Abstract
Whether placing a fistula first is the superior predialysis approach among octogenarians is unknown. We analyzed data from a cohort of 115,425 incident hemodialysis patients ≥67 years old derived from the US Renal Data System with linked Medicare claims, which allowed us to identify the first predialysis vascular access placed rather than the first access used. We used proportional hazard models to evaluate all-cause mortality outcomes based on first vascular access placed, considering the fistula group as the reference. In the study population, 21,436 patients had fistulas as the first predialysis access placed, 3472 had grafts, and 90,517 had catheters. Those patients with a catheter as the first predialysis access placed had significantly inferior survival compared with those patients with a fistula (HR=1.77; 95% CI=1.73 to 1.81; P<0.001). However, we did not detect a significant mortality difference between those patients with a graft as the first access placed and those patients with a fistula (HR=1.05; 95% CI=1.00 to 1.11; P=0.06). Analyzing mortality stratified by age groups, grafts as the first predialysis access placed had inferior mortality outcomes compared with fistulas for the 67 to ≤79-years age group (HR=1.10; 95% CI=1.02 to 1.17; P=0.007), but differences between these groups were not statistically significant for the 80 to ≤89- and the >90-years age groups. In conclusion, fistula first does not seem to be clearly superior to graft placement first in the elderly, because each strategy associates with similar mortality outcomes in octogenarians and nonagenarians.
Currently, fistula first is the general recommendation for all hemodialysis (HD) patients,1–3 with more recent discussions placing equal importance on a catheters last strategy.4 For the elderly, past and recent large cohort studies have shown that patients with arteriovenous fistulas (AVFs) have better survival compared with patients with catheters, with the next best vascular access being arteriovenous grafts (AVGs).5,6 These outcomes were based on the vascular access first used for dialysis and not the access first placed, but the latter may better reflect the actual effect of the fistula first initiative on nephrology practice.
Strong implications exist for different predialysis vascular access placement strategies in the elderly. For one, there is a greater competing risk of death before dialysis initiation in this age group,2,7 and therefore, many fistulas may never be used. In addition, although one third of fistulas fail to mature,8 those patients >65 years old have two times the failure rate compared with the younger population.9 This increased failure rate is associated with increased access-related complications and procedures. The higher rate of fistulas that fail to mature may contribute to a greater use of catheters at the time of dialysis initiation. Therefore, although the incident use of AVGs in the elderly decreased from 28.2% in the mid-1990s to 4.2% recently, the incident catheter use has increased from 56.8% to 82.3%.5,6,10
The incident HD population is aging, with an annual increase of 8%–16% in those patients >75 years old. With this increase, it is important to define factors associated with outcomes in the elderly population and particularly, octogenarians. The aim of this study is to investigate the mortality rate associated with the initial type of vascular access placed rather than the access used at initiation of HD in the elderly population. Specifically, we questioned whether fistula first as an intention to treat strategy may not be the clearly superior predialysis vascular access placement strategy in octogenarians.
Results
Baseline Characteristics
The total study cohort consisted of 115,425 incident HD patients with identified first predialysis vascular access placed: 21,436 (18.6%) were defined as having an AVF as their first predialysis access placed, 3472 (3.0%) had a graft, and 90,517 (78.4%) had a catheter. The mean age of ESRD onset in the entire study population was 76.9±6.4 years. When the study group was stratified by age, 65% were in the 67- to 79-years age group, 32.2% were in the 80- to 89-years age group, and 2.8% were in the ≥90-years age group. In our study population of patients older than 67 years, there were notable differences between our population and what is known of the racial profile of the general US HD population (75.5% whites compared with 65.7% all ages nationwide11). An additional full description of baseline characteristics and differences between the study groups is listed in Table 1.
Table 1.
