Abstract
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) has a higher diagnostic accuracy for pancreatic cancer than other techniques. This article will review the current advances and considerations for optimizing diagnostic yield for EUS-guided sampling of solid pancreatic lesions. Preprocedural considerations include patient history, confirmation of appropriate indication, review of imaging, method of sedation, experience required by the endoscopist, and access to rapid on-site cytologic evaluation. New EUS imaging techniques that may assist with differential diagnoses include contrast-enhanced harmonic EUS, EUS elastography, and EUS spectrum analysis. FNA techniques vary, and multiple FNA needles are now commercially available; however, neither techniques nor available FNA needles have been definitively compared. The need for suction depends on the lesion, and the need for a stylet is equivocal. No definitive endosonographic finding can predict the optimal number of passes for diagnostic yield. Preparation of good smears and communication with the cytopathologist are essential to optimize yield.
Keywords: Endoscopic ultrasound—guided fine-needle aspiration, fine-needle biopsy, pancreatic lesions
Endoscopic ultrasound—guided fine-needle aspiration (EUS-FNA) has evolved into a first-line procedure for the diagnosis of solid pancreatic lesions. The differential diagnosis for solid pancreatic masses is broad and includes both malignant and benign causes (Table 1). Primary pancreatic ductal adenocarcinoma is the most common cause, accounting for at least 85% of solid pancreatic masses. It is currently the fourth leading cause of cancer death in the United States.1,2 In 2011, there were 44,030 new cases of pancreatic cancer, and 37,660 deaths were attributed to pancreatic cancer.2
Table 1.
Differential Diagnosis of Malignant and Benign Solid Pancreatic Lesions
| Malignant tumors |
| Primary pancreatic ductal adenocarcinoma (>85%) |
| Secondary metastatic tumors |
| Lung |
| Breast |
| Renal |
| Prostate |
| Melanoma |
| Gastrointestinal tract carcinoma (eg, esophageal, gastric, ampullary, and colorectal) |
| Osteosarcoma |
| Neuroendocrine tumors |
| Lymphoma |
| Solid pseudopapillary tumors |
| Pancreatic acinar cell carcinoma |
| Malignant cystic lesions with solid components (mucinous cystadenoma or intraductal papillary mucinous neoplasm) |
| Benign tumors and pseudotumors |
| Focal pancreatitis and chronic pancreatitis |
| Autoimmune pancreatitis |
| Microcystic serous cystadenoma |
| Other masquerading lesions, such as splenule |
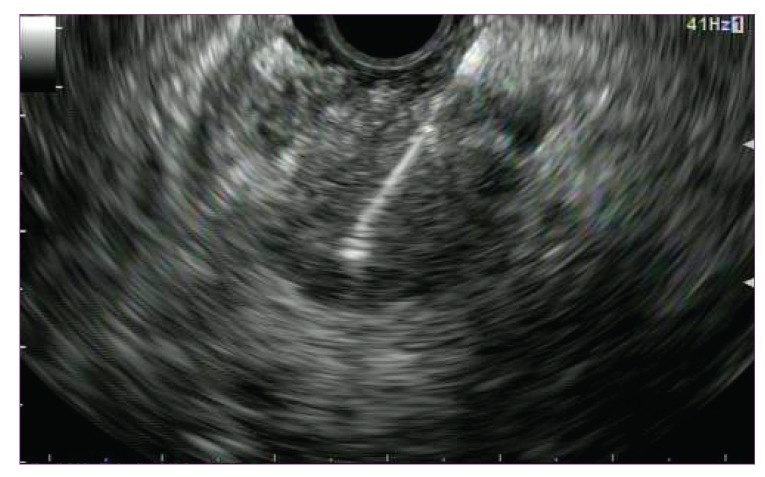
EUS-FNA enables the acquisition of representative material for cytopathologic evaluation of the pancreas in most cases (Figure 1). A recent large meta-analysis of 33 published studies (12 retrospective and 21 prospective) between 1997 and 2009 involving 4,984 patients demonstrated that EUS-FNA has a pooled sensitivity for malignant cytology of 85—91%, specificity of 94—98%, positive predictive value of 98—99%, and negative predictive value of 65—72%, depending on whether atypical or suspicious results were included.3
Figure 1.
Endoscopic ultrasound—guided fine-needle aspiration of a pancreatic mass.
EUS-FNA has a higher diagnostic accuracy for pancreatic cancer than alternate techniques such as percutaneous computed tomography (CT) or transabdominal ultrasound—guided approaches, especially for lesions less than 3 cm.4-15 Nonetheless, the diagnostic yield of EUS-FNA may be limited for a variety of reasons. These include the nature and location of the lesion, the presence of necrosis or inflammation, the visualization of the lesion, needle size, the stylet used, suction, FNA technique, the experience of the endoscopist and cytologist, the presence (or absence) of rapid on-site cytologic evaluation (ROSE), and cytology processing sampling. False-negative results for malignancy may occur in up to 20—40% of cases.16,17 Repeat EUS-FNA is recommended as the second-line test in patients in whom there is a strong clinical suspicion of malignancy but a nondiagnostic finding on initial examination.17-20 Recent enhancements in imaging and sampling may improve the efficacy and efficiency of pancreatic EUS-FNA.
Preprocedural Considerations
Several preprocedural considerations are important to optimize the success of EUS-FNA of solid pancreatic lesions.
Patient History
A careful history in the patient who presents with a pancreatic mass may provide useful information regarding a likely diagnosis. The insidious onset of symptoms, such as jaundice and/or unexplained weight loss in the presence of a new pancreatic mass, may strongly suggest an underlying malignant diagnosis. The finding of an elevated serum carbohydrate antigen 19-9 (CA19-9) level may increase the pretest probability of an underlying pancreatic adenocarci-noma, although the CA19-9 level can be modestly elevated in bile duct obstruction or can be normal in the presence of pancreatic cancer.21 A history of chronic pancreatitis, an immune disorder, or a personal or family history of malignancy or other risk factors may provide clues to an underlying cause. The time interval between the diagnosis of a primary carcinoma and subsequent pancreatic metas-tases is variable and may be years. However, incidental or asymptomatic presentation is not uncommon. Therefore, a comprehensive working differential diagnosis for all cases needs to be considered. Techniques for FNA may be modified according to suspicion of a certain diagnosis.
Indication
The success of any procedure begins with an appropriate indication. In general, FNA is considered when results will affect management. Suspected malignant lesions that are potentially resectable (only 15—20%) may not require FNA if results will not change management. Exceptions to this include cases in which neoadjuvant therapy is being considered or to exclude the presence of a possible pseudotumor that would not benefit from surgery.1 EUS alone may still be of benefit for locoregional staging in borderline resectable cases and in detecting unsuspected metastasis, which can occur in up to 10% of patients.22,23
Review of Imaging
Review of imaging prior to the procedure can be critical to successful EUS-FNA and provide a roadmap for identifying a lesion. A dedicated contrast-enhanced pancreatic protocol CT study or magnetic resonance imaging is ideal when available. Most pancreatic adenocarcinomas are hypoechoic relative to the surrounding parenchyma. Highly vascular lesions that are enhanced on CT may be suggestive of lesions such as neuroendocrine or renal cell carcinoma metastasis. Some lesions, especially in the setting of acute or chronic pancreatitis, may not be well defined or seen on CT imaging (up to 34% in one study24). Cystic lesions, especially when complex or microcystic, may appear solid. Surrounding anatomy—such as atrophic parenchymal changes, abrupt cutoff of a dilated main pancreatic or common bile duct, or invasion of locoregional vascular structures—may tip off the presence of an occult mass. Evidence of metastasis should also be investigated.
Sedation
Adequate sedation for EUS-FNA of the pancreas is important because these procedures are typically longer than standard endoscopy procedures. Sedation is usually provided with conscious sedation or with monitored anesthesia care/ total intravenous anesthesia. Propofol may be preferred for these cases because the length of the procedure may be unpredictable for a variety of reasons, especially if a lesion is difficult to find or diagnose. Intraprocedural cytologic assessment may contribute to longer procedure times in this setting. Furthermore, a poorly sedated patient may be predisposed to an increased and unnecessary risk of complications with FNA or to having nondiagnostic results.
Endoscopist Experience
Although a number of factors may affect diagnostic accuracy, the experience of the endoscopist is likely significant. Diagnostic yield may vary significantly among endosonographers. A multicenter retrospective review of 1,075 patients suggested that the diagnostic yield of malignancy in solid pancreatic masses could be used as a benchmark for quality performance measurement, given its high pretest probability; a final cytologic diagnosis of malignancy was made in 71% of solid pancreatic masses, and it was suggested that endoscopists with a diagnostic rate of less than 52% likely need performance reassess-ment.25 Guidelines for EUS credentialing have been published, although there is likely substantial individual variation in the learning curve to perform EUS of the pancreas.26,27 Diagnostic accuracy of EUS-FNA for pancreatic masses has been shown to increase with experience after a minimum of 75—100 cases for interpretative competence and 25—50 cases for FNA.26-31 Nonetheless, it is reasonable to assume that endoscopists performing a high volume of FNAs are likely to have more success because the procedure is highly operator-dependent with significant interoperator variability.
