Abstract
Presented in this paper is a case of a young Filipino man presenting with recurrent acute gouty flares leading to chronic tophaceous gout and unusual cutaneous manifestations (miliary gout, panniculitis, ulcerations). Unusual sites within the body (torso, shoulder, forearms, thigh) revealed multiple urate dermal deposition. Self-medication with steroids eventually led to secondary Cushing's syndrome and eventual emergence of metabolic complications.
Background
Gout is a systemic disorder characterised by recurrent arthritis and hyperuriacemia with urate deposition in synovial and non-articular tissues.1 The common cutaneous manifestations of gout are intradermal or subcutaneous nodules called tophi. They occur in avascular tissue over the ears, olecranon and prepatellar bursae, or in acral sites, often associated with tendons. They may discharge a chalky material that reveals negatively birefringent needle-shaped crystals.2 Aside from the usual tophi formation within joint spaces, more atypical dermatological manifestations in the form of pustules, ulcerations and panniculitis may occur in patients with gout.3
The objective of this paper is to present the unusual cutaneous manifestations in a young male patient with chronic gout. This paper will also try to highlight the unusual deposition sites of urate crystals not commonly seen in patients with chronic tophaceous gout.
Case presentation
This is a case of 35-year-old Filipino man presenting with a 15 year history of gouty arthritis, tophi formation in the joints and skin. The patient had no known comorbidities, had a good functional capacity and an unremarkable childhood and adolescence until the age of 20 when he started to note bilateral ankle and first metatarsophalangeal (MTP) swelling which were partially relieved with non-steroidal anti-inflammatory drugs (NSAIDs). He became asymptomatic over the next 4 years without any medications until its recurrence at the age of 24. The patient now experienced worsening polyarthritis affecting ambulation thus necessitating consult and eventual diagnosis of acute gouty arthritis.
There was recurrence of gouty attacks at the age of 27. The patient self-medicated with high-dose steroid (dexamethasone 8 mg/day) which provided complete resolution of symptoms. The patient took this as a daily maintenance medication until this consult.
At the age of 31, the patient started to note gradual eruption of multiple tophi over the finger joints leading to limitation of movement. He also noticed appearance of multiple yellow nodules along the arms, back, thigh, legs and neck (figure 1). He noted hyperpigmentation and inflammation of the lesions in the thigh. Through time, these skin lesions would ulcerate and exude chalk-like materials. The patient would self-medicate with antibiotics. Persistence of the skin lesions and recurrence of gouty attacks prompted another consult where patient was started on allopurinol and colchicine. He was later referred to our institution.
Figure 1.
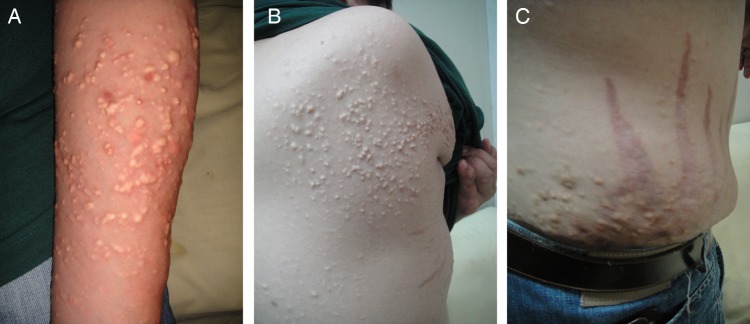
‘Miliary Gout’ multiple cutaneous tophi on forearm, shoulder, flank area.
The patient had a strong family history for gouty arthritis with his dad and uncle having been diagnosed with gout during their 50s. However, he was the only one who presented with peculiar skin lesions. He lives in the city, work as an employee with a sedentary lifestyle. He has no known vices.
Physical examination revealed presence of multiple golden subcutaneous non-tender, movable hard nodules measuring 1 cm in diameter along the forearms, shoulders and upper torso (figure 1). There were multiple hard irregular masses measuring 4–5 cm in diameter over hand and finger joints with deformity and limitation of motion (figure 2). Several hand joints were noted to be warm and tender. Multiple hyperpigmented ulcers with erythematous borders and eschar along the posterior thigh (figure 3). Podagra was appreciated (figure 4). Incidental findings of Cushing's features (moon facies, buffalo hump, supraclavicular fat pad, abdominal striae, truncal obesity, acne formation) were apparent from chronic steroid intake (figure 5). Patient had white opaque lenses. Other systemic and neurological PE findings were unremarkable.
