cardiovascular events depends on the door-to-balloon time and type of drug-eluting stent, it also depends on the patient’s ability to adhere to medication schedules, to follow up with his or her physician, to change his lifestyle, including smoking cessation, diet, and exercise, and to access and pay for health care services and secondary prevention.
2. Opportunity to improve health care
The United States health care system’s costs are the highest in the world, but quality and patient outcomes lag behind those of other countries. Furthermore, the United States health care is characterized by striking gaps (McGlynn et al., 2003; Pham et al., 2007) including: (1) variation in care across health care systems and among clinicians, (2) fragmentation of care, (3) disparities in access and patient outcomes, (4) marginal safety, and (5) unsustainable rises in costs. These forces contribute to observed adverse outcomes such as preventable deaths, re-admissions, and hospital acquired infections. Some experts contend that the United States health care system faces a hard choice—either to cut costs or to sacrifice quality. This is a false choice and there is a third option—to design, implement, and evaluate systems of care that simultaneously improve outcomes and reduce costs.
In the 20th century, clinicians saved lives by inventing new and more effective medications, performing open heart surgery, and treating heart attack patients with stents. In the 21st century, clinicians will save lives by improving coordination of care, enhancing communication and teamwork, engaging patients and families in shared decision making, and embracing a culture of change and continuous improvement. Fatalism is leaving health care as events which once appeared beyond our control, like medication errors and patient falls, are coming within our influence—but only if we act together as an interprofessional team.
Health care organizations across the world are rapidly transforming to achieve the triple aims of better patient care and health care experience, better population health, and more affordable care. Stakeholders in health care, including patients, payers, and policymakers, expect clinicians and organizations to achieve all three aims simultaneously, and not only one or two of them. Recently, 11 chief executive officers of leading United States health care systems proposed a “Checklist for High Value Health Care” consisting of 10 key strategies to improve outcomes and reduce costs simultaneously (Cosgrove et al., 2013): (1) leadership with visible priorities; (2) culture of continuous improvement and learning; (3) information technology best practices at point of care; (4) use of evidence-based protocols; (5) optimized use of resources (personnel, space, and equipment); (6) integrated care; (7) shared decision making; (8) targeted service lines for resource intensive patients; (9) embedded safeguards to prevent injury and harm; (10) internal transparency of performance, outcomes, and costs.
How will clinicians and health care organizations achieve these goals in a manner harmonized with the Institute of Medicine’s domains of quality (Ferguson, 2012)—care that is safe, timely, effective, efficient, equitable, and patient-centered? How will clinical research inform clinicians and health care organizations about what to do and how to do it?
3. Goals of outcomes research
Outcomes research holds the potential and promise to help transform health care delivery and patient outcomes by focusing on the “end results or outcomes” of health care. Health care can be characterized and measured by attributes including structure, processes, and outcomes. Structural attributes are features of health care organizations or clinicians, related to their capacity to provide high quality care, such as electronic medical records, computerized physician order entry, or nurse-to-patient staffing ratios. Process measures are health care related activities performed for, on behalf of, or by a patient, such as prescribing statins at discharge for patients with acute myocardial infarction or door-to-balloon time for patients with ST-elevation myocardial infarction. Intermediate clinical outcome measures are changes in physiologic state that lead to a long-term health outcome, such as low-density lipoprotein levels or adherence to prescribed medications. Health outcome measures represent the health status of a patient resulting from care (including either desirable or adverse outcomes), such as 30-d mortality rates and 30-d hospital re-admission rates.
Outcomes research focuses on understanding and improving intermediate clinical outcomes and health outcomes through better information, better clinical decision making, and better health care delivery. It is a new scientific field developed in the last decade and draws from clinical medicine, statistics, informatics, epidemiology, social sciences, real-world practice, improvement science, implementation science, and policy (Krumholz, 2011). Outcomes research, positioned at the interface of these disciplines, is an inherently practical form of clinical research that not only describes gaps in health care outcomes but also strives to find solutions to resolve those gaps (Ting et al., 2009).
