Abstract
Pulmonary vein thrombosis is undiagnosed and thought to be rare. Stroke is a serious clinical problem and atrial fibrillation is associated with it. As a cardiac thrombus, a thrombus in the left atrial appendage and the left atrium are well known, but a pulmonary vein thrombus is not thought to be a common cause of stroke. A 69-year-old woman with transient ischaemic stroke had chest pain and was examined by 64-slice multidetector CT (64-MDCT). 64-MDCT illustrated no coronary artery stenosis but a thrombus in the left lower pulmonary vein (LLPV), which was in contact with the lower surface of the LLPV. The pulmonary vein cells in contact with the thrombus lack oxygen and nutrients, which may control physiological processes, such as development, differentiation and pathological responses in the pulmonary vein. These effects are unknown and more studies are desirable. 64-MDCT can demonstrate a thrombus in the pulmonary vein and hence a pulmonary vein thrombus is not rare.
Background
Stroke is a suddenly developing temporary or often a long persistent damage of the brain, and is the second leading cause of death and the leading cause of permanent disability worldwide.
The risk for stroke increases with age, hypertension, hyperlipidaemia, atherosclerosis, atrial fibrillation, a family history of stroke, and a previous stroke or a temporal ischaemic attack (TIA). However, not all strokes are alike. It is important to modify what causes stroke risk and to prevent stroke in healthcare. Primary and secondary stroke prevention strategies differ according to stroke subtype, for example, anticoagulation for cardioembolic strokes, platelet inhibition for large vessel disease, antihypertensive treatment and statins for most subtypes.
Cardiac thrombosis is important because we use anticoagulants to prevent stroke. As a cardiac thrombus, a thrombus in the left atrial appendage (LAA) and the left atrium are well known, and transoesophageal echocardiography (TEE) is usually performed to detect them. A 64-slice multidetector CT (64-MDCT) becomes an option to assess the coronary artery plaque. We reported that a 64-MDCT can illustrate LAA thrombi more easily and accurately than TEE.1
We report some cases of a thrombus in the pulmonary vein using 64-MDCT. In 2012, we reported two cases of the small pulmonary vein thrombus,2 3 and in 2013, we reported the large size thrombus4 and the completely occluded right and left upper pulmonary vein thrombosis.5 Presently, the number of cases reporting a thrombus in the pulmonary vein without thoracic surgery is few and diagnosis of a thrombus in the pulmonary vein is not yet well recognised. Illustrated images of a thrombus in the pulmonary vein, which show a thrombus in contact with the wall of the pulmonary vein, have not yet been reported. We report a new case of a pulmonary vein thrombus.
Case presentation
The patient was a 69-year-old woman with transient ischaemic stroke and had been treated with clopidogrel (75 mg once a day) for a few years. Serum D-dimer level was 1.0 μg/mL (normal; <1.0 μg/mL), the activity of protein S was 96% (normal; 60–150%), and the activity of protein C was 62% (normal; 64–146%). The patient was diagnosed with a first degree atrial–ventricle block. The patient was referred to our hospital for the evaluation of chest pain. The chest roentgenogram showed no lung cancer. The patient had no symptoms of cough, sputum or cerebral infarction. Although the patient had some small calcification of coronary artery and no stenosis in coronary artery, a thrombus in the left lower pulmonary vein (LLPV) was detected in axial (figure 1) and sagittal (figures 2–5) images on contrast enhancements by a 64-MDCT scan. The patient had no thrombus in the LAA. The MRI of the brain showed no cerebral infarction.
Figure 1.
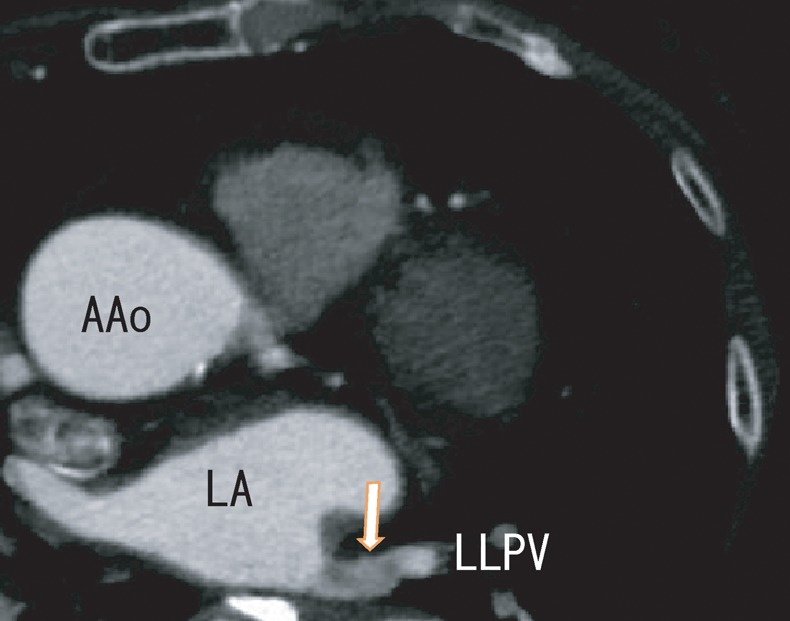
Axial images illustrated an LLPV thrombus as the defect of contrast enhancements (arrow). AAo, ascending aorta; LA, left atrium; LLPV, left lower pulmonary vein.