Baseline characteristics of the study population at the time of ESRD (HD initiation)
| Characteristic | Entire Study Population (n=115,425) | Access Type: Fistula (n=21,436) | Access Type: Graft (n=3472) | Access Type: Catheter (n=90,517) | P Value |
|---|---|---|---|---|---|
| Age at ESRD onset, yr | |||||
| Mean (SD) | 76.9 (6.4) | 76.2 (6.0) | 76.2 (6.0) | 77.2 (6.5) | <0.001 |
| Median (interquartile range) | 77 (10) | 76 (10) | 76 (10) | 77 (10) | |
| Age categories (yr), % | <0.001 | ||||
| 67–79 (n=74,997) | 65 | 69.7 | 69.5 | 63.7 | |
| 80–89 (n=37,149) | 32.2 | 28.9 | 29.1 | 33.1 | |
| >90 (n=3279) | 2.8 | 1.4 | 1.4 | 3.2 | |
| Race, % | <0.001 | ||||
| White | 75.5 | 77.8 | 62.2 | 75.5 | |
| Black | 20.3 | 18.1 | 33.2 | 20.3 | |
| Native American | 0.7 | 0.8 | 0.6 | 0.6 | |
| Asian | 3.5 | 3.3 | 3.9 | 3.5 | |
| Other | 0.1 | 0.04 | 0.1 | 0.1 | |
| Sex, % | <0.001 | ||||
| Woman | 47.1 | 41.6 | 57.3 | 48 | |
| Man | 52.9 | 58.4 | 42.7 | 52 | |
| BMI (kg/m2) | 27.3 (6.8) | 27.9 (6.5) | 28.0 (6.9) | 27.1 (6.8) | <0.001 |
| BMI categories (kg/m2) | |||||
| Underweight (<18.5) | 6.0 | 4.1 | 4.8 | 6.5 | <0.001 |
| Normal (18.5–24.9) | 36.0 | 32.4 | 33.2 | 37.0 | |
| Overweight (25–29.9) | 30.7 | 33.4 | 30.2 | 30.0 | |
| Obese (≥30) | 27.3 | 30.1 | 31.8 | 26.5 | |
| Comorbidity index | 8.3 (1.6) | 8.1 (1.5) | 8.2 (1.5) | 8.3 (1.6) | <0.001 |
| Diabetes, % | <0.001 | ||||
| Yes | 55.1 | 56.2 | 59.9 | 54.6 | |
| No | 44.9 | 43.8 | 40.1 | 45.4 | |
| Malignancy, % | <0.001 | ||||
| Yes | 11.4 | 10.4 | 10 | 11.7 | |
| No | 88.6 | 89.6 | 90 | 88.3 | |
| PVD, % | <0.001 | ||||
| Yes | 18.3 | 18.2 | 17.6 | 18.3 | |
| No | 81.7 | 81.8 | 82.4 | 81.7 | |
| Duration of pre-ESRD nephrology care, % | <0.001 | ||||
| No care | 31.1 | 5.6 | 6.7 | 38.1 | |
| 0–6 months | 10.7 | 13.7 | 13 | 9.9 | |
| 6–12 months | 22.1 | 29.1 | 31.1 | 20.1 | |
| >12 months | 22.7 | 45.7 | 42.8 | 16.5 | |
| Missing | 13.3 | 5.8 | 6.4 | 15.4 | |
| Primary cause of ESRD, % | <0.001 | ||||
| Diabetes | 40.7 | 44.8 | 48.4 | 39.4 | |
| GN | 4.1 | 5.7 | 4.5 | 3.8 | |
| Hypertension | 36.4 | 37.3 | 37 | 36.1 | |
| Cystic disease | 0.9 | 2.1 | 1.4 | 0.6 | |
| Other | 18 | 10.1 | 8.6 | 20.2 |
Continuous variables are presented as mean (SD), and categorical variables are presented as the percent of total. P values are based on ANOVA test. Nonsignificant P value supports the null hypothesis stating that all group means are equal to each other.
There was a significant association between duration of care and type of initial predialysis vascular access (P<0.001). Of those patients who had a fistula or graft as their first vascular access placed, 45.7% and 42.8%, respectively, were seen by a nephrologist for more than 1 year before initiating HD compared with only 16.5% with a catheter as first HD access. Conversely, only 5.6% and 6.7%, respectively, of those patients with a fistula or graft as first access, compared with 38.1% of those patients with a catheter, had no predialysis nephrology care provided.
Survival Analysis
Entire Study Population
The proportional hazards models were adjusted for potential confounding factors as listed above, with the AVF group used as the reference in the analyses. In the entire study population, a catheter as an initial predialysis access was associated with worse mortality compared with an AVF (hazard ratio [HR]=1.77, 95% confidence interval [CI]=1.73 to 1.81; P<0.001), which is shown in Table 2. However, having an AVG as the initial predialysis access did not show statistically significant mortality difference compared with an AVF (HR=1.05, 95% CI=1.00 to 1.11; P=0.06).
