Abstract
Black Americans are disproportionally infected with hepatitis C virus (HCV) and are less likely than whites to respond to treatment with peginterferon (PEG-IFN) plus ribavirin (RBV). The impact of race on HCV treatment eligibility is unknown. We therefore performed a retrospective analysis of a phase 3B multicenter clinical trial conducted at 118 United States community and academic medical centers to evaluate the rates of and reasons for HCV treatment ineligibility according to self-reported race. In all, 4,469 patients were screened, of whom 1,038 (23.2%) were treatment ineligible. Although blacks represented 19% of treated patients, they were more likely not to be treated due to ineligibility and/or failure to complete required evaluations (40.2%) than were nonblack patients (28.5%; P < 0.001). After the exclusion of persons not treated due to undetectable HCV RNA or nongenotype 1 infection, blacks were 65% less likely than nonblacks to be eligible for treatment (28.1% > 17.0%; relative risk, 1.65; 95% confidence interval, 1.46–1.87; P< 0.001). Blacks were more likely to be ineligible due to neutropenia (14% versus 3%, P < 0.001), anemia (7% versus 4%, P = 0.02), elevated glucose (8% versus 3%, P < 0.001), and elevated creatinine (5% versus 1%, P < 0.001).
Conclusion
Largely due to a higher prevalence of neutropenia and uncontrolled medical conditions, blacks were significantly less likely to be eligible for HCV treatment. Increased access to treatment may be facilitated by less conservative neutrophil requirements and more effective care for chronic diseases, namely, diabetes and renal insufficiency.
Chronic hepatitis C virus (HCV) infection is an important public health problem that affects ≈3.2 million persons in the United States.1,2 Although the majority of HCV-infected Americans are non-Hispanic whites, blacks are disproportionately infected; ≈3% of the black population is HCV-infected, compared with 1.5% of the non-Hispanic white population.1 Despite this significant disease burden, HCV treatment rates for blacks have been relatively low in clinical practice and research settings.3,4 For example, in the United States Veterans Affairs Health System, blacks are 36% less likely than whites to be prescribed treatment for hepatitis C.5,6
Although the reasons for low rates of treatment among HCV-infected blacks have not been fully elucidated, multiple factors likely contribute. Therapeutic nihilism may account for some of this disparity. Compared with whites, black Americans have a higher prevalence of poorly responsive virus, such as HCV genotype 1 infection and high HCV RNA levels, and a lower prevalence of certain host factors, such as the favorable interleukin (IL)-28B polymorphism, leading to substantially lower sustained virologic response (SVR) rates with peginterferon (PEG-IFN) and ribavirin (RBV).7–11 Limited access to medical care as a result of high treatment costs, inadequate health insurance, or perceived bias may also contribute to a low treatment rate among blacks.12 Further, there are numerous relative and absolute contraindications to the use of PEG-IFN and RBV, including cytopenias, unstable medical or psychiatric disease, and, in some settings, active illicit drug use.11 Although some of these contraindications, such as neutropenia, are known to have a greater prevalence among blacks, the impact of race on eligibility for HCV treatment is largely unknown.13,14
The Individualized Dosing Efficacy Versus Flat Dosing to Assess Optimal Pegylated Interferon Therapy (IDEAL) study population provides a unique opportunity to evaluate the impact of race on HCV treatment eligibility.15 First, by assessing more than 4,400 patients from 118 community and academic centers, the cohort provides broad representation of HCV disease in the U.S. Second, with the exception of the lower-dose PEG-IFN alfa-2b arm, the HCV treatments evaluated closely resemble the regimens approved by the U.S. Food and Drug Administration (FDA).16,17 Third, all medical evaluations and treatments were provided at no cost to patients, removing potential barriers to treatment based on the inability to afford care. Finally, the percentage of blacks treated in this study (≈19%) was representative of the HCV prevalence in the general population. Accordingly, the objective of the analysis was to determine the rate of HCV treatment eligibility according to race and, among those not eligible, to determine the reasons for HCV treatment ineligibility.
Materials and Methods
Design Overview
The IDEAL study has been described in detail elsewhere.15 Briefly, this was a phase 3B, randomized, parallel-group, U.S. multicenter study of PEG-IFN alfa-2b 1.5 µg/kg/wk or 1.0 µg/kg/wk or PEG-IFN alfa-2a combined with RBV for the treatment of chronic HCV infection. Persons 18–70 years of age were eligible if they had compensated liver disease due to HCV genotype 1 infection and were treatment-naive. The primary endpoint was SVR, defined as an undetectable HCV RNA 24 weeks after stopping therapy. The study was approved by each center’s Institutional Review Board and was conducted in accordance with provisions of the Declaration of Helsinki and Good Clinical Practice guidelines. Each patient provided informed consent for participation in the study.
Setting and Participants
Patients were enrolled from 118 academic (64.4%) and community (35.6%) centers in the U.S. and were required to meet eligibility criteria consistent with standard HCV treatment guidelines: white blood cell (WBC) count ≥3,000/mm3; absolute neutrophil count (ANC) ≥l,500/mm3; platelet count ≥80,000/mm3; hemoglobin (Hb) ≥12 g/dL for women and ≥13 g/dL for men; normal serum creatinine (SCr) and thyroid stimulating hormone; no known human immunodeficiency virus (HIV) or hepatitis B virus (HBV) infections; fasting glucose 70–140 mg/dL (and if 116–140 mg/dL or if diabetic, HbAlc ≤8.5%); absence of moderate and severe psychiatric disorders and/ or recent substance abuse as well as uncontrolled medical conditions such as obesity (weight >125 kg) and clinically significant heart disease.
Study Screening Protocol
Prior to HCV treatment, patients underwent two separate screening visits. The first screening visit evaluation included measurement of vital signs, height, and weight; collection of a medical history, medication use, and demographic data, including self-reported race (with options defined by the investigator as Caucasian, black, Hispanic, Asian, American Indian, or other); laboratory testing for complete blood count and nonfasting chemistry panel; antinuclear antibodies; serum pregnancy test; HCV RNA level by reverse-transcription polymerase chain reaction (RT-PCR); and HCV genotype. At the second visit, a physical examination, an assessment for depression by way of the Center for Epidemiologic Studies Depression (CES-D) Scale, and additional laboratory testing (including a fasting blood chemistry profile) were performed. Because of the two-step process, some clinical and laboratory data were available only for patients who reached the second screening visit. Liver biopsy performed within 3 years of treatment was required.
