Abstract
Agranulocytosis is a rare yet life-threatening complication of methimazole therapy for hyperthyroidism. We present the case of a 37-year-old female recently started on methimazole for hyperthyroidism who presented to our facility for evaluation of suspected thyroid storm. In addition to having abnormal thyroid indices, she was noted to have an odontogenic abscess, and was septic with profound neutropenia. Her symptoms resolved quickly following incision and drainage of her abscess and treatment with broad-spectrum antibiotics. Her neutrophil count improved significantly following cessation of methimazole and administration of granulocyte colony-stimulating factor. Diagnosis was initially confounded by the similarity between symptoms of early sepsis and those of thyroid storm. This case report discusses the factors leading to diagnostic delay and highlights the dangerous manifestations of neutropenia in patients on methimazole therapy.
Background
Agranulocytosis is a rare complication of the treatment of hyperthyroidism with the thionamide class of medications, occurring in 0.2–0.5% of patients on methimazole therapy.1 Bacterial infection in the setting of neutropenia—from methimazole or other cause—is rapidly fatal if untreated, and represents a medical emergency.2 Our case highlights a potential pitfall in the early recognition and subsequent management of a rare life-threatening condition. The diagnosis proved challenging because the patient's symptoms of fever, tachycardia, diaphoresis, agitation, chest pain and tremor along with her abnormal thyroid function tests are commonly seen in thyroid storm. In addition, recent surgery (a common precipitant) together with the patient's medication non-compliance, further added to suspicion for thyroid storm. Our case serves to remind physicians of the importance of maintaining a high index of suspicion for neutropenia in all patients presenting with fever, sore throat or other infectious symptoms while on methimazole treatment.
Case presentation
A 37-year-old female with a history of hyperthyroidism, recently initiated on methimazole, was transferred to our emergency department with concern for thyroid storm. The patient had undergone bilateral lumpectomy for breast cancer less than 1 week previously. One day before presentation, the patient noted subjective fevers, chills, abdominal and chest pain, night sweats and anxiety. On initial evaluation she was noted to be tachycardic at 140 bpm, febrile to 38.8°C, and demonstrated a tremor on physical examination. A CT scan was performed out of concern for pulmonary embolism. Imaging demonstrated a 3 cm mass in the left thyroid gland. Thyroid stimulating hormone (TSH) level was undetectable, however lactic acid level and troponin were normal. The patient was given intravenous fluids, 25 mg of oral metoprolol and 650 mg of oral acetaminophen, and was transferred to our institution for further management of suspected thyroid storm.
On evaluation of her medical history in the emergency department, the patient stated that her hyperthyroidism was diagnosed 6 years ago and had been medically managed, although she was non-compliant at that time. She denied any prior history of thyroid surgery or radioactive iodine treatment. She was recently started on 7.5 mg methimazole/day for her hyperthyroidism by a new primary care physician, and was taking no other medications. The patient gave the additional history of right-sided facial pain and swelling for the past 2 days. The patient's vital signs were notable for a blood pressure of 112/63 with a heart rate of 140 bpm, a respiratory rate of 26 breaths/min and a temperature of 38.2°C. On physical examination the patient demonstrated a tremor in all extremities, and tenderness with fluctuance over the left lower mandibular border, surrounding tooth 19.
Investigations
A complete blood count with differential revealed 7.58×103/μL white blood cells with 0% neutrophils. Thyroid testing was notable for a total T3 of 185 ng/dL (upper limit of normal being 178 ng/dL), free T4 of 3 ng/dL (upper limit of normal being 1.2 ng/dL) and a TSH of 0.036 μIU/mL (lower limit being 0.4 μIU/mL). Lactic acid was within normal limits. Initial blood cultures were negative. Electrocardiogram demonstrated sinus tachycardia.
Differential diagnosis
As outlined above, the initial diagnosis was thyroid storm. See discussion below for a detailed commentary on the diagnosis in this case.
Treatment
Following transfer to our facility and upon discovery of febrile neutropenia with the likely source of odontogenic abscess, oral surgery was consulted for incision and drainage. Approximately 0.5 µL of purulent material was drained from the soft tissues adjacent to tooth 19. The patient was treated with intravenous piperacillin/tazobactam and vancomycin, 2 L of normal saline and 20 mg of oral propranolol. She was admitted to the hospital and was given 300 μg of subcutaneous granulocyte colony-stimulating factor (GCSF; filgrastim) for treatment of methimazole-induced agranulocytosis. The patient was continued on intravenous piperacillin/tazobactam and vancomycin for 3 days and then transitioned to oral amoxicillin/clavulanic acid prior to discharge. She was maintained on 10 mg of oral propranolol twice daily as an outpatient for symptomatic management of hyperthyroidism. Methimazole was discontinued upon presentation to our emergency department.
