Abstract
We present a case of a 53-year-old woman with abdominal discomfort for 6 months. The liver was enlarged. Contrast CT scan of the abdomen revealed a 10 cm hypervascular tumour at the right lobe of the liver. Right hepatectomy with complete excision of the tumour was achieved. Histological and immunohistochemical findings were consistent with perivascular epithelioid cell tumour. She is regularly followed up with contrast CT assessment. There is no tumour recurrence 12 months after the operation.
Background
Primary perivascular epithelioid cell tumour (PEComa) of the liver is a very rare condition that only a few reports are present in the current literatures. It belongs to the family of mesenchymal tumours consisting of perivascular epithelioid cells. Histologically, perivascular epithelioid cells demonstrate a clear or granular cytoplasm and central round nucleus without prominent nucleoli. The presentation of the disease can present from a benign condition such as angiomyolipoma to ones that are malignant like PEComa.
We report the clinical presentation, diagnostic approach and treatment of this patient. This case highlights the diagnostic challenge and follow-up management of this disease.
Case presentation
A 53-year-old woman presented with severe dull abdominal pain in the right upper quadrant for 6 months. She was a hepatitis B virus carrier. She did not consume alcohol and there was no history of trauma. On physical examination, there was no jaundice and pallor. There was no obvious abdominal mass or tenderness detected in her abdomen.
Investigations
Initial blood test showed that the haemoglobin level was 12 g/dL, the white cell count was 5×109/L, the platelet count was 231×109/L, the bilirubin level was 24 μmol/L and the α fetoprotein level was 4 ng/mL. A contrast CT of the abdomen was performed (figure 1A,B) revealing a 10 cm hypervascular tumour at the right lobe of the liver. The tumour showed a washout pattern in the delayed portal venous phase. In view of the tumour with a severe symptom, right hepatectomy was performed. The histopathology (figure 2) showed sheets of epithelioid and spindle-shaped cells of moderate cellularity. The spindle-shaped cells displayed a perivascular arrangement surrounding convoluted thick-walled blood vessels. Immunohistochemical stain (figure 3) of the tumour showed positivity for human melanoma black 45 (HMN45) and Melan-A. The tumour cells were negative for hepatocytic markers HEP-PAR-1, ALK1, CD21, Desmin and CD 31.
Figure 1.
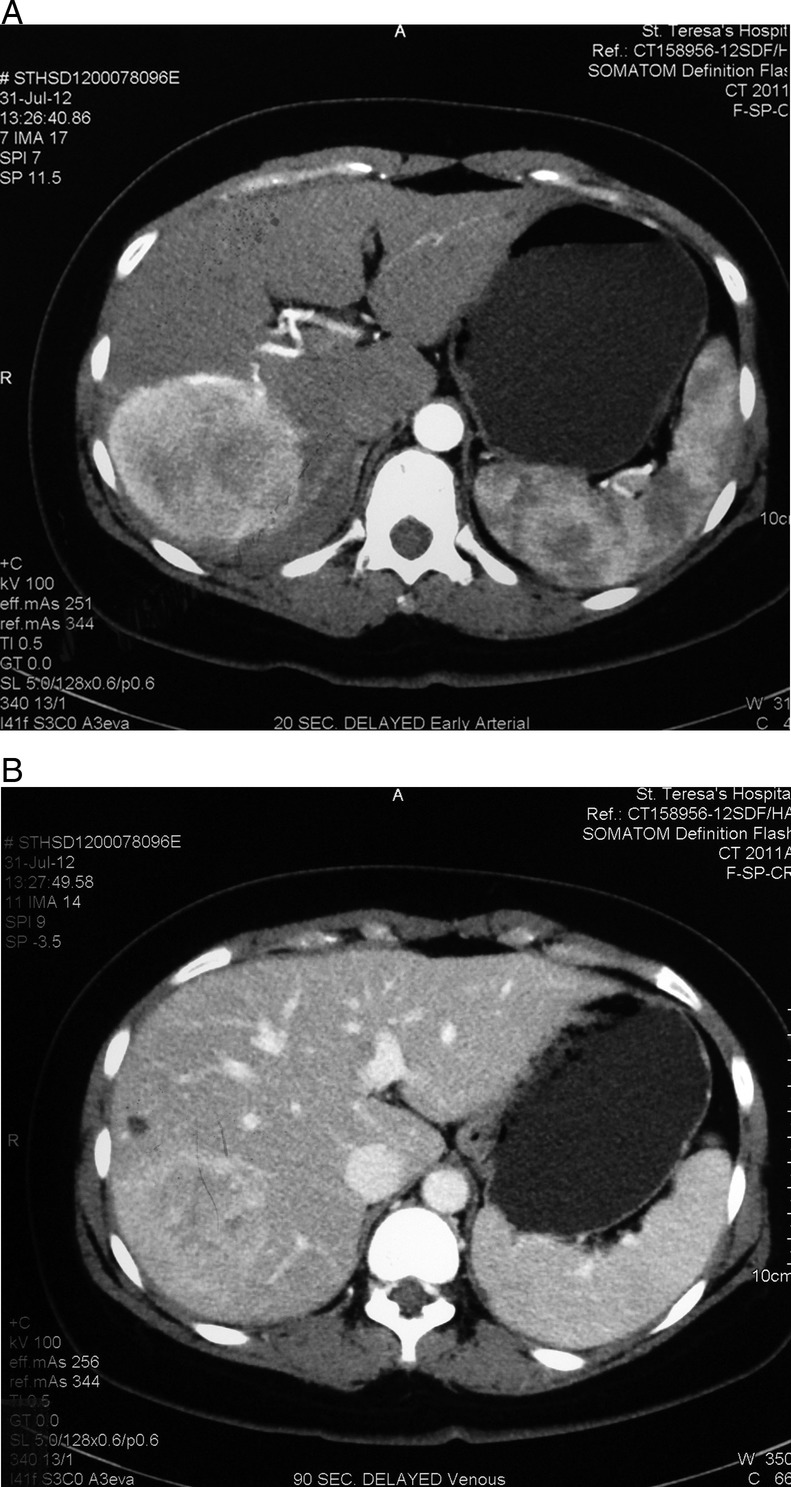
(A) Contrast CT scan showing a large tumour at the right lobe of the liver with arterial enhancement at postcontrast image. (B) Contrast CT scan showing vague contrast enhancement of tumour with ‘washout’ pattern at 90 s postcontrast image.
