Abstract
Herpes simplex virus (HSV) is a double-stranded virus belonging to human herpes virus family. Although it exists in eight various forms, HSV-1 causes most of the oral infections. Since dentists are more likely to be consulted in the case of oral infections, familiarity with these lesions becomes mandatory. It is more commonly reported in children and rarely in adults. This article presents an acute episode of primary herpetic gingivostomatitis in a 32-year-old male patient.
Background
Herpetic infections commonly affect the dental profession's anatomical area of responsibility and the diagnosis and management of such infections fall in the purview of oral healthcare providers. To administer competent care to patients with herpetic infections, clinicians must understand the disease, its treatment, the impact the disease or its treatment may have on the patient and the extent to which the presence of a herpetic infection may impact on caregivers in the clinical process.
Case presentation
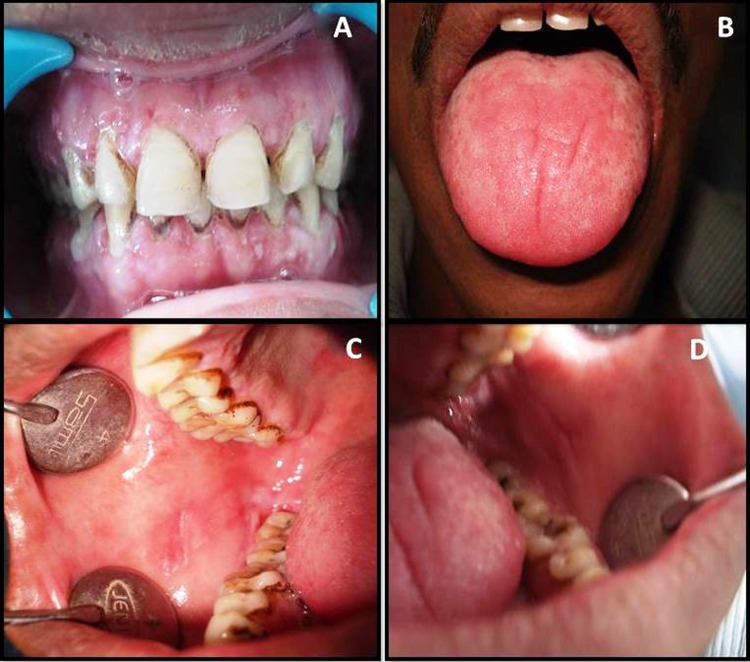
A 32-year-old man reported to the outpatient department with a burning sensation in the mouth that worsened on eating hot and spicy food. He gave a history of ulcers in the entire mouth since 2 days. Medical history revealed that he was suffering from fever and generalised weakness. He had not taken any medical or dental treatment for the problem. Family history was unremarkable. On intraoral examination, gingiva appeared fiery red in colour and multiple vesicles were present on the attached mucosa (figure 1A). Multiple vesicles and ulcers were seen along the lateral border and anterior surface of the tongue (figure 1B). Both sided buccal mucosa revealed multiple vesicles and papules. These ulcers coalesced together, thereby giving a geographic map like configuration (figure1C,D). On the basis of clinical features, diagnosis of acute primary herpetic gingivostomatitis was made. Treatment started immediately and the patient responded well showing healing of lesions after 2 weeks (figure 2).
Figure 1.
A 32-year-old male patient presenting with acute primary herpetic gingivostomatitis:(A) Multiple vesicles on both keratinised and non-keratinised mucosa. The gingiva is fiery red in colour. (B) Multiple ulcers present along the lateral border and anterior dorsal surface of tongue. (C) Multiple vesicles and papules coalesce in large map like configuration on right buccal mucosa. (D) Multiple vesicles and papules coalesce in large map like configuration on right buccal mucosa.
Figure 2.
Photographs of the same patient, 2 weeks after treatment showing complete healing of the lesions as seen on gingival (A), tongue (B), both-sided buccal mucosa (C and D).
Investigations
The diagnosis of primary herpetic gingivostomatitis is generally defined by the clinical data, and no confirmative tests are necessary.1 The available investigations are:
Viral culture is considered the gold standard and the most sensitive of the diagnostic techniques, but is generally limited to the hospital setting.
Direct immunofluorescence technique also not readily available and is restricted to hospital setting.
Tzanck test demonstrates multinucleated epithelial giant cells which are consistent with a herpes virus infection. It generally detects only about 60% of herpes simplex virus (HSV) infections.
Smears also yield no information as to whether the viral agent is HSV-1, HSV-2 or Varicella zoster virus.
Differential diagnosis
Recurrent herpes simplex infection
Major apthous stomatitis
Erythema multiformae
Treatment
The patient was instructed to eat nutritious, soft, blend diet and the following medications were prescribed:
acyclovir 200 mg five times a day, to be rinsed and swallowed.
benzydamine hydrochloride mouthwash (0.15 g/100 mL)was prescribed for symptomatic relief from burning sensation.
Analgesics and antipyretics (Aceclofenac 100 mg and Paracetamol 500 mg) were given to address fever and malaise.
