Abstract
Background:
Vilazodone is the latest US Food and Drug Administration approved antidepressant agent available in the USA. Its putative mechanism of antidepressant action enhances the release of serotonin across the brain's serotonergic pathways specifically by inhibiting the serotonin transporter, similar to a selective serotonin reuptake inhibitor (SSRI), and simultaneously stimulating serotonin-1a receptors via partial agonism, similar to the anxiolytic bus-pirone. This combined activity in the single vilazodone agent has been termed by the authors as being a serotonin partial agonist and reuptake inhibitor or (SPARI).
Methods:
A MEDLINE and Internet search was conducted and the resultant preclinical and clinical evidence was reviewed. The authors attempt to review laboratory data, animal model data and human trial data to develop a translational theory on the mechanism of antidepressant action of this agent and also its adverse effect potential.
Results:
Randomized, controlled empirical data for vilazodone have gained it approval for treating major depressive disorder. It combines two well known pharmacodynamic mechanisms of serotonergic action into a novel agent. Although no head-to-head studies against other antidepressants have been published, the efficacy data for vilazodone appear comparable to other known antidepressants, with similar gastrointestinal side effects to SSRI or serotonin norepinephrine reuptake inhibitor (SNRI) antidepressants, but possibly with a lower incidence of sexual side effects and weight gain.
Discussion:
Vilazodone will lend itself to the current armamentarium in the treatment of major depressive disorder and may hold promise for patients who cannot tolerate other antide-pressants. Its unique SPARI mechanism of action could also be efficacious for patients who do not respond to SSRI or SNRI antidepressant monotherapies.
Keywords: antidepressant, major depressive disorder, serotonin, vilazodone
Introduction
Vilazodone is the latest US Food and Drug Administration (FDA) approved antidepressant treatment (ADT). This paper reviews preclinical pharmacokinetic information, pharmacodynamic information, and finally, the current publicly available clinical data for this product. The goal of this brief review is also to link preclinical to clinical data in order to construct a theoretical model on the proposed mechanism of antidepressant action of vilazodone.
Clinicians have been using the same mechanistic approaches to the treatment of major depressive disorder (MDD) since the 1950s by boosting monoamine (serotonin [5HT], norepinephrine or dopamine) activity, mostly by blocking reuptake transporters, originally with tricyclic antidepressants and in recent years with selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs). The National Institute of Mental Health's STAR*D trial suggests that remission from a prototypical agent of the SSRI class occurs about one-third of the time with initial monotherapy in patients with MDD, and each subsequent ADT yields less favorable outcomes as treatment-resistant depression increases. After four successive ADTs, about two-thirds of patients finally achieve remission, but many of these do not sustain remission for more than a few months [Rush et al. 2006]. Thus, one-third of patients with MDD continue to have significant symptoms after treatment with a sequence of agents for about a year, and many of those who achieve remission do not sustain it. Given these modest results, researchers continue to look for new ways to treat depression and with novel pharmacologic mechanisms.
In the absence of a remarkable breakthrough drug in the area of nonmonoamine agents, that is, hormonal, peptide, genetic, neuromodulation [Schwartz, 2010], clinicians have resorted to higher levels of rational polypharmacy in order to gain full remission when monotherapies fail by using combination drug treatment earlier and earlier in treatment selection [Blier et al. 2010; Rush, 2010; Schwartz and Rush, 2007]. To boost antidepressant efficacy in patients whose condition fails to respond adequately to an SSRI, numerous second-generation atypical antipsychotics (SGAs) are now approved: aripiprazole, quetiapine, quetiapine XR, olanzapine—fluoxetine combination, but with potential additional side effects and costs [Weisler et al. 2009; Corya et al. 2006].
A unique mechanistic approach is that of vilazodone, an agent that combines two mechanisms in a single drug, namely that of the SSRIs with 5HT1A receptor partial agonist actions, or a serotonin partial agonist reuptake inhibitor (SPARI). Specifically, this agent increases the availability and activity of the neurotransmitter serotonin and its neuropathways. Vilazodone blocks the serotonin reuptake pump (serotonin transporter or SERT), desensitizes serotonin receptors (especially 5HT1A autoreceptors), and therefore presumably increases serotonergic neurotransmission. Its partial agonist actions at presynaptic somatodendritic 5HT1A autoreceptors may theoretically enhance serotonergic activity and contribute to antidepressant actions as well [Stahl, 2011; Hudziak, 2005; Pies, 1998]. This partial agonist action also occurs at the level of the postsynaptic 5HT1A receptor, which may theoretically diminish sexual dysfunction [Hudziak, 2005; Pies, 1998]. This effect has been noted in studies where the 5HT1A receptor partial agonist buspirone is used [Othmer and Othmer, 1987]. In support of this theoretical information, 5HT1A receptor agonism animal models suggest possible rapid onset of antide-pressant efficacy, and more robust serotonergic actions, suggesting greater antidepressant efficacy compared with SSRIs [Dawson and Watson, 2009; Hogg and Dalvi, 2004; Duxon et al. 2000]. However, these preclinical suggestions have yet to be confirmed specifically for vilazodone in human clinical trials. Vilazodone, with SPARI actions, has recently garnered FDA approval for treating MDD as of January 2011 (http://www.drugs.com/history/viibryd.html) on the basis of regulatory placebo-controlled trials that show its antidepressant efficacy and general tolerability profile. However, the lack of head-to-head comparisons with other antidepressants, especially SSRIs, make potential efficacy and tolerability comparisons to known ADT agents difficult. What is known about the pharmacokinetics, pharmacodynamics and currently available clinical trial results of vilazodone will be reviewed here.