Figure 2.
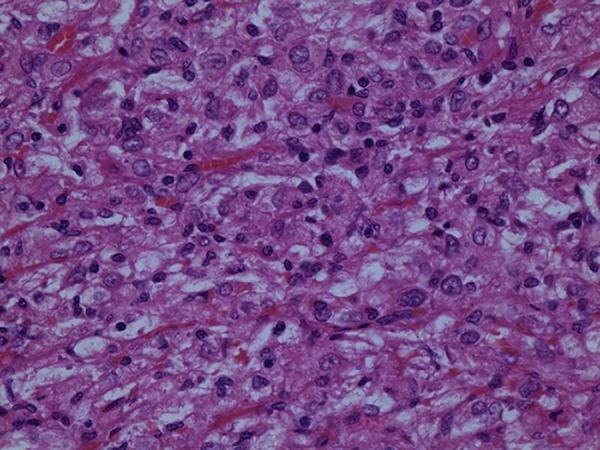
Histopathology showed sheets of epithelioid and spindle-shaped cells of moderate cellularity. The spindle-shaped cells displayed a perivascular arrangement surrounding convoluted thick-walled blood vessels.
Figure 3.
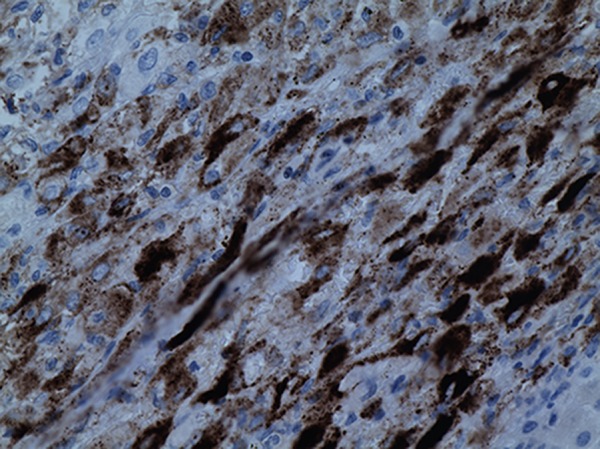
Immunohistochemical stain of the tumour showed positivity for human melanoma black 45 (HMN45) and Melan-A.
Differential diagnosis
Radiological diagnosis can be challenging because there can be quantitative variation of adipose tissue, irregular vessels and smooth muscle cells. The differential diagnosis for PEComa with hypervascular presentation included vascular tumour-like hepatocellular carcinoma and haemangioma. For PEComa with more adipose cell, the differential diagnoses include angiomyolipoma and liposacroma. In this case, it was only after resection, the current diagnosis of PEComa could be made by immunohistochemical staining.
Treatment
Laparotomy was performed using right subcostal incision with sternal extension. Intraoperative ultrasonography showed a vascular tumour at the right lobe of the liver. No additional lesion was detected. Right hepatectomy was performed. The specimen showed more than 2 cm margin from the vascular tumour (figure 4). No adjuvant treatment was given to this patient.
Figure 4.

Specimen revealed a large tumour with a wide margin from the liver transection surface.
Outcome and follow-up
The patient had a good recovery. The blood loss was 300 cm3 during the operation. Her liver function returned to normal 5 days after the surgery. She resumed a normal diet on day 3 and was discharged home 5 days after the hepatectomy. Although the pathology was in favour of a benign potential of the PEComa, patients was followed up at 3 month intervals by a contrast CT scan of the abdomen.