The importance of an experienced cytopathologist also should not be underestimated because a small possibility of a false-positive result does exist.32-34 EUS-FNA of solid pancreatic lesions has otherwise been demonstrated to be a safe procedure, with an overall complication rate of about 2.5%, which includes a 1—2% risk of pancreatitis.35-37 The risk of tumor seeding is thought to be very low and has been limited to a few case reports.38-40 The risk is lower than that for percutaneous biopsy.41 The importance of tumor seeding is also likely limited to a few exceptional circumstances, most notably FNA of potentially resect-able lesions in the distal body and tail of the pancreas that may result in gastric wall seeding. Detailed discussion of the risks of seeding and the pros and cons of pursuing EUS-FNA and fine-needle biopsy (FNB) of resectable solid pancreatic masses is beyond the scope of this paper and has been discussed by the authors elsewhere.12
Rapid On-Site Cytologic Evaluation
ROSE has been demonstrated to improve the overall diagnostic sensitivity and accuracy of FNA of solid pancreatic masses by up to 10—15%.42 Intraprocedural feedback on the adequacy of sampling and the potential need for additional material for ancillary studies (ie, immuno-histochemistry or flow cytometry for lymphoma) may have a significant clinical impact.42-47 Reliability of gross visual assessment for tissue specimen adequacy by either an endosonographer or a cytotechnician has been shown to be inferior to assessment by a cytopathologist; however, if no cytopathologist is available, assessment should be attempted by the endosonographer.48-50
ROSE is not available in many centers because of increased expense and resources. However, it may provide more optimal patient care and ultimately be cost-effective by reducing the need for repeat or alternate procedures.51 It may also reduce procedure time and risk by minimizing the total number of needle passes. It is often still practical and more efficient to take 2—3 passes before asking a pathologist to review the findings.52 Direct communication with a cytopathologist during the evaluation is strongly encouraged to facilitate the interpretation of findings.
Optimal Techniques for Endoscopic Ultrasound Imaging of Solid Pancreatic Lesions
Locating the lesion is the first priority. Approximately 65% of pancreatic cancers occur in the pancreatic head.53 Lesions in the pancreatic head or its uncinate region are best visualized and sampled from the duodenum, whereas lesions in the pancreatic body and tail are best evaluated from the stomach. Knowledge of patient anatomy is particularly important if a history of esophageal—gastric surgery or stricture exists.
EUS has the ability to accurately detect and sample small lesions, even those less than 1 cm.15 The majority of pancreatic malignancies will appear hypoechoic relative to the surrounding parenchyma, which makes them readily identifiable. Difficult-to-detect lesions are usually small (<1 cm) and/or poorly defined. The presence of inflammatory change or fatty infiltration in the background of a pancreatic mass may make visualization difficult. It is estimated that up to 20—35% of patients undergoing EUS-FNA of pancreatic lesions have underlying chronic pancreatitis or postobstructive parenchymal changes.54-56
Local anatomic clues, as previously mentioned, can help. Some lesions may have morphologic characteristics that suggest a diagnosis, such as the discrete, well-circumscribed, smooth, regular borders of a neu-roendocrine tumor; the microcystic, honeycombed appearance of a serous cystadenoma; or the diffuse, infiltrative appearance of a lymphoma with associated adenopathy. The usual frequency for EUS of the pancreas is 5.0—7.5 MHz with conventional B mode imaging. Fine adjustment of the gain setting on the EUS processor as well as image enhancements with water and power Doppler are usually helpful. Many experienced endosonographers exclusively use the linear echoendo-scope to evaluate the pancreas when FNA is planned, although a second pass with the radial echoendoscope may be helpful.57 New EUS imaging techniques may help distinguish pancreatic adenocarcinoma from other pancreatic processes, as discussed below.
Contrast-Enhanced Harmonic Endoscopic Ultrasound
Contrast-enhanced harmonic EUS (CEH-EUS) involves intravenous injection of an ultrasound contrast agent that can provide assessment of the microvascularization and perfusion patterns within a pancreatic mass. The contrast agent consists of microbubbles that oscillate when exposed to sound waves, resulting in acoustic signals that are converted to color images, which enables distinction among tissue types.58 Initial studies enhanced only power Doppler signals, which have low sensitivity for detecting small vessels and were limited by tissue artifacts. New-generation contrast agents and echoendoscopes equipped with improved contrast-enhanced harmonic imaging technology allow for increased resolution.
Pancreatic adenocarcinoma has a distinct hypovas-cular appearance compared with other processes, such as neuroendocrine tumors or chronic and autoimmune pancreatitis, which have a hyper- or isovascular appear-ance.59-63 In a recent meta-analysis of 12 studies and 1,139 patients, hypoenhanced lesions seen on CEH-EUS had a pooled sensitivity of 94% and specificity of 89% for the differential diagnosis of pancreatic adenocarcinoma in patients with pancreatic mass lesions.64
Endoscopic Ultrasound Elastography
EUS elastography is a technique that analyzes differences in the elastic properties of tissue. Several studies have shown that it may be used to distinguish benign from malignant pancreatic masses.65-73 Pancreatic cancer typically has a hard or stiff appearance in comparison with pancreatitis, which is usually mixed (represented by a difference in color on EUS). Second-generation EUS elastography enables more objective quantitative analysis of tissue stiffness.70 In a prospective study of 130 consecutive patients with solid pancreatic masses and 20 controls with a normal pancreas, the sensitivity, specificity, positive and negative predictive values, and accuracy of quantitative EUS elastography for malignancy were 100%, 85.5%, 90.7%, 100%, and 94%, respectively.70 EUS elastography was helpful in differentiating pancreatic cancer from inflammatory masses (sensitivity, 100%; specificity, 96%) and neuroendocrine tumors (sensitivity, 100%; specificity, 88%).
Endoscopic Ultrasound Spectrum Analysis
EUS spectrum analysis of backscattered radiofrequency ultrasound signals that underlie grayscale EUS images also has been recently introduced to provide quantitative tissue characterization within the pancreas. This technology also can be used with electronic array echoendoscopes to distinguish between chronic pancreatitis and pancreatic cancer.74
Role of New Endoscopic Ultrasound Imaging Techniques
None of the techniques discussed above have yet to be widely adapted. Although it is unlikely that they will completely replace the need for FNA, they may be useful in select cases to target optimal areas for FNA within a lesion. They may also assist in making clinical decisions for management of cases in which EUS-FNA findings are negative.61
Optimal Techniques for Sampling of Solid Pancreatic Lesions
Once visualized, the next challenge is obtaining an adequate specimen. This requires accurate placement of the needle into the lesion, which by itself does not guarantee an adequate sample. Several factors have been demonstrated to be important.
The nature and consistency of the lesion plays a significant factor in the quality of the specimen obtained for cytologic interpretation. Adjustment in technique and/or additional passes may be required to maximize the chance of diagnosis. Well-differentiated tumors may be more difficult to diagnose; one study showed that a significantly higher number of aspirations were required to make a diagnosis for well-differentiated tumors (5.50±2.71; P<.001) versus moderately differentiated tumors (2.73±1.22), moderately to poorly differentiated tumors (3.37±2.11), or poorly differentiated tumors (2.28±1.06).42,75
Large tumors are more likely to be necrotic and/or fibrotic with an indurated consistency, making it difficult to puncture them or move the needle within the lesion. Resultant cytologic yield may be scant despite good needle position because malignant cells are embedded within fibrous stroma and necrotic tissue.51,52,76 Small tumors may not only be difficult to accurately target but also may have a greater tendency to be displaced or fall out of the lesion during needle advancement. Vascular lesions produce a bloody specimen that will obscure visualization of cellular aspirate. Inflammation that occurs with chronic pancreatitis, for example, may obscure or mimic a pancreatic malignancy by causing a reactive process that produces cellular changes that are indistinguishable from well-differentiated neoplasia.54-56 The sensitivity of EUS-FNA to diagnose malignancy in the setting of chronic pancreatitis was shown to be considerably lower than that in patients with a normal pancreatic parenchyma (54% vs 89%) in one study.55
FNA techniques vary, and the best technique is unknown. The site of FNA within a lesion is thought to be important. In general, the shorter the distance needed to reach the target lesion, the better. Targeting the periphery is generally advised for large lesions that may be centrally necrotic. However, the periphery also may provide reactive desmoplasia and inflammatory debris induced by the tumor.51 Therefore, “fanning” the needle throughout the lesion is recommended.52,75 Reactive changes also may occur around indwelling biliary stents or surrounding nonlesional tissue, which may render false-positive results. Needle movement within the lesion may be important. Usually, quick back-and-forth jabbing or “staccato” movements (~5—10) are recommended versus slow movements. Short “ice pick” movements versus long strokes within the lesion may break up tissue for better cytologic yield at the expense of making the sample bloodier.
