Abstract
In cases of coronary artery spasm, life-threatening ventricular arrhythmias are possible and can lead to sudden cardiac death. Treatment for this condition includes implantable cardioverter defibrillators, but their effectiveness in patients who present with ventricular fibrillation is debated. Our patient presented with intractable ventricular fibrillation episodes that triggered shocks from her implanted defibrillator. At 2 years of follow-up, we placed her on 200 mg/day of oral amiodarone, after identifying short-coupled premature contractions as the trigger for the ventricular fibrillation. In the 2 years following initiation of this drug therapy, the patient had no further fibrillation episodes.
Background
Coronary artery spasm often causes life-threatening ventricular arrhythmias and sudden cardiac death.1 While implantable cardioverter defibrillators (ICD) have improved mortality in high-risk patients with coronary artery spasm,1–4 the efficacy of ICD in patients with ventricular fibrillation (VF) related to coronary artery spasm is still controversial.2 3 Here, we present the case of a patient with coronary artery spasm, who had multiple episodes of appropriate ICD shocks despite sufficient medical treatment. Ultimately, pharmaceutical therapy appeared to eliminate her episodes of VF.
Case presentation
A 53-year-old woman with a history of hypertension and cerebral bleeding 5 years previously experienced a sudden episode of VF. An emergency medical team was activated, and the VF was successfully defibrillated with an automatic external defibrillator. The patient was taken to a cardiac care unit by the emergency medical team. She had experienced no anginal symptoms prior to the VF. The patient was obese, but had no history of diabetes.
Investigations
The 12-lead ECG on admission to the cardiac care unit was normal (figure 1), and an echocardiogram showed no wall motion abnormalities (figure 2). The major results of blood testing are shown in table 1. Postcardiac arrest blood tests revealed an increased serum transaminase, lactate dehydrogenase, creatine phosphokinase and white cell count. A troponin T test was negative. Four days following her admission, VF recurred following prominent ST segment elevation on the ECG. In this episode, as well, the patient did not report any anginal symptoms (figure 3). The VF was immediately defibrillated with an external defibrillator, and the ST segment elevation normalised after successful defibrillation. An echocardiogram also demonstrated normal wall motion, and blood tests showed no abnormality at that time. A coronary angiography was performed, which appeared normal; however, an acetylcholine provocation test induced multivessel coronary artery spasms (figure 4). A signal-averaged ECG was negative (figure 5). As a result of these findings, transient myocardial ischaemia owing to coronary artery spasm was considered to be the cause of the VF.
Figure 1.
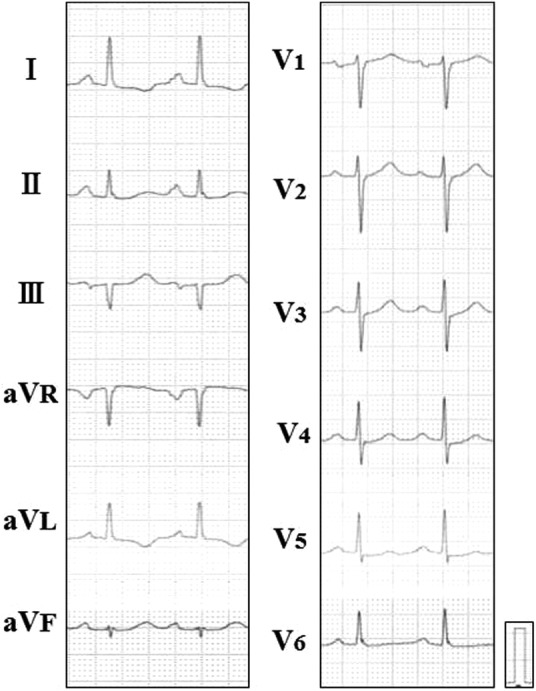
The 12-lead ECG results on admission. The ECG did not indicate ischaemic changes, pre-excitation or repolarisation abnormalities such as short or long QT, J wave or Brugada syndrome.