Discussion
Perivascular epithelioid cell neoplasms formed a rare group of mesenchymal tumour probably arising from the perivascular epithelioid cells throughout the body.1 This diagnosis has a relatively short history. The concept of perivascular epithelioid cells and its tumour classification was established in 2003 by the WHO.2 PEComa consisted of a range of lesion including angiomyolipoma, lymphangiomyomatosis, clear cell ‘sugar’ tumour of the lung and other lesions comprising perivascular epithelioid cells in soft tissues.3 4 The urology system and the uterus are the more common sites of this condition.5 6 The incidence is higher in woman at the age of their 50s. PEComa is a disease that is associated with the tuberous sclerosis complex but can occur in normal individuals.7
The patient is usually asymptomatic until the lesion grows in size and cause localised pressure effect or stretching of the liver capsule. The lesion itself in not hormonal secreting and there is no serological markers for identification of this tumour. Contrast CT scan is the most common imaging modalities that detect this abnormality. For lesion with strong vascular component like this case, there will be vascular enhancement in the arterial phase and the lesion remained enhanced even in the delayed phase of the CT scan.
Clinically, it is difficult to differentiate a benign tumour from a malignant variant. However, it is suggested that, histological evaluation as well as size might provide valuable prognostic information. Tumour with a size larger than 5 cm, mitotic count of more than 1 in the ×50 high power fields and the presence of tumour cell coagulative necrosis are poor prognostic predictors for malignant PEComa.8 9
Resection of the lesion relieved the symptom of this patient and provided full histological evaluation as variant carrying malignant potential could occur. Even though there is no malignant feature in our current case, diligent follow-up with regular contrast CT scan should be carried out as the course of this disease is still largely unknown. Metastases are still possible despite there is no malignant features in the primary resected lesion. In case of metastasis, there has not been a consensus on the treatment modalities although surgery, radiotherapy, chemotherapy and targeted therapy have been suggested.10–13 There have been only 10 cases of PEComa of liver reported so far. Since this is a rare disease entity, documentation of the tumours presentation, investigation method, treatment modality, follow-up protocol and recurrence pattern is important to understand the nature history of this disease.
Learning points.
Perivascular epithelioid cell neoplasms formed a rare group of mesenchymal tumour arising from the perivascular epithelioid cells throughout the body.
Contrast CT scan usually showed a vascular tumour at the arterial and portal venous phases which may mimic hepatocellular carcinoma and haemangioma.
Long-term follow-up is necessary even in patients where malignant features are absent as the natural history of this disease is not well documented.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hornick JL, Fletcher CD. PEComa: what do we know so far? Histopathology 2006;2013:75–82 [DOI] [PubMed] [Google Scholar]
- 2.Folpe AL, Kwiatkowski DJ. Perivascular epithelioid cell neoplasms: pathology and pathogenesis. Hum Pathol 2010;2013:1–15 [DOI] [PubMed] [Google Scholar]
- 3.Bonetti F, Pea M, Martignoni G, et al. Clear cell (‘sugar’) tumor of the lung is a lesion strictly related to angiomyolipoma—the concept of a family of lesions characterized by the presence of the perivascular epithelioid cells (PEC). Pathology 1994;2013:230–6 [DOI] [PubMed] [Google Scholar]
- 4.Martignoni G, Pea M, Reghellin D, et al. PEComas: the past, the present and the future. Virchows Arch 2008;2013:119–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martignoni G, Pea M, Reghellin D, et al. Perivascular epithelioid cell tumor (PEComa) in the genitourinary tract. Adv Anat Pathol 2007;2013:36–41 [DOI] [PubMed] [Google Scholar]
- 6.Sukov WR, Cheville JC, Amin MB, et al. Perivascular epithelioid cell tumor (PEComa) of the urinary bladder: report of 3 cases and review of the literature. Am J Surg Pathol 2009;2013:304–8 [DOI] [PubMed] [Google Scholar]
- 7.Zeng JP, Dong JH, Zhang WZ, et al. Hepatic angiomyolipoma: a clinical experience in diagnosis and treatment. Dig Dis Sci 2010;2013:3235–40 [DOI] [PubMed] [Google Scholar]
- 8.Folpe AL, Mentzel T, Lehr HA, et al. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol 2005;2013:1558–75 [DOI] [PubMed] [Google Scholar]
- 9.Selvaggi F, Risio D, Claudi R, et al. Malignant PEComa: a case report with emphasis on clinical and morphological criteria. BMC Surg 2011;2013:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeon IS, Lee SM. Multimodal treatment using surgery, radiotherapy, and chemotherapy in a patient with a perivascular epithelioid cell tumor of the uterus. J Pediatr Hematol Oncol 2005;2013:681–4 [DOI] [PubMed] [Google Scholar]
- 11.Parfitt JR, Bella AJ, Wehrli BM, et al. Primary PEComa of the bladder treated with primary excision and adjuvant interferon-alpha immunotherapy: a case report. BMC Urol 2006;2013:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parfitt JR, Bella AJ, Izawa JI, et al. Malignant neoplasm of perivascular epithelioid cells of the liver. Arch Pathol Lab Med 2006;2013:1219–22 [DOI] [PubMed] [Google Scholar]
- 13.Zekry N, Rettenmaier MA, Abaid LN, et al. Perivascular epithelioid cell neoplasms: a systematic review of prognostic factors. J Minim Invasive Gynecol 2009;2013:527–32 [DOI] [PubMed] [Google Scholar]


