Abstract
A 76-year-old man presented with abdominal pain and constipation for 1 month. The pain was dull aching in nature and over the right upper abdomen. He also reported decreased appetite. The patient had no previous attacks of acute pancreatitis or history of trauma. There was no history of fever or melena. On visual inspection of the abdomen, there was a mass effect protruding out of the right mid-abdomen. The mass was approximately measuring 15×15 cm, firm in consistency, non-tender, non-mobile and not moving with respiration. Haematological investigations were normal. Both amylase and lipase were within normal limits. A CT of the abdomen revealed a large well-defined thin-walled cystic lesion measuring 10.3×13.9×14.3 cm in the right lumbar and iliac region without calcification or haemorrhage. A diagnosis of retroperitoneal cyst was made and the patient was taken up for surgery. Histology of the cyst showed the absence of epithelia and was reported as pseudocyst.
Background
Retroperitoneal pseudocyst is usually pancreatic in origin. Non-pancreatic retroperitoneal pseudocyst is very rare. It is slow growing and does not give rise to symptoms until it attains large size and compresses over the adjacent structures. Care has to be taken during dissection of the large pseudocyst as there is possibility of inadvertent injury to the vital structures like duodenum, ureter and major vessels, thereby adding to the morbidity.
Case presentation
A 76-year-old man presented with abdominal pain and constipation for 1 month duration. The pain was dull aching in nature and over the right upper abdomen. He reported decreased appetite and constipation. The patient had no previous attacks of acute pancreatitis or history of trauma. There was no history of fever or melena. He had no urinary symptoms. On visual inspection of the abdomen, there was a mass effect protruding out of the right mid-abdomen. The mass was approximately measuring 15×15 cm, non-tender, non-mobile and not moving with respiration. The margins were well-defined and it was firm in consistency. A diagnosis of retroperitoneal cyst (RC) was made with the help of imaging and the patient was taken up for surgery.
Investigations
Haematological investigations were normal. Both amylase and lipase were within normal limits.
A CT scan of the abdomen showed a large well-defined thin-walled cystic lesion measuring 10.3×13.9×14.3 cm in the right lumbar and iliac region without calcification or haemorrhage (figure 1). Superior mesenteric vessels were seen draping the anterior aspect of the lesion. Rest of the bowel was normal.
Figure 1.

CT of the abdomen showing a large well-defined thin-walled cystic lesion measuring 10.3×13.9×14.3 cm in the right lumbar and iliac region without calcification or haemorrhage.
Histology of the cyst showed the absence of epithelia and was reported as pseudocyst (figure 2).
Figure 2.
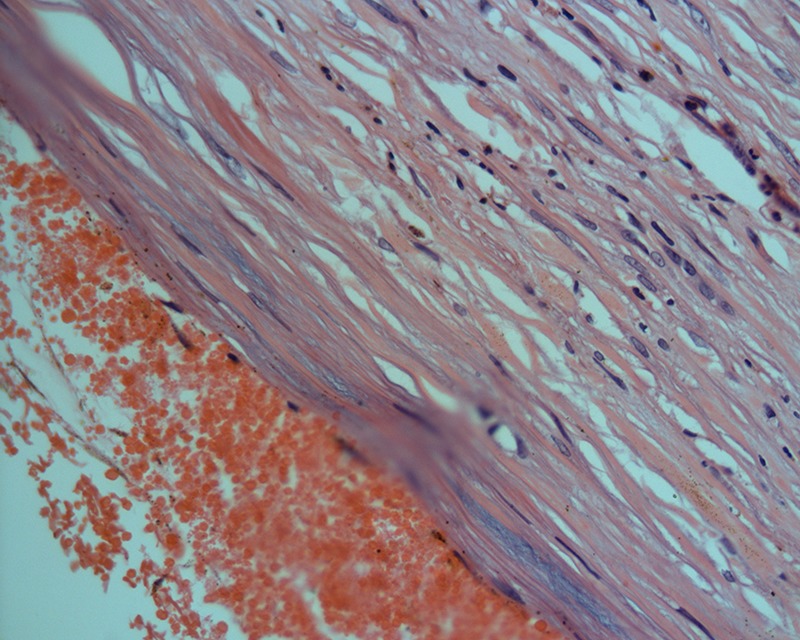
Histology of the cyst showing the absence of epithelium.
Differential diagnosis
Simple cyst
Mesenteric cyst
Treatment
The cyst was excised in toto after separating it from the duodenum, transverse colon and the ureter (figure 3). The major vessels were preserved.
Figure 3.