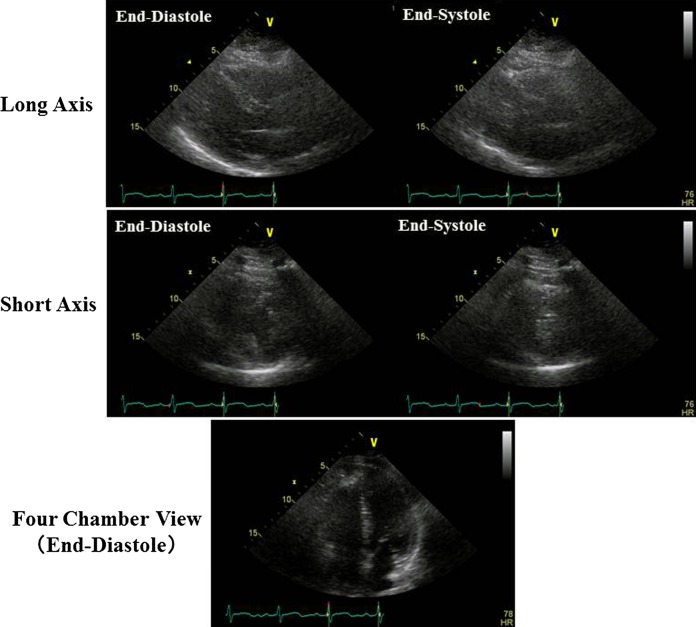
Figure 2.
Echocardiogram at admission, indicating completely normal heart function. Wall thickness of the ventricular septum and left ventricular posterior wall were 11.4 and 11.0 mm, respectively. Left ventricular end-diastolic and systolic diameters were 36.3 and 24.6, respectively. Left ventricular ejection fraction was calculated as 0.69. No dilation of the left and right atria, right ventricle or inferior vena cava was noted.
Table 1.
The major data of blood tests on the admission due to the first episode of ventricular fibrillation
| WBC | 11 400/μL | AST | 163 IU/L |
| Hb | 14.4 g/dL | ALT | 149 U/L |
| Ht | 42.3% | LDH | 479 U/L |
| Platelet | 25.1×104/μL | CPK | 251 IU/L |
| Total bilirubin | 0.7 mg/dL | ||
| Total-cholesterol | 210 mg/dL | BUN | 10.7 mg/dL |
| LDL-cholesterol | 65 mg/mL | Creatine | 0.4 mg/dL |
| HDL-cholesterol | 126 mg/dL | Na | 138 mEq/L |
| Triglyceride | 69 mg/dL | K | 4.0 mEq/L |
| HbA1c | 4.7% | Cl | 104 mEq/L |
| BNP | 4 pg/mL | Troponin T test | (–) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; CPK, creatine phosphokinase; Hb, haemoglobin; HbA1c, glycated haemoglobin; HDL, high density lipoprotein; Ht, haematocrit; LDH, lactate dehydrogenase; LDL, low density lipoprotein; WBC, white blood cell.
Figure 3.
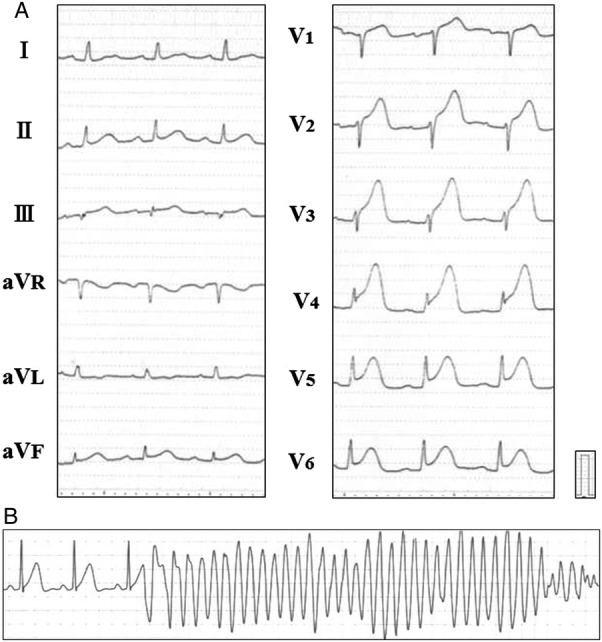
ST segment elevation suddenly manifested on the fourth day in the hospital (A), followed by ventricular fibrillation (B) and without any symptoms from the patient.
