Abstract
Physicians play an important role in CR referral and enrollment. Despite established benefits and recommendations, cardiac rehabilitation (CR) enrollment rates are pervasively low. The reasons cardiac patients are missing from CR programs are multifactorial and include provider factors. A number of studies have now investigated physician factors associated with referral to CR programs and patient enrollment. The objective of this study was to qualitatively and systematically review this literature. A literature search of MEDLINE, PsycINFO, CINAHL, Embase, and EBM was conducted for published articles from database inception to October 2011. Overall, 17 articles were included following a process of independent review of each article by 2 authors. Seven (41.2%) were graded as good quality according to Downs and Black criteria. There were no randomized controlled trials. Results showed that medical specialty (ie, cardiac specialists more likely to refer; n = 8 studies) and other physician‐reported reasons (eg, physician report of their reasons for CR referral and physician sex) were related to referral. Physician factors related to patient enrollment in CR were physician endorsement, medical specialty, being referred, and physician attitudes toward CR. Physician factors are consistently related to CR referral and enrollment. The role of physician endorsements in promoting patient enrollment should be optimized and exploited.
Introduction
Cardiovascular diseases are among the leading cause of morbidity and mortality worldwide.1 Burden is projected to rise globally to 83 million cases in 2020.1 Cardiac rehabilitation (CR) is an outpatient secondary prevention program comprised of structured exercise training and comprehensive education and counseling to promote optimal functioning for patients.2 Participation in CR has been shown to improve health behavior, improve exercise capacity, promote psychological wellbeing, reduce rehospitalization, and reduce mortality by 25%, all in a cost‐effective manner.3, 4 Accordingly, CR is recognized in clinical practice guidelines as a standard element of the continuum of cardiac care,2, 5, 6 and a recent American Heart Association Presidential Advisory and Science Advisory promote the importance of CR referral by physicians.7, 8
Despite these established benefits and recommendations, CR enrollment rates are pervasively low. In the United States, participation rates range from 14% to 55% after myocardial infarction.9 In the United Kingdom, 28.6% of eligible patients were enrolled in CR in 2004, despite a national target of 85%.10 In Canada, approximately 30% of eligible cardiac inpatients enroll in CR.11 The reasons cardiac patients are missing from CR programs are multifactorial and include health system‐, provider‐, and patient‐related factors.12 The preponderance of literature in this area has focused on patient‐related correlates of CR use. However, arguably 1 of the chief explanatory factors is failure of physicians to refer.13 Physician recommendations to attend has long been known as a key factor affecting patient participation in CR.14 A number of studies have since investigated physician factors associated with referral to CR programs and patient enrollment. This literature has not yet been reviewed and synthesized to our knowledge. The objective of this study was to qualitatively and systematically review the literature investigating physician factors related to CR referral and enrollment.
Methods
The criteria for considering studies for this review included types of studies, types of participants, and types of outcome measures. For the types of studies, peer‐reviewed studies in print or published ahead of print were considered for inclusion. Primary or secondary studies were included whether they were observational or interventional in design. Qualitative studies were not included, but served to inform interpretation of quantitative findings. Reviews were identified as a source of additional primary studies. For the types of participants, healthcare providers with a scope of practice to sign off on CR referral (cardiologists, cardiovascular surgeons, family doctors, internists, or nurse practitioners) were considered and alternatively inpatients or outpatients who were eligible for CR reporting on perceived recommendation by the healthcare provider with the scope to refer. Referral and/or enrollment in CR were used as the types of outcome measures.
Search Methods for Identification of Studies
Literature published between 1946 and October 2011 was searched using the MEDLINE, PsycINFO, CINAHL, Embase, and EBM electronic databases. The search strategy was composed of 3 concepts: (1) cardiac conditions (eg, myocardial infarction), (2) practitioners focus (eg, physician practice patterns); and (3) the outcome of interest (eg, referral). The terms were adjusted to each database so that studies were not missed by the search strategy. A snowball hand search was undertaken after the first selection of articles. Search strategy is depicted in Table 1.
Table 1.