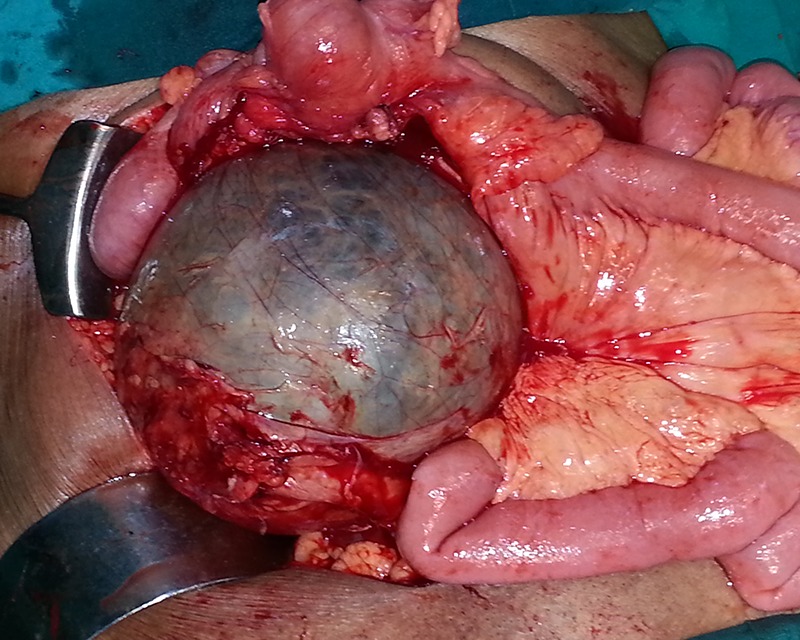
Intraoperative image: large retroperitoneal cyst separated from caecum and small bowel.
Outcome and follow-up
Postoperatively, the patient developed biliary leak and was managed conservatively with nil per oral, fluids and antibiotics. He recovered in 2 weeks and was discharged after suture removal. He is on regular follow-up.
Discussion
RCs are cysts originating within the fatty areolar tissue of the retroperitoneum without any communication to the adjacent structures. They are rare, with an incidence of 1/5750–1/250 000.1 They are usually slow growing within the connective tissue and do not give rise to symptoms until they attain large size and compress over the adjacent structures. The pathogenesis of these cysts remains unclear. The differential diagnosis of cystic lesions in the retroperitoneum is extensive and includes non-neoplastic cysts—such as pseudocyst, enteric duplication cyst, enteric cyst, mesothelial cyst, lymphocele and parasitic cyst—and neoplastic cysts—such as cystic lymphangioma, mucinous cystadenoma, epidermoid cyst, cystic teratoma, cystic mesothelioma and cystic degeneration of solid tumours.2
Cysts that do not have an epithelial lining are termed as pseudocysts. A pseudocyst is mostly pancreatic in origin, more common in the peripancreatic region and is associated with high levels of amylase and lipase. Our patient had no previous history of acute pancreatitis and both amylase and lipase were normal. Pseudocysts which are non-pancreatic and non-parasitic are rare within the retroperitoneum, and usually arise from the mesentery or the omentum. They usually contain serous fluid. Symptoms are non-specific and on examination there may be a palpable freely movable abdominal mass.3 They can have sudden abdominal pain when there is infection or bleeding within the pseudocyst. Large pseudocysts can press over the adjacent structures and have symptoms of constipation, vomiting and abdominal fullness. Both ultrasonography and CT scan of the abdomen can be diagnostic. Pseudocysts are usually unilocular or multilocular fluid-filled cysts with thick walls.4 Long-standing cysts can get calcified and give the classical appearance of an egg shell. On histopathology, the cyst wall contains fibrous tissue without an epithelial lining. Surgical excision is the mainstay of the treatment of the pseudocyst.5 The cyst has to be excised in toto in order to prevent any recurrence owing to residual cyst wall. The cyst has to be meticulously dissected from the adherent bowel and retroperitoneal structures. Care has to be taken to identify the ureter and stent it preoperatively thereby avoiding inadvertent injury. In case of large cysts, the fluid can be aspirated and then the dissection continued. Nowadays, laparoscopic excision of the pseudocyst is performed, but in our case the cyst was too large to be amenable for laparoscopic surgery.6 Marsupialisation and partial excision are not preferred procedures.
Learning points.
Non-pancreatic retroperitoneal pseudocyst is rare and can attain enormous size.
Symptoms are non-specific and on examination there may be a palpable freely movable abdominal mass.
Sudden abdominal pain may be owing to infection or bleeding within the pseudocyst.
The cyst wall has to be excised in toto in order to prevent any recurrence.
Footnotes
Contributors: RP was involved in concept and design of the case report and also the guarantor. YS was involved in manuscript preparation and GR in manuscript editing. RB was involved in defining the intellectual content and literature search.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Alzaraa A, Mousa H, Dickens P, et al. Idiopathic benign retroperitoneal cyst: a case report. J Medl Case Rep 2008;2013:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stoupis C, Ros PR, Abbitt PL, et al. Bubbles in the belly: imaging of cystic mesenteric or omental masses. Radiographics 1994;2013:729–37 [DOI] [PubMed] [Google Scholar]
- 3.Okur H, Kucukarydin M, Ozokutan BH, et al. Mesenteric, omental and retroperitoneal cysts in children. Eur J Surg 1997;2013:673–7 [PubMed] [Google Scholar]
- 4.Yang DM, Jung DH, Kim H, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics 2004;2013:1353e65. [DOI] [PubMed] [Google Scholar]
- 5.Burkett JS, Pickleman J. The rationale for surgical treatment of mesenteric and retroperitoneal cysts. Am Surg 1994;2013:432–5 [PubMed] [Google Scholar]
- 6.Downey DM, Dolan JP, Hunter JG. Laparoscopic resection of a giant retroperitoneal cyst. San Francisco, CA: American College of Surgeons Clinical Congress, 2005. (video presentation) [Google Scholar]