4. Domains of outcomes research
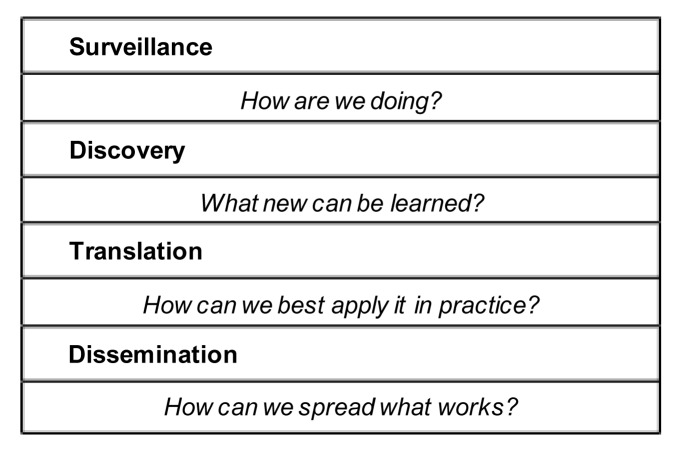
Outcomes research consists of four domains of activities: surveillance, discovery, translation, and dissemination (Fig. 2). Surveillance research addresses the question: How are we doing? Surveillance is a necessary and critical first step to understand what gaps exist in our current health care delivery system, either at the local, regional, national, or international level. Surveillance starts with an environmental scan of what care is actually delivered, rather than what care should be delivered according to clinical practice guidelines. For example, in a study of 12 cities in the United States, McGlynn et al. (2003) showed that on average only 55% of patients received treatments recommended by clinical practice guidelines, ranging from 68% of patients with coronary artery disease to 25% of patients with atrial fibrillation who received ideal, recommended care. Clinical databases and registries, payer claims and financial databases, and survey studies are alternative approaches to collect and analyze data to understand better the gap between usual, routine clinical care and ideal, recommended clinical care.
Fig. 2.
Outcomes research—types of activities
Discovery research addresses the questions: What new approaches can be learned and what works, for whom, and in what context? After illuminating the gaps in clinical care and patient outcomes, discovery research endeavors to find new ways to organize and deliver care that can resolve those gaps. There are three general approaches for discovery research, including multivariable statistical modeling, action-oriented quality improvement, and mixed-methodology positive deviance. Multivariable statistical modeling research determines which characteristics of hospitals or patients are associated with patient outcomes. One example is the development and validation of risk prediction scores to identify which patients, after percutaneous coronary intervention, are at low (<1%), intermediate (1%–3%), and high (>3%) risk for major bleeding events (Mehta et al., 2009). Action-oriented quality improvement research represents a single organization or work unit internally developing, implementing, and testing interventions to improve patient outcomes. These interventions and best practices are typically informed by a small sample of experts and often may not be applicable to other contexts. For example, a quality improvement team strived to reduce hospital acquired infections by trying interventions such as hand hygiene and disinfection of surfaces with bleach (Orenstein et al., 2011). Mixed-methodology positive deviance research aims to identify existing top performing organizations and to understand how they are delivering care. This approach requires the following: performance measures that are valid, widely accepted, available, and accessible; a range and distribution in performance where top performers can be reliably identified; top performers that are willing to share best practices and a learning network that can be developed; and qualitative and quantitative methods that can be reliably used (Bradley et al., 2009). For example, novel interventions to improve door-to-balloon time for patients with ST-elevation myocardial infarction in the United States were developed using positive deviance research. These interventions included enabling the emergency department physician to activate the cardiac catheterization lab team and providing real-time feedback of performance to emergency department cardiac catheterization lab staff (Bradley et al., 2006).
Translation research addresses the question: How can we best apply proven interventions to clinical practice? Translation focuses on the practical issues of what are the facilitators and barriers for hospitals and clinicians to adopt novel interventions and methods to provide care. For example, in the United States, it took 25 years and 6 weeks from the discovery that β-blockers improve survival after myocardial infarction in the β-Blocker Heart Attack Trial (BHAT) to achieve the performance standard that 90% of patients after acute myocardial infarction are discharged from the hospital on a β-blocker (Lee, 2007). This lag in translation is not related to unintelligent or forgetful clinicians. Rather, it relates to systems and processes of care to ensure that the best care is provided to every patient, every day. Further, decades of research have shown that in the current era, translation typically occurs passively, much like diffusion; if the goal was to accelerate the speed of translation, then it must be actively managed. Recently, federal funding agencies in the United States have begun to prioritize grants for translational research (Westfall et al., 2007).