Search Strategy
| Concept | Search Terms–MEDLINE | Search Terms–Embase |
|---|---|---|
| Cardiac conditions | Coronary disease | Coronary artery disease |
| Heart disease | Heart disease | |
| Cardiovascular disease | Cardiovascular disease | |
| Coronary artery disease | Heart infarction | |
| Myocardial infarction | Myocardial infarction | |
| Cardiac rehabilitation | ||
| Practitioner focus | Attitudes to health personnel | Doctor patient relation |
| Physician's practice patterns | Medical specialist | |
| Physician–patient relations | Physician | |
| Professional competence | Cardiovascular surgeon | |
| Physician | Cardiologist | |
| Physician's role | Advanced practice nurse | |
| Cardiovascular surgeon | ||
| Cardiologist | ||
| Nurse practitioners | ||
| Rehabilitation /referral | Referral and consultation | Physician attitude |
| Access/adherence /enrollment | Prejudice | Clinical practice |
| Patient acceptance of healthcare | Health personnel attitude | |
| Patient compliance | Patient referral | |
| Ambulatory care | Patient attitude | |
| Attitude to health | Patient selection | |
| Health services accessibility | Ambulatory care | |
| Healthcare disparities | Attitude to health | |
| Outpatients | Healthcare disparity | |
| Inpatients | Outpatient | |
| Patient dropouts | Outpatient department | |
| Treatment refusal | Cardiac patient | |
| Patient participation | Rehabilitation patient | |
| Refusal to participate | Heart rehabilitation | |
| Patient selection | Patient dropout | |
| Physician or provider perception | Cardiac rehabilitation | |
| Patient care management | Physician or provider perception | |
| Health behavior | Health behavior | |
| Cardiac inpatient or outpatient | Cardiac inpatient or outpatient | |
| Gatekeeping | Cardiac referral or access or enrollment | |
| Eligibility determinants | Cardiac rehabilitation patient | |
| Cardiac referral or access or enrollment | Rehabilitation center | |
| Rehabilitation | Rehabilitation center | |
| Cardiac rehabilitation patient | Cardiac rehabilitation program | |
| Rehabilitation centers | Cardiology clinic | |
| Rehabilitation center | Coronary care unit | |
| Cardiac rehabilitation program | Cardiac care | |
| Cardiology clinic | Patient compliance | |
| Cardiac care facilities | Program access | |
| Cardiac care | Program adherence | |
| Patient compliance | Program utilization | |
| Program access | Program enrollment | |
| Program adherence | Patient attendance | |
| Program utilization | Health behavior | |
| Program enrollment | ||
| Patient attendance | ||
| Health behavior |
Data Collection and Analysis
Two reviewers (G.M.G. and P.P.) independently screened the references identified by the search strategy by title and abstract. To be selected, abstracts had to meet the eligibility criteria of this study. The full‐text reports of all selected citations were obtained and assessed independently for eligibility by these 2 reviewer, based on the defined inclusion criteria. Any disagreements were resolved by consultation with a third author (S.G.).
Data extraction was undertaken by a single reviewer (G.M.G.) and checked by a second reviewer (P.P.). The Downs and Black scale15 was selected to assess the quality of the studies as it is appropriate to evaluate nonrandomized investigations, and it contained the highest number of relevant items for the needs of this review. However, as not all items were relevant to the various study types included in this review, a modified version of the checklist was employed for each of the study types, excluding questions related to randomized controlled trials (Table 2). Therefore, a modified version of the Downs and Black checklist was used with the final checklist consisting of 18 items. The tool was used to describe points in 4 areas: reporting, external validity, internal validity (bias), and internal validity (confounding). Each study was scored for the presence of 1 or more items in each domain, with overall judgment of potential for bias based on a total score of 0 to 18, with a higher score indicating higher methodological quality. The classification of each study as good, fair, or poor was based on cut points according to the US Preventive Services Task Force approach.16
Table 2.
Modified Version of the Downs and Black Checklist
| No. | Question | Yes | No | Unclear |
|---|---|---|---|---|
| Reporting (7) | ||||
| 1 | Is the hypothesis/aim/objective of the study clearly described? | □ | □ | □ |
| 2 | Are the main outcomes to be measured clearly described in the Introduction or Methods section? | □ | □ | □ |
| If the main outcomes are first mentioned in the Results section, the question should be answered no. | ||||
| 3 | Are the characteristics of the patients included in the study clearly described? | □ | □ | □ |
| In cohort studies and trials, inclusion and/or exclusion criteria should be given. In case–control studies, a case definition and the source for controls should be given. | ||||
| 4 | Are the interventions of interest clearly described? | □ | □ | □ |
| Treatments and placebo (where relevant) that are to be compared should be clearly described. | ||||
| 6 | Are the main findings of the study clearly described? | □ | □ | □ |
| Simple outcome data (including denominators and numerators) should be reported for all major findings so that the reader can check the major analyses and conclusions. (This question does not cover statistical tests that are considered below.) | ||||
| 9 | Have the characteristics of patients lost on follow‐up been described? | □ | □ | □ |
| This should be answered yes where there were no losses to follow‐up or where losses to follow‐up were so small that findings would be unaffected by their inclusion. This should be answered no where a study does not report the number of patients lost to follow‐up. | ||||
| 10 | Have actual probability values been reported (eg, for the main outcomes except where the probability value is less than 0.001? | □ | □ | □ |
| For example, 0.035 rather than <0.05) | ||||
| External validity (3) | ||||
| 11 | Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | □ | □ | □ |
| The study must identify the source population for patients and describe how the patients were selected. Patients would be representative if they comprised the entire source population, an unselected sample of consecutive patients, or a random sample. Random sampling is only feasible where a list of all members of the relevant population exists. Where a study does not report the proportion of the source population from which the patients are derived, the question should be answered as unable to determine. | ||||
| 12 | Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | □ | □ | □ |
| The proportion of those asked who agreed should be stated. Validation that the sample was representative would include demonstrating that the distribution of the main confounding factors was the same in the study sample and the source population. | ||||
| 13 | Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? | □ | □ | □ |
| For the question to be answered yes, the study should demonstrate that the intervention was representative of that in use in the source population. The question should be answered no if, for example, the intervention was undertaken in a specialist center unrepresentative of the hospitals most of the source population would attend. | ||||
| Internal validity–bias (4) | ||||
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow‐up of patients, or in case–control studies, is the time period between the intervention and outcome the same for cases and controls? | □ | □ | □ |
| Where follow‐up was the same for all study patients the answer should be yes. If different lengths of follow‐up were adjusted for by, for example, survival analysis, the answer should be yes. Studies where differences in follow‐up are ignored should be answered no. | ||||
| 18 | Were the statistical tests used to assess the main outcomes appropriate? | □ | □ | □ |
| The statistical techniques used must be appropriate to the data. For example, nonparametric methods should be used for small sample sizes. Where little statistical analysis has been undertaken but where there is no evidence of bias, the question should be answered yes. If the distribution of the data (normal or not) is not described, it must be assumed that the estimates used were appropriate and the question should be answered yes. | ||||
| 19 | Was compliance with the intervention/s reliable? | □ | □ | □ |
| Where there was noncompliance with the allocated treatment or where there was contamination of 1 group, the question should be answered no. For studies where the effect of any misclassification was likely to bias any association to the null, the question should be answered yes. | ||||
| 20 | Were the main outcome measures used accurate (valid and reliable)? | □ | □ | □ |
| For studies where the outcome measures are clearly described, the question should be answered yes. For studies that refer to other work or that demonstrates the outcome measures are accurate, the question should be answered as yes. | ||||
| Internal validity–confounding (selection bias) (4) | ||||
| 21 | Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited from the same population? | □ | □ | □ |
| For example, patients for all comparison groups should be selected from the same hospital. The question should be answered unable to determine for cohort and case–control studies where there is no information concerning the source of patients included in the study. | ||||
| 22 | Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited over the same period of time? | □ | □ | □ |
| For a study that does not specify the time period over which patients were recruited, the question should be answered as unable to determine. | ||||
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | □ | □ | □ |
| This question should be answered no for trials if: the main conclusions of the study were based on analyses of treatment rather than intention to treat, the distribution of known confounders in the different treatment groups was not described, or the distribution of known confounders differed between the treatment groups but was not taken into account in the analyses. In nonrandomized studies, if the effect of the main confounders was not investigated or confounding was demonstrated but no adjustment was made in the final analyses, the question should be answered as no. | ||||
| 26 | Were losses of patients to follow‐up taken into account? | □ | □ | □ |
| If the number of patients lost to follow‐up is not reported, the question should be answered as unable to determine. If the proportion lost to follow‐up was too small to affect the main findings, the question should be answered yes. | ||||
Given the nature of the literature, quantitative synthesis of data was not possible. The multiple sources of heterogeneity observed across studies (in terms of participants and outcomes) meant that undertaking a formal meta‐analysis was not considered appropriate. Thus, the employment of Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) criteria recognizes that several of the criteria do not apply to this article. Heterogeneity among included studies was explored qualitatively. Studies were grouped according to whether the primary participants were providers or patients, and the outcome of interest (referral, enrollment, or both).
Results
A flow diagram depicting the search results, reasons for exclusion, and study selection is presented in the Figure 1. Overall, 17 articles were included in this systematic review.
Figure 1.
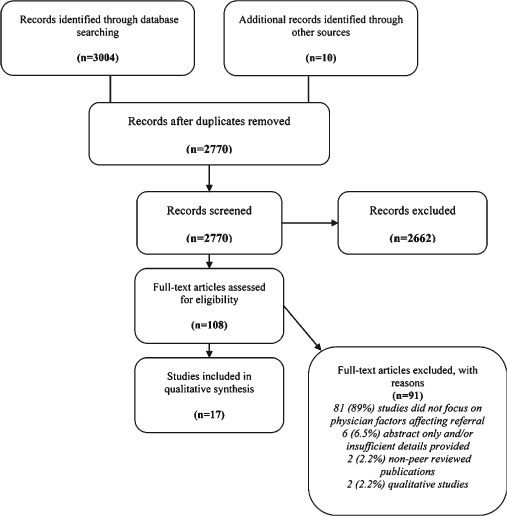
Flow diagram of study selection process.
Characteristics of Included Studies
Table 3 summarizes the methodological characteristics of the included studies. Included studies varied in methodology, type of participants, and type of outcomes reported. Eight (47%) studies were cross‐sectional in design,14, 17, 18, 19, 20, 21, 22, 23 8 (47%) were cohort studies (5 prospective24, 25, 26, 27, 28 and 3 retrospective29, 30, 31), and 1 (6%) study used a mixed‐methods design.32 Patients were the primary participants in the majority of included studies (n = 13, 76.5%14, 17, 19, 22, 23, 24, 25, 27, 28, 29, 30, 31, 32), whereas 3 (17.5%) studies included physicians as participants,18, 20, 21 and 1 (6%) study used both in a nested design.26 Seven (41%) studies14, 22, 23, 26, 27, 28, 32 reported CR enrollment as the outcome, 7 (41%) studies reported CR referral as the outcome,18, 19, 20, 21, 24, 30, 31 and 3 (17%) reported both.17, 25, 29 Nine (53%) studies were undertaken in the United States, 5 (29%) in Canada, and 1 (6%) each in Australia, China, and Scotland.
Table 3.