Statistical Analysis
Available data from patients who were discontinued from study participation prior to randomization were analyzed for differences in rates of and reasons for study ineligibility according to self-reported race. Categorical variables were summarized using proportions, and continuous variables were summarized using means, medians, and standard deviations. P values for comparison of blacks versus nonblacks are presented based on a χ2 test (for categorical variables) or t test (for continuous variables). Relative risk (RR) and 95% confidence interval (CI) were also computed to report the risk of HCV treatment ineligibility for black versus nonblack patients. All P values reported are nominal P values and have not been adjusted for multiple comparisons. All statistical analyses were done using SAS software.
Role of the Funding Source
This study was supported by grants from Schering-Plough Research Institute, now Merck Research Laboratories. The study sponsor collected and managed the data used in this work, and the study sponsor reviewed and approved the article. The study sponsor had no role in the design and conduct of the study, analysis, and interpretation of the data, or preparation of the article.
Results
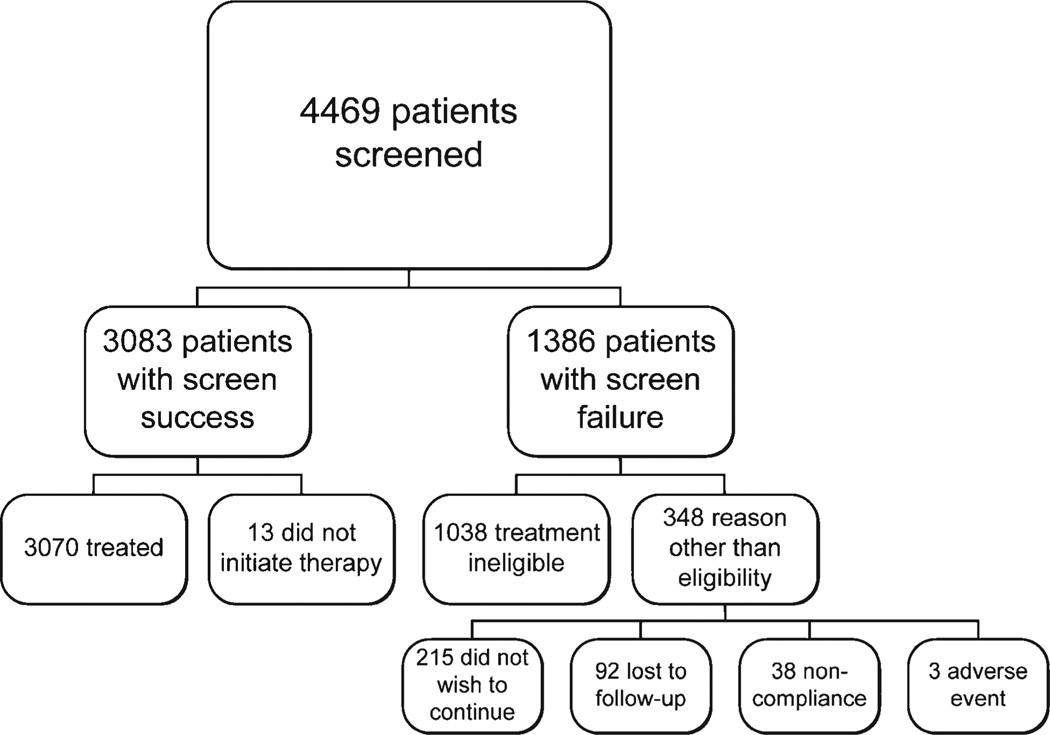
Overall, 4,469 patients (962 [21.5%] black and 3507 [78.5%] nonblack) were screened at community (1,670, 37.4%) and academic (2,799, 62.6%) centers (Fig. 1). Of those evaluated, 3,083 (69.0%) were eligible and randomized for treatment; 13 of these eligible patients were not treated. In all, 1,386 (31.0%) patients failed the screening process, including 502 at community sites (30.0% of screened patients) and 884 at academic sites (31.6% of screened patients). Demographic and clinical information for screened patients is summarized in Table 1. Compared with nonblacks, black patients were older, heavier, and were more likely to be infected with HCV genotype 1, subtype b (P < 0.001 for each). Of those patients who failed screening (n = 1,386), the majority (1,038, 74.9%) were found to be ineligible for HCV treatment in the study (Table 2). The most common reasons for treatment ineligibility included: preexisting or uncontrolled medical disease, 19.5% of patients who failed screening; undetectable or missing HCV-RNA or non-1 HCV genotype, 12.5%; preexisting, uncontrolled psychiatric disease including moderate-to-severe depression, 12.0%; abnormal hematology, 10.7%; abnormal blood chemistry, 10.0%; and/ or recent drug or alcohol abuse, 8.6%. For patients who failed screening for reasons other than ineligibility for treatment, the most common reason was patient preference not to continue (15.5% of patients who did not enter the treatment phase of the study).
Fig. 1.
Flow diagram of all 4,469 patients evaluated for hepatitis C treatment in the IDEAL study.
Table 1.