Lesions in the pancreatic uncinate region are the most difficult to sample by FNA. This is primarily because angulation of the endoscope and/or deflection of the endoscope tip needed to visualize the lesion may make passage of the needle difficult, especially in the long position. The resistance and bending encountered with passage of the needle may result in inadequate visualization and sampling. Sometimes, the endoscope will have to be pulled back into a straight position to remove the needle. In general, the straighter and shorter the endoscope position, the better; however, there can be an increased propensity for unstable endoscope position in the short position, which results in the endoscope falling back into the stomach.52
Transgastric FNA for lesions in the pancreatic body and tail also may be challenging due to tenting of the needle against the thicker and redundant gastric wall. To overcome this problem, suction of the gastric wall and a controlled, quick, forceful spearing motion is needed to puncture the lesion. The use of the needle depth adjustment lock will prevent overshooting the lesion. It may also be helpful to have an assistant hold the endoscope to minimize its movement with that of the needle.
Available needle sizes are 19 gauge (G), 22G, and 25G. The optimal needle size for FNA depends on the nature and location of the suspected lesion. The 22G or 25G needle is most commonly used for cytologic sampling of the pancreas. Multiple studies have compared the cytologic yield of FNA for 22G and 25G needles (Table 2).77-85 The overall diagnostic accuracy of these needles is similar and most have failed to show superiority. However, a meta-analysis involving 6 studies and 1,064 patients suggested that the 25G needle was more sensitive than the 22G needle (93% vs 84%) for diagnosing pancreatic malignancy.86 The smaller 25G needles may perform better because they provide a more cellular and less bloody aspirate with less tissue trauma for better cytologic interpretation. The 25G needle is also more flexible and technically easier to use in the pancreatic head and uncinate region.
Table 2.
Comparative Studies of Needles for EUS-FNA of the Pancreas
| Study | Number of pancreatic masses | Needle gauge | Percent diagnostic accuracy |
|---|---|---|---|
| Camellini L, et al83 (Prospective) | 43 | 22 | 86.5 |
| 41 | 25 | 89.2 | |
| Fabbri C, et al84 (Prospective) | 50 | 22 | 86.0 |
| 50 | 25 | 94.0 | |
| Song TJ, et al82 (Prospective) | 60 | 19 | 86.7 |
| 57 | 22 | 78.9 | |
| Sakamoto H, et al79 (Prospective) | 24 | 22 | 79.7 |
| 24 | 25 | 91.7 | |
| 24 | 19 Tru-cut | 54.1 | |
| Siddiqui UD, et al78 (Prospective) | 64 | 22 | 87.5 |
| 67 | 25 | 95.5 | |
| Lee JH, et al81 (Prospective) | 12 | 22 | 100 |
| 12 | 25 | 100 | |
| Yusuf TE, et al80 (Retrospective) | 540 | 22 | 84.0 |
| 302 | 25 | 92.0 |
EUS-FNA=endoscopic ultrasound—guided fine-needle aspiration.
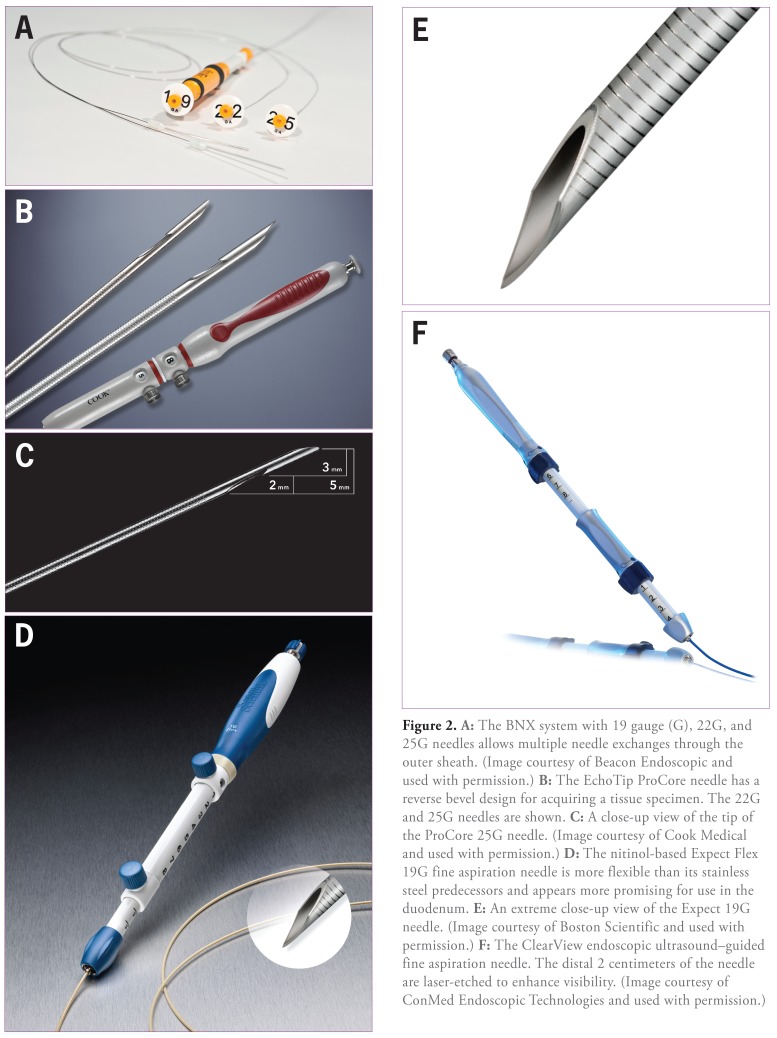
Multiple FNA needles are now commercially available (Table 3 and Figure 2). Head-to-head comparisons are lacking, though. Other than size, the primary differences include tip visibility; needle composition (stainless steel alloy vs nitinol or cobalt chromium), which may make a difference with respect to performance; penetration; push-ability; resistance to needle deformity; and durability. If the needle bends, it may be possible to carefully straighten the needle manually within the sheath between passes.
Table 3.
Commercially Available EUS-FNA Needles
| Manufacturer | Device | Needle gauge |
|---|---|---|
| Boston Scientific | Expect | 19, 22, 25 |
| Expect Flex | 19 | |
| Beacon Endoscopic | BNX | 19, 22, 25 |
| ConMed Corporation | Vizeon | 19, 22, 25 |
| ClearView | 19, 22, 25 | |
| Medi-Globe Corporation (not commercially available in the United States) | Sono Tip Pro Control | 19, 22, 25 |
| Sono Tip EUS-FNA System | 19, 22, 25 | |
| Hancke-Vilmann EUS-FNA System | 19, 22 | |
| Cook Medical | Echo Tip | 22 |
| Echo Tip Ultra | 19, 22, 25 | |
| Echo Tip ProCore | 19, 22, 25 | |
| Quick-Core | 19 | |
| Olympus | EZ Shot | 22 |
| EZ Shot 2 | 19, 22, 25 | |
| EZ Shot 2 with sideport | 22 | |
| PowerShot | 22 |
EUS-FNA=endoscopic ultrasound—guided fine-needle aspiration.
Figure 2.
A: The BNX system with 19 gauge (G), 22G, and 25G needles allows multiple needle exchanges through the outer sheath. (Image courtesy of Beacon Endoscopic and used with permission.) B: The Echo Tip ProCore needle has a reverse bevel design for acquiring a tissue specimen. The 22G and 25G needles are shown. C: A close-up view of the tip of the ProCore 25G needle. (Image courtesy of Cook Medical and used with permission.) D: The nitinol-based Expect Flex 19G fine aspiration needle is more flexible than its stainless steel predecessors and appears more promising for use in the duodenum. E: An extreme close-up view of the Expect 19G needle. (Image courtesy of Boston Scientific and used with permission.) F: The Clear View endoscopic ultrasound—guided fine aspiration needle. The distal 2 centimeters of the needle are laser-etched to enhance visibility. (Image courtesy of ConMed Endoscopic Technologies and used with permission.)
