Abstract
Infundibular dilations (IDs) are funnel-shaped enlargements in the origin of intracranial arteries. Usually, IDs occur at the junction between posterior communicating artery (PcomA) and internal carotid artery (ICA). Progression from an ID of the PcomA to aneurysms has been described, but is unclear whether an ID is a preaneurysmal state or a normal anatomical variant. The authors describe a 55-year-old female patient presenting multiple intracranial aneurysms with a small one arising from an ID at the level of posterior communicating segment of ICA. To the best of our knowledge, after a criterious search in the English literature, it is the first description of such unusual combination. The preoperative neurosurgical planning is discussed as well as the importance of intraoperative findings to the best management of this unusual situation.
Background
Infundibular dilations (IDs) are funnel-shaped symmetrical enlargements in the origin of cerebral arteries. The nature of these dilations is a matter of discussion.1 Some authors consider an ID as a preaneurysmal lesion,2–4 while others believe that is a normal variant.3 Although an infundibulum may represent an incompletely regressed remnant of previously dominant fetal vessels, it should be considered as a potential source of future subarachnoid haemorrhage (SAH).1 5–7 There are several reports on the literature about ID associated or not intracranial aneurysms and SAH. To the best of our knowledge, it is the first description of an aneurysm arising from an ID at the level of posterior communicating artery (PcomA). The preoperative neurosurgical planning is discussed as well as the importance of intraoperative findings to the best management of this unusual situation.
Case presentation
A 55-year-old female patient was referred to the neurosurgical department because of severe headache whose intensity increased in the last week and presented no response to analgesics. She had no loss of consciousness and she was 15 points on Glasgow Coma Scale.
Investigations
CT scans were performed and revealed no SAH. The three-dimensional CT angiography (3D-CTA) showed aneurysms on the right middle cerebral artery (MCA) bifurcation and the ophthalmic segment of the left internal carotid artery (ICA). The patient was submitted to digital subtraction angiography (DSA), whose results confirmed not only the aneurysms found by 3D-CTA but also revealed a small aneurysm arising from an ID at the level of right PcomA, which had no fetal pattern (figure 1).
Figure 1.
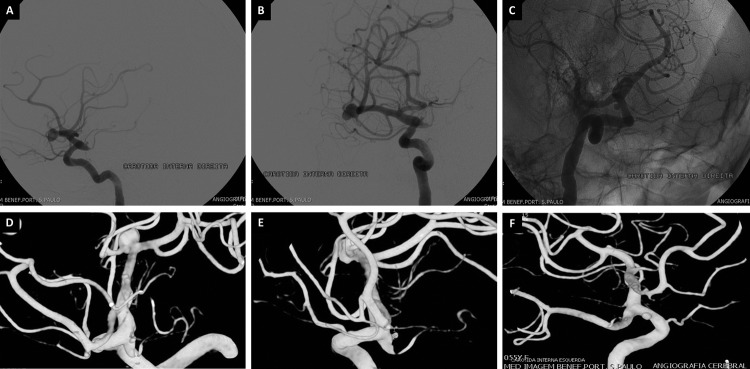
Preoperative digital subtraction angiography (DSA) images. (A and B) Aneurysm of the right middle cerebral artery and infundibular dilation at the origin of posterior communicating artery with a small aneurysm arising from this artery. (C) Aneurysm in the ophthalmic segment of the left internal carotid artery. (D, E and F) 3D reconstruction of DSA images.
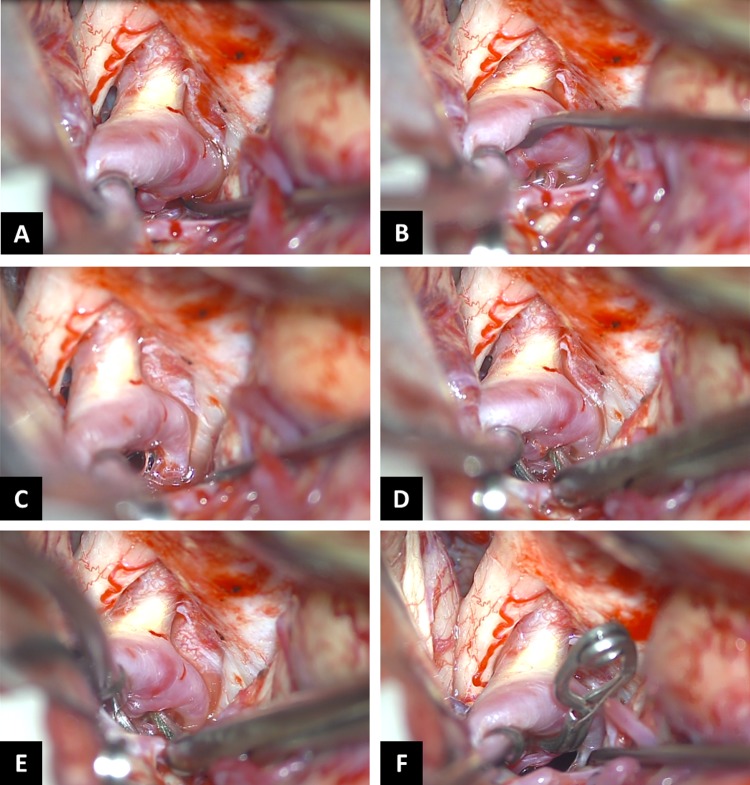
Figure 2.