Vilazodone pharmacodynamics
Vilazodone is a combined SSRI and 5HT1A receptor partial agonist [Sorbera et al. 2001]. The authors use the term SPARI to define this class of ADT [Stahl, 2011]. This mechanistic way of treating MDD should look familiar to clinicians because it would be similar to the common depression treatment strategy of augmenting SSRI monotherapy (fluoxetine, sertraline, paroxetine, among others) with the commercially available 5HT1A receptor partial agonist anxiolytic, buspirone [Barowsky and Schwartz, 2006]. Buspirone is currently approved for treating generalized anxiety disorder [Stahl, 2011]. In fact, the STAR*D trial studied patients who did not respond to treatment with citalopram, comparing augmentation with either buspirone or with bupropion sustained release, and found no significant differences in remission rates between these two combination treatments [Trivedi et al. 2006].
In theory, as there are limited animal models and no direct head-to-head comparative trials available for vilazodone, a single monotherapy agent like vilazodone that combines the same pharmacologic actions as the combination of an SSRI with buspirone would be able to provide the potential efficacy benefits of this combination, particularly if administered early in treatment [Stahl, 2010, 2009]. Instead of starting with SSRI monotherapy with dose escalation for 12 weeks, waiting for it to potentially fail (which occurred in two-thirds of cases in the STAR*D trial) followed by the subsequent addition of buspirone for another several weeks, vilazodone allows immediate, simultaneous combination of these two pharmacodynamic properties at the outset of treatment. Because the product is not as complex or risky as an second-generation antipsychotic (SGA) augmentation approach, it would in theory produce a smaller side effect burden, especially given its absence of metabolic and movement disorders. A full discussion of the clinical effectiveness and adverse effects of vilazodone is forthcoming. Unfortunately, these considerations and comparisons to STAR*D outcomes remain merely theoretical since there are no studies reporting a comparison of vilazodone with other active treatments or combinations of treatments.
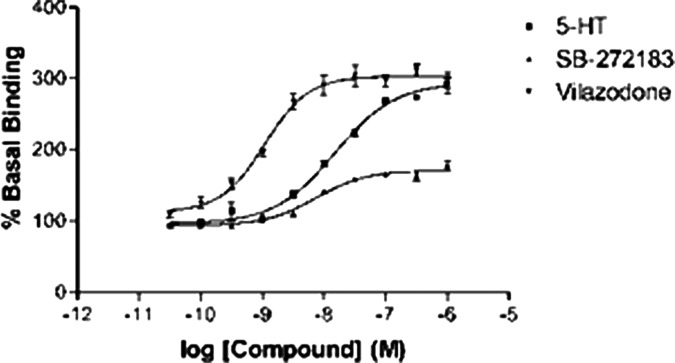
In preclinical animal models, vilazodone was suggestive of a potential rapid onset ADT [Page et al. 2002; Bartoszyk et al. 1997] in that rodent vocalization, forced swim test, elevated maze, and predator-induced stress models appeared positive for antidepressant effects [Adamec et al. 2004; Treit et al. 1993; Treit, 1990; Pellow et al. 1985]. In vitro tests demonstrated that vilazodone has serotonin neurotransmission enhancing potential, in part because of robust blockade of the SERT [Roberts et al. 2005] (Figure 1) and in part because of direct partial agonist actions on 5HT1A receptors (Figure 2). Animal model (rat) analysis of vilazodone supports the 5HT1A receptor partial agonism serotonergic property [Hughes et al. 2005; Heinrich et al. 2004]. In fact, one such study revealed that vilazodone increased cortical 5HT levels more than an SSRI (fluoxetine) alone, which makes sense in that two serotonergic mechanisms should have additive cortical effects. Whether this means improved onset of efficacy or tolerability remains to be investigated in future trials [Page et al. 2002].
Figure 1.
Vilazodone promotes dose-dependent serotonin transporter inhibition. 5-HT, serotonin. (Reproduced with permission from Dawson and Watson [2009].)
Figure 2.
Vilazodone promotes dose-related binding and agonism on serotonin 1a (5HT1a) receptors. (Reproduced with permission from Dawson and Watson [2009].)