Fine-Needle Biopsy
The diagnostic cytologic yield of EUS-FNA with a 22G or 25G needle may be limited for several types of lesions. Suggested indications for FNB include failure of FNA with a 22G or 25G needle, suspicion of metastatic tumors requiring special studies for identification, and diagnosis of neuroendocrine tumors, lymphoma, or autoimmune pancreatitis. In some instances, extra passes for cell block may be performed to facilitate additional studies (such as immunohistochemistry analysis, flow cytometry, or other ancillary tests) when a particular diagnosis is suspected. Usually, needle rinse alone will be insufficient. However, a core histopathologic specimen may be essential for diagnosis because cellular and tissue architecture are preserved. Until recently, this has usually required use of a larger 19G FNA needle or “tru-cut” spring-loaded biopsy needle (eg, Quick-Core, Cook Medical), which has met with variable success and complication rates of approximately 2—4%.87-89 Although 19G needles may provide a larger tissue sample, potentially improving diagnostic accuracy, they are difficult to use in the duodenum and have a higher rate of technical failure for pancreatic head lesions due to stiffness of needle and scope angulation.89 Tru-cut biopsy was not shown to be superior to FNA with respect to overall diagnostic accuracy except perhaps in certain situations such as autoimmune pancreatitis and lymphoma.87-89 Combining techniques may improve diagnostic yield and may be useful, especially when on-site cytology is not available.79,90-92
Experience is accumulating with a recently developed high-definition fine biopsy needle with a reverse bevel design for acquiring a tissue specimen (EchoTip ProCore, Cook Medical; Figures 2B and 2C). In the initial multicenter evaluation, FNB with the ProCore 19G needle was technically feasible in 45 (95.7%) of 47 pancreatic tumor cases, with a diagnostic accuracy rate of 89.4%.93 Technical failures occurred in only 2 of 35 cases from the duodenum. The 19G needle was still reported to be more difficult to pass, although this did not impair sample quality, and no complications were reported. In cases in which only 1 needle pass was performed, the overall accuracy of EUS-FNB was 89.6%. Success appeared to depend on involvement of a pathologist with experience in handling materials obtained by FNA or FNB.
A ProCore 22G needle then became available. In a prospective multicenter evaluation of solid pancreatic masses, core biopsies for histologic analysis were obtained in 55 (90.1%) of 61 masses.94 Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for histologic diagnosis were 87.5%, 100%, 100%, 41.7%, and 88.5%, respectively. Early experience suggests that the overall diagnostic accuracy of 93.7% with 19G and 22G ProCore needles was significantly higher than that of standard FNA needles for diagnosis of solid pancreatic masses (79.7%; P=.0039).95
The 19G ProCore needle may provide a better histo-logic sample quality than the 22G ProCore needle.96 One randomized trial comparing the 22G aspiration needle and 22G biopsy needle showed comparable results for EUS-guided sampling of solid pancreatic mass lesions with no significant difference in diagnostic yield or technical per-formance.97 Recently, a 25G ProCore needle also has been released and is under study.98
Early clinical experience with a nitinol-based 19G FNA needle (Expect Flex, Boston Scientific) suggested that it is more flexible than its stainless steel predecessors and appears more promising for use in the duodenum (Figures 2D and 2E).99,100
Suction or No Suction
The need for suction likely depends on the lesion. The use of suction and how it is performed during FNA vary widely. No standard suction technique has been established. Normal suction is generally performed using a 10 mL syringe and may be applied constantly, intermittently, or manually. Most clinicians will adjust the strength of suction depending on the nature of the lesion and aspirate. Low or no suction is preferred if the aspirate is bloody; blood contamination may decrease diagnostic yield and quality.52 Suction is preferred if the initial aspirate is scant; active suction may increase cellularity in fibrotic solid pancreatic lesions.75,101 The European Society of Gastrointestinal Endoscopy (ESGE) technical guideline recommends the application of continuous suction for EUS-FNA of solid masses but no suction for lymph nodes.27
Limited studies have shown no significant improvement in diagnostic yield of EUS-FNA with or without suction.101-103 Only one randomized trial involving 52 patients has compared suction with no suction for EUS-FNA of the pancreas; no significant differences were found in diagnostic yield (92.3% vs 80%; P=.10), blood in specimen (76.9% vs 88.5%; P=.14), or cellularity (100% vs 100%; P=1).101 Continuous, high, negative-pressure mechanical suction (35 mL of a 60 mL syringe) with a 22G needle in one study yielded a tissue core adequate for histologic evaluation in 96% of solid masses.104 The fine-needle stylet capillary suction technique, which uses only capillary aspiration achieved by slow withdrawal of the stylet, may be more sensitive and has a higher negative predictive value than suction aspiration of solid pancreatic lesions. Quality of the cytology specimen and cellular material obtained were shown to be better in 55% of capillary suctions compared with 33% of standard suctions in one study.105
A recent abstract comparing EUS-guided pancreas biopsy techniques using the ProCore needle suggested that superior tissue adequacy was obtained with the capillary aspiration suction method—whereby the stylet is slowly removed over approximately 30—40 sec as the needle is moved back and forth—versus standard 5 cc and 10 cc suctions.106 Reasons for this are unclear but may be related to a venting mechanism associated with the reverse bevel versus cutting action. Suction should be turned off before removing the needle from the lesion to avoid aspiration of intestinal contaminant.
Stylet or No Stylet
The function of the stylet is to prevent occlusion of the needle with gastrointestinal contaminant as it is passed into the target lesion. The stylet is usually slightly withdrawn from the tip of the needle to facilitate puncture through the gastric or duodenal wall. Once the needle is in the lesion, the stylet is pushed in completely to clear the needle of any intervening tissue and then is removed. The stylet is reloaded in between passes. Three randomized studies evaluating the benefit of FNA with or without the stylet (22G needles) have shown no improvement in diagnostic yield or sample quality but a possible tendency for increased bloody aspirate with the stylet.107-110 The ESGE technical guideline states that there is insufficient evidence to recommend for or against using the stylet.27 Interestingly, the capillary suction technique that includes slow withdrawal of the stylet may provide better-quality specimens (especially when used in conjunction with the ProCore needle), although further studies are pending.105,106
Number of Passes
Most studies have shown that maximal diagnostic yield can be obtained after 3—5 passes for pancreatic masses if ROSE is available and if the quality of the passes is high. In the absence of ROSE, the recommended number of passes is 5—7 for solid pancreatic lesions.42,111 The incremental yield of additional passes beyond this becomes negligible.51 The determination of specimen adequacy by gross inspection has been shown to be poor. Direct feedback from the cytologist during the procedure can provide useful information regarding the adequacy of the specimen and need for additional passes.27,47,51,111
Erickson and colleagues showed that a general policy of 5 passes would mean that too few or too many passes would be made in about 50% of patients.42 No definitive endosonographic finding can predict the optimal number of passes. The presence of underlying chronic pancreatitis makes diagnosis more difficult. Tumors that are well differentiated may be a predictor of the need for a larger number of FNA passes.110 Highly vascular lesions give progressively less diagnostic material because the number of passes increases due to blood contamination.51 Aspiration needles may become difficult to use after 3—4 passes due to accumulation of material and blood in the needle or bending or blunting of the needle. In pancreatic cases, this necessitated the use of additional needles in about 15% of cases and increased overall procedure time.24
Cytologic Sample Processing
Preparation of good smears is the last important step. Training is required to learn this technique, especially if a cytotechnician is not present. It is not known to what degree variability in technique affects outcomes, but this is yet another good reason to communicate with the cytologist. The ESGE and the British Society for Clinical Cytology have published guidelines.27,112
The way that material is expressed from the needle onto a slide may influence diagnostic yield. Reinsertion of the stylet, air-filled syringe, or both can be used to express material onto the slide. The stylet allows for more control and the removal of a possible clot, although it is more time consuming and is possibly associated with an increased risk of needlestick injury.52,109
Air insertion may result in uncontrolled splatter of aspirate and air drying artifacts or clotting of the speci-men.52 Thin smears are desirable to avoid excessive cellular overlap that may impair interpretation. Close inspection of the aspirate with careful separation of excessive blood clots from tissue material is helpful. Air-dried slides stained with Romanofsky staining (ie, Diff-Quik, Siemens) provide morphologic assessment on-site. Although Diff-Quik staining usually provides adequate findings for a preliminary diagnosis, ethanol-fixed and Papanicolaou-stained material provides the best nuclear detail. The smears must be placed immediately into alcohol to minimize air drying artifacts.51 Material also may be placed in a liquid medium or fixative for cell block, which can then be formalin-fixed, paraffin-embedded, and sectioned for standard hematoxylin and eosin staining or other ancillary testing. Cell blocks are used as a complement of, not a substitute, for smears.27 Liquid-based cytology preparations may be useful if immediate cytologic evaluation is not available. However, it is expensive; all material must be placed directly into a liquid fixative.52
Molecular Analysis
FNA aspirates from pancreatic masses may be used for various molecular tests, including KRAS mutation analysis, as the mutation may be present in 75—95% of pancreatic adenocarcinoma.108,109 The routine use of KRAS mutation analysis combined with cytology for increasing the diagnostic yield of pancreatic malignancy is unclear and not the standard of care.113-116 Emerging future applications for select indeterminate cases and personalized cancer care may clarify the exact role of KRAS and other mutations that can be tested in an EUS-FNA sample.