Outcome and follow-up
Following incision and drainage of her periodontal abscess, the patient remained afebrile throughout her hospital stay. She had not taken methimazole for 2 days and treating physicians held it on admission as well. The patient's initial neutrophil count rapidly improved from an initial count of 0/μL to 90×103/μL in 1 day. After one dose of GCSF her neutrophil count increased further from 90×103 to 7230×103/μL. No additional doses of GCSF were given (figure 1). The patient's anxiety and tachycardia improved with treatment of her infection and low-dose propranolol administration. She was asymptomatic 3 days after presentation and was discharged with strict precautions against taking methimazole or propylthiouracil and planned endocrinology follow-up. The patient received ablative radioactive iodine therapy for a toxic thyroid nodule and had no further symptoms of thyrotoxicosis.
Figure 1.
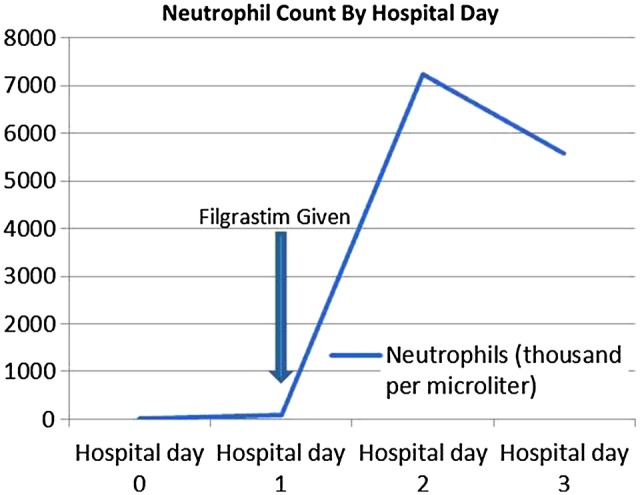
Graph displaying the patient's neutrophil count by hospital day. The arrow indicates the single administration of the granulocyte colony-stimulating factor analogue, filgrastim (300 μg subcutaneously).
Discussion
Thionamide medications including carbimazole, its active metabolite methimazole, and propylthiouracil, are the most common initial treatment for thyrotoxicosis in many countries, and are increasingly used as a first-line treatment in the USA where radioactive iodine therapy has traditionally been popular.1–3 Agranulocytosis is a rare side-effect of thionamide medication use, occurring in 0.2–0.5% of patients taking methimazole. Methimazole-induced agranulocytosis is considered an idiosyncratic drug reaction which may occur at any time during therapy and at any dose. It is most common during the first 2–3 months of therapy and at higher daily doses.4 Many physicians regularly monitor patients’ complete blood counts during therapy, however this can be ineffective given the rapidity with which agranulocytosis can develop.
Infectious symptoms such as fever or sore throat are often the initial presentation of agranulocytosis.5 There are several reports describing the discovery of antithyroid drug-induced agranulocytosis in the setting of occult bacterial or fungal infections.6–8 Treatment entails withdrawal of the offending agent and avoidance of all thionamide agents in the future due to concerns about cross-reactivity.9 GCSF is useful for the treatment of agranulocytosis from thionamide medications (see cited articles and references therein).10 11
Thyroid storm is a rare complication of hyperthryoidism which presents with extreme symptoms of thyrotoxicosis including tachycardia, cardiovascular collapse, arrhythmia, hypotension, fever, psychiatric disturbances and gastrointestinal upset. Examination reveals tremor, lid lag and moist/warm skin. Thyroid function test results are often similar to those seen in hyperthyroidism, and there are no specific values which differentiate thyroid storm from uncomplicated hyperthyroidism.12 Thyroid storm is often precipitated by an acute event such as surgery (thyroidal or non-thyroidal), infection or childbirth. Abrupt withdrawal of antithyroid medications can also precipitate thyroid storm. Clinical decision making tools have been proposed for the recognition of thyroid storm, with the most referenced being that by Burch and Wartofsky in 1993; unfortunately the diagnosis is not certain in many cases.13
In this case, there are several reasons why the correct diagnosis was delayed and thyroid storm was initially suspected as the underlying illness. First, this patient had incompletely treated thyrotoxicosis at baseline with abnormal thyroid function tests, a large thyroid mass on CT imaging, and a fine tremor and anxiety on examination, suggesting she likely had a component of thyrotoxicosis upon presentation as well as sepsis. Second, this patient's recent surgery and questionable medication compliance were thought to represent possible precipitants for thyroid storm. Finally, the patient's symptoms of sepsis, including tachycardia, fever, mildly low blood pressures, night sweats and agitation, could all be explained by thyroid storm. Using the aforementioned clinical decision rules suggested by Burch and Wartofsky, the patient would have scored 65 (for agitation, tachycardia at 140 bpm, temperature at 38.8°C and mild abdominal pain) which is ‘highly suggestive of thyroid storm’.13
This report reflects, to the authors’ best knowledge, the first depiction of sepsis and agranulocytosis in a patient on methimazole mimicking thyroid storm. Such cases serve as an important reminder to physicians that, despite its ubiquity, the diagnosis of sepsis can be challenging. It also adds to the literature suggesting that GCSF is effective in shortening the recovery time of methimazole-induced agranulocytosis. While our patient made a full recovery, this case highlights the critical importance of considering agranulocytosis in patients on methimazole therapy who present with infectious symptoms.