Demographic and Clinical Characteristics of Patients Screened for HCV Treatment
| Total Screened |
Screen Failures |
Screen Successes |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Black (n = 962J |
Nonblack (n = 3507) |
P* | Black (n = 387) |
Nonblack (n = 999) |
P* | Black (n = 575) |
Nonblack (n = 2508) |
P* | |
| Male sex, n (%) | 527 (55) | 2155 (61) | <0.001 | 218 (56) | 625 (63) | 0.10 | 309 (54) | 1530 (61) | 0.001 |
| Race, n (%) | |||||||||
| White | 0 | 3034 (87) | 0 | 838 (84) | 0 | 2196 (88) | |||
| Black | 962 (100) | 0 | 387 (100) | 0 | 575 (100) | 0 | |||
| Hispanic | 0 | 332 (9) | 0 | 118 (12) | 0 | 214 (9) | |||
| Other | 0 | 141 (4) | 0 | 43 (4) | 0 | 98 (4) | |||
| Age, mean (SD), y | 49.9 (6.9) | 47.1 (8.1) | <0.001 | 50.0 (6.9) | 47.2 (8.0) | <0.001 | 49.8 (7.0) | 47.0 (8.2) | <0.001 |
| Weight, mean (SD), kg | 87.6 (16.0) | 82.8 (17.2) | <0.001 | 88.5 (17.9) | 83.5 (18.7) | <0.001 | 87.1 (14.6) | 82.5 (16.5) | <0.001 |
| HCV risk factor, n (%) | |||||||||
| Injection drug use | 565 (59) | 2351 (67) | <0.001 | 200 (52) | 631 (63) | <0.001 | 365 (63) | 1720 (69) | 0.02 |
| Transfusion-associated | 195 (20) | 652 (19) | .24 | 80 (21) | 154 (15) | .01 | 115 (20) | 498 (20) | 0.94 |
| Other or missing | 202 (21) | 504 (14) | <0.001 | 107 (28) | 214 (21) | .007 | 95 (17) | 290 (12) | 0.001 |
| ALT > ULN, n (%) | 539 (56) | 1734 (49) | <0.001 | 268 (69) | 759 (76) | .05 | 271 (47) | 975 (39) | <0.001 |
| HCV genotype 1 subtype, n (%) | |||||||||
| 1a | 550 (57) | 2090 (60) | .18 | 211 (55) | 506 (51) | .09 | 339 (59) | 1584 (63) | 0.06 |
| 1b | 369 (38) | 1131 (32) | <0.001 | 139 (36) | 267 (27) | <0.001 | 230 (40) | 864 (34) | 0.01 |
| 1a/lb | 11 (1) | 66 (2) | .12 | 5 (1) | 14 (1) | .91 | 6 (1) | 52 (2) | 0.10 |
| HCV genotype non-1, n (%) | 9 (2) | 140 (14) | <0.001 | NA | NA | ||||
| HCV-RNA undetectable, n (%) | 3 (0.8) | 19 (2) | .14 | NA | NA | ||||
Abbreviations: HCV, hepatitis C virus; ALT, alanine aminotransferase; ULN, upper limit of normal; RNA, ribonucleic acid; NA, not applicable.
P values were not adjusted for multiplicity.
Table 2.
Reasons for HCV Treatment Ineligibility Among All Patients According to Race
| Black* (n = 962) | Nonblack* (n = 3507) | Relative Risk (95% CI) | P† | |
|---|---|---|---|---|
| Failed screening evaluation | 387 (40) | 999 (28) | 1.41 (1.29–1.55) | <0.001 |
| HCV treatment not initiated for reason other than treatment ineligibility | 103 (11) | 245 (7) | 1.53 (1.23–1.91) | <0.001 |
| Did not wish to continue | 55 (6) | 160 (5) | 1.25 (0.93–1.69) | 0.14 |
| Lost to follow-up | 39 (4) | 53 (2) | 2.68 (1.79–4.03) | <0.001 |
| Noncompliance | 7 (1) | 31 (1) | 0.82 (0.36–1.86) | 0.64 |
| Adverse event | 2 (<1) | 1 (<1) | n/a‡ | N/a‡ |
| HCV treatment ineligible§ | 284 (30) | 754 (21) | 1.37 (1.22–1.54) | <0.001 |
| Abnormal hematologic value | 65 (7) | 83 (2) | 2.85 (2.08–3.92) | <0.001 |
| Abnormal chemistry value | 60 (6) | 78 (2) | 2.80 (2.02–3.90) | <0.001 |
| Poorly controlled diabetes mellitus | 14 (1) | 15 (0.4) | 3.40 (1.65–7.02) | <0.001 |
| Clinically significant cardiac disease | 5 (0.5) | 13 (0.4) | 1.40 (0.50–3.92) | 0.52 |
| Preexisting or uncontrolled medical disease‖ | 74 (8) | 196 (6) | 1.38 (1.06–1.78) | 0.02 |
| Preexisting or uncontrolled psychiatric disease¶ | 41 (4) | 125 (4) | 1.20 (0.85–1.69) | 0.31 |
| Recent drug or alcohol abuse | 19 (2) | 101 (3) | 0.69 (0.42–1.11) | 0.12 |
| Exclusionary virology including HCV RNA not detected, non-1 HCV genotype and missing | 14 (1) | 159 (5) | 0.32 (0.19–0.55) | <0.001 |
| HCV treatment ineligible for reason other than exclusionary virology | 270 (28) | 595 (17) | 1.65 (1.46–1.87) | <0.001 |
Abbreviations: CI, confidence interval; HCV, hepatitis C virus; RNA, ribonucleic acid.
Data shown are number (percentage of total number).
P values were not adjusted for multiplicity.
Chi-square calculation not performed due to small sample size.
Patients may have more than 1 reason for ineligibility.
Identified by the investigator at the time of screening; no further information describing the specific preexisting or uncontrolled medical condition(s) was available.
Clinical diagnosis or Center for Epidemiologic Studies Depression Scale score >25.
Screen failure was more frequent in black patients (40.2%, 387 of 962 screened) compared with non-black patients (28.5%, 999 of 3,507 screened). Overall, black patients were 41% more likely to fail screening than nonblack patients (RR, 1.41; 95% CI, 1.29– 1.55; P < 0.001) (Table 2). Racial differences were also observed in the subgroup of 1,038 patients who were ineligible for HCV treatment. Overall, 29.5% (284 of 962 screened) of blacks and 21.5% (754 of 3,507 screened) of nonblacks were ineligible for treatment, indicating that black patients were 37% more likely to be ineligible for HCV treatment (RR of ineligibility, 1.37; 95% CI, 1.22–1.54; P < 0.001). However, nonblack patients were more likely than blacks to be excluded on the basis of undetectable plasma HCV RNA (which would not require treatment) or infection with HCV genotype 2 or 3 (which would not preclude treatment) (P < 0.001). Importantly, after restriction of the analysis to viremic patients with genotype 1 infection, black patients were 65% less likely to be eligible for HCV treatment than were nonblack patients (RR of protocol ineligibility, 1.65; 95% CI, 1.46–1.87; P < 0.001) (Table 2).