Molecular analysis of FNA samples in pancreatic cancer may improve understanding of molecular mechanisms of cancer development and therapies. For example, fine-needle aspirates have recently been used to identify the predictive marker hENT1 for gemcitabine response in pancreatic cancer.117 Measurement of Ki-67 from FNA also has proven useful in the assessment of malignant behavior of pancreatic neuroendocrine tumors and the prediction of 5-year survival.118
Summary
Multiple variables influence the diagnostic yield of EUS-FNA. Identifying which ones are most important for a given lesion in any given situation remains a challenge. Awareness of these potential variables and the ability to modify techniques when indicated will no doubt enhance outcomes. Advances in EUS technology and refinements in current techniques hold promise for continued improvement and expanded applications of this procedure.
Footnotes
Dr. Weston has received consumable supplies from Cook Medical for a research project. Dr. Bhutani has received a temporary loan of equipment and consumable supplies for research from Boston Scientific.
References
- 1.Dumonceau JM, Polkowski M, Larghi A, et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2011;43:897–912. doi: 10.1055/s-0030-1256754. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 3.Hewitt MJ, McPhail MJ, Possamai L, et al. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc. 2012;75:319–331. doi: 10.1016/j.gie.2011.08.049. [DOI] [PubMed] [Google Scholar]
- 4.Mertz HR, Sechopoulos P, Delbeke D. EUS, PET, and CT scanning for evaluation of pancreatic adenocarcinoma. Gastrointest Endosc. 2000;52:367–371. doi: 10.1067/mge.2000.107727. [DOI] [PubMed] [Google Scholar]
- 5.Gress F, Gottlieb K, Sherman S, et al. Endoscopic ultrasonography-guided fine-needle aspiration biopsy of suspected pancreatic cancer. Ann Intern Med. 2001;134:459–464. doi: 10.7326/0003-4819-134-6-200103200-00010. [DOI] [PubMed] [Google Scholar]
- 6.Mallery JS, Centeno BA, Hahn PF, et al. Pancreatic tissue sampling guided by EUS CT/US, and surgery: a comparison of sensitivity and specificity. Gastrointest Endosc. 2002;56:218–224. doi: 10.1016/s0016-5107(02)70181-8. [DOI] [PubMed] [Google Scholar]
- 7.Harewood GC, Wiersema MJ. Endosongraphy-guided fine needle aspiration biopsy in the evaluation of pancreatic masses. Am J Gastroenterol. 2002;97:1386–1391. doi: 10.1111/j.1572-0241.2002.05777.x. [DOI] [PubMed] [Google Scholar]
- 8.DeWitt J, Devereaux B, Chriswell M, et al. Comparison of endoscopic ultra-sonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann Intern Med. 2004;141:753–763. doi: 10.7326/0003-4819-141-10-200411160-00006. [DOI] [PubMed] [Google Scholar]
- 9.Volmar KE, Vollmer RT, Jowell PS, et al. Pancreatic FNA in 1000 cases: a comparison of imaging modalities. Gastrointest Endosc. 2005;61:854–861. doi: 10.1016/s0016-5107(05)00364-0. [DOI] [PubMed] [Google Scholar]
- 10.Horwhat JD, Paulson EK, McGrath K, et al. A randomized comparison of EUS-guided FNA versus CT or US-guided FNA for the evaluation of pancreatic mass lesions. Gastrointest Endosc. 2006;63:966–975. doi: 10.1016/j.gie.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 11.Erturk SM, Mortelé KJ, Tuncali K, et al. Fine-needle aspiration biopsy of solid pancreatic masses: comparison of CT and endoscopic sonography guidance. AJR Am J Roentgenol. 2006;187:1531–1535. doi: 10.2214/AJR.05.1657. [DOI] [PubMed] [Google Scholar]
- 12.Chaya C, Nealon WH, Bhutani MS. EUS or percutaneous CT/US-guided FNA for suspected pancreatic cancer: when tissue is the issue. Gastrointest Endosc. 2006;63:76–78. doi: 10.1016/j.gie.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Dewitt J, Devereaux BM, Lehman GA, et al. Comparison of endoscopic ultrasound and computed tomography for the preoperative evaluation of pancreatic cancer: a systematic review. Clin Gastroenterol Hepatol. 2006;4:717–725. doi: 10.1016/j.cgh.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Hartwig W, Schneider L, Diener MK, et al. Preoperative tissue diagnosis for tumours of the pancreas. Br J Surg. 2009;96:5–20. doi: 10.1002/bjs.6407. [DOI] [PubMed] [Google Scholar]
- 15.Uehara H, Ikezawa K, Kawada N, et al. Diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration for suspected pancreatic malignancy in relation to the size of lesions. J Gastroenterol Hepatol. 2011;26:1256–1261. doi: 10.1111/j.1440-1746.2011.06747.x. [DOI] [PubMed] [Google Scholar]
- 16.Dewitt J, McGreevy K, Sherman DS, et al. Utility of a repeated EUS at a tertiary referral center. Gastrointest Endosc. 2008;67:610–619. doi: 10.1016/j.gie.2007.09.037. [DOI] [PubMed] [Google Scholar]
- 17.Iglesias-Garcia J, Dominguez-Munoz JE, Lozano-Leon A, et al. Impact of endoscopic-ultrasound fine needle biopsy for diagnosis of pancreatic masses. World J Gastroenterol. 2007;13:289–293. doi: 10.3748/wjg.v13.i2.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eloubeidi MA, Varadarajulu S, Desai S, et al. Value of repeat endoscopic ultrasound-guided fine needle aspiration for suspected pancreatic cancer. J Gastroenterol Hepatol. 2008;23:567–570. doi: 10.1111/j.1440-1746.2007.05119.x. [DOI] [PubMed] [Google Scholar]
- 19.Tadic M, Kujundzic M, Stoos-Veic T, et al. Role of repeated endoscopic ultrasound-guided fine needle aspiration in small solid pancreatic masses with previous indeterminate and negative cytological findings. Dig Dis. 2008;26:377–382. doi: 10.1159/000177025. [DOI] [PubMed] [Google Scholar]
- 20.Bhutani MS, Gress FG, Giovannini M, et al. The No Endosonographic Detection of Tumor (NEST) study: a case series of pancreatic cancers missed on endoscopic ultrasonography. Endoscopy. 2004;36:385–389. doi: 10.1055/s-2004-814320. [DOI] [PubMed] [Google Scholar]
- 21.Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA19-9) as a biomarker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33:266–270. doi: 10.1016/j.ejso.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Fritscher-Ravens A, Sriram PV, Krause C, et al. Detection of pancreatic metas-tases by EUS-guided fine-needle aspiration. Gastrointest Endosc. 2001;53:65–70. doi: 10.1067/mge.2001.111771. [DOI] [PubMed] [Google Scholar]
- 23.Dewitt J, Jowell P, Leblanc J, et al. EUS-guided FNA of pancreatic metastases: a multicenter experience. Gastrointest Endosc. 2005;61:689–696. doi: 10.1016/s0016-5107(05)00287-7. [DOI] [PubMed] [Google Scholar]
- 24.Erickson RA, Garza AA. Impact of endoscopic ultrasound on the management and outcome of pancreatic carcinoma. Am J Gastronterol. 2000;95:2248–2254. doi: 10.1111/j.1572-0241.2000.02310.x. [DOI] [PubMed] [Google Scholar]
- 25.Savides TJ, Donohue M, Hunt G, et al. EUS-guided FNA diagnostic yield of malignancy in solid pancreatic masses: a benchmark for quality performance measurement. Gastrointest Endosc. 2007;66:277–282. doi: 10.1016/j.gie.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 26.Eisen GM, Dominitz JA, Faigel DO, et al. Guidelines for credentialing and granting privileges for endoscopic ultrasound. Gastrointest Endosc. 2001;54:811–814. doi: 10.1016/s0016-5107(01)70082-x. [DOI] [PubMed] [Google Scholar]
- 27.Polkowski M, Larghi A, Weynand B, et al. Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012;44:190–206. doi: 10.1055/s-0031-1291543. [DOI] [PubMed] [Google Scholar]
- 28.Hoffman BJ, Wallace MB, Eloubeidi MA, et al. How many supervised procedures does it take to become competent in EUS? Results of a multicenter three year study. Gastrointest Endosc. 2000;51 AB139. [Google Scholar]