Table 2.
The association of first dialysis access placed with patient mortality from the time of HD initiation in the entire study population and subgroups by Cox proportional hazards model
| Variable | Outcome: Patient Mortality after ESRD (HD Initiation) | |||
|---|---|---|---|---|
| Access Type: Graft | Access Type: Catheter | |||
| Hazard Ratio (95% CI) | P | Hazard Ratio (95% CI) | P | |
| Entire study population | 1.05 (1.00–1.11) | 0.06 | 1.77 (1.73–1.81) | <0.001 |
| Age categories, yr | ||||
| 67–79 | 1.10 (1.02–1.17) | 0.007 | 1.78 (1.73–1.84) | <0.001 |
| 80–89 | 0.98 (0.89–1.08) | 0.67 | 1.74 (1.67–1.81) | <0.001 |
| ≥90 | 1.09 (0.74–1.60) | 0.67 | 1.78 (1.52–2.09) | <0.001 |
| Race | ||||
| White | 1.06 (1.00–1.13) | 0.06 | 1.75 (1.71–1.80) | <0.001 |
| African American | 1.05 (0.94–1.17) | 0.37 | 1.84 (1.73–1.95) | <0.001 |
| Native American | 1.29 (0.66–2.53) | 0.46 | 1.70 (1.27–2.29) | 0.004 |
| Asian | 1.30 (0.96–1.76) | 0.09 | 1.91 (1.64–2.23) | <0.001 |
| Other | 1.25 (0.21–7.53) | 0.80 | 2.12 (0.57–7.9) | 0.26 |
| Sex | ||||
| Woman | 1.02 (0.94–1.10) | 0.68 | 1.73 (1.67–1.80) | <0.001 |
| Man | 1.09 (1.01–1.18) | 0.03 | 1.79 (1.74–1.85) | <0.001 |
| History of diabetes | ||||
| Yes | 1.07 (0.99–1.14) | 0.07 | 1.75 (1.69–1.80) | <0.001 |
| No | 1.04 (0.95–1.13) | 0.40 | 1.79 (1.73–1.86) | <0.001 |
| History of malignancy | ||||
| Yes | 1.19 (1.01–1.39) | 0.03 | 1.88 (1.75–2.01) | <0.001 |
| No | 1.04 (0.98–1.10) | 0.25 | 1.74 (1.70–1.79) | <0.001 |
| History of PVD | ||||
| Yes | 1.07 (0.95–1.20) | 0.26 | 1.64 (1.56–1.72) | <0.001 |
| No | 1.05 (0.99–1.12) | 0.12 | 1.80 (1.76–1.85) | <0.001 |
| Duration of pre-ESRD nephrology care | ||||
| No care | 1.16 (0.96–1.41) | 0.12 | 1.71 (1.57–1.86) | <0.001 |
| Less than 6 months | 1.08 (0.93–1.26) | 0.32 | 1.82 (1.71–1.94) | <0.001 |
| 6–12 months | 1.01 (0.92–1.12) | 0.82 | 1.79 (1.71–1.86) | <0.001 |
| More than 12 months | 1.06 (0.98–1.16) | 0.15 | 1.77 (1.70–1.84) | <0.001 |
Fistula group was used as reference. The results shown are derived from 20 separate proportional hazard models; each of the models was adjusted for the following covariates: age at ESRD onset, race, sex, BMI, comorbidity index, type of access first placed, primary cause of ESRD, and duration of pre-ESRD nephrology care. 95% CI, 95% confidence interval.
Age Subgroups
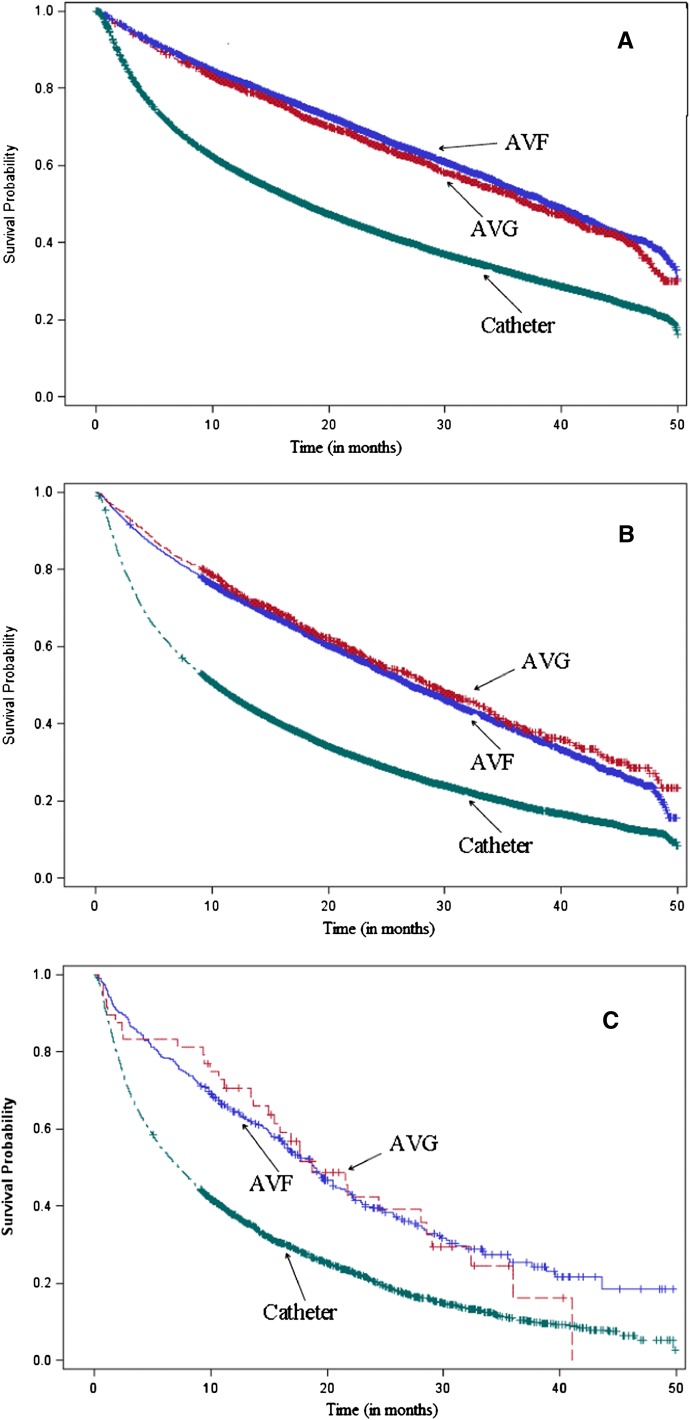
Because our primary aim was to assess if fistula first is the optimal strategy in octogenarians and given the lack of a significant association comparing the AVF group with the AVG group in the entire study population, we stratified the study cohort by age into three groups: 67–79, 80–89 (octogenarian group), and ≥90 years (nonagenarian group). All age groups showed significantly increased HRs associated with the use of a catheter compared with an AVF (HR=1.78, 95% CI=1.73 to 1.84; HR=1.74, 95% CI=1.67 to 1.81; and HR=1.78, 95% CI=1.52 to 2.09, respectively, for each age group; P<0.001 for each). However, compared with the entire study population, the association between AVG and mortality was different in different age groups. Patients in the 67–79 group did show a statistically significant mortality benefit associated with an AVF first placed predialysis compared with an AVG (HR=1.10, 95% CI=1.02 to 1.17; P=0.007). However, both octogenarian and nonagenarian groups did not show statistical differences if an AVG was placed first predialysis compared with an AVF placed first predialysis (HR=0.98, 95% CI=0.89 to 1.08; P=0.67 and HR=1.09, 95% CI=0.74 to 1.60 P=0.67, respectively) (Figure 1 and Table 2).