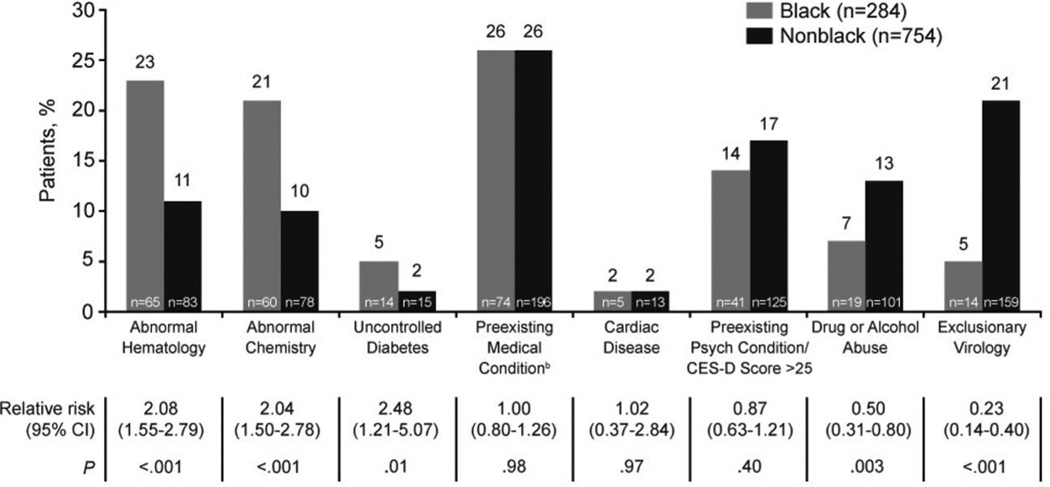
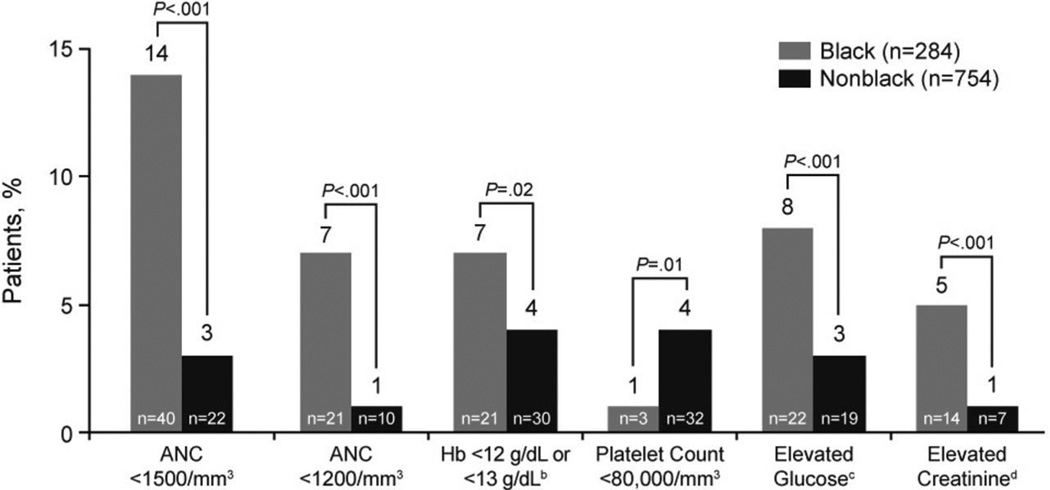
Racial differences in the frequencies and types of contraindications to HCV treatment were apparent in the subset of patients found to be ineligible (n = 1,038, Figs. 2, 3). Compared with nonblacks, black patients were more likely to be ineligible for HCV treatment on the basis of abnormal hematology findings (23% versus 11%; RR, 2.08; 95% CI, 1.55–2.79; P < 0.001), abnormal blood chemistry values (21% versus 10%; RR, 2.04; 95% CI, 1.50–2.78; P < 0.001), and/ or uncontrolled diabetes mellitus (5% versus 2%; RR, 2.48; 95% CI, 1.21–5.07; P = 0.01) (Fig. 2). The hematologic parameters affecting blacks more than non-blacks included neutropenia (14% versus 3% for ANC <l,500/mm3, P < 0.001; 7% versus 1% for ANC <l,200/mm3, P < 0.001) and anemia (7% versus 4%, P = 0.02); thrombocytopenia was less common among blacks than nonblacks (1% versus 4%, P = 0.01) (Fig. 3). The abnormal blood chemistry values that were more likely to exclude blacks from HCV treatment were elevated blood glucose (8% versus 3%, P < 0.001) and serum creatinine levels (5% versus 1%, P < 0.001). Among patients who failed to meet HCV treatment eligibility criteria, blacks were less likely than nonblacks to be excluded because of recent drug or alcohol abuse (7% versus 13%; RR, 0.50; 95% CI, 0.31–0.80; P = 0.003) and/or exclusionary virology (5% versus 21%; RR, 0.23; 95% CI, 0.14–0.40; P < 0.001) (Fig. 2). No difference in treatment eligibility was observed between black and nonblack patients with respect to cardiac disease or psychiatric conditions including moderate-to-severe depression.
Fig. 2.
Prevalence of contraindications to HCV treatment among black and nonblack patients determined to be ineligible. aPatients may have had more than one reason for ineligibility, bIdentified by the investigator at the time of screening; no further information describing the specific preexisting or uncontrolled medical condition(s) was available.
Fig. 3.
Prevalence of specific hematologic and metabolic abnormalities among black and nonblack patients determined to be ineligible for HCV treatment. aPatients may have had more than one reason for ineligibility. bHb levels <12 g/dL for women and <13 g/dL for men. cGlucose levels >140 mg/dL. dGreater than normal serum creatinine level.