- 29.Harewood GC, Wiersema LM, Hailing AC, et al. Influence of EUS training and pathology interpretation on accuracy of EUS-guided fine needle aspiration of pancreatic masses. Gastrointest Endosc. 2002;55:669–673. doi: 10.1067/mge.2002.123419. [DOI] [PubMed] [Google Scholar]
- 30.Mertz H, Gautam S. The learning curve for EUS-guided FNA of pancreatic cancer. Gastrointest Endosc. 2004;59:33–37. doi: 10.1016/s0016-5107(03)02028-5. [DOI] [PubMed] [Google Scholar]
- 31.Eloubeidi MA, Tamhane A. EUS-guided FNA of solid pancreatic masses: a learning curve with 300 consecutive procedures. Gastrointest Endosc. 2005;61:700–708. doi: 10.1016/s0016-5107(05)00363-9. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz DA, Unni KK, Levy MJ, et al. The rate of false-positive results with EUS-guided fine-needle aspiration. Gastrointest Endosc. 2002;56:868–872. doi: 10.1067/mge.2002.129610. [DOI] [PubMed] [Google Scholar]
- 33.Levy MJ, Gleeson FC, Campion MB, et al. Prospective cytological assessment of gastrointestinal luminal fluid acquired during EUS: a potential source of false-positive FNA and needle tract seeding. Am J Gastroenterol. 2010;105:1311–1318. doi: 10.1038/ajg.2010.80. [DOI] [PubMed] [Google Scholar]
- 34.Gleeson FC, Kipp BR, Caudill JL, et al. False positive endoscopic ultrasound fine needle aspiration cytology: incidence and risk factors. Gut. 2010;59:586–593. doi: 10.1136/gut.2009.187765. [DOI] [PubMed] [Google Scholar]
- 35.Eloubeidi MA, Gress FG, Savides TJ, et al. Acute pancreatitis after EUS-guided FNA of solid pancreatic masses: a pooled analysis from EUS centers in the United States. Gastrointest Endosc. 2004;60:385–389. doi: 10.1016/s0016-5107(04)01714-6. [DOI] [PubMed] [Google Scholar]
- 36.Adler DG, Jacobson BC, Davilla RE, et al. ASGE guideline: complications of EUS. Gastrointest Endosc. 2005;61:8–12. doi: 10.1016/s0016-5107(04)02393-4. [DOI] [PubMed] [Google Scholar]
- 37.Eloubeidi MA, Tamhane A, Varadarajulu S, et al. Frequency of major complications after EUS-guided FNA of solid pancreatic masses: a prospective evaluation. Gastrointest Endosc. 2006;63:622–629. doi: 10.1016/j.gie.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 38.Paquin SC, Gariépy G, Lepanto L, et al. A first report of tumor seeding because of EUS-guided FNA of a pancreatic adenocarcinoma. Gastrointest Endosc. 2005;61:610–611. doi: 10.1016/s0016-5107(05)00082-9. [DOI] [PubMed] [Google Scholar]
- 39.Chong A, Venugopal K, Segarajasungam D, et al. Tumor seeding after EUS-guided FNA of pancreatic tail neoplasia. Gastrointest Endosc. 2011;74:933–935. doi: 10.1016/j.gie.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 40.Katanuma A, Maguchi H, Hashigo S, et al. Tumor seeding after endoscopic ultrasound-guided fine needle aspiration of cancer in the body of the pancreas. Endoscopy. 2012;44:E160–E161. doi: 10.1055/s-0031-1291716. [DOI] [PubMed] [Google Scholar]
- 41.Micames C, Jowell PS, White R, et al. Lower frequency of peritoneal carci-nomatosis in patients with pancreatic cancer diagnosed by EUS-guided FNA vs. percutaneous FNA. Gastrointest Endosc. 2003;58:690–695. doi: 10.1016/s0016-5107(03)02009-1. [DOI] [PubMed] [Google Scholar]
- 42.Erickson RA, Sayage-Rabie L, Beissner RS. Factors predicting the number of EUS guided fine needle passes for diagnosis of pancreatic malignancies. Gastroin-test Endosc. 2000;51:184–190. doi: 10.1016/s0016-5107(00)70416-0. [DOI] [PubMed] [Google Scholar]
- 43.Klapman JB, Logrono R, Dye CE, et al. Clinical impact of on-site cytopathol-ogy interpretation on endoscopic ultrasound-guided fine needle aspiration. Am J Gastroenterol. 2003;98:1289–1294. doi: 10.1111/j.1572-0241.2003.07472.x. [DOI] [PubMed] [Google Scholar]
- 44.Eloubeidi MA, Tamhane A, Jhala N, et al. Agreement between rapid onsite and final cytologic interpretations of EUS-guided FNA specimens: implications for the endosonographer and patient management. Am J Gastroenterol. 2006;101:2841–2847. doi: 10.1111/j.1572-0241.2006.00852.x. [DOI] [PubMed] [Google Scholar]
- 45.Pellisé Urquiza M, Fernádez-Esparrach G, Solé M, et al. Endoscopic ultrasound-guided fine needle aspiration: predictive factors of accurate diagnosis and cost-minimization analysis of on-site pathologist. Gastroenterol Hepatol. 2007;30:319–324. doi: 10.1157/13107565. [DOI] [PubMed] [Google Scholar]
- 46.Iglesias-Garcia J, Dominguez-Munoz JE, Abdulkader I, et al. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of solid pancreatic masses. Am J Gastroenterol. 2011;106:1705–1710. doi: 10.1038/ajg.2011.119. [DOI] [PubMed] [Google Scholar]
- 47.Itoi T, Tsuchiya T, Itokawa F, et al. Histological diagnosis by EUS-guided fine-needle aspiration biopsy in pancreatic solid masses without on-site cytopathologist: a single-center experience. Dig Endosc. 2011;23(suppl 1):34–38. doi: 10.1111/j.1443-1661.2011.01142.x. [DOI] [PubMed] [Google Scholar]
- 48.Savoy AD, Raimondo M, Woodward TA, et al. Can endosonographers evaluate on-site cytologic adequacy? A comparison with cytotechnologists. Gastrointest Endosc. 2007;65:953–957. doi: 10.1016/j.gie.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 49.Nguyen YP, Maple JT, Zhang Q, et al. Reliability of gross visual assessment of specimen adequacy during EUS-guided FNA of pancreatic masses. Gastrointest Endosc. 2009;69:1264–1270. doi: 10.1016/j.gie.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 50.Hikichi T, Irisawa A, Bhutani MS, et al. Endoscopic ultrasound-guided fine needle aspiration of solid pancreatic masses with rapid on-site cytological evaluation by endosonographers without attendance of cytopathologists. J Gastroenterol. 2009;44:322–328. doi: 10.1007/s00535-009-0001-6. [DOI] [PubMed] [Google Scholar]
- 51.Kulesza P, Eltoum I. Endoscopic ultrasound-guided fine-needle aspiration: sampling, pitfalls and quality management. Clin Gastroenterol Hepatol. 2007;5:1248–1254. doi: 10.1016/j.cgh.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 52.Savides TJ. Tricks for improving EUS-FNA accuracy and maximizing cellular yield. Gastrointest Endosc. 2009;69(2 suppl):S130–S133. doi: 10.1016/j.gie.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 53.Greenlee RT, Murray T, Bolden S, et al. Cancer statistics, 2000. CA Cancer J Clin. 2000;50:7–33. doi: 10.3322/canjclin.50.1.7. [DOI] [PubMed] [Google Scholar]
- 54.Fritscher-Ravens A, Topalidis T, Bobrowski C, et al. Endoscopic ultrasound-guided fine-needle aspiration in focal pancreatic lesions: a prospective intraindi-vidual comparison of two needle assemblies. Endoscopy. 2001;33:484–490. doi: 10.1055/s-2001-14970. [DOI] [PubMed] [Google Scholar]
- 55.Fritscher-Ravens A, Brand L, Knofel WT, et al. Comparison of endoscopic ultrasound-guided fine needle aspiration for focal pancreatic lesions in patients with normal parenchyma and chronic pancreatitis. Am J Gastroenterol. 2002;97:2768–2775. doi: 10.1111/j.1572-0241.2002.07020.x. [DOI] [PubMed] [Google Scholar]
- 56.Varadarajulu S, Tamhane A, Eloubeidi MA. Yield of EUS-guided FNA of pancreatic masses in the presence or the absence of chronic pancreatitis. Gastrointest Endosc. 2005;62:728–736. doi: 10.1016/j.gie.2005.06.051. [DOI] [PubMed] [Google Scholar]
- 57.Shin EJ, Topazian M, Syngal S, et al. Radial versus linear and second look endoscopic ultrasound (EUS) improved detection of pancreatic lesions: a randomized tandem study. GastrointestEndosc. 2012;75(4S) AB130. [Google Scholar]