Characteristics of the Studies Included in This Review (N = 17)
| Study Author (Year), Country | Study Design | Subjects | Description of Sample and Size | Methods | Quality Assessment Classification (Points) |
|---|---|---|---|---|---|
| Ades et al. (1992), USA | Cross‐sectional | Patients | Cardiac inpatients eligible for CR, n = 226 | Guided interview: to collect demographic, medical, and psychosocial data. Telephone interview (prior to discharge or shortly thereafter): to describe the strength of their primary physician's recommendation regarding CR participation (graded from 1 to 5). | Fair (11) |
| Ayanian et al. (2002), USA | Retrospective cohort | Patients | Inpatients with a diagnosis of AMI, n = 35 520 | Patients identified in 7 states during 1994 and 1995. From Medicare claims, it was identified ambulatory visits to cardiologists, internists, and family practitioners. | Good (15) |
| Barber et al. (2001), USA | Cross‐sectional | Patients | Cardiac inpatients eligible for CR, n = 347 | Phase I patients: follow‐up by mail survey +3 months after discharge mailed questionnaire. Phase II patients: follow‐up by phone +6 weeks after discharge phone interview. | Good (16) |
| Bittner et al. (1999), USA | Prospective cohort | Patients | Cardiac inpatients after discharge and eligible for CR, n = 995 | Patients eligible for CR were identified from hospital discharge dataset. Referral rates to the CR program among patients hospitalized for CHD were computed over an 18‐month period. | Fair (10) |
| Dunlay et al. (2009), USA | Prospective cohort | Patients | Cardiac inpatients post‐MI after discharge and eligible to CR, n = 179 | Subjects completed a 46‐item questionnaire before hospital discharge (to measure health motivation, person's judgment of their own capacities as related to controlling their heart disease, and self‐assessment of health status, importance of CR to the patient, motivating factors, education, living situation, transportation availability, insurance, and fears and concerns about rehabilitation. | Good (15) |
| Grace et al. (2004), Canada | Cross‐sectional | Physicians | Primary care physicians, cardiologists, and cardiovascular surgeons, n = 179 | Survey included sociodemographic characteristics, a hypothetical case scenario, physicians were asked whether they would refer the patient, and a 26‐item questionnaire asking questions about patients characteristics influenced the physician's referral practices and physician's attitude about CR. | Good (14) |
| Grace et al. (2008), Canada | Prospective cohort | Patients Physicians | Cardiologists and outpatients; cardiologists, n = 97 and outpatients, n = 1268 | Cardiologists completed a survey regarding CR attitudes. Outpatients were surveyed prospectively to assess factors affecting CR enrollment. Patients were mailed a follow‐up survey 9‐months later to self‐report CR enrollment. The enrollment was checked by the CR site. | Good (18) |
| Grace, Grewal, Stewart (2008), Canada | Cross‐sectional | Physicians | Primary care physicians and cardiac specialists (cardiologists or cardiovascular surgeons); n = 104 primary care physicians and n = 81 cardiac specialists | Questionnaire application (mailed), which included sociodemographic items, and 26 investigator‐developed items scored on a 5‐point Likert scale about factors affecting physician's referral. | Fair (12) |
| Jones et al. (2003), Canada | Cross‐sectional, qualitative | Patients | Outpatients eligible to CR, enrollers and nonenrollers, n = 20 enrollers and n = 9 nonenrollers | A 16‐item questionnaire was used to measure the importance of variables that have been found to be associated with participation in CR. A semistructured interview guide was also developed to promote discussion of perceptions and experiences with CR. | Poor (6) |
| King et al. (2001), Canada | Prospective cohort | Patients | Cardiac inpatients ready for discharge after an AMI or CABG, n = 304 | Two weeks and 6 months after discharge, respondents were given a list of factors commonly thought to influence attendance at CR. | Fair (9) |
| Mak et al. (2005), China | Prospective cohort | Patients | Cardiac patients recruited for a phase I CR program (not proceeding to phase II), n = 41 | Evaluation of factors related to phase II: baseline assessment, comprehensive program and documentation of barriers. | Fair (7) |
| Missik (2001), USA | Cross‐sectional | Patients | Women enrolled and nonenrolled in CR after a cardiac event, n = 370 | A self‐reported instrument (eg, to collect data about physician referral to CR, health insurance coverage) and medical records reviews were used to collect data. | Fair (12) |
| Pell et al. (1996), Scotland | Retrospective cohort | Patients | Inpatients with a discharge diagnosis of MI, n = 881 | Scottish morbidity record data were used to identify all patients discharged from Glasgow hospitals from June 1994 to November 1994 with MI. | Fair (11) |
| Scott et al. (2005), Australia | Retrospective cohort | Patients | Patients who died or were discharged after troponin‐positive ACS, n = 2156 | The proportion of highly eligible patients in total and in each category who received specific clinical interventions during admission or at discharge were determined at the level of individual patients using intervention‐specific eligibility criteria derived from evidence‐based clinical practice guidelines. | |
| Stiller and Holt (2004), USA | Cross‐sectional | Patients | Outpatients with at least 1 cardiac diagnosis and eligible for phase II CR, n = 203 | Participants were approached before their discharge from the hospital. Three‐weeks after their discharge, patients were mailed a questionnaire. Patients were also contacted by phone. | Fair (9) |
| Suter et al. (1992), USA | Cross‐sectional | Physicians | Cardiologists, cardiovascular surgeons, internists, and family practitioners, n = 32 | Contact letter (physicians randomly selected). Those who responded receive a questionnaire and should return it within 2 weeks. Thirty‐two questionnaires returned. | Poor (4) |
| Yates et al. (2003), USA | Cross‐sectional | Patients | Cardiac inpatients hospitalized over a 1‐year period at a regional (rural) medical center, n = 222 | Mail surveys. | Good (13) |
Abbreviations: ACS, acute coronary syndrome; AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; CR, cardiac rehabilitation; MI, myocardial infarction.
Hypothetical.
Started.
Completed.
The quality of the all studies was assessed and ratings are shown in Table 3. Overall, 7 (41%) studies were considered good, 8 (47%) fair, and 2 (12%) were considered poor.
