Abstract
Basidiobolomycosis is a rare fungal infection caused by Basidiobolus ranarum a worldwide environmental saprophyte fungus that is potentially a pathogen. B ranarum mainly affects the subcutaneous tissues but gastrointestinal and disseminated infections rarely have been reported previously. We report a case of B ranarum infection in a 12-year-old immunocompetent boy presented with abdominal pain from 2 months earlier before admission in the hospital. Abdominal CT scan revealed a lobulated mass-like lesion in the vicinity of right lower quadrant enveloping ascending colon and terminal ileum with involvement of mesentery. Histopathological examination showed severe full-thickness infiltration of inflammatory cells mainly eosinophils admixed with multinucleated giant cells and large areas of necrosis with granulomatous feature. Periodic acid Schiff staining demonstrated thin-walled septate fungal hyphae's surrounded by eosinophilic material (Splendore-Hoppeli phenomenon) identified as a basidiobolomycosis.
Background
Basidiobolomycosis is a fungal infection caused by Basidiobolus ranarum belonging to the zygomycetes family manifested by chronic subcutaneous infections with worldwide spread pattern.1–19 First it has been reported from the USA and then with lower incidence rate in East and West Africa, Indonesia, Iran, Saudi Arabia and India.1–19 Rarely it may affect gastrointestinal (GI) tract, retroperitoneum, pulmonary and nasal cavity rather than subcutaneous tissues. Its rarity may cause difficulties and delay in diagnosis, and therefore there is a high mortality rate especially in paediatrics.2–19 Patients might be presented with abdominal pain, mass-like lesions, peripheral blood eosinophilia and fever. Disseminated onset, a fatal form, has been reported recently in immunocompetent as well as immunocompromised patients but it is extremely rare.3 The route of the infection is mysterious and should be reserved in the soil, decayed organic, GI tract matters of amphibians, fish, reptiles and insectivorous bats.1–19 We report a case of basidiobolomycosis in a 12-year-old boy presented with abdominal pain and mass-like lesion in the right lower quadrant that at first misdiagnosed as a colonic malignant tumour clinically and radiologically. Rarity of the disorder in our country (Iran) with non-specific clinical presentation introduced it as a mysterious infection, an unknown condition for our specialists, so we start briefly discussion of GI basidiobolomycosis manifestations by looking towards radiological, clinical and histopathological characteristics.
Case presentation
A 12-year-old boy was admitted to emergency ward with abdominal pain, haematuria and fever. The patient was from south of Iran (Minab city in Hormozgan province) a tropical climate area. Based on the clinical history his progressive abdominal pain had started 2 months prior to admission. On physical examination he had abdominal tenderness in the right lower quadrant and no history of previous travelling to other countries was observed.
Investigations
Complete blood count showed leucocytosis (14 500/mm3) with neutrophilia (90%), haemoglobin (Hg 9.8 g/dL; normal range 4–10×1000/µL), haematocrit (32.9%) and red blood cell distribution width (19.8%; normal range 10.4–14.6%). Urine analysis showed presence of protein (1+), red blood cells (3+) with white cell count (7–8). Erythroid sedimentation rate (ESR) was increased up to 96 mm/h (normal range <15) and C reactive protein (CRP) was reported (positive 3+). Sodium as well as potassium rates were lower than normal (sodium 118 mEq/L and potassium 2.9 mEq/L) (normal range for sodium 132–146 mEq/L and for potassium 3.5–5.3 mEq/L). Serum ferritin was 624.8 ng/mL (men 40–430 ng/mL). Urea 67 mg/dL (normal range 15–50). In direct stool examination red blood cells (12–14/high power field) were reported but ova of parasites was not seen. Abdominal sonography showed thickening of ileum terminalis and ascending colon with right hydronephrosis grade 2. CT scan showed a lobulated mass-like lesion in the vicinity of right lower quadrant enveloping ascending colon and terminal ileum with involvement of the mesentery and anterior abdominal wall. Partial obstruction of the lumens by the lesion especially in the junction of the caecum and terminal ileum was noted (figure 1A,B).
Figure 1.