Figure 1.
Kaplan–Meier survival curves by age groups. (A) Survival curve: 67- to 79-years age group. (B) Survival curve: 80- to 89-years age group (octogenarians). (C) Survival curve: ≥90-years age group. Note that there was a statistically significant difference between AVF and AVG in the 67–79 group but a nonsignificant difference in the 80–89 group.
Age and Comorbidity Subgroups
Analysis was further stratified by individual comorbidities (i.e., diabetes, malignancy, and peripheral vascular disease [PVD] in each of the age groups) (Table 3). Comparing a catheter placed first with an AVF placed first predialysis, mortality outcomes were significantly worse in all age groups independent of the comorbidity. Comparing an AVG placed first with an AVF placed first predialysis by specific comorbidity, patients in the 67–79 group did not show statistically significant differences to patients with a history of malignancy or PVD, but a significant advantage of AVF in patients with diabetes mellitus was shown (HR=1.10, 95% CI=1.01 to 1.20; P=0.02). Comparing placing an AVG first with an AVF first in the octogenarian group, all comorbidity groups did not show a significant difference in survival, with the exception that history of malignancy was associated with a survival advantage in those patients with an AVF placed first (HR=1.31, 95% CI=1.02 to 1.67; P=0.03). Whether these subgroup differences represent a selection of patients having an AVF placed first because of a suspected better prognosis cannot be assessed by this study.
Table 3.
The association of first dialysis access placed with patient mortality from the time of ESRD for the comorbidities of malignancy, diabetes, and PVD in age-specific population subgroups by proportional hazards model
| Risk Group | Outcome: Patient Mortality after ESRD (HD Initiation) | |||
|---|---|---|---|---|
| Access Type: Graft | Access Type: Catheter | |||
| Hazard Ratio (95% CI) | P | Hazard Ratio (95% CI) | P | |
| 67–79 yr (n=74,997) | ||||
| History of malignancy | 1.12 (0.91–1.38) | 0.27 | 1.87 (1.71–2.05) | <0.001 |
| No history of malignancy | 1.09 (1.02–1.18) | 0.01 | 1.78 (1.72–1.83) | <0.001 |
| History of diabetes | 1.10 (1.01–1.20) | 0.02 | 1.78 (1.71–1.85) | <0.001 |
| No history of diabetes | 1.09 (0.97–1.23) | 0.14 | 1.81 (1.72–1.91) | <0.001 |
| History of PVD | 1.12 (0.97–1.29) | 0.12 | 1.66 (1.56–1.77) | <0.001 |
| No history of PVD | 1.09 (1.01–1.18) | 0.03 | 1.83 (1.77–1.89) | <0.001 |
| 80–89 yr (n=37,149) | ||||
| History of malignancy | 1.31 (1.02–1.67) | 0.03 | 1.90 (1.70–2.13) | <0.001 |
| No history of malignancy | 0.94 (0.85–1.03) | 0.19 | 1.68 (1.61–1.76) | <0.001 |
| History of diabetes | 0.98 (0.85–1.12) | 0.74 | 1.68 (1.58–1.78) | <0.001 |
| No history of diabetes | 0.98 (0.86–1.11) | 0.72 | 1.76 (1.67–1.85) | <0.001 |
| History of PVD | 0.97 (0.79–1.20) | 0.77 | 1.59 (1.45–1.73) | <0.001 |
| No history of PVD | 0.98 (0.88–1.09) | 0.69 | 1.76 (1.68–1.84) | <0.001 |
| ≥90 yr (n=3279) | ||||
| History of malignancy | 1.40 (0.31–6.44) | 0.66 | 1.65 (1.07–2.55) | 0.02 |
| No history of malignancy | 1.03 (0.69–1.55) | 0.87 | 1.77 (1.49–2.10) | <0.001 |
| History of diabetes | 1.09 (0.58–2.02) | 0.79 | 1.51 (1.10–2.07) | 0.01 |
| No history of diabetes | 1.04 (0.63–1.73) | 0.86 | 1.86 (1.55–2.24) | <0.001 |
| History of PVD | 1.27 (0.30–5.42) | 0.74 | 1.63 (1.08–2.47) | 0.02 |
| No history of PVD | 1.10 (0.74–1.65) | 0.63 | 1.80 (1.51–2.13) | <0.001 |
Fistula group was used as the reference. The Cox models were adjusted for age at ESRD onset, race, sex, BMI, comorbidity index, type of first access placed, duration of pre-ESRD nephrology care, and primary cause of ESRD. 95% CI, 95% confidence interval.