Physician Factors Affecting CR Referral
Medical Specialty
Table 4 is a summary of findings of the studies included in this review. Having an appointment with a cardiologist or a cardiac surgeon at discharge, or seeing a cardiologist while hospitalized was identified by 3 studies as a significant correlate of CR referral, from the perspective of both patients and physicians.19, 29, 31 The Barber et al. study,17 in particular, found that at hospital discharge, patients scheduled for an appointment with a cardiologist or a cardiac surgeon had more than twice the odds of being referred to CR when compared to patients scheduled with a family physician (P < 0.02). However, 2 studies did not find a significant relationship between cardiologist involvement and CR referral.24, 30
Table 4.
Summary of Findings of the Studies Included in this Review (N = 17)
| Study Author (Year), Country | CR Outcome | Physician Factor | Results |
|---|---|---|---|
| Ades et al. (1992), USA | Enrollment | Strength of the primary physician's recommendation | Low physician recommendation to CR: participation was 1.8%; high physician recommendation to CR: participation was 66% (P < 0.0001) |
| Ayanian et al. (2002), USA | Referral | Appointment with a cardiologist | Patients who saw a cardiologist were more likely to be referred that those who did not to report having received CR (P = 0.03). |
| Barber et al. (2001), USA | Referral, enrollment | Appointment at discharge with a cardiologist/cardiac surgeon | Appointment with a cardiac specialist compared to family physician at hospital discharge: referral to CR (OR = 2.33, P < 0.02); 6–12 weeks postdischarge: enrollment (OR = 1.44, P < 0.001). |
| Bittner et al. (1999), USA | Referral | Appointment at discharge with a cardiologist/cardiac surgeon | Trend toward higher referral rates among cardiologists compared with cardiovascular surgeons, internists, and other medical specialties (P value not provided). |
| Dunlay et al. (2009), USA | Referral, enrollment | In‐hospital care by a cardiologist, referral | Factors related to enrollment: in‐hospital care by a cardiologist (P < 0.001, OR = 18.82); being referred while in hospital (P < 0.001, OR = 12.16). Independent factors related to CR enrollment: being referred while in hospital (P < 0.001, OR = 6.14). |
| Grace et al. (2004), Canada | Referral | Physicians' perceptions of referral practices, medical specialty | Factors related to referral: geographic access, uncertainty regarding which provider was responsible for referral, perceptions of patient motivation, multifactorial nature of CR, patient characteristics. Family physicians were less likely to refer than cardiologists and cardiac surgeons (P < 0.001). |
| Grace et al. (2008), Canada | Enrollment | Recommendation of CR, intentions to refer, positive perceptions of CR | Physician factors related to CR enrollment: recommendation of CR utilization was significant (P = 0.01). Intentions to refer (P = 0.79) and positive perceptions of CR (P = 0.15) were not significant. |
| Grace, Grewal, Stewart (2008), Canada | Referral | Medical specialty, physicians' perceptions of CR | Primary care physicians were more likely to endorse lack of familiarity with CR site locations (P < 0.001), lack of standardized referral forms (P < 0.001), inconvenience (P = 0.04), program quality (P = 0.004), lack of discharge communication from CR (P = 0.001) as factors negatively impacting CR referral practices than cardiac specialists. Cardiac specialists were significantly more likely to perceive their colleagues (P < 0.001) and department (P < 0.001) as regularly referring patients, intend to refer their patients (P < 0.001), and enlist assistance completing their CR referral forms by allied healthcare professionals in their practice (P = 0.04) than primary care physicians. |
| Jones et al. (2003), Canada | Enrollment | Physician recommendation | Physician recommendation was significant factor for patients when deciding to enroll or not (P < 0.05). |
| King et al. (2001), Canada | Enrollment | Physician recommendation | A factor for patients who decided to enroll (68% of patients were influenced by physicians). |
| Mak et al. (2005), China | Enrollment | Physician recommendation, referral | CR enrollment was associated with being referred by a physician (7% of patients identified lack of referral as a barrier to CR enrollment). |
| Missik (2001), USA | Enrollment | Physician referral | Women's participation in CR was related to physician referral (P < 0.001). |
| Pell et al. (1996), Scotland | Referral, enrollment | Appointment with a cardiac specialist | Referral: more likely to be referred to CR than if seen by general physician (OR = 1.59, P < 0.05). Enrollment: more likely to enroll in CR than if seen by a general physician (OR = 2, P < 0.05). Type of consultant: associated with referral (OR = 0.63, P < 0.05). |
| Scott et al. (2005), Australia | Referral | Cardiologist involvement | Cardiologist involvement (transfer or nontransfer to cardiology unit) was not related to CR referral (P = 1.0). |
| Stiller and Holt (2004), USA | Referral | Physician sex | The only variable related to referral was physician sex (P = 0.02, OR = 13.05) (small sample size: female physicians = 4, male = 21). |
| Suter, Bona, Suter (1992), USA | Referral | Perceptions of CR | Majority of respondents indicated that patients who have survived a MI or have undergone CABG are most likely to benefit from outpatient CR. Reasons for nonreferral: unlikelihood of medical insurance coverage, perceived lack of patient motivation, perceptions of unqualified CR staff, practical reasons (distance), and safety concerns. |
| Yates et al. (2003), USA | Enrollment | Physician recommendation, referral | Patients were more likely to participate if their physician explained its benefits (OR = 6.54) and if they were told about it during hospitalization (OR = 4.12, P < 0.001). |
Abbreviations: ACS, acute coronary syndrome; AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; CR, cardiac rehabilitation; OR, odds ratio.