- 58.Sanchez MVA, Varadarajulu S, Napoleon B. EUS contrast agents: what is available, how do they work, and are they effective? Gastrointest Endosc. 2009;69:71–77. doi: 10.1016/j.gie.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 59.Hocke M, Schulze E, Gottschalk P, Topalidis T, Dietrich CF. Contrast-enhanced endoscopic ultrasound in discrimination between focal pancreatitis and pancreatic cancer. World J Gastroenterol. 2006;12:246–250. doi: 10.3748/wjg.v12.i2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hocke M, Ignee A, Topalidis T, Stallmach A, Dietrich CF. Contrast-enhanced endosonographic Doppler spectrum analysis is helpful in discrimination between focal chronic pancreatitis and pancreatic cancer. Pancreas. 2007;35:286–288. doi: 10.1097/MPA.0b013e318093f964. [DOI] [PubMed] [Google Scholar]
- 61.Napoleon B, Alvarez-Sanchez MV, Gincoul R, et al. Contrast-enhanced harmonic endoscopic ultrasound in solid lesions of the pancreas: results of a pilot study. Endoscopy. 2010;42:564–570. doi: 10.1055/s-0030-1255537. [DOI] [PubMed] [Google Scholar]
- 62.Săftoiu A, Iordache SA, Gheonea DI, et al. Combined contrast-enhanced power Doppler and real-time sonoelastography performed during EUS used in the differential diagnosis of focal pancreatic masses (with videos) Gastrointest Endosc. 2010;72:739–747. doi: 10.1016/j.gie.2010.02.056. [DOI] [PubMed] [Google Scholar]
- 63.Ishikawa T, Itoh A, Kawashima H, et al. Usefulness of EUS combined with contrast-enhancement in the differential diagnosis of malignant versus benign and preoperative localization of pancreatic endocrine tumors. Gastrointest Endosc. 2010;71:951–959. doi: 10.1016/j.gie.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 64.Gong T, Hu D, Zhu Q. Contrast-enhanced EUS for differential diagnosis of pancreatic mass lesions: a meta-analysis. Gastrointest Endosc. 2012;76:301–309. doi: 10.1016/j.gie.2012.02.051. [DOI] [PubMed] [Google Scholar]
- 65.Saftoiu A, Vilman P. Endoscopic ultrasound elastography—a new imaging technique for the visualization of tissue elasticity distribution. J Gastrointestin Liver Dis. 2006;15:161–165. [PubMed] [Google Scholar]
- 66.Giovannini M, Hookey LC, Bories E, et al. Endoscopic ultrasound elastog-raphy: the first step towards virtual biopsy? Preliminary results in 49 patients. Endoscopy. 2006;38:344–348. doi: 10.1055/s-2006-925158. [DOI] [PubMed] [Google Scholar]
- 67.Janssen J, Schlorer E, Greiner L. EUS elastography of the pancreas: feasibility and pattern description of the normal pancreas, chronic pancreatitis and focal pancreatic lesions. Gastrointest Endosc. 2007;65:971–978. doi: 10.1016/j.gie.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 68.Hirche TO, Ignee A, Barreiros AP, et al. Indications and limitations of endo-scopic ultrasound elastography for evaluation of focal pancreatic lesions. Endoscopy. 2008;40:910–917. doi: 10.1055/s-2008-1077726. [DOI] [PubMed] [Google Scholar]
- 69.Giovannini M, Thomas B, Erwan B, et al. Endoscopic ultra-sound elastog-raphy for evaluation of lymph nodes and pancreatic masses: a multicenter study. World J Gastroenterol. 2009;15:1587–1593. doi: 10.3748/wjg.15.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, et al. EUS elastography for the characterization of solid pancreatic masses. Gastrointest Endosc. 2009;70:1101–1108. doi: 10.1016/j.gie.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 71.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, et al. Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology. 2010;139:1172–1180. doi: 10.1053/j.gastro.2010.06.059. [DOI] [PubMed] [Google Scholar]
- 72.Hocke M, Ignee A, Dietrich CF. Contrast-enhanced endoscopic ultrasound in the diagnosis of autoimmune pancreatitis. Endoscopy. 2011;43:163–165. doi: 10.1055/s-0030-1256022. [DOI] [PubMed] [Google Scholar]
- 73.Saftoiu A, Dietrich CF, Vilmann P. Contrast-enhanced harmonic endoscopic ultrasound. Endoscopy. 2012;44:612–617. doi: 10.1055/s-0032-1308909. [DOI] [PubMed] [Google Scholar]
- 74.Kumon RE, Repaka A, Atkinson M, et al. Characterization of the pancreas in vivo using EUS spectrum analysis with electronic array echoendoscopes. Gastrointest Endosc. 2012;75:1175–1183. doi: 10.1016/j.gie.2012.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Binmoeller KF, Rathod V. Difficult pancreatic mass FNA; tips for success. Gastrointest Endosc. 2002;56:S86–S91. doi: 10.1016/s0016-5107(02)70093-x. [DOI] [PubMed] [Google Scholar]
- 76.Robins DB, Katz RL, Evans DB, et al. Fine needle aspiration of the pancreas: in quest of accuracy. Acta Cytol. 1995;39:1–10. [PubMed] [Google Scholar]
- 77.Fabbri C, Polifemo AM, Luigiano C, et al. Comparative study of EUS-guided 25 gauge needle versus EUS-guided 22 gauge needle for FNA in patients with solid pancreatic masses: preliminary results. Dig Liver Dis. 2009;41:S60–S61. [Google Scholar]
- 78.Siddiqui UD, Rossi F, Rosenthal LS, et al. EUS-guided FNA of solid pancreatic masses: a prospective, randomized trial comparing 22-gauge and 25-gauge needles. Gastrointest Endosc. 2009;70:1093–1097. doi: 10.1016/j.gie.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 79.Sakamoto H, Kitano M, Komaki T, et al. Prospective comparative study if the EUS guided 25-gauge FNA needle with the 19-gauge Trucut needle and 22-gauge FNA needle in patients with solid pancreatic masses. J Gastroenterol Hepatol. 2009;24:384–390. doi: 10.1111/j.1440-1746.2008.05636.x. [DOI] [PubMed] [Google Scholar]
- 80.Yusuf TE, Ho S, Pavey DA, et al. Retrospective analysis of the utility of endo-scopic ultrasound-guided fine-needle aspiration (EUS-FNA) in pancreatic masses, using a 22-gauge or 25-gauge needle system: a multicenter experience. Endoscopy. 2009;41:445–458. doi: 10.1055/s-0029-1214643. [DOI] [PubMed] [Google Scholar]
- 81.Lee JH, Stewart J, Ross WA, et al. Blinded prospective comparison of the performance of 22-gauge and 25-gauge needles in endoscopic ultrasound-guided fine needle aspiration of the pancreas and peri-pancreatic lesions. Dig Dis Sci. 2009;54:2274–2281. doi: 10.1007/s10620-009-0906-1. [DOI] [PubMed] [Google Scholar]
- 82.Song TJ, Kim JH, Lee SS, et al. The prospective randomized, controlled trial of endoscopic ultrasound-guided fine-needle aspiration using 22G and 19G aspiration needles for solid pancreatic or peripancreatic masses. Am J Gastroenterol. 2010;105:1739–1745. doi: 10.1038/ajg.2010.108. [DOI] [PubMed] [Google Scholar]
- 83.Camellini L, Carlinfante G, Azzolini F, et al. A randomized clinical trial comparing 22G and 25G needles in endoscopic ultrasound-guided fine-needle aspiration of solid lesions. Endoscopy. 2011;43:709–715. doi: 10.1055/s-0030-1256482. [DOI] [PubMed] [Google Scholar]
- 84.Fabbri C, Polifemo AM, Luigiano C, et al. Endoscopic ultrasound-guided fine needle aspiration with 22- and 25-gauge needles in solid pancreatic masses: a prospective comparative study with randomization of needle sequence. Dig Liver Dis. 2011;43:647–652. doi: 10.1016/j.dld.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 85.Gerke H. EUS-guided FNA: better sample with smaller needles? Gastrointest Endosc. 2009;70:1098–1100. doi: 10.1016/j.gie.2009.06.033. [DOI] [PubMed] [Google Scholar]
- 86.Madhoun M, Wani SB, Early DS, et al. The diagnostic accuracy of 22- and 25-gauge needles in EUS-FNA of solid pancreatic lesions: a meta-analysis. Gastro- intest Endosc. 2011;73(4S) doi: 10.1055/s-0032-1325992. AB154. [DOI] [PubMed] [Google Scholar]
- 87.Thomas T, Kaye PV, Ragunath K, et al. Efficacy, safety, and predictive factors for a positive yield of EUS-guided Trucut biopsy: a large tertiary referral center experience. Am J Gastroenterol. 2009;104:584–591. doi: 10.1038/ajg.2008.97. [DOI] [PubMed] [Google Scholar]
- 88.Larghi A, Verna EC, Stavropoulos SN, et al. EUS-guided trucut needle biopsies in patients with solid pancreatic masses: a prospective study. Gastrointest Endosc. 2004;59:185–190. doi: 10.1016/s0016-5107(03)02538-0. [DOI] [PubMed] [Google Scholar]