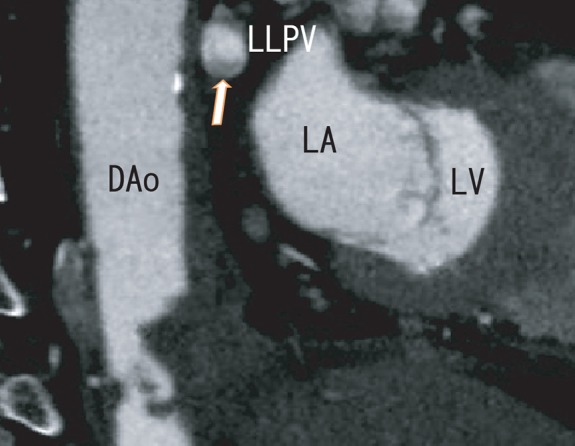
Figure 2.
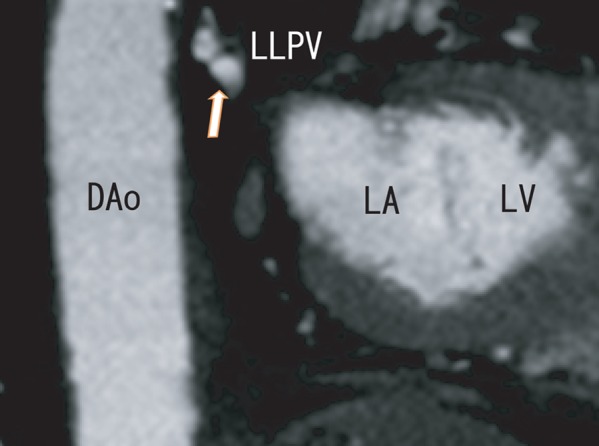
Sagittal images illustrated no clear defect of contrast enhancements in the LLPV (arrow). Dao, descending aorta; LA, left atrium; LLPV, left lower pulmonary vein; LV, left ventricle.
Figure 3.
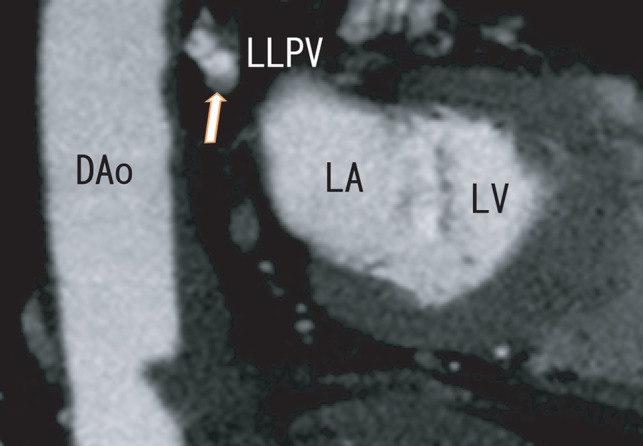
Sagittal images illustrated a small thrombus (5×3 mm) in the LLPV as the defect of contrast enhancements (arrow), which attached to the lower surface of the LLPV. Dao, descending aorta; LA, left atrium; LLPV, left lower pulmonary vein; LV, left ventricle.
Figure 4.
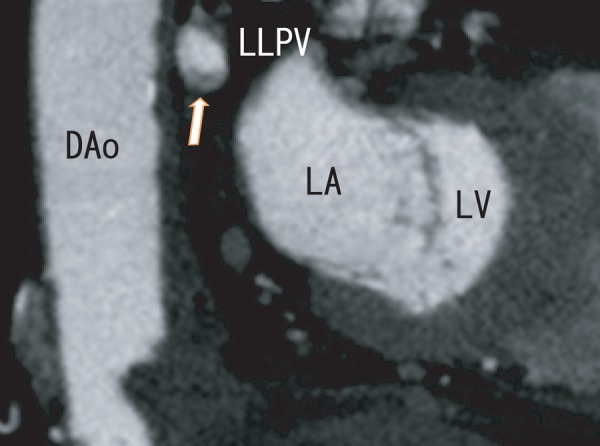
Sagittal images illustrated the same thrombus in the LLPV as the defect of contrast enhancements (arrow), which became larger (9×4 mm) and attached to the lower surface of the LLPV. Dao, descending aorta; LA, left atrium; LLPV, left lower pulmonary vein; LV, left ventricle.