Attitudes toward CR and referral of a hypothetical patient were examined and compared by medical specialty in another study.18 Results showed that medical specialty was significantly related to referral, such that family physicians were less likely than specialty providers to refer. Grace et al20 went on to examine factors affecting referral practices among generalists vs specialists. Two groups of physicians (104 primary care physicians and 81 cardiac specialists) were surveyed. When compared to cardiac specialists, primary care physicians were more likely to endorse lack of familiarity with CR site locations (P < 0.001), lack of standardized referral forms, inconvenience, program quality, and lack of discharge communication from CR as factors negatively impacting CR referral practices, and less likely to perceive their colleagues and department as regularly referring patients, intending to refer their patients, and to enlisting assistance completing their CR referral forms by allied health professionals in their practice than primary care physicians.20 When asked what are the most important factors affecting referral to CR, primary care physicians and cardiac specialists reported geographic accessibility, patient motivation, patient benefit, medical characteristics of patients (ie, obesity, sedentary lifestyle), quality of the program, knowledge of available programs, the nature of the referral process, and patient age.20 In addition, primary care physicians reported that referral to CR was another physician's responsibility and cardiac specialists reported CR as the standard of care.
Physician Reports of Their Reasons for CR Referral
Two studies examined physician perceptions of factors affecting their referral practices.18, 21 In 1 of the studies by Grace et al.,18 179 physicians (primary care, cardiologists, or cardiac surgeons) from Ontario, Canada completed a mailed survey to describe their preferences in managing cardiac patients and the barriers they face in referring patients to CR. When asked to report the most important factors affecting their referral of patients to CR, the physicians most frequently identified geographic access, perceptions of patient motivation, reported patient benefit, and medical indications for CR such as risk factors.18 Factor analysis of Likert‐type responses to 26 attitudinal items revealed 4 referral factors: beliefs about the benefits of CR, patient characteristics (eg, motivation), awareness of CR sites and referral processes, and referral norms.18
In the other study by Suter et al.,21 32 physicians (cardiologists, cardiovascular surgeons, internists, and family practitioners) from Arkansas completed a mailed survey that asked why a physician would not refer a patient with cardiovascular disease to CR. Almost half identified lack of insurance coverage, and nearly 40% cited lack of patient motivation.21 In addition, 25% identified practical reasons for nonreferral (most often inconvenience due to distance), and about 5% identified safety concerns.21
Physician Sex
This characteristic was identified in 1 study,19 and was the only significant physician characteristic related to referral (P = 0.02), with male physicians more likely to refer than female physicians. However, careful consideration must be given to this study, because the proportion of physicians who were female (n = 4) was significantly smaller than males. Physician sex was unrelated to referral of a hypothetical patient in a study by Grace et al20 and also unrelated to patient referral in a multilevel study of outpatients of 97 physicians.33
Physician Factors Affecting Patient Enrollment in CR
Physician Recommendations
This review has identified the strength of physician recommendations as the most consistently identified factor affecting patient CR enrollment. This finding was supported in 6 studies,14, 23, 26, 27, 28, 32 and there were no negative or null findings related to the association between recommendation and patient enrollment.
In an early and seminal study of 22 666 cardiac inpatients eligible for CR, Ades et al14 found that CR participation was significantly related to the strength of the primary care physician recommendations. With post hoc analysis of patient characteristics related to the strength of physician recommendations, it was found that older age and female sex were significantly related to fewer positive recommendations by physicians.14 Similarly, additional research in Canada found that those patients who enrolled in the program perceived moderately strong physician recommendations to enroll, whereas those who did not enroll perceived either weak or no recommendations at all.14
Medical Specialty
Having an appointment with a cardiologist or a cardiac surgeon at discharge or seeing a cardiologist while hospitalized is shown not only to relate to referral but also to enrollment. In the study by Dunlay et al.,25 patients who were primarily cared for by a cardiologist in the hospital and received recommendations about CR during this period had much higher rates of enrollment. According to Barber et al.,17 an appointment with a cardiac specialist and referral at discharge had a strong effect on enrollment, with patients referred by cardiologists or cardiac surgeons having more than 4 times greater odds of participation (P < 0.001), as long as the referral was made at discharge.17
Being Referred
This review identified 6 studies where CR enrollment was strongly associated with being referred by a physician.17, 22, 23, 25, 26, 28 For instance, in a comparative study by Missik,22 370 women (CR participants and nonparticipants) completed a self‐reported instrument to identify factors related to their participation in CR. Results showed that women's enrollment in CR was primarily related to a single factor: physician referral.
Physician Attitudes Toward CR
In a multilevel study of cardiac outpatients and their providers, several physician attitudes were shown to relate to patient CR enrollment in bivariate analyses.26 Lower rates of CR enrollment were related to patients whose cardiologists were more skeptical about the benefits of CR, who considered the local CR program to be of poorer quality, and who had previous negative experience with a CR program.26
Discussion
Although reviews of patient‐level factors affecting CR referral and enrollment can easily be found in the literature,7, 33, 34, 35 few reviews have focused on the physician level.30 This review has demonstrated that physician factors are consistently related to CR referral and patient enrollment. First and foremost, the role of physician recommendations in promoting patient enrollment was reinforced, as highlighted in a recent American Heart Association Science Advisory.7 Second, variation in CR referral by medical specialty was also consistently demonstrated, with specialists more likely to refer than generalists. Third, factors related to a physician's propensity to refer were synopsized. Normative referral practice, proximate availability of CR programs of which physicians are familiar, and physician perceptions of patient motivation to participate in CR for example, were also related to their referral.