- 89.Levy MJ, Wiersema MJ. EUS-guided Trucut biopsy. Gastrointest Endosc. 2005;62:417–426. doi: 10.1016/j.gie.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 90.Gins A, Wiersema MJ, Clain JE, et al. Prospective study of a Trucut needle for performing EUS-guided biopsy with EUS-guided FNA rescue. Gastrointest Endosc. 2005;62:597–601. doi: 10.1016/j.gie.2005.04.049. [DOI] [PubMed] [Google Scholar]
- 91.Itoi T, Itokawa F, Sofuni A, et al. Puncture of solid pancreatic tumors guided by endoscopic ultrasonography: a pilot study series comparing Trucut and 19-gauge and 22-gauge aspiration needles. Endoscopy. 2005;37:362–366. doi: 10.1055/s-2004-826156. [DOI] [PubMed] [Google Scholar]
- 92.Shah SM, Ribeiro A, Levi J, et al. EUS-guided fine needle aspiration with and without trucut biopsy of pancreatic masses. JOP. 2008;9:422–430. [PubMed] [Google Scholar]
- 93.Iglesias-Garcia J, Poley JW, Larghi A, et al. Feasibility and yield of a new EUS histology needle: results from a multicenter, pooled, cohort study. Gastrointest Endosc. 2011;73:1189–1196. doi: 10.1016/j.gie.2011.01.053. [DOI] [PubMed] [Google Scholar]
- 94.Giovannini M, Genevieve MM, Iglesias-Garcia J, et al. Prospective multicenter evaluation of a novel 22G Echo-Tip ProCore histology EUS needle in patients with a solid pancreatic mass. Gastrointest Endosc. 2011;73(4S):AB152–AB153. [Google Scholar]
- 95.Iglesias-Garcia J, Abdulkader I, Larino-Nola J. Differential diagnosis of solid pancreatic masses: do ProCore histology needles improve the diagnostic yield of standard cytology needles? Gastrointest Endosc. 2012;75(4S):AB203. [Google Scholar]
- 96.Petrone MC, Arcidiacono PG, Bruno MJ, et al. Comparison between EUS-guided 19G and 22G ProCore needle biopsies in pancreatic masses: a prospective multicenter study in 72 cases. Gastrointest Endosc. 2012;75(4S):AB195. [Google Scholar]
- 97.Bang JY, Hebert-Magee S, Trevino J, et al. Randomized trial comparing the 22-gauge aspiration and 22-gauge biopsy needles for EUS-guided sampling of solid pancreatic mass lesions. Gastrointest Endosc. 2012;76:321–327. doi: 10.1016/j.gie.2012.03.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Park DH, Lee HJ, Hong SM, et al. Results of prospective randomized trial on endoscopic ultrasound (EUS) guided core biopsy of the pancreas comparing trucut needle biopsy versus new core histology needle (Chn, 19G, 22G and 25G) in a porcine model. Which needle is best? Gastrointest Endosc. 2012;75(4S):AB186. [Google Scholar]
- 99.Al-Haddad MA, Raijman I, Das A, et al. Early clinical experience with a new EUS-guided 19-gauge flexible fine needle aspiration device: a multicenter study. Gastrointest Endosc. 2012;75(4S):AB146. [Google Scholar]
- 100.Varadarajulu S, Bang JY, Hebert-Magee S, et al. Assessment of the technical performance of the flexible 19-gauge EUS-FNA needle. Gastrointest Endosc. 2012;76:336–343. doi: 10.1016/j.gie.2012.04.455. [DOI] [PubMed] [Google Scholar]
- 101.Puri R, Vilmann P, Săftoiu A, et al. Randomized controlled trial of endo-scopic ultrasound-guided fine-needle sampling with or without suction for better cytological diagnosis. Scand J Gastroenterol. 2009;44:499–504. doi: 10.1080/00365520802647392. [DOI] [PubMed] [Google Scholar]
- 102.Wallace MB, Kennedy T, Durkalski V, et al. Randomized controlled trial of EUS-guided fine needle aspiration techniques for the detection of malignant lymphadenopathy. Gastrointest Endosc. 2001;54:441–447. doi: 10.1067/mge.2001.117764. [DOI] [PubMed] [Google Scholar]
- 103.Kundu S, Conway J, Gilbert K, et al. Suction or no suction? Interval results from an ongoing prospective, partially blinded, randomized trial of endoscopic ultrasound (EUS) guided fine needle aspiration of solid lesion. Gastrointest Endosc. 2009;69:S248. [Google Scholar]
- 104.Larghi A, Noffsinger A, Dye CE, et al. EUS-guided fine needle tissue acquisition by using high negative pressure suction for the evaluation of solid masses: a pilot study. Gastrointest Endosc. 2005;62:768–774. doi: 10.1016/j.gie.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 105.Chen AM, Park WG, Friedland S, et al. Endoscopic ultrasound-guided fine needle aspiration versus fine-needle capillary sampling biopsy of pancreatic solid lesions: does technique matter? Gastrointest Endosc. 2011;73(4S):AB331. [Google Scholar]
- 106.Kothari S, Chen AM, Pai R, et al. Comparison of EUS-guided pancreas biopsy techniques using the Procore™ needle. Gastrointest Endosc. 2012;75(4S):AB145. [Google Scholar]
- 107.Wani S, Gupta N, Gaddam S, et al. A comparative study of endoscopic ultrasound guided fine needle aspiration with and without a stylet. DigDis Sci. 2011;56:2409–2414. doi: 10.1007/s10620-011-1608-z. [DOI] [PubMed] [Google Scholar]
- 108.Rastogi A, Wani S, Gupta N, et al. A prospective, single-blind, randomized, controlled trial of EUS-guided FNA with and without a stylet. Gastrointest Endosc. 2011;74:58–64. doi: 10.1016/j.gie.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 109.Sahai AV, Paquin SC, Gariépy G. A prospective comparison of endoscopic ultrasound-guided fine needle aspiration results obtained in the same lesion, with and without the needle stylet. Endoscopy. 2010;42:900–903. doi: 10.1055/s-0030-1255676. [DOI] [PubMed] [Google Scholar]
- 110.Wani S, Early DS, Kunkel J, et al. Diagnostic yield of malignancy during EUS-guided FNA of solid lesions with and without a stylet: a prospective, single blind, randomized controlled trial. Gastrointest Endosc. 2012;76:328–335. doi: 10.1016/j.gie.2012.03.1395. [DOI] [PubMed] [Google Scholar]
- 111.Leblanc JK, Ciaccia D, Al-Assi MT, et al. Optimal number of EUS-guided fine needle passes needed to obtain a correct diagnosis. Gastrointest Endosc. 2004;59:475–481. doi: 10.1016/s0016-5107(03)02863-3. [DOI] [PubMed] [Google Scholar]
- 112.Kocjan G, Chandra A, Cross P, et al. BSCC code of practice—fine needle aspiration cytology. Cytopathology. 2009;20:283–296. doi: 10.1111/j.1365-2303.2009.00709.x. [DOI] [PubMed] [Google Scholar]
- 113.Khalid A, Nodit L, Zahid M, et al. Endoscopic ultrasound fine needle aspirate DNA analysis to differentiate malignant and benign pancreatic masses. Am J Gastroenterol. 2006;101:2493–2500. doi: 10.1111/j.1572-0241.2006.00740.x. [DOI] [PubMed] [Google Scholar]
- 114.Bournet B, Souque A, Senesse P, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy coupled with KRAS mutation assay to distinguish pancreatic cancer from pseudotumoral chronic pancreatitis. Endoscopy. 2009;41:552–557. doi: 10.1055/s-0029-1214717. [DOI] [PubMed] [Google Scholar]
- 115.Takahashi K, Yamao K, Okubo K, et al. Differential diagnosis of pancreatic cancer and focal pancreatitis by using EUS— guided FNA. Gastrointest Endosc. 2005;61:76–79. doi: 10.1016/s0016-5107(04)02224-2. [DOI] [PubMed] [Google Scholar]
- 116.Maluf-Filho F, Kumar A, Gerhardt R, et al. Kras mutation analysis of fine needle aspirate under EUS guidance facilitates risk stratification of patients with pancreatic mass. J Clin Gastroenterol. 2007;41:906–910. doi: 10.1097/MCG.0b013e31805905e9. [DOI] [PubMed] [Google Scholar]
- 117.Farrell JJ, Wong JL, Donahue TR, et al. Development and validation of an EUS-FNA based predictive marker of gemcitabine response in pancreatic cancer. Gastrointest Endosc. 2011;73:249–250. [Google Scholar]
- 118.Piani C, Franchi GM, Cappelletti C, et al. Cytological Ki-67 in pancreatic endocrine tumours: an opportunity for pre-operative grading. Endocr Relat Cancer. 2008;15:175–181. doi: 10.1677/ERC-07-0126. [DOI] [PubMed] [Google Scholar]