Figure 2.

Classic chronic tophaceous gout resulting to hand joint deformities.
Figure 3.
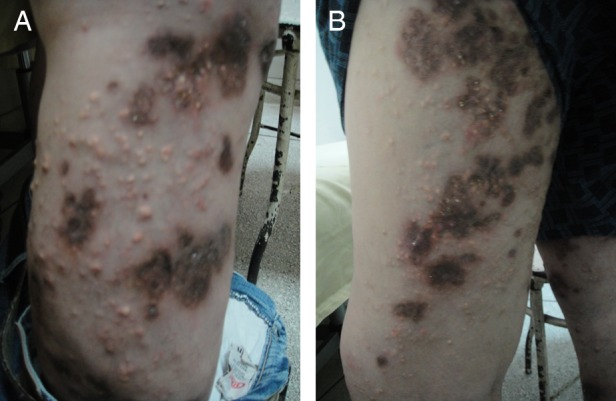
Multiple hyperpigmented ulcerations along the thigh and lower legs.
Figure 4.

Classic podagra with the left larger than the right.
Figure 5.

Abdominal striae and truncal obesity—secondary Cushing's features.
Investigations
Workups included blood tests revealing secondary diabetes mellitus (elevated fasting blood sugar of 180 mg/dL glycated haemoglobin 11.2%), severe hyperuricaemia (551.76 mg/L) and hypercholesterolaemia (206 mg/dL). Leg and hand radiographs revealed focal osteopenia, subcutaneous calcifications and joint deformities consistent with gouty arthritis (figure 6). Skin biopsy of the forearms, scapular and thigh areas revealed presence of urate crystals which were grossly golden in colour. The typical strongly negative birefringent needle-shaped cystals were then seen on polarised microscopy. These findings were all consistent with our diagnosis for chronic tophaceous deposition within subcutaneous skin tissue.
Figure 6.
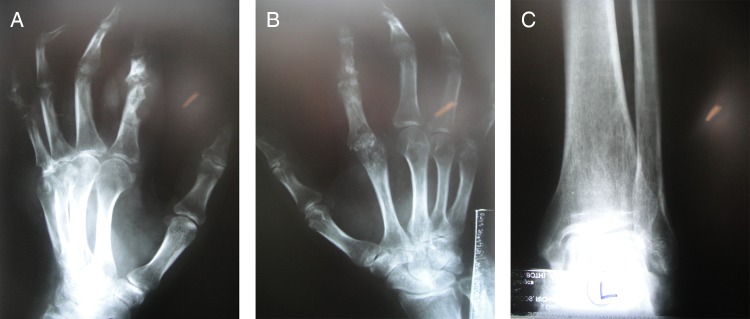
X-ray revealing focal osteopenia, subcutaneous calcifications and joint deformities.
Differential diagnosis
Gout as a disease usually presents in three clinical stages: acute gouty arthritis, intercritical period and chronic tophaceous gout. During the acute phase, patients usually present with mono-oligoarticular arthritis with the first MTP ‘Podagra’ as the pathognomonic symptom of gouty arthritis. Some of the common diseases that may present similarly with gouty arthritis include pseudogout, osteoarthritis, septic arthritis, rheumatoid arthritis and reactive arthritis. Aspiration of synovial fluid and examination under microscopy is the diagnostic of choice to ultimately diagnose gouty arthritis during the acute phase.4
However, as the disease progresses towards the chronic tophaceous phase, presentation and differentials may differ as the patient begins to have urate tissue deposition manifesting differently as the acute phase. Active arthritis may be absent and replaced with joint deformities instead. Cutaneous tophi described as yellow skin lesions can be mistaken as xanthomas, necrobiosis lipoidica in diabetes, pseudoxanthoma elasticum or sebaceous tumours.5 Skin biopsy and appearance of chalk-like material on open skin and joint surrounding is the gold standard for the diagnosis of gout in this phase.6
Our patient was seen during the chronic tophaceous state hence differentials were directed towards the identification of peculiar skin lesions rather than the joint abnormalities. The gross appearance of chalk-like material together with microscopic confirmation of urate crystals indeed documented the diagnosis of chronic tophaceous gout which is disseminated in character.