Having an appointment with a cardiologist or a cardiac surgeon at discharge, or seeing a cardiologist while hospitalized, were identified as important factor associated with CR referral from both patient and physician perspectives.17, 29, 31 A provider effect was observed in the referral of cardiac patients to CR; merely scheduling an appointment with a cardiac specialist significantly increased the likelihood of a patient being referred to CR at the time of discharge. Although it is preferred for patients to be referred prior to hospital discharge to mitigate lengthy waits to initiate CR services,13 this finding is also troubling. Studies have shown that access to cardiologists varies substantially according to characteristics of the patient (ie, low socioeconomic status) and the hospital (ie, academic vs community, whether it has a CR program).36 Therefore, there is a need for more medical education and training about CR benefits for primary care physicians treating cardiac patients regarding the vital role of CR in outpatient care. Moreover, better communication between specialists and primary care physicians is needed to ensure the referral is made, and that it is made early in the patient care journey.13 Although there were no randomized trials of interventions to promote referral among primary care physicians identified in this review, the Davies et al37 Cochrane review of randomized trials to promote CR uptake identified a successful study, whereby nurses integrated into general physician practices were successful in ensuring great CR use. This may also serve as an appropriate strategy to CR referral gaps in the community.
With regard to CR enrollment, patients identified the strength of a physician's recommendation as the most important factor. An article published recently shows that patients who perceive greater physician CR endorsement were over 2 times more likely to enroll (odds ratio = 2.0738). They also show that such endorsements are related to significantly greater patient participation in CR, whereby patients who perceived greater endorsement attended a significantly greater number of prescribed sessions than those perceiving lesser physician endorsement. It was disconcerting to note, however, that in the seminal study by Ades et al.,14 older and female patients perceived significantly lower endorsements of CR. This more recently published study by Tsui et al38 also replicates and extends these findings, showing that women and older patients perceived significantly lower physician endorsements for CR, and also that patients with lower income, lower education, and who were retired perceived lower endorsements as well. These findings reiterate the treatment‐risk paradox, such that vulnerable patients who arguably stand to gain the most benefit from CR are least likely to access it.
Another study identified in the Cochrane review of randomized trials promoting uptake37 demonstrated the effectiveness of a motivational CR letter provided to patients.39 This may be particularly helpful given the variation in perceived physician endorsements, particularly among vulnerable patients. If such patient education material could be combined with physician endorsements, this would perhaps ensure all patients are receiving the same information about CR. Such a letter may also have the added benefit of reminding or prompting physicians to initiate the CR referral and corresponding discussion with the patient. In addition, there is a newer body of evidence in regard to the efficacy of motivational interviewing.
The findings presented in this review should be interpreted with caution. The studies reviewed herein are limited with respect to sample, design, and measurement. Regarding sample and design, most studies were conducted at a single center with little patient diversity (ie, gender, socioeconomic status), therefore limiting generalizability. In addition, physicians and patients who responded to surveys about CR are likely different than nonresponders such that they are more positive in their attitudes about CR. Second, many of the studies were cross‐sectional in design, making causal conclusions impossible. Potential biases in the review process were minimal.
Conclusion
This review has reiterated the important role of physician referrals and endorsements of CR to patients in the use of these proven services. Moreover, findings underscore the variation in CR referral by physician specialty and the lower physician CR endorsements for patients who may be less likely to access these services. Physician endorsement at the time of CR referral should be considered to promote universally effective messaging to all indicated patients.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Roger VL, Go AS, Lloyd‐Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stone JA, Arthur HM, Suskin N, eds. Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention: Translating Knowledge Into Action. 3rd ed Winnipeg, Canada: Canadian Association of Cardiac Rehabilitation; 2009. [Google Scholar]
- 3. Heran BS, Chen JM, Ebrahim S, et al. Exercise‐based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7):CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise‐based cardiac rehabilitation post‐myocardial infarction: a systematic review and meta‐analysis of randomized controlled trials. Am Heart J 2011;162:571–584.e2. [DOI] [PubMed] [Google Scholar]
- 5. American Association of Cardiovascular and Pulmonary Rehabilitation . Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 4th ed. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 6. British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, Stroke Association . JBS2. Joint British Societies' guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;61:1–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arena R, Williams M, Forman DE, et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: the valuable role of healthcare professionals in the inpatient and home health settings: a science advisory from the American Heart Association. Circulation. 2012;125:1321–1329. [DOI] [PubMed] [Google Scholar]