Vascular Access Conversions before HD Initiation
Of 115,425 patients in the study population, 21,436 had an AVF placed as their first predialysis access; however, only 50.7% of them initiated dialysis with an AVF, whereas 43.4% initiated dialysis with a catheter and 5.9% initiated dialysis with an AVG. Of 3472 patients who had an AVG placed as their first access, only 25.4% initiated HD with a catheter. Of 37,149 octogenarians, 6198 had an AVF placed as their first predialysis access, of which 43.2% used a catheter at the time of dialysis initiation. In contrast, of 1010 octogenarians who had an AVG placed as their first access, only 24.4% had converted to a catheter at the time of dialysis initiation.
Discussion
To our knowledge, this study is the first large population-based study in the elderly evaluating survival outcomes associated with the vascular access first placed in the predialysis period (access first placed as opposed to the type of access first used for HD, which has been studied previously). Placing an AVF first had favorable, although statistically nonsignificant, survival outcomes compared with placing an AVG first in the entire study cohort. Whereas those patients in the 67–79 group benefited from predialysis placement of an AVF first compared with an AVG, survival outcomes were found to be equivalent in the octogenarians and nonagenarians. However, a catheter placed as first access was found to be the clearly inferior option in all groups. Of those patients with a catheter placed first, many more (38.1%) had no predialysis nephrology care compared with those patients with an AVF or AVG placed first (only 5.6% and 6.7%, respectively), a factor reported to be associated with poor outcomes.12
Prior literature based on the access first used in the elderly had almost uniformly reported AVF as the superior access.5,6,13 This finding includes outcomes specific to octogenarians. In a study of recent incident octogenarian HD patients (n=29,839), those patients initiating HD with an AVF showed a relative survival benefit of 45%, and those patients initiating HD with an AVG showed a relative survival benefit of 26% compared with catheters.6 However, all these outcomes were based on access first used as opposed to access first placed. This information introduces significant selection bias and may not reflect the first predialysis vascular access planned, which is the aim of the Fistula First Initiative. Our data showed that, of 21,436 patients who had an AVF as their first access placed, only 50.7% actually used an AVF at the time of dialysis initiation, whereas 100% by definition attempted Fistula First.
Our finding that octogenarians and nonagenarians have similar survival outcomes whether an AVF or AVG is placed first predialysis may be explained by the greater number of patients eventually initiating HD with a catheter because of unsuccessful or delayed maturation of AVFs in the elderly. In the octogenarian group, the likelihood that patients initiated dialysis with a catheter was 77% greater if an AVF had been placed first rather than an AVG. In prior studies, access conversions of AVFs or AVGs to catheters have been found to adversely affect mortality, increasing it by 81%.14 Furthermore, placing an AVG predialysis compared with postdialysis is associated with less catheter dependence and decreased frequency of catheter-related bacteremia.15
In addition, the competing risk of death in octogenarians is higher and may minimize potential long-term benefits of placing an AVF over an AVG. It has been reported that the 1-year survival of those patients >75 years old on HD is 53.5%, whereas at 5 years, it is as low as 2.4%.16,17
Overall, our data suggest that fistula first is not the clearly superior strategy in the elderly population, particularly for octogenarians and nonagenarians. However, our data support the notion that placing a catheter first does seem to be the associated inferior strategy. Therefore, the question remains if placing an AVG versus an AVF is the best predialysis vascular access strategy in the elderly population. There are several implications based on these two different strategies. First, in the CKD stage IV elderly population, the rate of decline in renal function and the time of dialysis initiation are often less predictable. It had been described recently by Vachharajani et al.18 in a single center study that 30.6% of CKD octogenarians died of nonrenal causes before needing dialysis. Recent prospective and observational studies showed that, compared with current initiation practice, a delay in the timing of dialysis initiation is not associated with worse outcomes.19,20 Using this time to plan and create a fistula or graft seems prudent. Finally, as noted here, vascular access failure rate is higher in the elderly; our study showed that only 50.7% of those patients with an AVF first placed used an AVF at the time of HD initiation and that a higher percentage of those patients within the AVF first group used catheters at dialysis initiation compared with the AVG first group (43% versus 25%). Future investigation should be directed to the complications and vascular procedures required using the different strategies as well as patient preferences and cost-effectiveness.
Overall, there currently exists some controversy between advocates of fistula first and catheter last.21,22 We are presenting data here to support a competing strategy of AVG first in many octogenarians when individual characteristics, such as uncertain prognosis for survival, poor vasculature, or variable rate of progression to ESRD, may make this option preferable to the nephrologist.