Treatment
Colchicine (1.5 mg/day) was given for gout control and prednisone (20 mg/day). Upon resolution of gouty flares, patient was then started on allopurinol (300 mg/day) as well as educated about his disease and advised compliance to treatment.
Outcome and follow-up
Patient was educated on his disease and advised compliance to treatment and diet that led to a complete resolution of the gouty attack. Steroid was slowly tapered and discontinued after 2 months. There was resolution of military cutaneous gouty lesions after 3 months of allopurinol treatment. He also had a cataract surgery and enrolled in an exercise and rehabilitation programme. He is currently on regular follow-up with management directed at aggressive lowering of hyperuricaemia and prevention of future tophi formation.
Discussion
Although our patient presented with a classic history and clinical course, there were striking peculiarities with regard to the chronic complications and physical findings. While most of the patients with chronic tophaceous gout present with tophi around the joint, synovium, olecranon, knee and tragus, our patient had multiple tophi deposits all over the skin which were discovered to be called ‘Miliary or Disseminated Cutaneous Gout’.7 8 Multiple ulcerations and panniculitis were also noted and described.9 These lesions eventually became infected and were misdiagnosed as common skin infection. Similar cases were presented by Ebner et al10 and Orzan et al.11
Gout may be diagnosed without further investigations in someone with hyperuricaemia and the classic podagra. Synovial fluid analysis may be done if the diagnosis is in doubt.6 X-rays, while useful for identifying chronic gout, have little utility in acute attacks.12 A definitive diagnosis of gout is based on the identification of MSU crystals in synovial fluid or a tophus characterised as strongly negative birefringent needle-shaped crystals. Hyperuricaemia is a classic feature of gout. Gout occurs, however, nearly half of the time without hyperuricaemia, and most people with raised uric acid levels never develop gout. Thus, the diagnostic utility of measuring uric acid level is limited.13
The initial aim of treatment is to settle the symptoms of an acute attack through different drugs which include NSAIDs, colchicine and steroids, while options for prevention include allopurinol, probenecid, rasburicase and febuxostat.14–16 Ice applied for 20–30 min several times a day decreases pain.17 The management of chronic gout is directed at lowering and maintaining serum uric acid at subsaturating levels, with a target level of <6.0 mg/dL.18 19 Long-term achievement of this goal has been proven to reduce incidence or disappearance of gouty flares and dissolution of tophaceous deposits.20–22 Without treatment, episodes of acute gout may develop into chronic gout with destruction of joint surfaces, joint deformity and painless tophi. These tophi occur in 30% of those who are untreated for 5 years. With aggressive treatment, they may dissolve.12 23
Chronic self-medication with steroids even complicated this case as metabolic complications appeared and Cushing's features were documented. Earlier diagnosis, drug compliance and patient education might have prevented the progression of a simple gouty attack to a more serious disseminated tophaceous deposits leading to joint deformities and skin disfigurement.
Learning points
Knowledge of atypical cutaneous manifestations (panniculitis, pustules and ulcerations) of gout may facilitate earlier diagnosis and prompt treatment leading to prevention of complications.
Aggressive reduction in serum uric acid can lead to gradual resolution of cutaneous tophi.
Side effects of medications especially steroids should always be put into consideration to prevent metabolic complications.