Intraoperative images. (A) Infundibular dilation of the right posterior communicating artery (PcomA) with a small aneurysm arising from this artery. (B) Small perforating artery arising from PcomA, close to the proximal aneurysm’ neck. (C) PcomA with several small perforating arteries arising from this artery and oculomotor nerve. (D–F) Aneurysm’ clipping.
Treatment
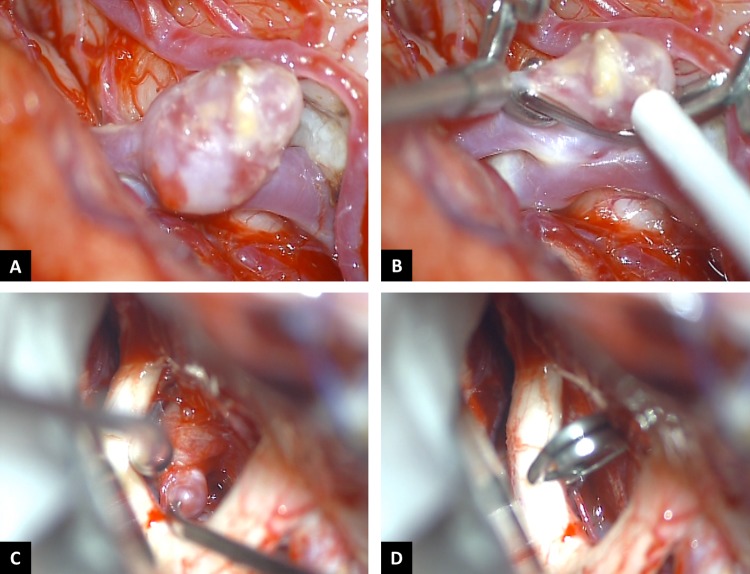
Based on DSA images, we decided to perform a right pterional craniotomy to clip the MCA aneurysm and also to put a clip at the origin of right PcomA to occlude the ID and its aneurysm, which would be an effective treatment without major risks to the patient. After MCA An. clipping, the origin of right PcomA was dissected and the presence of the ID confirmed. However, there were several perforating arteries arising close to the ID An. and also from PcomA, which changed our previous idea to a simple aneurysm clipping and preservation of PcomA with all perforating arteries. After clipping, the patency of flow in the PcomA and anterior choroidal artery was confirmed with the aid of micro-Doppler. In addition, a contra-lateral clipping of the aneurysm arising from the ophthalmic segment of the left ICA was performed without difficulty (figure 3).
Figure 3.
Intraoperative images. (A and B) Right MCA bifurcation aneurysm, pre and post clipping, respectively. (C and D) Aneurysm arising from Opthalmic segment of left ICA, pre and post clipping, respectively.
Outcome and follow-up
The postoperative period was uneventful and the postoperative DSA images performed 7 days after surgery revealed a complete occlusion of all aneurysms and preservation of PcomA (figure 4).
Figure 4.
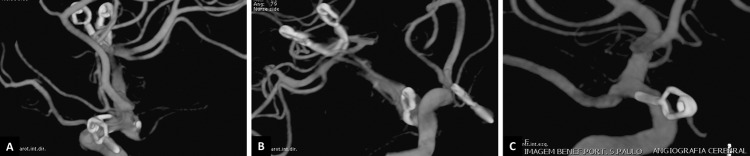
Postoperative DSA images showing (A and B) complete occlusion of MCA and ID aneurysms, as well as, (C) left ophthalmic segment of ICA.
Discussion
IDs of cerebral arteries are most frequently observed at the origin of the PcomA. Other locations are anterior choroidal artery, ophthalmic artery, MCA and superior cerebellar artery.8 Its incidence by angiography or autopsy ranges from 7% to 25%.2 4 Although the relationship between IDs and aneurysms has not been clearly defined, the progression of an ID of the PcomA to an aneurysm has been described and reported.9 However, an aneurysm arising individually from an ID is a no-reported situation.
The angiographic criteria for diagnosis of ID’s PcomA are: (1) the origin of the PcomA trunk from the apex of the dilation; (2) the maximum diameter is less than 3 mm; (3) the shape is round or conical, not saccular or irregular and (4) the infundibular widening has no aneurysm-like neck.10 Thus, an ID should appear as a symmetrical bulge without a neck in marked contrast to an intracranial aneurysm, which bulges asymmetrically from a well-defined neck.11
The pathophysiology of an aneurysm growing from ID is intriguing and remains open. One explanation is that due to defects and loss of internal elastic lamina, already studied by Hassler12 and Stehbens,13 associated by haemodynamic stress in the ID, leading to aneurysm formation.