There are certain limitations to our study. Survival bias by definition exists in our study by using the US Renal Data System (USRDS), because to be entered in the USRDS data system, one must survive to the time of initiation of renal replacement therapy. The higher chance of dying predialysis with an AVF over an AVG, because AVFs are usually placed farther in advance of HD than AVGs, might further favor the AVF group that has survived to the time of HD initiation and entered into our study. In our study population, 41.8% did not have a nephrologist involved until less than 6 months before starting dialysis, a factor that has practical implications in planning for future dialysis and having the time needed to arrange for vascular access. In addition, the role of shorter duration of predialysis nephrology care might have predisposing factors, such as education levels and medical adherence, which we cannot analyze but may affect the type of patient who receives an AVF first. Also, we were limited to the available data in USRDS/Medicare claims, which does not allow us to distinguish the type of fistula placed, obviating any comparison of the outcomes between first placing, for instance, a brachiocephalic versus a radiocephalic fistula compared with an AVG. Because our comorbidity data were derived from Centers for Medicare and Medicaid Services (CMS) Form 2728, there is a potential that misreporting or underreporting of comorbidities might affect our analysis. Finally, given the retrospective and observational nature of our study, there is a potential for selection bias by the physician or the patient; therefore, healthier patients may be more likely to be considered for an AVF rather than an AVG or a catheter. However, this bias would favor a better outcome in AVF group, and therefore, our findings of similar survival outcomes, regardless of an AVF or AVG first placed, supports AVG first as an alternate vascular access strategy in the elderly.
The strengths of this study are the large sample size and overall accuracy of the data. Our primary outcome of all-cause mortality is captured accurately from USRDS data, with minimal loss of follow-up, along with use of Medicare claims to help identify our primary variables of interest.
In conclusion, a fistula first strategy may not apply to octogenarians, with an AVG being an acceptable alternative. However, catheters remain the worst access to be placed initially, supporting a catheter last strategy. These observational data suggest that placing an AVG first decreases the chance of initiating HD with a catheter compared with AVF first. In the elderly, fistula first should be used in patients who have a high chance for a successful fistula, and the remainder of patients should be considered for a graft first before HD initiation.
Concise Methods
Data Sources
We used USRDS linked with Medicare claims data to identify our retrospective cohort of interest. Medicare claims searched by Common Procedural Terminology (CPT-4) codes for vascular access were used to identify the first predialysis vascular access placed. The USRDS dataset provided patients’ clinical data to describe baseline characteristics (derived from CMS Form 2728), the vascular access actually used at HD initiation, exact times of death, and dates of transplantation. This study included incident HD patients ≥67 years old from January 1, 2005 to December 31, 2008 with confirmed first predialysis access placed. We used the minimum age of 67 years, because we combined Medicare data from 2003 to make all study patients potentially Medicare eligible 2 years preceding dialysis initiation.
Study Population
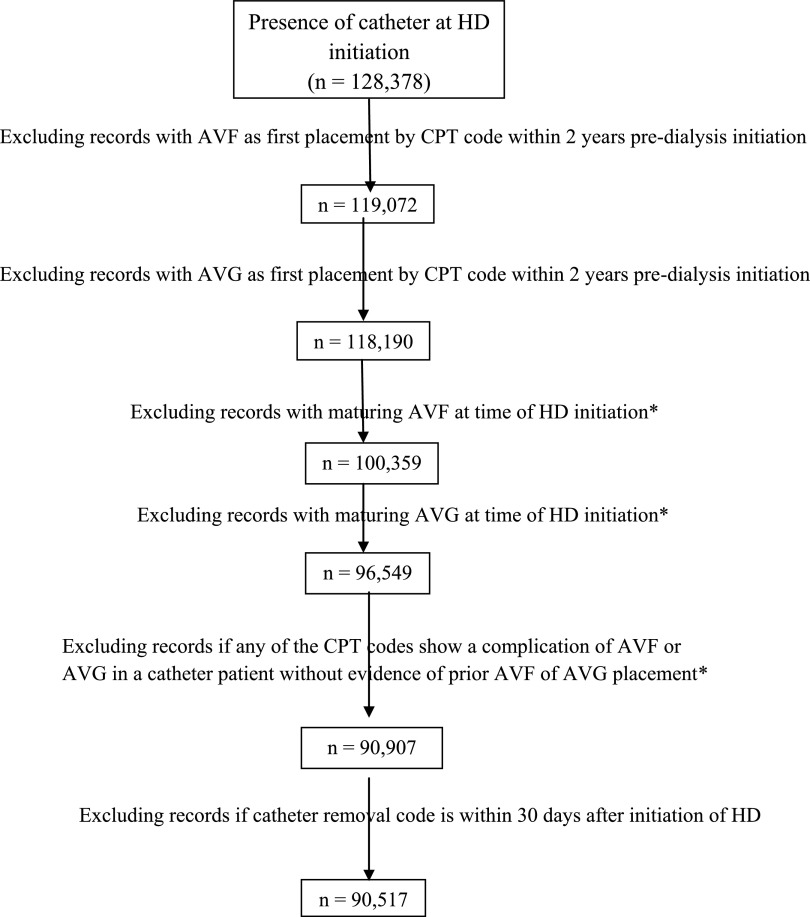
The final study population was assembled based on identifying the initially placed HD access: AVF, AVG, or catheter. We identified our AVF group as those patients who had their first predialysis vascular access CPT-4 claim for AVF creation (36818, 36819, 36820, 36825, and 36821). Similarly, we identified our AVG group as those patients who had their first predialysis CPT-4 claim for AVG creation (36830). Because the CPT-4 codes for tunneled dialysis catheter placement were less reliable, we derived our catheter group using data from both the USRDS and the Medicare CPT-4 claims as depicted in Figure 2. The definition of the catheter group was based on the assumption that catheters would be placed shortly before the time of HD initiation, and those catheters would be considered as the first access placed if no evidence of a prior AVF or AVG placement was identified. In the catheter cohort, to identify only the ESRD population (rather than those patients with AKI who recovered renal function), we excluded those patients with a catheter removal CPT-4 code <30 days from the date of HD initiation who did not have a prior AVF or AVG placement. The final study population consisted of incident HD patients divided into three groups based on their first vascular access placed in the 2-year predialysis period.