Outcome and follow-up
The patient responded well to the medication and complete healing was seen after 2 weeks (figure 2).
Discussion
Two of the known Herpesviridae, herpes simplex viruses type 1 (HSV-1) and HSV-2, are responsible for primary and recurrent mucocutaneous herpetic infections. HSV-1 is predominately associated with orolabial infections, while HSV-2 is predominately associated with genital disease. Orogenital contact may allow either serotype to cause oral or genital lesions. The two forms of HSV have a similar structure, but differ in antigenicity, although HSV-2 is reputed to be of greater virulence.2 Structurally, the herpes virus is made up of three components:
capsid shell—which consists proteins and double-stranded DNA.
envelop—which consists of a lipid bilayer with 11 embedded glycoproteins, four of which are essential for viral entry into host cells.
tegument—which is a proteinaceous region between the capsid and the envelope.3
Following exposure, the virions attach to the host cells which is mediated by envelop-related viral proteins. Once the virus has gained entry into the cytoplasm, it loses its capsid proteins by the process known as uncoating and the viral nucleic acid is transported into the host-cell nucleus. In the host-cell nucleus, the viral genome is replicated. In the next step, the new viral genome is transcribed into mRNA, which subsequently is translocated to host-cell ribosomes. The viral proteins synthesised by host-cell ribosomes are assembled with the duplicate viral genome. Assembly is followed by maturation, a process essential for the newly formed virions to become infectious. The newly synthesised viruses, in turn, may infect other epithelial cells or enter sensory nerve endings.4 5
Most herpetic infections are transmitted from infected persons to others through direct contact with a lesion or infected body fluids, for example, vesicular exudates, saliva and genital fluids.
Clinically, HSV-1 infections begin with prodromal symptoms of fever, loss of apetite, malaise and myalgia. Within few days of prodromal symptoms, erythema and clusters of vesicles and/or ulcers appear on the hard palate, attached gingival and dorsum of tongue and non-keratinised mucosa of buccal and labial mucosa, ventral tongue and soft palate.3 6 Vesicles break down to form ulcers that are usually 1–5 mm and coalesce to form larger ulcers with scalloped borders and marked surrounding erythema. The gingiva is often fiery red, and the mouth is extremely painful, causing difficulty in eating. (Our patient reported with all these features.)
It is important to distinguish primary from recurrent herpetic infection. History may be helpful in distinguishing primary from secondary infection, as patients with a secondary infection will recall previous episodes of vesicular eruptions on their lips.4 5 7
Treatment modalities include
Nutritional supplements.
Analgesics such as acetaminophen to manage the associated pain and malaise.
- Antiviral drugs:
- Acyclovir: in cream or as oral suspension administered in a rinse and swallow technique.
- Valacyclovir: increase the bioavailability of acyclovir (to which it is converted via hepatic metabolism) by 3–5 times.
- Famciclovir: the oral prodrug of penciclovir has an oral bioavailability 3–5 times that of acyclovir.
Both penciclovir and acyclovir function through competitive inhibition of viral DNA synthesis by means of selective phosphorylation by viral thymidine kinase. Although acyclovir is a more potent inhibitor of viral DNA polymerase, the advantage of penciclovir and its analogues is that it is present in infected cells at much higher concentrations and for longer periods than acyclovir and its analogues.6 7
Learning points.
Acute forms of herpes simplex virus infection pose a high risk for transmission. Thus, protective measures (gloves, mouth masks) should be taken while examining these patients.
Antiviral drug do not affect dormant virus protected in nerve ganglions, and therefore will not eliminate the virus completely, so the patient may suffer from recurrent herpes labialis again.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lawall MA, Almeida JFA, Bosco JMD, et al. Primary herpetic gingivostomatitis in adult: case report. Revista Odonto Ciência 2005;2013:191–4 [Google Scholar]
- 2.Chandrasekar PH. Identification and treatment of herpes lesions. Adv Wound Care 1999;2013:254–62 [PubMed] [Google Scholar]
- 3.Kolokotronis A, Doumas S. Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis. Clin Microbiol Infect 2006;2013:202–11 [DOI] [PubMed] [Google Scholar]
- 4.Regezi JA, Sciubba JJ. Oral pathology-clinical pathologic correlations. Philadelphia: Saunders, 2003 [Google Scholar]
- 5.Arduino PG, Porter SR. Herpes simplex virus type 1 infection: overview on relevant clinico-pathological features. J Oral Pathol Med 2008;2013:107–21 [DOI] [PubMed] [Google Scholar]
- 6.Quinn JP, Dalziel RG, Nash AA. Herpes virus latency in sensory ganglia—a comparison with endogenous neuronal gene expression. Prog Neurobiol 2000;2013:167–79 12 [DOI] [PubMed] [Google Scholar]
- 7.Miller CS, Danaher RJ. Asymptomatic shedding of herpes simplex virus (HSV) in the oral cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;2013:43–50 [DOI] [PubMed] [Google Scholar]