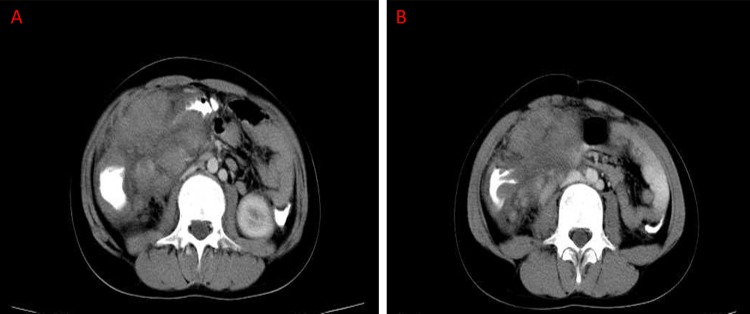
(A) CT scan revealing a lobulated mass like lesion in the vicinity of right lower quadrant enveloping ascending colon and terminal ileum. (B) CT scan demonstrating enveloping ascending colon by the lesion with involvement of the mesentery and anterior abdominal wall.
The patient underwent terminal ileum and caecal resection with right hemicolectomy (measuring 50×10 cm). The tumour was located at 20 cm from the ileocecal valve and extended to mid-portion of right ascending colon. On cut surface the tumour had a firm consistency, pink-grey-yellowish coloured surface and almost totally obstructed the colonic lumina and thickened ileum terminalis and caecal wall (figure 2). Pericolic fatty tissue was also involved and regional lymph nodes were enlarged. Histopathological examination showed colonic wall that was severely infiltrated by inflammatory cells mostly eosinophil's, neutrophils and lymphoplasma cells admixed with multinucleated giant cells contain foreign body-like structures (figure 3A,B). Eosinophil's aggregated in microabscess formations with large areas of necrosis surrounded by young fibroblasts. Inflammatory cells spread through serosa and pericolic fatty tissue. Lymph nodes were also involved by necrosis and inflammatory cells infiltration. Histopathological findings were suggestive of inflammatory bowel disease, GI tuberculosis and other infectious diseases. In periodic acid Schiff (PAS) staining numerous thin-walled septate fungal hyphae surrounded by eosinophilic proteinaceous material were seen (Splendore-Hoppeli phenomenon) determined as a basidiobolomycosis (figure 4A–D). One week after the first operation and prescription of oral itraconazole (100 mg/twice daily) the patient presented with vomiting, abdominal pain, postsurgery entrocutaneous fistula formation, high-degree fever, imbalance of electrolytes, increased urea and toxic condition. After treatment of water-electrolyte imbalance and stabilisation of the patient's condition, amphotericin B was prescribed for him.
Figure 2.

Resected tumour had a firm consistency, pink-grey-yellowish coloured surface and near totally obstructed the colonic lumina with thickened ileum terminalis and caecal wall.
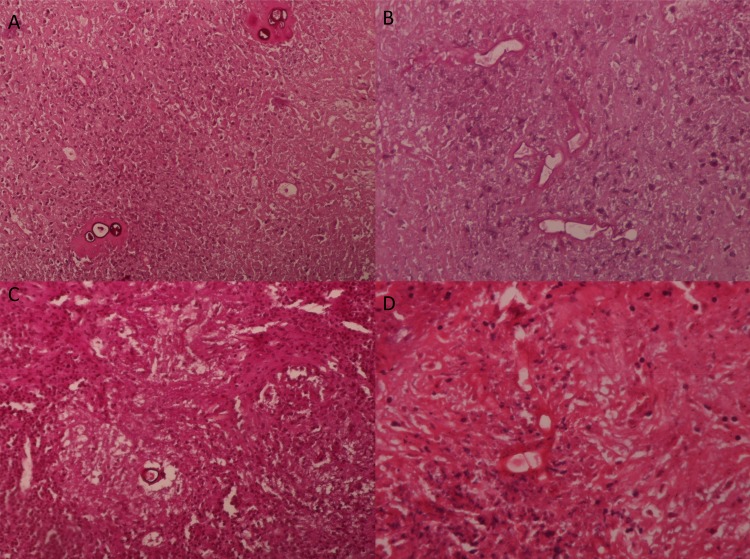
Figure 3.
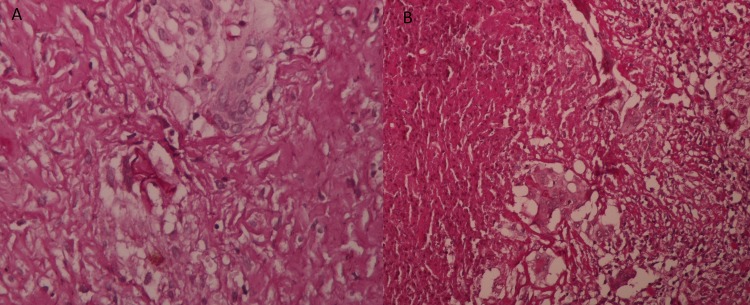
(A and B) Severely infiltration of colonic tissue by inflammatory cells mostly eosinophils, neutrophils and lymphoplasma cells admixed with multinucleated giant cells contain foreign body-like structures (H&E staining, objective ×40).