Figure 5.
Sagittal images illustrated the same thrombus in the LLPV as the defect of contrast enhancements (arrow), which became again larger (10×5 mm) and attached to the lower surface of the LLPV. Dao, descending aorta; LA, left atrium; LLPV, left lower pulmonary vein; LV, left ventricle.
After the 3 months clopidogrel (75 mg once a day) and dabigatran (220 mg twice daily) therapy, the thrombus in the LLPV did not dissolve much (not shown here).
Treatment
Clopidogrel (75 mg once a day).
Discussion
In this manuscript, we showed a thrombus in the LLPV. The thrombus covered one thirds of the area of LLPV surface (figure 5), which was the first demonstration as far as we know. Although we reported the small size thrombus,2 3 the middle size thrombus4 and complete occlusion,5 the images in figures 3–5 are new. LAA thrombi are well known as a cause of ischaemic stroke. Not only a LAA thrombus but a pulmonary vein thrombus also causes ischaemic stroke. This patient had transient ischaemic stroke, which may be caused by a part of the detected LLPV thrombus. To prevent ischaemic stroke, it may be important for patients with TIA to examine pulmonary vein thrombi by 64-MDCT.
Blood stasis and hypercoagulability are two crucial predisposing factors for the development of venous thrombosis. Congenital deficiencies in antithrombin III, protein C or protein S and the antiphospholipid antibodies represent well-established risk factors. In this case, the activity of protein C (62%) was low (normal: 64–146%), which might be associated with the formation of the thrombus in the LLPV. The patient was 69 years old. In older population, the activity of the body is decreased, which generally decreases the amount of blood and the blood flow in the pulmonary vein . So, blood stasis may result in pulmonary vein thrombi.
In figures 3–5, the thrombus is in contact with the inferior wall of the LLPV. The tissue of pulmonary vein wall in contact with the thrombus lacks oxygen and nutrients, which may effect cell biology of pulmonary vein in contact and may control physiological processes such as development and differentiation and pathological responses of the pulmonary vein. The development of the pulmonary vein myocardium is associated with atrial fibrillation. Poor oxygen and poor nutrient may be associated with the development of the pulmonary vein myocardium. More studies are desired.
To prevent stroke, it may be important for patients with transient ischaemic stroke to examine pulmonary vein thrombi by 64-MDCT.
Learning points.
In this study, we showed the thrombus is in contact with the pulmonary vein wall. As far as we know, these images are the first to show the thrombus in contact with the pulmonary vein wall.
In this case, it is difficult to identify the thrombus in pulmonary vein by transoesophageal echocardiography because of pulmonary air, but it is easily seen by 64-slice multidetector CT (64-MDCT).
To prevent ischaemic stroke, it may be important for patients with transient ischaemic attack to examine the pulmonary vein thrombi by 64-MDCT, even if they do not have atrial fibrillation.
The poor oxygen and poor nutrient circumstances, because of pulmonary vein thrombi, have the possibility to be associated with the development of the pulmonary vein myocardium.
A pulmonary vein thrombus may be so strong and firm that it does not cause ischaemic stroke so easily. The trait of a pulmonary vein thrombus is unclear.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Takeuchi H. A 64-slice multi-detector CT scan could evaluate the change of the left atrial appendage thrombi of the atrial fibrillation patient, which was reduced by warfarin therapy. BMJ Case Rep. Published Online: 19 Aug 2011.10.1136/bcr.11.2009.2491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takeuchi H. A thrombus of the right upper pulmonary vein: detection by the use of a 64-MDCT. BMJ Case Rep. Published Online: 14 Sept 2012.10.1136/bcr.12.2011.5446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takeuchi H. 64-MDCT showed the thrombus in the pulmonary vein of the patient with angina pectoris. BMJ Case Rep. Published Online: 13 Oct 2012.10.1136/bcr.02.2012.5839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeuchi H. 64-MDCT can depict the thrombi expanded from the left lower pulmonary vein to the left atrium in the patient with angina pectoris. BMJ Case Rep. Published Online: 3 Apr 2013. doi: 10.1136/bcr.2013-008750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takeuchi H. 64-MDCT scan demonstrated pulmonary vein thrombus J Neurol Neurophysiol 2013;2013:002. [Google Scholar]