Discussion
Due to its large size, geographically diverse treatment centers, representative proportion of black patients, and use of FDA-approved medications, the IDEAL study population represents a unique sample of patients who sought treatment for HCV infection in the U.S. Further, the criteria for HCV treatment eligibility in this postapproval study were similar to those recommended for use in routine clinical practice by expert guidelines and outlined in the product information approved by the FDA.11,8–22 In this context, the findings that nearly 25% of patients presenting to medical centers for treatment of hepatitis C were ineligible for PEG-IFN/RBV and that black Americans were 65% more likely than nonblack Americans to be ineligible for therapy have important public health implications, particularly in the context of the Institute of Medicine report on viral hepatitis and liver cancer in the U.S.23
Hepatitis C disproportionately affects black Americans; the prevalence of chronic HCV infection and resultant liver disease is higher among blacks than other racial and ethnic group in the U.S.1,24Further, among black patients in the IDEAL study and other clinical trials, the sustained virologic response rates to treatment with PEG-IFN/RBV have been markedly lower than those for patients from other populations with similar clinical characteristics.8–10,15 Recent genome-wide association studies suggest that the observed differential response is in part due to genetic polymorphisms near the gene for IL-28B; other research suggests that the difference is unlikely to be explained by factors that may be modifiable, such as differences in drug pharmacokinetics or patient adherence.7 In this context, the observation that black Americans are less likely to be eligible for treatment with PEG-IFN/RBV indicates that the difference in successful HCV treatment outcomes between black and nonblack patients is even greater than what has been reported in clinical trials in which only treatment-eligible patients are observed, particularly if blacks are less likely to enroll in HCV treatment trials, as has been seen in clinical trials of other chronic medical conditions.25 Further, whereas the use of specific HCV protease inhibitors, such as telaprevir or boceprevir, will increase the SVR rate among HCV-infected patients, including blacks, these treatments will not impact the rate of HCV treatment eligibility in clinical trials or practice because PEG-IFN/ RBV will remain the backbone of treatment regimens involving these first-generation protease inhibitors.26,27
Unlike host genetic polymorphisms, barriers to HCV treatment eligibility may be amenable to interventions that could improve uptake of therapy. Among the reasons for HCV treatment ineligibility, inadequately controlled diabetes mellitus was more common among blacks than nonblacks. This finding is not unexpected because diabetes mellitus, higher hemoglobin A1c levels (among persons with diabetes mellitus), and medical complications associated with diabetes are more prevalent among blacks than non-Hispanic white adults in the U.S.28,29 Although the explanation for the diabetes-related racial differences among patients presenting for HCV treatment in IDEAL is likely multifactorial, diabetes represents a modifiable barrier to treatment. Previous studies have suggested that inadequate access to primary medical care and health insurance may, in part, explain the increased prevalence of suboptimal diabetes control among blacks; improved access to healthcare may therefore enhance HCV treatment eligibility among black Americans.30–32
Blacks were also more likely to be ineligible due to renal insufficiency. Although a single serum creatinine measurement is insufficient to diagnose chronic kidney disease, black Americans are more likely than non-Hispanic whites to have estimated glomerular filtration rates less than 60 mL/min/1.73 m2 or elevated urinary albumin-to-creatinine ratios, and they are at greater risk for renal disease.33,34 Although the cause of abnormal renal function was not assessed, the association between diabetes and renal disease suggests that the observed racial differences in diabetes control may also have contributed to a greater risk of renal insufficiency among blacks presenting for HCV treatment.35 In addition, compared with nonblacks, body weight was higher among treatment-eligible and -ineligible black patients; given the association between increasing body-mass index and chronic kidney disease (CKD), this difference may also have contributed to the increased prevalence of abnormal renal function among blacks.35 Because of the interplay between renal disease, diabetes mellitus, obesity, and other medical conditions (e.g., hypertension), more effective comprehensive medical care may also help address this racial difference. Of note, HCV treatment ineligibility on the basis of impaired renal function is largely due to markedly decreased clearance of RBV, leading to increased risk and severity of anemia during therapy.36 Based on this, RBV is not approved for use in persons with estimated creatinine clearance <50 mL/min; however, pharmacokinetic studies suggest that adjustment of RBV dose based on creatinine clearance may effectively achieve safe, therapeutic drug exposure.37,38 Further research is needed to determine whether ribavirin dose adjustment is an effective strategy for treating HCV in patients ineligible for treatment with ribavirin due to renal impairment.
Another factor that contributed to higher rates of HCV treatment ineligibility among black patients was neutropenia. Given that constitutional neutropenia without apparent clinical consequence is more prevalent among blacks, this observation was not unexpected.13 Recently, the VIRAHEP-C study, which evaluated response to PEG-IFN/RBV in black and white Americans, applied a less conservative absolute neutrophil count value (>l,000/mm3) for HCV treatment eligibility; importantly, no increased frequency of neutropenia-associated morbidity was observed.10 Further, studies have failed to document a relationship between the development of interferon-related neutropenia and the incidence of bacterial infections.39,40 Accordingly, recent revisions to the HCV treatment guidelines from the American Association for the Study of Liver Disease recommend that neutropenia should not prevent treatment with PEG-IFN/RBV.11 Wider application of a less conservative ANC threshold for PEG-IFN therapy would increase HCV treatment eligibility among blacks. For example, if an ANC threshold of ≥ 1,200/ mm had been utilized in the present study, 50% of the black patients excluded because of neutropenia would have been eligible. Accordingly, practice guidelines and clinical trials of PEG-IFN-based therapy, including those with novel direct-acting antiviral drugs, should adopt a less conservative ANC threshold (e.g., 1,000 or 1,200 cells/mm3) to minimize the medically unnecessary exclusion of black patients. Similar to neutropenia, more blacks than nonblacks were ineligible for HCV treatment due to anemia. This racial difference mirrors population-based studies which demonstrate that black Americans have lower average hemoglobin levels than whites even after controlling for the greater prevalence of conditions like thalassemia and/ or iron-deficiency.13,41 Because anemia due to PEG-IFN/ RBV may have clinically significant consequences, the application of more liberal eligibility criteria (e.g., lower required hemoglobin level) is not likely to be feasible. HCV treatment regimens that do not include RBV may be needed to overcome this barrier to therapy.