Figure 4.
(A and B) Numerous thin-walled septate fungal hyphae were seen surrounded by eosinophilic proteinecoius material ((Splendore-Hoppeli phenomenon) determining basidiobolomycosis (periodic acid Schiff staining, objective ×20). (C and D) Thin-walled fungal structures surrounded by eosinophilic material (H&E staining, objective ×20).
Differential diagnosis
In differential diagnosis of severe infiltration of inflammatory cells, especially eosinophilic microabscess formation admixed with multinucleated giant cells, one should consider inflammatory bowel disease such as Crohn's disease that has a similar histopathological findings and is involved in the colon and the ileum terminalis (backwash ileitis). Second differential diagnosis could be intestinal tuberculosis which produces granulomatous inflammation with central caseous necrosis and multinucleated giant cells, foreign body and Langhans type. In rare conditions fungal infections such as basidiobolomycosis should be considered despite its rarity but high mortality rate, for confirmation PAS staining should be performed. Sarcoidosis or amoebiasis might be placed in the bottom of the list of diagnosis.
Treatment
After surgical resection of the salient lesion itraconazole (100 mg/twice daily) and in the second admission amphotericin B were prescribed. Despite 2 weeks prescription of amphotericin B, there was no relief in fever and abdominal pain; however, itraconazole (100 mg/twice daily) therapy was continued.
Outcome and follow-up
The general condition of the patient did not improve despite treatment. After acute onset of a severe septic shock and pulmonary insufficiency the patient expired.
Discussion
Basidiobolomycosis is a saprophyte fungal infection caused by B ranarum and it affects mainly the subcutaneous tissues in young men after traumatic inoculation. B ranarum is a member of the zygomycetes and subphylum Entomophthoromycotina.1–19 In the past GI involvement was rarely reported.4–6 Disseminated basidiobolomycosis, a least common form, also was reported with high mortality rate.3 The route of visceral involvement is unknown and immunecompetent and immunocompromised patients could be infected via ingestion of contaminated soil, animal faeces or foods. Diagnosis of GI basidiobolomycosis is difficult because of its rarity and non-specific clinical and radiological manifestations.1–19 In all reported cases leucocytosis with eosinophilia, ESR elevation with positive CRP reaction were reported but our patient had a leucocytosis without eosinophilia. Our case had renal function impairment with haematuria, electrolytes imbalance and increased urea that has not been reported in any of the previous cases. Histopathological findings are similar to inflammatory bowel disease (Crohn's disease), GI tuberculosis, amoebiasis and sarcoidosis, generally misdiagnosed causing delay in treatment. One clue is severe infiltration of inflammatory cells with eosinophilic microabscess formation, a finding that could suggest basidiobolomycosis. Culture is a gold standard but histopathological findings composed of Splendore-Hoeppli phenomenon is diagnostic for this type of fungal infection and confirmed the diagnosis. Treatment with itraconazole seems to be more effective than other antifungal drugs such as amphotericin B.2–19 But in our patient neither of them (itraconazole and amphotericin B) was effective and he died with septic shock and pulmonary insufficiency.
In conclusion GI basidiobolomycosis is a rare and mysterious fungal infection that mimic malignant tumour and should be considered in the differential diagnosis of GI mass lesions, among both immunecompetent and immunecompromised patients. Delay in diagnosis and disseminated type could be life-threatening.
Learning points.
Gastrointestinal (GI) basidiobolomycosis could simulate malignant lesions and should be considered as one of the differential diagnosis of mass like lesions in GI tract.
Delay in diagnosis of basidiobolomycosis could be life-threatening and antifungal treatment should be considered as soon as possible.