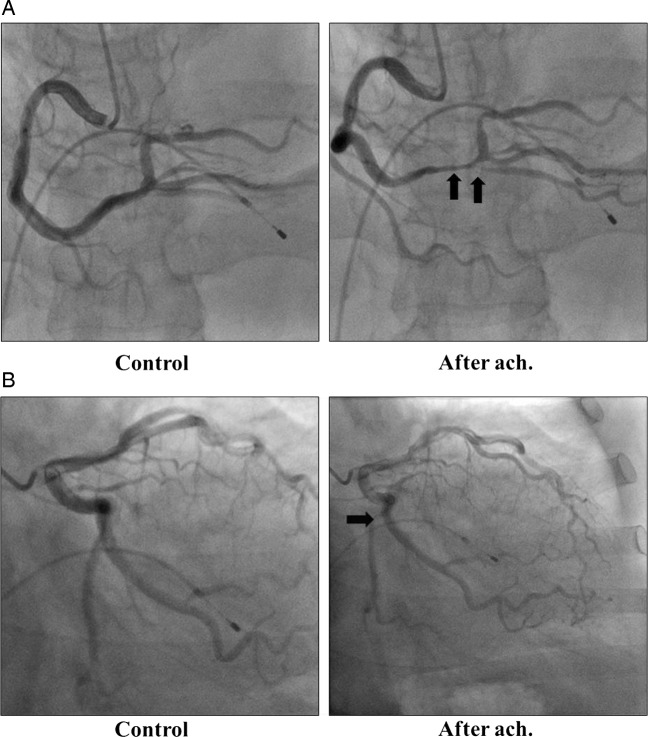
Figure 4.
Right coronary angiography (A) and left coronary angiography showed normal coronary appearance in control conditions (left panels). Injections of acetylcholine (ach.) at a dose of 50 μg induced multi-vessel coronary artery spasm (indicated by arrows), as shown in the right panels.
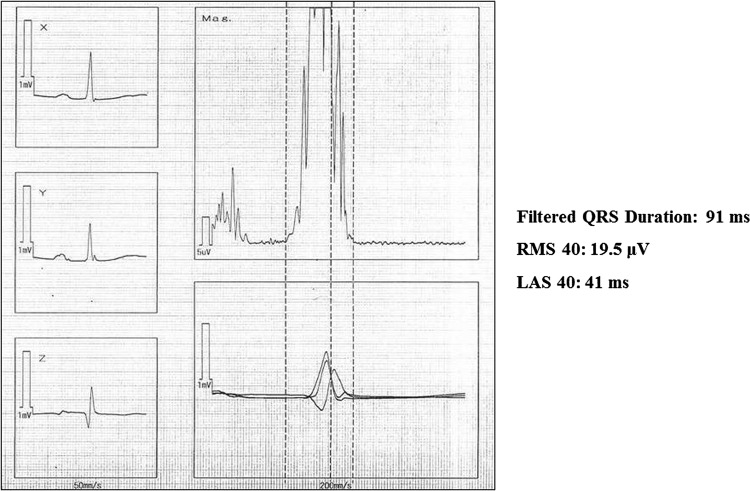
Figure 5.
Negative results of a signal-averaged ECG study.
Differential diagnosis
Coronary artery disease, cardiomyopathies, channelopathies such as short or long QT syndrome, J wave syndrome, Brugada syndrome and electrolyte abnormalities should be considered as a cause of VF. After admission, we ruled out acute coronary syndrome, other acute cardiovascular events and electrolyte abnormalities leading to VF. Based on the angiography, ECG, echocardiogram and provocation test findings, cardiomyopathies and channelopathies were unlikely, whereas coronary artery spasm was the most possible cause leading to VF in the present case.