Our study has several limitations. First, the HCV treatment eligibility criteria applied in this clinical trial may be more restrictive than those used by physicians in clinical practice, which could result in a higher rate of treatment ineligibility than would be observed in other settings. However, in this study of FDA-approved medications the eligibility criteria were modeled on expert guidelines and current product labels for both PEG-IFNs. Second, whereas we did not detect differences in the screen failure rate at academic and community sites, we do not have data regarding the rate of HCV treatment, if any, of the ineligible patients at each individual site and cannot exclude the potential for differences in clinical practice at the academic and community sites. Third, we cannot exclude the possibility of selection bias if blacks with HCV and comorbid medical conditions were more likely than otherwise healthy HCV-infected blacks to seek primary medical care and then subsequently be referred for HCV treatment. If otherwise healthy blacks with HCV infection are less likely to access primary medical care than are otherwise healthy whites with HCV infection, our findings may overestimate racial differences in HCV treatment eligibility. Data on possession of health insurance might have provided a surrogate marker for access to medical care, but these data were not collected at screening. Fourth, because we sampled patients who presented to expert medical centers seeking HCV treatment, these data are highly likely to overestimate the proportion of patients eligible for HCV therapy compared with the general population in the U.S. Indeed, several reports suggest that as many as 60% of unselected HCV-infected patients may not be candidates for current HCV treatment.5,18 Thus, this analysis represents a conservative estimate of rates of ineligibility in black and nonblack Americans. Fifth, categorization of race was self-reported. Recent analysis of DNA from a large subset of patients enrolled in the IDEAL study suggests that the misclassification rate for race was ≈ 8%.7 Although not insignificant, this is unlikely to influence the overall findings. Sixth, whereas we would have liked to perform an assessment for differential rates of eligibility between Hispanic whites and non-Hispanic whites, we were unable to do so because data on this racial distinction were not collected at screening. Finally, patients were excluded based on the findings of clinical and laboratory assessments performed at only one or two time-points. In clinical practice, medical interventions (e.g., better treatment of diabetes) could effectively correct some of these exclusionary abnormalities.
In conclusion, compared with nonblacks, black Americans are ≈65% less likely to be eligible for HCV treatment. Although there are multiple factors underlying this observed racial difference, several barriers to HCV treatment that were more prevalent in blacks, such as inadequately controlled diabetes mellitus and renal insufficiency, may be overcome with comprehensive strategies to provide effective medical care, thereby increasing eligibility for current and future HCV treatments that include PEG-IFN/RBV In addition, the adoption of less conservative requirements for absolute neutrophil counts would be expected to make more blacks eligible to receive HCV treatment. Nonetheless, when considered in the context of markedly lower SVR rates for blacks treated with PEG-IFN/RBV, the finding that blacks are also significantly less likely to be eligible for this treatment underscores the need for novel antiviral regimens to impact HCV disease among black Americans.
Acknowledgment
M. T Melia serves as advisor for Tibotec. A.J. Muir consults for Zymogenetics, receives grant/research support from Schering-Plough, Valeant, Vertex, Zymogenetics, and speaks for Schering-Plough. J. McCone speaks for Schering-Plough and Roche. M.L. Shiffman serves as advisor for Gilead, Schering-Plough, Anadys, Vertex, Biolex, Human Genome Sciences, Novartis, and Zymogenetics, consults for Roche and Pfizer, receives grant/research support from Roche, Schering-Plough, Vertex, Biolex, GlaxoSmithKline, Globeimmune, Human Genome Sciences, Idenix, Tibotec, Zymogenetics, and Gilead, and speaks for Roche and Schering-Plough. J. King and F.A. Nunes receive grant/research support from Schering-Plough. S.K. Herrine receives grant/research support from Human Genome Sciences, Roche, and Schering-Plough. G. W. Galler serves as advisor for Schering-Plough and Gilead and speaks for Takeda. J. Bloomer and W. Cassidy receive grant/ research support from Schering-Plough and Roche. K.A. Brown serves as advisor for Schering-Plough, consults for Blue Cross, receives grant/research support from Schering-Plough, Bristol-Myers Squibb, and Bayer-Onyx, and speaks for Schering-Plough, Roche, Gilead, and Bayer-Onyx. K.D. Mullen serves as advisor for Salix, Ocera, and Hyperion, receives grant/research support from Salix, and speaks for Hoffman La Roche and CLDG. N. Ravendhran receives grant/research support from Schering-Plough, Roche, Gilead, and Bristol-Myers Squibb. R. Ghalib receives grant/research support from Roche, Schering-Plough, Gilead, Vertex, Pharmasett, Debio, Biolex, Abbott, Merck, Medarex, Bristol-Myers Squibb, Idenix, Idera, Cleveland Clinic, and Duke Clinical Research and speaks for Roche and Three Rivers. N. Boparai is an employee of Schering-Plough Research Institute. S. Noviello consults for Schering-Plough. C.A. Brass is an employee of and holds stock in Schering-Plough. J.K. Albrecht is an employee of Schering-Plough. J.G. McHutchison consults for Abbott, Anadys, Biolex, Gilead, National Genetics Institute, Pharmasset, Pfizer, and United Therapeutics and receives grant/research support from GlaxoSmithKline, Globe Immune, Human Genome Sciences, Idera, Intarcia, Medtronics, Novartis, Roche, Schering-Plough, Vertex Pharmaceuticals, Virochem, and Osiris Therapeutics. M.S. Sulkowski serves as advisor for Roche, Schering-Plough, Merck, Human Genome Sciences, BIPI, Gilead, Vertex, Tibotec, Bristol-Myers Squibb, and Pfizer and receives grant/research support from Mederax, Peregrine, Debiopharm, and Abbott. R. Jiang has nothing to disclose.
Supported by grants from Schering-Plough Research Institute, now Merck Research Laboratories. Trial Registration: ClinicalTrials.gov; NCT00081770; www.clinicalTrials.gov.
Abbreviations
- ANC
absolute neutrophil count
- CES-D
Center for Epidemiologic Studies Depression
- CI
confidence interval
- FDA
United States Food and Drug Administration
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- HPV
human immunodeficiency virus
- IDEAL
Individualized Dosing Efficacy versus Flat Dosing to Assess Optimal Pegylated Interferon Therapy
- IL-28B
interleukin-28B
- PEG-IFN
pegylated interferon
- RBV
ribavirin
- RNA
ribonucleic acid
- RT-PCR
real-time polymerase chain reaction
- SCr
serum creatinine
- SVR
sustained virologic response
- WBC
white blood cell.
Footnotes
Presented in part at the 60th Annual Meeting of the American Association for the Study of Liver Diseases; October 30-November 3, 2009; Boston, MA. Poster #848.