Regarding to the best management of unusual variants, the preoperative neuroradiological assessment should be carried out with DSA to guide the surgical strategy.14 However, intraoperative findings may change the surgical planning, especially in the presence of perforating arteries not visible on DSA images.15 The planned strategy would be occlusion of the PcomA at its origin since the posterior circulation was independent. Nevertheless, intraoperative findings of perforating arteries close to the An. and arising from PcomA changed our policy to avoid risks of postoperative neurological deficit related to perforating artery occlusion.
Learning points.
Intracranial aneurysm arising from ID is a unique situation.
Preoperative neuroradiological assessment is paramount to the best neurosurgical planning.
The intraoperative findings may change the surgical strategy, especially when perforating arteries are at risk of occlusion.
Footnotes
Contributors: BJAP, VMH and JGdO were involved in the conception and design, acquisition of data or analysis and interpretation of data. BJAP and JGdO were involved in the drafting or revising the manuscript critically for important intellectual content. BJAP, CVMH and JGdO gave the final approval of the version published.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fischer S, Hopf N, Henkes H. Evolution from an infundibulum of the posterior communicating artery to a saccular aneurysm. Clin Neuroradiol 2011;2013:87–90 [DOI] [PubMed] [Google Scholar]
- 2.Ebina K, Ohkuma H, Iwabuchi T. An angiographic study of incidence and morphology of infundibular dilation of the posterior communicating artery. Neuroradiology 1986;2013:23–9 [DOI] [PubMed] [Google Scholar]
- 3.Epstein F, Ransohoff J, Budzilovich GN. The clinical significance of junctional dilatation of the posterior communicating artery. J Neurosurg 1970;2013:529–31 [DOI] [PubMed] [Google Scholar]
- 4.Saltzman GF. Infundibular widening of the posterior communicating artery studied by carotid angiography. Acta Radiol 1959;2013:415–21 [DOI] [PubMed] [Google Scholar]
- 5.Koike G, Seguchi K, Kyoshima K, et al. Subarachnoid hemorrhage due to rupture of infundibular dilation of a circumflex branch of the posterior cerebral artery: case report. Neurosurgery 1994;2013:1075–7 [DOI] [PubMed] [Google Scholar]
- 6.Ohyama T, Ohara S, Momma F. Fatal subarachnoid hemorrhage due to ruptured infundibular widening of the posterior communicating artery—case report. Neurol Med Chir (Tokyo) 1994;2013:172–5 [DOI] [PubMed] [Google Scholar]
- 7.Trasi S, Vincent LM, Zingesser LH. Development of aneurysm from infundibulum of posterior communicating artery with documentation of prior hemorrhage. AJNR Am J Neuroradiol 1981;2013:368–70 [PMC free article] [PubMed] [Google Scholar]
- 8.Endo S, Furuichi S, Takaba M, et al. Clinical study of enlarged infundibular dilation of the origin of the posterior communicating artery. J Neurosurg 1995;2013: 421–5 [DOI] [PubMed] [Google Scholar]
- 9.Martins C, Macanovic M, Costa e Silva IE, et al. Progression of an arterial infundibulum to aneurysm: case report. Arq Neuropsiquiatr 2002;2013:478–80 [DOI] [PubMed] [Google Scholar]
- 10.Fox JL, Baiz TC, Jakoby RK. Differentiation of aneurysm from infundibulum of the posterior communicating artery. J Neurosurg 1964;2013:135–8 [DOI] [PubMed] [Google Scholar]
- 11.Marshman LA, Ward PJ, Walter PH, et al. The progression of an infundibulum to aneurysm formation and rupture: case report and literature review. Neurosurgery 1998;2013:1445–8 [DOI] [PubMed] [Google Scholar]
- 12.Hassler O. The posterior communicating artery at different ages. Gerontologia 1963;2013:187–92 [DOI] [PubMed] [Google Scholar]
- 13.Stehbens WE. Histopathology of cerebral aneurysms. Arch Neurol 1963;2013:272–85 [DOI] [PubMed] [Google Scholar]
- 14.de Oliveira JG, du Mesnil de Rochemont R, Beck J, et al. A rare anomaly of the anterior communicating artery complex hidden by a large broad-neck aneurysm and disclosed by three-dimensional rotational angiography. Acta Neurochir (Wien) 2008;2013:279–84 [DOI] [PubMed] [Google Scholar]
- 15.de Oliveira JG, Beck J, Seifert V, et al. Assessment of flow in perforating arteries during intracranial aneurysm surgery using intraoperative near-infrared indocyanine green videoangiography. Neurosurgery 2007;2013(3 Suppl):63–72 [DOI] [PubMed] [Google Scholar]