Treatment
Following testing, the patient was placed on oral diltiazem at a dose of 240 mg/day, isosorbide mononitrate at a dose of 40 mg/day and nicorandil at a dose of 15 mg/day to prevent coronary artery spasm leading to VF. In addition, because the patient agreed to an ICD implantation, we implanted a single-chamber ICD (Current VR; St Jude Medical, Sylmar, California, USA), considering the patient's history.
Outcome and follow-up
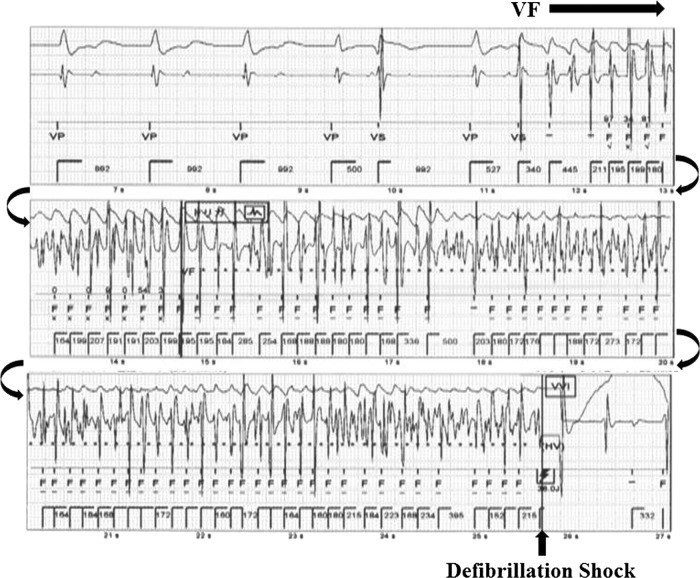
The patient did well for 2 years following implantation, but then visited our emergency room again, reporting about transient loss of consciousness. The routine examinations including ECG, echocardiogram and blood tests did not show any abnormality. ICD telemetry revealed one episode of shock therapy due to VF (figure 6). ST segment change was not apparent on the telemetry data. The patient reported having never forgotten to take medications and had not experienced chest pain prior to the loss of consciousness. Although we increased the dose of nitrates up to 80 mg/day, the patient received another appropriate ICD shock 3 months later. Eventually, oral amiodarone at a dose of 200 mg/day was started, as the VF was always triggered by short-coupled premature ventricular contractions. During the subsequent follow-up periods over the course of 2 years, no ventricular arrhythmia episodes were documented following initiation of amiodarone.
Figure 6.
Implantable cardioverter defibrillators telemetry at the time of an episode of shock therapy because of ventricular fibrillation. ST segment change was not detected on the telemetry data. A similar episode occurred 3 months later. VF: ventricularfibrillation.
Discussion
Coronary artery spasm, especially multivessel spasm, causes life-threatening ventricular arrhythmias leading to sudden cardiac death. Takagi et al4 reported that coronary artery spasms were documented in 6% of patients resuscitated from cardiac arrest, and cardiac arrest occurred in 2.4% patients with coronary artery spasms. They emphasised that the patients with coronary artery spasm and episodes of cardiac arrest were a high-risk group for future adverse cardiac events including sudden cardiac death.4 In patients with severe coronary artery spasms, ventricular arrhythmias are caused by prolonged myocardial ischaemia, which induces abnormal transmural dispersion of refractoriness. An ICD is not a fundamental treatment for such patients; therefore, aggressive medical therapy is still required. Although the efficacy of secondary preventive ICD implantation on mortality in high-risk patients with coronary artery spasm is still controversial,2 3 ICDs have saved numbers of patients from potential sudden cardiac death.4
The present case was a patient who was successfully resuscitated from sudden-onset VF. Of interest, her ECG at rest was normal, and the echocardiograms showed no structural heart disease. Signal-averaged ECG was also negative. Only a transient ST segment elevation on ECG just before the subsequent episodes of VF was observed. Coronary angiography revealed provocative multivessel coronary artery spasm, following intracoronary injection of acetylcholine in this patient. Throughout the examinations, acute coronary syndrome, idiopathic cardiomyopathies, short or long QT syndrome, J wave and Brugada syndrome and electrolyte abnormalities were not plausible as causes of VF. As in previous studies, the diagnostic accuracy of coronary artery spasm by intracoronary injection of acetylcholine was very high.5 The sensitivity and specificity have been estimated at 90% and 99%, respectively5; therefore, we considered in this case that the VF was led by silent myocardial ischaemia owing to coronary spasm.