- 8. Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. [DOI] [PubMed] [Google Scholar]
- 9. Suaya JA, Shepard DS, Normand SL, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. [DOI] [PubMed] [Google Scholar]
- 10. Bethell HJ, Evans JA, Turner SC, et al. The rise and fall of cardiac rehabilitation in the United Kingdom since 1998. J Public Health (Oxf). 2007;29:57–61. [DOI] [PubMed] [Google Scholar]
- 11. Dafoe W, Arthur H, Stokes H, et al.; Canadian Cardiovascular Society Access to Care Working Group on Cardiac Rehabilitation. Universal access: but when? Treating the right patient at the right time: access to cardiac rehabilitation. Can J Cardiol. 2006;22:905–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Scott LA, Ben‐Or K, Allen JK. Why are women missing from outpatient cardiac rehabilitation programs? A review of multilevel factors affecting referral, enrollment, and completion. J Womens Health. 2002;11:773–791. [DOI] [PubMed] [Google Scholar]
- 13. Grace SL, Russell KL, Reid RD, et al. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Int Med. 2011;171:235–241. [DOI] [PubMed] [Google Scholar]
- 14. Ades PA, Waldmann ML, McCann WJ, et al. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–1035. [PubMed] [Google Scholar]
- 15. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20:21–35. [DOI] [PubMed] [Google Scholar]
- 17. Barber K, Stommel M, Kroll J, et al. Cardiac rehabilitation for community‐based patients with myocardial infarction: factors predicting discharge recommendation and participation. Clinical Epidemiol. 2001;54:1025–1030. [DOI] [PubMed] [Google Scholar]
- 18. Grace SL, Evindar A, Abramson BL, et al. Physician management preferences for cardiac patients: factors affecting referral to cardiac rehabilitation. Can J Cardiol. 2004;20:1101–1107. [PubMed] [Google Scholar]
- 19. Stiller JJ, Holt MM. Factors influencing referral of cardiac patients for cardiac rehabilitation. Rehabil Nurs. 2004;29:18–23. [DOI] [PubMed] [Google Scholar]
- 20. Grace SL, Grewal K, Stewart DE. Factors affecting cardiac rehabilitation referral by physician specialty. J Cardiopulm Rehabil Prev. 2008;28:248–252. [DOI] [PubMed] [Google Scholar]
- 21. Suter P, Bona S, Suter W. Views of Arkansas physicians on cardiac rehabilitation. J Cardiopul Rehab. 1992;12:32–35. [Google Scholar]
- 22. Missik E. Women and cardiac rehabilitation: accessibility issues and policy recommendations. Rehabil Nurs. 2001;26:141–147. [DOI] [PubMed] [Google Scholar]
- 23. Yates BC, Braklow‐Whitton JL, Agrawal S. Outcomes of cardiac rehabilitation participants and nonparticipants in a rural area. Rehabil Nurs. 2003;28:57–63. [DOI] [PubMed] [Google Scholar]
- 24. Bittner V, Sanderson B, Breland J, et al. Referral patterns to a university‐based cardiac rehabilitation program. Am J Cardiol. 1999;83:252–255. [DOI] [PubMed] [Google Scholar]
- 25. Dunlay SM, Witt BJ, Allison TG, et al. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Grace SL, Gravely‐Witte S, Brual J, et al. Contribution of patient and physician factors to cardiac rehabilitation enrollment: a prospective multilevel study. Eur J Cardiovasc Prev Rehabil. 2008;15:548–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. King KM, Humen DP, Smith HL, et al. Predicting and explaining cardiac rehabilitation attendance. Can J Cardiol. 2001;17:291–296. [PubMed] [Google Scholar]
- 28. Mak YM, Chan WK, Yue CS. Barriers to participation in a phase II cardiac rehabilitation programme. Hong Kong Med J. 2005;11:472–475. [PubMed] [Google Scholar]
- 29. Pell J, Pell A, Morrison C, et al. Retrospective study of influence of deprivation on uptake of cardiac rehabilitation. BMJ. 1996;313:267–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Scott IA, Duke AB, Darwin IC, et al. Variations in indicated care of patients with acute coronary syndromes in Queensland hospitals. Med J Aust. 2005;182:325–330. [DOI] [PubMed] [Google Scholar]
- 31. Ayanian JZ, Landrum MB, Guadagnolu E, et al. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med. 2002;347:1678–1686. [DOI] [PubMed] [Google Scholar]
- 32. Jones LW, Farrell JM, Jamieson J, et al. Factors influencing enrollment in a cardiac rehabilitation exercise program. Can J Cardiovasc Nurs. 2003;13:11–15. [PubMed] [Google Scholar]
- 33. Daly J, Sindone AP, Thompson DR, et al. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002;17:8–17. [DOI] [PubMed] [Google Scholar]
- 34. Cooper AF, Jackson G, Weinman J, et al. Factors associated with cardiac rehabilitation attendance: a systematic review of literature. Clin Rehabil. 2002;16:541–552. [DOI] [PubMed] [Google Scholar]
- 35. Jackson L, Leclerc J, Erskine Y, et al. Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors. Heart. 2005;91:10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Alter DA, Iron K , Austin PC, et al.; SESAMI Study Group. Socioeconomic status, service patterns, and perceptions of care among survivors of acute myocardial infarction in Canada. JAMA. 2004;231:1100–1107. [DOI] [PubMed] [Google Scholar]
- 37. Davies P, Taylor F, Beswick A, et al. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2010;(7):CD007131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tsui CK, Shanmugasegaram S, Jamnik V, et al. Variation in patient perceptions of healthcare provider endorsement of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2012;32:192–197. [DOI] [PubMed] [Google Scholar]
- 39. Wyer SJ, Earll L, Joseph S, et al. Increasing attendance at a cardiac rehabilitation programme: An intervention study using the theory of planned behaviour. Coronary Health Care. 2001;5:154–159. [Google Scholar]