Author Contributions: Drs. Melia and Sulkowski had access to all the study data, take responsibility for the accuracy of the analysis, and had authority over article preparation and the decision to submit the article for publication. The authors thank the study coordinators, nurses, and patients involved in the study as well as Lisa Pedicone, PhD, Michael Geffner, MD, Richard Valanzola, Andrew Baczkowski, Kenneth Koury, Karen Kelly, Misti Lina-berry, Helen Nguyen, and Peter Savino from Schering-Plough Research Institute, now Merck Research Laboratories for their contributions in conducting the study. The authors also thank the study investigators of the IDEAL study team: Afdhal, Nezam; Al-Osaimi, Abdullah; Bacon, B; Balart, Luis; Bennett, Michael; Bernstein, David; Bini, Edmund; Black, Martin; Bonilla, Hector; Box, Terry; Boyer, Thomas; Brau, Norbert; Brown, Robert; Bruno, Christine; Chung, Raymond; Clain, David; Crippin, Jeffrey; Dalke, Douglas; Davis, Charles; Davis, Gary; Davis, Mitchell; Felizarta, Franco; Firpi-Morell, Roberto; Flamm, Steven; Franco, Jose; Freilich, Bradley; Galati, Joseph; Gibas, Alexandra; Godofsky, Eliot; Gordon, Fredric; Gross, John; Harrison, Stephen; Herrera, Jorge; Herring, Robert; Hu, Ke-Qin; Israel, Jonathan; Jacobson, Ira; Joshi, Shobha; Khalili, Mandana; Kilby, Alan; King, Paul; Koch, Alvaro; Krawitt, Edward; Kugelmas, Marcelo; Kwo, Paul; Lambiase, Louis; Lawitz, Eric, Lebovics, Edward; Lee, William; Levin, James; Levine, Robert; Lidofsky, Steven; Lucey, Michael; Mailliard, Mark; Marsano, Luis; Martin, Paul; McGarrity, Thomas; Mikolich, Dennis; Morgan, Timothy; Munoz, Santiago; Nelson, Donald; Nyberg, Anders; Nyberg, Lisa; Oh, Sangik; Pandya, Prashant; Pauly, Mary Pat; Peine, Craig; Perrillo, Robert; Poleynard, Gary; Poordad, Fred; Post, Anthony; Poulos, John; Pound, David; Rabinovitz, Mordechai; Ready, Joanna; Reddy, Rajender; Reindollar, Robert; Reuben, Adrian; Rossaro, Lorenzo; Rothman, Lawrence; Rubin, Raymond; Rustgi, Vinod; Ryan, Michael; Schiff, E; Schmidt, Warren; Semon, William; Sepe, Thomas; Sherman, Kenneth; Sjogren, Maria; Sjogren, Robert; Smith, Coleman; Stein, Lawrence; Strauss, Robert; Swaim, Mark; Szabo, Gyongnyi; Thurn, Joseph; Tong, Myron; Vierling, John; Wu, George; Yapp, Rockford; Younes, Ziad; Zaman, Atif.
References
- 1.Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;16:705–7l4. doi: 10.7326/0003-4819-144-10-200605160-00004. 144. [DOI] [PubMed] [Google Scholar]
- 2.Hepatology; National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C; 2002-June 10-12, 2002; 2002. pp. S3–S20. [DOI] [PubMed] [Google Scholar]
- 3.McHutchison JG, Poynard T, Pianko S, Gordon SC, Reid AE, Dienstag J, et al. The impact of interferon plus ribavirin on response to therapy in black patients with chronic hepatitis C. The International Hepatitis Interventional Therapy Group. Gastroenterology. 2000;119:1317–1323. doi: 10.1053/gast.2000.19289. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen GC, Segev DL, Thuluvath PJ. Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45:1282–1289. doi: 10.1002/hep.21580. [DOI] [PubMed] [Google Scholar]
- 5.Butt AA, Justice AC, Skanderson M, Rigsby MO, Good CB, Kwoh CK. Rate and predictors of treatment prescription for hepatitis C. Gut. 2007;56:385–389. doi: 10.1136/gut.2006.099150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rousseau CM, Ioannou GN, Todd-Stenberg JA, Sloan KL, Larson MF, Forsberg CW, et al. Racial differences in the evaluation and treatment of hepatitis C among veterans: a retrospective cohort study. Am J Public Health. 2008;98:846–852. doi: 10.2105/AJPH.2007.113225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461:399–401. doi: 10.1038/nature08309. [DOI] [PubMed] [Google Scholar]
- 8.Muir AJ, Bornstein JD, Killenberg PG. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. N Engl J Med. 2004;350:2265–2271. doi: 10.1056/NEJMoa032502. [DOI] [PubMed] [Google Scholar]
- 9.Jeffers LJ, Cassidy W, Howell CD, Hu S, Reddy KR. Peginterferon alfa-2a (40 kd) and ribavirin for black American patients with chronic HCV genotype 1. Hepatology. 2004;39:1702–1708. doi: 10.1002/hep.20212. [DOI] [PubMed] [Google Scholar]
- 10.Conjeevaram HS, Fried MW, Jeffers LJ, Terrault NA, Wiley-Lucas TE, Afdhal N, et al. Peginterferon and ribavirin treatment in African American and Caucasian American patients with hepatitis C genotype 1. Gastroenterology. 2006;131:470–477. doi: 10.1053/j.gastro.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Ghany MG, Strader DB, Thomas DL, Seeff LB. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–1374. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Artinyan A, Mailey B, Sanchez-Luege N, Khalili J, Sun CL, Bhatia S, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116:1367–1377. doi: 10.1002/cncr.24817. [DOI] [PubMed] [Google Scholar]
- 13.Reed WW, Diehl LF. Leukopenia, neutropenia, and reduced hemoglobin levels in healthy American blacks. Arch Intern Med. 1991;151:501–505. [PubMed] [Google Scholar]
- 14.Streiff MB, Mehta S, Thomas DL. Peripheral blood count abnormalities among patients with hepatitis C in the United States. Hepatology. 2002;35:947–952. doi: 10.1053/jhep.2002.32486. [DOI] [PubMed] [Google Scholar]
- 15.McHutchison JG, Lawitz EJ, Shiffman ML, Muir AJ, Galler GW, McCone J, et al. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med. 2009;361:580–593. doi: 10.1056/NEJMoa0808010. [DOI] [PubMed] [Google Scholar]
- 16.PEGASYS (peginterferon alfa-2a)Prescribing Information. Nutley NJ: Hoffman-La Roche; 2010. Revised March 2010. [Google Scholar]
- 17.PEGINTRON (peginterferon alfa-2b) Prescribing Information. Kenilworth, NJ: Schering; 2010. Revised January 2010. [Google Scholar]
