Abstract
Parenteral thiamine has a very high safety profile. The most common adverse effect is local irritation; however, anaphylactic or anaphylactoid reactions may occur, mostly related to intravenous administration. We describe a 44-year-old man, a chronic alcoholic, who was admitted with alcohol intoxication and developed cardiac arrest due to anaphylactic shock following intravenous thiamine infusion. The patient was successfully resuscitated after 15 min and repeated epinephrine administrations. He was discharged in good health after 14 days. This case report emphasises both the importance of recognising the symptoms of anaphylaxis and the fact that facilities for treating anaphylaxis and cardiopulmonary resuscitation should be available when thiamine or for that matter, any drug is given in-hospital.
Background
Thiamine deficiency is not an uncommon clinical condition and may require rapid parenteral repletion. Parenteral thiamine administration is generally safe. Transient local irritation is the most common adverse effect; however, anaphylactic or anaphylactoid reactions may occur, mostly related to intravenous administration.
This case report describes a 44-year-old man who developed cardiac arrest due to a severe anaphylactic reaction to thiamine.
Case presentation
A 44-year-old alcohol-intoxicated man with no known allergies was admitted to the emergency department because of diffusely located squeezing pain in the chest and the abdomen. The abdomen was moderately tender on palpation, but there was no abdominal guarding. The patient had been drinking alcohol the entire day.
Vital parameters at admission were: pulse 90 bpm, blood pressure 110/85 mm Hg and temperature 35.9°C. Arterial blood gases did not show any acid–base abnormalities and the oxygenation status was normal as well. Blood glucose was 5.9 mM. The patient had a history of ischaemic heart disease, but the ECG at admission showed sinus rhythm with no signs of ischaemia.
Treatment
According to local guidelines, the patient was given an intravenous administration of 300 mg of thiamine hydrochloride at admission. He had received this drug on several previous occasions without any complications. No other drugs were given, and besides a considerable amount of beer the patient had not consumed anything for the entire day.
Shortly after administration of thiamine, the patient was found unresponsive with abnormal rattling respiration. Cardiopulmonary resuscitation with chest compressions and bag-mask ventilation in the ratio 30:2 was started immediately, and the cardiac arrest team including an anaesthetist was called. The initial rhythm analysis revealed pulseless electrical activity, and epinephrine was given according to advanced life support guidelines. The patient was intubated to allow uninterrupted compressions and ventilation. After 15 min, sinus rhythm was re-established. This was followed by a short period of atrial fibrillation with right bundle branch block, which was converted to a stable sinus rhythm with an intravenous bolus of 300 mg of amiodarone.
Investigations
A CT of the patient's thoracic and abdominal cavities showed no pathology besides several fractured ribs. A subsequently performed coronary angiography showed no new pathology of the coronary arteries and serial measurements of troponin T were normal. Serum tryptase confirmed the diagnosis of anaphylaxis. The samples were obtained after 1 and 24 h, respectively (figure 1).
Figure 1.
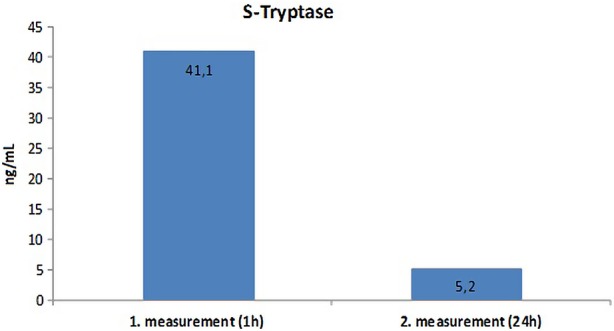
Serum tryptase levels of the patient.
Outcome and follow-up
The patient was transferred to the intensive care unit, and he was discharged in good health after 14 days.
Discussion
Hypersensitivity reactions are common; however, most reactions are subclinical and require no treatment. Anaphylaxis is a far more severe, potentially fatal hypersensitivity reaction. The condition is rare but can be observed after exposure to almost any substance.1
The central mechanism of anaphylaxis is the production of immunoglobulin E (IgE) that triggers the allergic response after binding to receptors on mast cells (MC) and basophil granulocytes (BG); however, non-IgE-mediated or non-immune release of mediators can also occur. Exposure to an allergen allows IgE to activate MC and BG, resulting in the release of histamine and other mediators such as proteases, mainly tryptase.2 This leads to vasodilation. The symptoms are a combination of dermatological, respiratory, cardiovascular, neurological and gastrointestinal symptoms, with the former two being the most frequent. Signs of anaphylaxis normally present within 5–30 min after exposure to an allergen.3 4 Rapid administration of epinephrine is lifesaving.5
Repeated measurements of serum tryptase levels can confirm mastocytosis and thereby the diagnosis of anaphylaxis. Optimally, the measurement should be carried out within 15 min to 3 h of symptom onset and then again after 24 h. If the tryptase level is greater than 11.4 ng/mL in acute serum compared with baseline serum, the diagnosis of anaphylaxis is confirmed; however, a tryptase level that is within normal limits cannot be used to refute the clinical diagnosis of anaphylaxis and in these cases, typically food-induced anaphylaxis or in patients with anaphylaxis who are normotensive, the history trumps the test results.6 7
Thiamine or vitamin B1 (figure 2) is used for treating vitamin deficiency syndromes such as beriberi and Wernicke's encephalopathy. Since the clinical presentation of Wernicke's encephalopathy is variable, thiamine should be given to all patients at risk or in whom the condition is suspected. High incidences of thiamine deficiency are found among chronic alcoholics, malnourished patients and after bariatric surgery, but also after chronic diuretic therapy and during hyperemesis gravidarum.8
Figure 2.