Figure 2.
Catheter cohort derivation flow diagram. *These patients were excluded from the entire study, because it could not be ascertained by CPT codes predialysis when the AVF or AVG (listed as maturing on Form 2728 at HD initiation) was placed as a primary access by intention to treat.
Primary Outcome
All-cause mortality (time to death) was the primary outcome of interest. Because the time between vascular placement and dialysis initiation varies, to avoid lead time bias, we measured time to death from the date of HD initiation. Patients who received a renal transplant after HD initiation were censored from the analysis at the time of renal transplantation.
Statistical Analyses
The baseline characteristics and demographic data of our population were tabulated by the first predialysis vascular access placed. Summary statistics are presented as percentages for categorical data and mean (±SD) for continuous variables. Differences in baseline characteristics between the groups were tested using the chi-squared test for categorical variables and one-way ANOVA for continuous variables. We examined the relationship of first access placed (AVF, AVG, or catheter) to mortality. Cox proportional hazards models were used to evaluate these relationships adjusted for covariates. We did not find any evidence for violation of proportional hazards assumption. We included the following covariates in the multivariate analysis: age at HD initiation, sex, race, comorbidity index (described below and includes history of diabetes), body mass index (BMI), cause of ESRD, and duration of nephrology care.12,23–26 Clinical information at the time of dialysis initiation was derived from the CMS Form 2728.
To adjust for patient comorbidities, we formed a comorbidity coefficient similar to the Charlson comorbidity index. Each of the comorbid conditions available in the dataset contributed one point to the composite index, with additional points given for older age as described elsewhere.27 We previously used similar approaches to describe comorbidities using abbreviated Davies28 and Charlson29 comorbidity indices by including information available in the USRDS dataset. These abbreviated indices were validated in the past by strong association with clinical outcomes.30,31
The association between initial vascular access placed and mortality was analyzed in the entire study population as well as subgroups based on age, race, sex, and comorbidity index, with a focus on age subgroups to highlight outcomes specific to octogenarians. We further analyzed subgroups divided by specific comorbidities (i.e., diabetes, malignancy, and PVD) to evaluate if potential effect of the vascular access would be influenced by comorbidity.6,32 All analyses were performed with SAS software version 9.2 (SAS Institute, Cary, NC).
Disclosures
None.
Acknowledgments
The study was fully funded from departmental funds.
The data reported here have been supplied by the US Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Vascular Access for Hemodialysis in Older Adults: A “Patient First” Approach,” on pages 1187–1190.
References
- 1.NKF-K/DOQI : III. NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: Update 2000. Am J Kidney Dis 37[Suppl 1]: S137–S181, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Lok CE: Fistula first initiative: Advantages and pitfalls. Clin J Am Soc Nephrol 2: 1043–1053, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Allon M: Current management of vascular access. Clin J Am Soc Nephrol 2: 786–800, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Lacson E, Jr, Lazarus JM, Himmelfarb J, Ikizler TA, Hakim RM: Balancing fistula first with catheters last. Am J Kidney Dis 50: 379–395, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Xue JL, Dahl D, Ebben JP, Collins AJ: The association of initial hemodialysis access type with mortality outcomes in elderly Medicare ESRD patients. Am J Kidney Dis 42: 1013–1019, 2003 [DOI] [PubMed] [Google Scholar]
- 6.DeSilva RN, Sandhu GS, Garg J, Goldfarb-Rumyantzev AS: Association between initial type of hemodialysis access used in the elderly and mortality. Hemodial Int 16: 233–241, 2012 [DOI] [PubMed] [Google Scholar]
- 7.O’Hare AM, Choi AI, Bertenthal D, Bacchetti P, Garg AX, Kaufman JS, Walter LC, Mehta KM, Steinman MA, Allon M, McClellan WM, Landefeld CS: Age affects outcomes in chronic kidney disease. J Am Soc Nephrol 18: 2758–2765, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Allon M, Robbin ML: Increasing arteriovenous fistulas in hemodialysis patients: Problems and solutions. Kidney Int 62: 1109–1124, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D: Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I). J Am Soc Nephrol 17: 3204–3212, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Lacson E, Jr, Wang W, Lazarus JM, Hakim RM: Change in vascular access and mortality in maintenance hemodialysis patients. Am J Kidney Dis 54: 912–921, 2009 [DOI] [PubMed] [Google Scholar]