Dissemination addresses the question: How to spread what works for one hospital or practice context to other hospitals. Dissemination research utilizes the REAIM (reach, effectiveness, adoption, implementation, maintenance) framework of reach, effectiveness, adoption, implementation, and maintenance. Reach measures how broadly the intervention is used by participants. Effectiveness refers to the impact of the intervention on patient outcomes. Adoption assesses how easy it is for participants to understand and implement the intervention within their practice context and clinical workflow. Implementation evaluates the facilitators and barriers to implement the intervention, and the correspondence between what was planned and what was achieved. Maintenance measures whether the intervention has become a usual, routine activity, and whether continuous monitoring of outcomes exists. Dissemination research requires developing learning networks to engage stakeholders and beneficiaries broadly. For example, the Door-to-Balloon Alliance for Quality spread interventions to improve door-to-balloon time to over 1 200 hospitals in the United States through a learning network (Krumholz et al., 2008).
5. Conclusions
Health care is on the cusp of extraordinary changes to achieve the triple aims of better patient care and health care experience, better population health, and more affordable care. To realize the societal expectation for high value health care, outcomes research represents a scientific field of study to illuminate the gaps in care, discover interventions that can close those gaps, translate proven interventions to specific clinical teams and practice contexts, and spread what works across a region or nation. Outcomes research has the potential and promise to provide a methodology to uncover what to do and how to do it, and enable the health care profession to achieve the right care, for the right patient, at the right time, the first time, every time, nothing more, and nothing less.
Footnotes
Compliance with ethics guidelines: Henry H. TING, Mei-xiang XIANG, and Jian-an WANG declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355(22):2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 2.Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci. 2009;4(1):25. doi: 10.1186/1748-5908-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cosgrove DM, Fisher M, Gabow P, Gottlieb G, Halvorson GC, James BC, Kaplan GS, Perlin JB, Petzel R, Steele GD, et al. Ten strategies to lower costs, improve quality, and engage patients: the view from leading health system CEOs. Health Aff (Millwood) 2013;32(2):321–327. doi: 10.1377/hlthaff.2012.1074. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson TJ. The Institute of Medicine Committee report “best care at lower cost: the path to continuously learning health care”. Circ Cardiovasc Qual Outcomes. 2012;5(6):e93–e94. doi: 10.1161/CIRCOUTCOMES.112.968768. [DOI] [PubMed] [Google Scholar]
- 5.Krumholz HM. Real-world imperative of outcomes research. JAMA. 2011;306(7):754–755. doi: 10.1001/jama.2011.1170. [DOI] [PubMed] [Google Scholar]
- 6.Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, Stern AF, Byrd JR, Brush JJ. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1(1):97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Lee TH. Eulogy for a quality measure. N Engl J Med. 2007;357(12):1175–1177. doi: 10.1056/NEJMp078102. [DOI] [PubMed] [Google Scholar]
- 8.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 9.Mehta SK, Frutkin AD, Lindsey JB, House JA, Spertus JA, Rao SV, Ou FS, Roe MT, Peterson ED, Marso SP. Bleeding in patients undergoing percutaneous coronary intervention: the development of a clinical risk algorithm from the National Cardiovascular Data Registry. Circ Cardiovasc Interv. 2009;2(3):222–229. doi: 10.1161/CIRCINTERVENTIONS.108.846741. [DOI] [PubMed] [Google Scholar]
- 10.Orenstein R, Aronhalt KC, McManus JJ, Fedraw LA. A targeted strategy to wipe out Clostridium difficile . Infect Control Hosp Epidemiol. 2011;32(11):1137–1139. doi: 10.1086/662586. [DOI] [PubMed] [Google Scholar]
- 11.Pham HH, Schrag D, O′Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for performance. N Engl J Med. 2007;356(11):1130–1139. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- 12.Ting HH, Shojania KG, Montori VM, Bradley EH. Quality improvement: science and action. Circulation. 2009;119(14):1962–1974. doi: 10.1161/CIRCULATIONAHA.108.768895. [DOI] [PubMed] [Google Scholar]
- 13.Westfall JM, Mold J, Fagnan L. Practice-based research—“Blue Highways” on the NIH roadmap. JAMA. 2007;297(4):403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]