Despite sufficient medical therapy for preventing coronary artery spasm, VF recurred. Thus, the co-existence of “idiopathic” VF with coronary artery spasm should also be ruled out.6 7 Nishizaki et al6 demonstrated abnormal ventricular repolarisation in patients with coronary artery spasm. Signal-averaged ECG did not indicate the existence of substrate for ventricular arrhythmias in the present case; however, we considered that the recurrent coronary artery spasm may have created tiny potential arrhythmic substrates leading to VF. This inference might be supported by the fact that amiodarone was effective in preventing further occurrence of VF.
In actual clinical practice, it is quite difficult to confirm whether induced coronary artery spasm represents a bystander finding or not. Nevertheless, this patient was able to avoid a fatal episode with an ICD implantation. Hybrid therapy with coronary dilators, an ICD and additional antiarrhythmic drugs are considered to be ideal in drug-refractory patients with coronary artery spasms.
Learning points.
Coronary artery spasm is an important cause of ventricular fibrillation (VF) and sudden cardiac death.
VF may occur without prior angina.
Medication doses that are considered to be sufficient may not always prevent coronary artery spasm leading to VF.
Coronary artery spasm can be associated with idiopathic VF.
The efficacy of implantable cardioverter defibrillators (ICD) is controversial, but a number of patient's lives have been saved by an ICD as in present case.
A combination therapy with coronary dilators, an ICD and antiarrhythmic
drugs may be needed in such patients.
Footnotes
Contributors: The efficacy of ICD in patients with coronary artery spasm and VF is still controversial. The present case provides further information about this controversy. A combination therapy with coronary dilators, an ICD and antiarrhythmic drugs may be ideal.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Myerburg RJ, Kessler KM, Mallon SM, et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med 1992;2013:1451–5 [DOI] [PubMed] [Google Scholar]
- 2.Chevalier P, Dacosta A, Defaye P, et al. Arrhythmic cardiac arrest due to isolated coronary artery spasm: long-term outcome of seven resuscitated patients. Am Coll Cardiol 1998;2013:57–61 [DOI] [PubMed] [Google Scholar]
- 3.Meisel SR, Mazur A, Chetboun I, et al. Usefulness of implantable cardioverter-defibrillators in refractory variant angina pectoris complicated by ventricular fibrillation in patients with angiographically normal coronary arteries. Am J Cardiol 2002;2013:1114–16 [DOI] [PubMed] [Google Scholar]
- 4.Takagi Y, Yasuda S, Tsunoda R, et al. Clinical characteristics and long-term prognosis of vasospastic angina patients who survived out-of-hospital cardiac arrest: multicenter registry study of the Japanese Coronary Spasm Association. Circ Arrhythm Electrophysiol 2011;2013:295–302 [DOI] [PubMed] [Google Scholar]
- 5.Okamura K, Yasue H, Matsuyama K, et al. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol 1988;2013:883–8 [DOI] [PubMed] [Google Scholar]
- 6.Takagi Y, Yasuda S, Tsunoda R, et al. Importance of dual induction tests for coronary vasospasm and ventricular fibrillation in patients surviving from out-of-hospital cardiac arrest. Circ J 2009;2013:767–9 [DOI] [PubMed] [Google Scholar]
- 7.Nishizaki M, Arita M, Sakurada H, et al. Induction polymorphic ventricular tachycardia by programmed ventricular stimulation in vasospastic angina pectoris. Am J Cardiol 1996;2013:355–60 [DOI] [PubMed] [Google Scholar]