- 11.US Renal Data System: USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 12.Bradbury BD, Fissell RB, Albert JM, Anthony MS, Critchlow CW, Pisoni RL, Port FK, Gillespie BW: Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol 2: 89–99, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Ekbal NJ, Swift PA, Chalisey A, Steele M, Makanjuola D, Chemla E: Hemodialysis access-related survival and morbidity in an elderly population in South West Thames, UK. Hemodial Int 12[Suppl 2]: S15–S19, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Bradbury BD, Chen F, Furniss A, Pisoni RL, Keen M, Mapes D, Krishnan M: Conversion of vascular access type among incident hemodialysis patients: Description and association with mortality. Am J Kidney Dis 53: 804–814, 2009 [DOI] [PubMed] [Google Scholar]
- 15.Shingarev R, Maya ID, Barker-Finkel J, Allon M: Arteriovenous graft placement in predialysis patients: A potential catheter-sparing strategy. Am J Kidney Dis 58: 243–247, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurella M, Covinsky KE, Collins AJ, Chertow GM: Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 146: 177–183, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Munshi SK, Vijayakumar N, Taub NA, Bhullar H, Lo TC, Warwick G: Outcome of renal replacement therapy in the very elderly. Nephrol Dial Transplant 16: 128–133, 2001 [DOI] [PubMed] [Google Scholar]
- 18.Vachharajani TJ, Moossavi S, Jordan JR, Vachharajani V, Freedman BI, Burkart JM: Re-evaluating the fistula first initiative in octogenarians on hemodialysis. Clin J Am Soc Nephrol 6: 1663–1667, 2011 [DOI] [PubMed] [Google Scholar]
- 19.Cooper BA, Branley P, Bulfone L, Collins JF, Craig JC, Fraenkel MB, Harris A, Johnson DW, Kesselhut J, Li JJ, Luxton G, Pilmore A, Tiller DJ, Harris DC, Pollock CA, IDEAL Study : A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med 363: 609–619, 2010 [DOI] [PubMed] [Google Scholar]
- 20.Wright S, Klausner D, Baird B, Williams ME, Steinman T, Tang H, Ragasa R, Goldfarb-Rumyantzev AS: Timing of dialysis initiation and survival in ESRD. Clin J Am Soc Nephrol 5: 1828–1835, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sales CM, Schmidt RJ: Fistula First clarifies definition of preferred access. Nephrol News Issues 24: 54–57, 2010 [PubMed] [Google Scholar]
- 22.Vassalotti JA, Jennings WC, Beathard GA, Neumann M, Caponi S, Fox CH, Spergel LM, Fistula First Breakthrough Initiative Community Education Committee : Fistula first breakthrough initiative: Targeting catheter last in fistula first. Semin Dial 25: 303–310, 2012 [DOI] [PubMed] [Google Scholar]
- 23.Stehman-Breen CO, Sherrard DJ, Gillen D, Caps M: Determinants of type and timing of initial permanent hemodialysis vascular access. Kidney Int 57: 639–645, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, Coresh J: Timing of nephrologist referral and arteriovenous access use: The CHOICE Study. Am J Kidney Dis 38: 494–501, 2001 [DOI] [PubMed] [Google Scholar]
- 25.Avorn J, Winkelmayer WC, Bohn RL, Levin R, Glynn RJ, Levy E, Owen W, Jr: Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J Clin Epidemiol 55: 711–716, 2002 [DOI] [PubMed] [Google Scholar]
- 26.Hasegawa T, Bragg-Gresham JL, Yamazaki S, Fukuhara S, Akizawa T, Kleophas W, Greenwood R, Pisoni RL: Greater first-year survival on hemodialysis in facilities in which patients are provided earlier and more frequent pre-nephrology visits. Clin J Am Soc Nephrol 4: 595–602, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gueye AS, Baird BC, Shihab F, Koford JK, Barenbaum AL, Leviatov A, Goldfarb-Rumyantzev AS: The role of the economic environment in kidney transplant outcomes. Clin Transplant 23: 643–652, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Davies SJ, Russell L, Bryan J, Phillips L, Russell GI: Comorbidity, urea kinetics, and appetite in continuous ambulatory peritoneal dialysis patients: Their interrelationship and prediction of survival. Am J Kidney Dis 26: 353–361, 1995 [DOI] [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 30.Goldfarb-Rumyantzev A, Hurdle JF, Scandling J, Wang Z, Baird B, Barenbaum L, Cheung AK: Duration of end-stage renal disease and kidney transplant outcome. Nephrol Dial Transplant 20: 167–175, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Tang H, Chelamcharla M, Baird BC, Shihab FS, Koford JK, Goldfarb-Rumyantzev AS: Factors affecting kidney-transplant outcome in recipients with lupus nephritis. Clin Transplant 22: 263–272, 2008 [DOI] [PubMed] [Google Scholar]
- 32.Xi W, MacNab J, Lok CE, Lee TC, Maya ID, Mokrzycki MH, Moist LM: Who should be referred for a fistula? A survey of nephrologists. Nephrol Dial Transplant 25: 2644–2651, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]