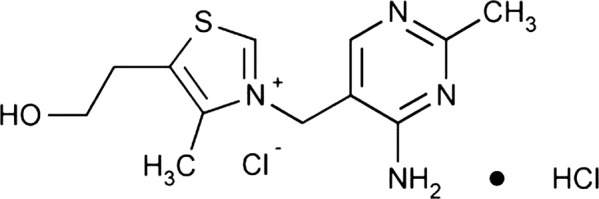
The structure of thiamine.
Thiamine has a very high safety profile. Adverse events are most commonly seen after multiple intravenous administrations.8 Nevertheless, the incidence of anaphylaxis because of parenteral administration of thiamine is unknown. The condition has been reported for the last six decades since the use began, but the reports are very scarce. A search of the PubMed database only gave 28 hits when using the search terms ‘Anaphylaxis AND Thiamine’. No reports of anaphylaxis due to orally administered thiamine exist. There are only a few casuistic reports describing anaphylaxis and fatalities because of administration of parenteral thiamine, but several reports of mildly allergic reactions.9–12 Moreover, a toxicity study described no anaphylactic reactions and only minor allergic reactions in 1.1% of the 989 patients included in the study.9
In conclusion it is recommended to continue the present use of thiamine. The implications of changing the present treatment strategy are far more dangerous than continued use. It is, however, important for physicians to be aware of the symptoms of anaphylaxis because the simple treatment is lifesaving when initiated at an early state.8
Learning points.
Thiamine deficiency is not an uncommon clinical condition and may require rapid parenteral repletion.
Parenteral thiamine has a very high safety profile; however, anaphylactic or anaphylactoid reactions may occur, mostly related to intravenous administration.
Facilities for treating anaphylaxis should be available when thiamine, or for that matter, any drug is given in hospital, including facilities for cardiopulmonary resuscitation and adrenaline.
Footnotes
Contributors: All authors have made substantive contributions to the study, and endorse the data and conclusions.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Simons FE, Ardusso LR, Bilò MB, et al. 2012 Update: World Allergy Organization guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol 2012;2013:389–99 [DOI] [PubMed] [Google Scholar]
- 2.Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol 2006;2013(2 Suppl Mini-Primer):S450–6 [DOI] [PubMed] [Google Scholar]
- 3.Khan BQ, Kemp SF. Pathophysiology of anaphylaxis. Curr Opin Allergy Clin Immunol 2011;2013:319–25 [DOI] [PubMed] [Google Scholar]
- 4.Lee KJ, Vadas P. Anaphylaxis: mechanisms and management. Clin Exp Allergy 2011;2013:923–38 [DOI] [PubMed] [Google Scholar]
- 5.Kemp SF, Lockey RF, Simons FE. Epinephrine: the drug of choice for anaphylaxis. Allergy 2008;2013:1061–70 [DOI] [PubMed] [Google Scholar]
- 6.Schwartz LB, Metcalfe DD, Miller JS, et al. Tryptase levels as an indicator of mast-cell activation in systemic anaphylaxis and mastocytosis. N Engl J Med 1987;2013:1622–6 [DOI] [PubMed] [Google Scholar]
- 7.Schwartz LB, Yunginger JW, Miller J, et al. Time course of appearance and disappearance of human mast cell tryptase in the circulation after anaphylaxis. J Clin Invest 1989;2013:1551–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sechi G, Serra A. Wernicke's encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol 2007;2013:442–55 [DOI] [PubMed] [Google Scholar]
- 9.Wrenn KD, Murphy F, Slovis CM. A toxicity study of parenteral thiamine hydrochloride. Ann Emerg Med 1989;2013:867–70 [DOI] [PubMed] [Google Scholar]
- 10.Johri S, Shetty S, Soni A, et al. Anaphylaxis from intravenous thiamine—long forgotten? Am J Emerg Med 2000;2013:642–3 [DOI] [PubMed] [Google Scholar]
- 11.Morinville V, Jeannet-Peter N, Hauser C. Anaphylaxis to parenteral thiamine (vitamin B1). Schweiz Med Wochenschr 1998;2013:1743–4 [PubMed] [Google Scholar]
- 12.Van Haecke P, Ramaekers D, Vanderwegen L, et al. Thiamine-induced anaphylactic shock. Am J Emerg Med 1995;2013:371–2 [DOI] [PubMed] [Google Scholar]