- 18.Falck-Ytter Y, Kale H, Mullen KD, Sarbah SA, Sorescu L, McCullough AJ. Surprisingly small effect of antiviral treatment in patients with hepatitis C. Ann Intern Med. 2002;136:288–292. doi: 10.7326/0003-4819-136-4-200202190-00008. [DOI] [PubMed] [Google Scholar]
- 19.Rowan PJ, Tabasi S, Abdul-Latif M, Kunik ME, El-Serag HB. Psychosocial factors are the most common contraindications for antiviral therapy at initial evaluation in veterans with chronic hepatitis C. J Clin Gastroenterol. 2004;38:530–534. doi: 10.1097/01.mcg.0000123203.36471.70. [DOI] [PubMed] [Google Scholar]
- 20.Seal KH, Currie SL, Shen H, Anand BS, Bini EJ, Brau N, et al. Hepatitis C treatment candidacy and outcomes among 4318 US veterans with chronic hepatitis C virus infection: does a history of injection drug use matter? J Clin Gastroenterol. 2007;41:199–205. doi: 10.1097/01.mcg.0000212644.82853.51. [DOI] [PubMed] [Google Scholar]
- 21.Markowitz JS, Gutterman EM, Hodes D, Klaskala W. Factors associated with the initiation of alpha-interferon treatment in Medicaid patients diagnosed with hepatitis C. J Viral Hepat. 2005;12:176–185. doi: 10.1111/j.1365-2893.2005.00607.x. [DOI] [PubMed] [Google Scholar]
- 22.Dienstag JL, McHutchison JG. American Gastroenterological Association technical review on the management of hepatitis C. Gastroenterology. 2006;130:231–264. doi: 10.1053/j.gastro.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell AE, Colvin HM, Palmer BR. Institute of Medicine recommendations for the prevention and control of hepatitis B and C. Hepatology. 2010;51:729–733. doi: 10.1002/hep.23561. [DOI] [PubMed] [Google Scholar]
- 24.Howell C, Jeffers L, Hoofnagle JH. Hepatitis C in African Americans: summary of a workshop. Gastroenterology. 2000;119:1385–1396. doi: 10.1053/gast.2000.19582. [DOI] [PubMed] [Google Scholar]
- 25.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 26.McHutchison JG, Everson GT, Gordon SC, Jacobson IM, Sulkowski M, Kauffman R, et al. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360:1827–1838. doi: 10.1056/NEJMoa0806104. [DOI] [PubMed] [Google Scholar]
- 27.Mederacke I, Wedemeyer H, Manns MP. Boceprevir, an NS3 serine protease inhibitor of hepatitis C virus, for the treatment of HCV infection. Curr Opin Investig Drugs. 2009;10:181–189. [PubMed] [Google Scholar]
- 28.Twombly JG, Long Q, Zhu M, Wilson PW, Venkat NK, Fraser LA, et al. Diabetes care in black and white veterans in the southeastern United States. Diabetes Care. 2010;33:958–963. doi: 10.2337/dc09-1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adams AS, Zhang F, Mah C, Grant RW, Kleinman K, Meigs JB, et al. Race differences in long-term diabetes management in an HMO. Diabetes Care. 2005;28:2844–2849. doi: 10.2337/diacare.28.12.2844. [DOI] [PubMed] [Google Scholar]
- 30.Rhee MK, Cook CB, El-Kebbi I, Lyles RH, Dunbar VG, Panayioto RM, et al. Barriers to diabetes education in urban patients: perceptions, patterns, and associated factors. Diabetes Educ. 2005;31:410–417. doi: 10.1177/0145721705277022. [DOI] [PubMed] [Google Scholar]
- 31.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149:170–176. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 32.Hadley J, Steinberg EP, Feder J. Comparison of uninsured and privately insured hospital patients. Condition on admission, resource use, and outcome. JAMA. 1991;265:374–379. [PubMed] [Google Scholar]
- 33.Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A, et al. United States Renal Data System 2008 Annual Data Report. Am J Kidney Dis. 2009;53(1 Suppl):S1–S374. doi: 10.1053/j.ajkd.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 34.McClellan W, Warnock DG, McClure L, Campbell RC, Newsome BB, Howard V, et al. Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol. 2006;17:1710–1715. doi: 10.1681/ASN.2005111200. [DOI] [PubMed] [Google Scholar]
- 35.Castro AF, Coresh J. CKD surveillance using laboratory data from the population-based National Health and Nutrition Examination Survey (NHANES) Am J Kidney Dis. 2009;53(3 Suppl 3):S46–S55. doi: 10.1053/j.ajkd.2008.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sulkowski MS, Wasserman R, Brooks L, Ball L, Gish R. Changes in haemoglobin during interferon alpha-2b plus ribavirin combination therapy for chronic hepatitis C virus infection. J Viral Hepat. 2004;11:243–250. doi: 10.1111/j.1365-2893.2004.00490.x. [DOI] [PubMed] [Google Scholar]
- 37.Bruchfeld A, Lindahl K, Schvarcz R, Stahle L. Dosage of ribavirin in patients with hepatitis C should be based on renal function: a population pharmacokinetic analysis. Ther Drug Monit. 2002;24:701–708. doi: 10.1097/00007691-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Kamar N, Chatelut E, Manolis E, Lafont T, Izopet J, Rostaing L. Ribavirin pharmacokinetics in renal and liver transplant patients: evidence that it depends on renal function. Am J Kidney Dis. 2004;43:140–146. doi: 10.1053/j.ajkd.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 39.Soza A, Everhart JE, Ghany MG, Doo E, Heller T, Promrat K, et al. Neutropenia during combination therapy of interferon alfa and ribavirin for chronic hepatitis C. Hepatology. 2002;36:1273–1279. doi: 10.1053/jhep.2002.36502. [DOI] [PubMed] [Google Scholar]
- 40.Cooper CL, Al Bedwawi S, Lee C, Garber G. Rate of infectious complications during interferon-based therapy for hepatitis C is not related to neutropenia. Clin Infect Dis. 2006;42:1674–1678. doi: 10.1086/504386. [DOI] [PubMed] [Google Scholar]
- 41.Beutler E, West C. Hematologic differences between African-Americans and whites: the roles of iron deficiency and alpha-thalassemia on hemoglobin levels and mean corpuscular volume. Blood. 2005;106:740–745. doi: 10.1182/blood-2005-02-0713. [DOI] [PMC free article] [PubMed] [Google Scholar]