Tissues with severe infiltration of inflammatory cells especially numerous eosinophils admixed with multinucleated giant cells should be stained by periodic acid Schiff staining method to reveal possible fungal infection.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Centers for Disease Control and Prevention (CDC) Gastrointestinal basidiobolomycosis-Arizona, 1994–1999. MMWR Morb Mortal Wkly Rep 1999;2013:710–13 [PubMed] [Google Scholar]
- 2.Nemenqani D, Yaqoob N, Khoja H, et al. Gastrointestinal basidiobolomycosis: an unusual fungal infection mimicking colon cancer. Arch Pathol Lab Med 2009;2013:1938–42 [DOI] [PubMed] [Google Scholar]
- 3.van den Berk GE, Noorduyn LA, van Ketel RJ, et al. A fatal pseudo-tumour: disseminated basidiobolomycosis. BMC Infect Dis 2006;2013:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khan ZU, Khoursheed M, Makar R, et al. Basidiobolus ranarum as an etiologic agent of gastrointestinal zygomycosis. J Clin Microbiol 2001;2013:2360–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussein MR, Musalam AO, Assiry MH, et al. Histological and ultrastructural features of gastrointestinal basidiobolomycosis. Mycol Res 2007;2013:926–30 [DOI] [PubMed] [Google Scholar]
- 6.Geramizadeh B, Foroughi R, Keshtkar-Jahromi M, et al. Gastrointestinal basidiobolomycosis, an emerging infection in the immunocompetent host: a report of 14 patients. J Med Microbiol 2012;2013:1770–4 [DOI] [PubMed] [Google Scholar]
- 7.El-Shabrawi MH, Kamal NM. Gastrointestinal basidiobolomycosis in children: an overlooked emerging infection?. J Med Microbiol 2011;2013:871–80 [DOI] [PubMed] [Google Scholar]
- 8.Al Jarie A, Al-Mohsen I, Al Jumaah S, et al. Pediatric gastrointestinal basidiobolomycosis. Pediatr Infect Dis J 2003;2013:1007–14 [DOI] [PubMed] [Google Scholar]
- 9.Lyon GM, Smilack JD, Komatsu KK, et al. Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literature. Clin Infect Dis 2001;2013:1448–55 [DOI] [PubMed] [Google Scholar]
- 10.Vikram HR, Smilack JD, Leighton JA, et al. Emergence of gastrointestinal basidiobolomycosis in the United States, with a review of worldwide cases Crowell MD. Clin Infect Dis 2012;2013:1685–91 [DOI] [PubMed] [Google Scholar]
- 11.Saadah OI, Farouq MF, Daajani NA, et al. Gastrointestinal basidiobolomycosis in a child; an unusual fungal infection mimicking fistulising Crohn's disease. J Crohns Colitis 2012;2013:368–72 [DOI] [PubMed] [Google Scholar]
- 12.Yousef OM, Smilack JD, Kerr DM, et al. Gastrointestinal basidiobolomycosis. Morphologic findings in a cluster of six cases. Am J Clin Pathol 1999;2013:610–16 [DOI] [PubMed] [Google Scholar]
- 13.Wasim Yusuf N, Assaf HM, Rotowa NA. Invasive gastrointestinal Basidiobolus ranarum infection in an immunocompetent child. Pediatr Infect Dis J 2003;2013:281–2 [PubMed] [Google Scholar]
- 14.Zavasky DM, Samowitz W, Loftus T, et al. Gastrointestinal zygomycotic infection caused by basidiobolus ranarum: case report and review. Clin Infect Dis 1999;2013:1244–8 [DOI] [PubMed] [Google Scholar]
- 15.Bigliazzi C, Poletti V, Dell'Amore D, et al. Disseminated basidiobolomycosis in an immunocompetent woman. J Clin Microbiol 2004;2013:1367–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Shanafey S, AlRobean F, Bin Hussain I. Surgical management of gastrointestinal basidiobolomycosis in pediatric patients. J Pediatr Surg 2012;2013:949–51 [DOI] [PubMed] [Google Scholar]
- 17.Radjou AN, Rajesh NG. Intestinal obstruction due to basidiobolus ranarum: an unusual case. Indian J Med Microbiol 2011;2013:186–8 [DOI] [PubMed] [Google Scholar]
- 18.Vera A, Hubscher SG, McMaster P, et al. Invasive gastrointestinal zygomycosis in a liver transplant recipient: case report. Transplantation 2002;15;2013:145–7 [DOI] [PubMed] [Google Scholar]
- 19.Fahimzad A, Karimi A, Rafiee TS, et al. Gastrointestinal basidiobolomycosis as a rare etiology of bowel obstruction. Turk J Med Sci 2006;2013:239–24 [Google Scholar]