Learning points.
Agranulocytosis is a life-threatening complication of methimazole therapy which may present with fever, sore throat or symptoms of sepsis.
Thyroid storm is a rare and potentially fatal endocrinological emergency which frequently occurs following a precipitant such as surgery or acute illness and presents with symptoms of severe thyrotoxicosis including tachycardia, arrhythmia, cardiovascular collapse, hypotension, fever, psychiatric disturbances and gastrointestinal upset.
In patients with underlying hyperthyroidism, sepsis may mimic thyroid storm in presentation and laboratory analysis, so clinical decision making tools may be misleading.
Physicians must maintain a high index of suspicion for neutropenia in patients on methimazole who present with infectious symptoms.
Footnotes
Contributors: SGR managed the case, performed the literature search, wrote the article and is the guarantor. FH contributed to the literature search and writing of the article. AAA had the idea for the article, helped manage the case, and contributed overall edits.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Franklyn JA, Boelaert K. Thyrotoxicosis. Lancet 2012;2013:1155–66 [DOI] [PubMed] [Google Scholar]
- 2.Cooksley T, Holland M. The febrile patient with neutropenia. Acute Med 2012;2013:246–50 [PubMed] [Google Scholar]
- 3.Wartofsky L, Glinoer D, Solomon B, et al. Differences and similarities in the diagnosis and treatment of Graves’ disease in Europe, Japan, and the United States. Thyroid 1991;2013:129–35 [DOI] [PubMed] [Google Scholar]
- 4.Takata K, Kubota S, Fukata S, et al. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid 2009;2013:559–63 [DOI] [PubMed] [Google Scholar]
- 5.Roeloffzen WW, Verhaegh JJ, van Poelgeest AE, et al. Fever or a sore throat after start of antithyroidal drugs? A medical emergency. Neth J Med 1998;2013:113–17 [DOI] [PubMed] [Google Scholar]
- 6.Cheng HT, Lin FY. Pseudomonas aeruginosa necrotizing fasciitis in a patient with methimazole-induced agranulocytosis. Am Surg 2011;2013:1561–2 [PubMed] [Google Scholar]
- 7.Ramírez C, Hernández AF, Méndez V, et al. Case report of mucormycosis in a patient with secondary methimazole-induced agranulocytosis. Gac Med Mex 2009;2013:235–8 [PubMed] [Google Scholar]
- 8.Pinto ME, Banda C, Seas C. Pulmonary aspergillosis due to methimazole-induced neutropenia: a case report. Rev Peru Med Exp Salud Publica 2012;2013:255–8 [DOI] [PubMed] [Google Scholar]
- 9.Cooper DS. Antithyroid drugs. N Engl J Med 1984;2013:1353–62 [DOI] [PubMed] [Google Scholar]
- 10.Dai WX, Zhang JD, Zhan SW, et al. Retrospective analysis of 18 cases of antithyroid drug (ATD)-induced agranulocytosis. Endocr J 2002;2013:29–33 [DOI] [PubMed] [Google Scholar]
- 11.Sun MT, Tsai CH, Shih KC. Antithyroid drug-induced agranulocytosis. J Chin Med Assoc 2009;2013:438–41 [DOI] [PubMed] [Google Scholar]
- 12.Nayak B, Burman K. Thyrotoxicosis and thyroid storm. Endocrinol Metab Clin North Am 2006;2013:663–86 [DOI] [PubMed] [Google Scholar]
- 13.Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am 1993;2013:263. [PubMed] [Google Scholar]