Footnotes
Contributors: TEL saw, examined and treated the reported patient. GR carried out revisions and changes with the manuscript. EP is the mentor and edited and approved the final version of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schumacher R, Chen L. ‘Gout and other Crystal-associated Arthropathies’ Harrisons’ Principles of internal medicine 17th edn. 2008:2165 [Google Scholar]
- 2.Miller AV. Gout. 2011 http://emedicine.medscape.com/article/329958-clinical. [Google Scholar]
- 3.Dahiya A, Leach J, Levy H. Gouty panniculitis in a healthy male. J Am Acad Dermatol 2007;2013(2 Suppl):S52–4 [DOI] [PubMed] [Google Scholar]
- 4.Chen LX, Schumacher HR. ‘Gout: an evidence-based review’. J Clin Rheumatol 2008;2013:S55–62 [DOI] [PubMed] [Google Scholar]
- 5.Bolognia J, Braverman I. Skin manifestations of internaldDisease. Harrisons’ principles of internal medicine. 17th edn. McGraw-Hill Professionals 2008:331 [Google Scholar]
- 6.Eggebeen AT. Gout: an update. Am Fam Physician 2007;2013:801–8 [PubMed] [Google Scholar]
- 7.Fallasca G. Metabolic diseases: gout. Dermatol Signs Intern Dis 2006;2013:498–508 [DOI] [PubMed] [Google Scholar]
- 8.Shukla R, Vender RB, Alhabeeb A, et al. Miliarial gout (a new entity). J Cutan Med Surg 2007;2013:31–4 [DOI] [PubMed] [Google Scholar]
- 9.Ochoa CD, Valderrama V, Mejia J, et al. Panniculitis: another clinical expression of gout. Rheumatol Int 2011;2013:831–5 [DOI] [PubMed] [Google Scholar]
- 10.Ebner H, Raab W. Chronic cutaneous gout. Hautarzt 1964;2013:429–32 [PubMed] [Google Scholar]
- 11.Orzan OA, Popescu I, Tudose I, et al. Severe disseminated cutaneous gout. Acta Endocrinol 2012;2013:131 [Google Scholar]
- 12.Richette P, Bardin T. Gout. Lancet 2010;2013:318–28 [DOI] [PubMed] [Google Scholar]
- 13.Schlesinger N. Diagnosing and treating gout: a review to aid primary care physicians. Postgrad Med 2010;2013:157–61 [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II: management. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheumatol Dis 2006;2013:1312–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaumacher HR, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, Randomized, Double-blind, Parallel-Group Trial. Arthritis Rheum 2008;2013:1540–8 [DOI] [PubMed] [Google Scholar]
- 16.Richette P, Briere C, Hoenen-Clavert V, et al. Rasburicase for tophaceous gout not treatable with allopurinol: an exploratory study. J in Rheumatol 2007;2013:2093–8 [PubMed] [Google Scholar]
- 17.Schlesinger N, Detry MA, Holland BK, et al. Local ice therapy during bouts of acute gouty arthritis. J Rheumatol 2002;2013:331–4 [PubMed] [Google Scholar]
- 18.Perez-Ruiz F, Liote F. Lowering serum uric acid levels: what is the optimal target for improving clinical outcomes in gout. Arthritis Rheumatol 2007;2013:1324–8 [DOI] [PubMed] [Google Scholar]
- 19.Li-Yu J, Clayburne G, Sieck M, et al. Treatment of chronic gout. Can we determine when urate stores are depleted enough to prevent attacks of gout?. J Rheumatol 2001;2013:577–80 [PubMed] [Google Scholar]
- 20.Perez-Ruiz F, Calabozo M, Pijoan JI, et al. Effect of Urate-lowering therapy on the velocity of size reduction of size reduction of tophi in chronic gout. Arthritis Rheumatol 2002;2013:356–60 [DOI] [PubMed] [Google Scholar]
- 21.Pillinger MH, Rosenthal P, Abeles AM. Hyperuricemia and gout: new insights into pathogenesis and treatment. Bull NYU Hosp Joint Dis 2007;2013:215–21 [PubMed] [Google Scholar]
- 22.Terkeltaub R. Update on gout: new therapeutic strategies and options. Nat Rev Rheumatol 2010;2013:30–8 [DOI] [PubMed] [Google Scholar]
- 23.Peterseim U, von Gizycki-Nienhaus B, Schattenkirchner M, et al. Gout tophi and Heberden nodules in hyperuricemia. Der Hautarzt 1994;2013:799–802 [DOI] [PubMed] [Google Scholar]