To further demonstrate how this theoretical serotonergic model might create human antidepressant effects, several dynamic steps must occur in the brain's serotonin neurocircuitry to allow anti-depressant effects. First, the central nervous system has to be exposed to an antidepressant capable of increasing 5HT levels robustly over several weeks [Stahl, 2008]. For example, SSRIs yield an increase in synaptic 5HT through SERT reuptake inhibition. This produces a desensitization and/or downregulation of presynaptic 5HT1A autoreceptors. Because the autoreceptors are now overstimulated, the 5HT neuron interprets this initially as toxic activity. As these autoreceptors become less effective because of overstimulation and desensitization, they offer less autoreceptor inhibition to the 5HT neuron and excess 5HT is released at the neuron terminals as a result. By directly agonizing the 5HT1A receptors in the central nervous system, vilazodone likely allows a faster, or greater, volume of 5HT1A receptor desensitization/downregulation upfront. This may lend more additive or synergistic 5HT effects than SSRI alone.
Thus, the rationale behind this pharmacodynamic combination is to yield a more rapid and larger scale desensitization of the somatodendritic 5HT1A autoreceptor system in the MDD brain. This mechanism essentially lowers the 5HT neurons' ability to regulate 5HT output, thus increasing 5HT neuronal firing and activity. This more aggressive, or additive, 5HT facilitation approach may then also directly stimulate postsynaptic 5HT1A heteroreceptors downstream (which instead of neuronal inhibition like the 5HT1A autoreceptors, may actually promote even more neuronal firing and activity of 5HT or other monoamine neurons) [Dawson and Watson, 2009].
Although this theoretical thinking underlies the development of vilazodone as a potentially novel antidepressant drug, there is as yet no clinical human evidence of rapid onset or more robust antidepressant action compared with SSRI or SNRI antidepressants. Furthermore, the presence of gastrointestinal side effects means that slower titration of vilazodone is necessary, starting at a dose lower than the maintenance dose for several days (to a few weeks), thus potentially masking any rapid onset effect in patients.
Vilazodone pharmacokinetics
Vilazodone's molecular structure is shown in Figure 3. According to the official FDA sanctioned Package Insert [Forest Pharmaceuticals, 2011] this drug is initially dosed at 10 mg/day in the morning for 1 week then dose escalated to 20 mg/day for a second week with the final titration to a daily dose of 40 mg. It comes in 10, 20 and 40 mg tablet strengths. This drug must be taken with food or it loses 50% of its bioavailability. There are no dosing changes required in patients with renal or hepatic conditions and a gradual withdrawal is suggested to avoid serotonin discontinuation syndrome. It is clinically contraindicated for use with MAOi ADT. Vilazodone is metabolized extensively by the hepatic p450 3A4 enzyme system. Its dose should be reduced to 20 mg/day with concomitant use of any potent 3A4 inhibitors, that is, erythromycin, amiodarone, protease inhibitors, or ketoconazole. Vilazodone's activity is due primarily to the parent drug and there are no clear active metabolites. The pharmacokinetics of vilazodone (5–80 mg) are dose proportional. Steady state is achieved in about 4 days of consistent dosing. Elimination of vilazodone is primarily by hepatic metabolism (3A4) with a terminal half life of approximately 25 h. It is 96–99% protein bound so it may disrupt digoxin or coumadin binding temporarily because it displaces these drugs into a nonprotein bound, free plasma state, which increases their availability and activity.
Figure 3.
Vilazodone molecular structure image. (Reproduced with permission from Dawson and Watson [2009].)
Clinical studies
Initial human studies showed sleep architecture changes consistent with other antidepressants. [Murck et al. 2001]. Dawson and Watson's [Dawson and Watson, 2009] review outlines phase II studies in a succinct manner. Vilazodone was administered to a total of 369 healthy volunteers and 1163 patients with depression but failed to demonstrate significant efficacy against placebo initially. Of note, active comparator studies have also failed to demonstrate efficacy because of failed clinical trials in which placebo effects were as great as drug effects. However, a subsequent phase III clinical trial demonstrated statistical significance against placebo for 410 patients with MDD. A new FDA drug application was made in 2009 (Bear Stearns Healthcare Conference; Newton, Massachusetts, USA; Business Wire, September 2007). Secondary, regulatory trials again showed efficacy and tolerability and vilazodone was FDA approved for MDD in January 2011.
The official company data and FDA Package Insert reveal positive regulatory, confirmatory trial information. At the time of this article, two peer-reviewed papers outline randomized, controlled trial in which 891 patients were studied. Significant improvements in multiple depression rating scales were noted when compared with placebo. Diarrhea, nausea, and somnolence were the greatest side effects noted [Khan et al. 2011]. There were clinically no significant differences for men or women in regards to sexual dysfunction outcome measures [Rickels et al. 2009]. Vilazodone efficacy in MDD was further established in two 8-week, multicenter, randomized, double-blind, placebo-controlled studies in adult (18–70 years of age) outpatients who met the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) [APA, 2000] criteria for MDD. Vilazodone was superior to placebo in the improvement of depressive symptoms, and evaluation of population subgroups based on age, gender, and race did not reveal any clear evidence of differential responsiveness. The most common side effects of vilazodone over placebo included diarrhea, nausea, and dry mouth and it does carry an increased lethality warning in young adult patients. It is not approved for pediatric depression. No blood laboratory or electrocardiogram changes were noted and no tests are required while administering this ADT. In these acute 8-week studies no abnormal weight gain or metabolic adverse effects were noted [Forest Pharmaceuticals, 2011]. Long-term, 52-week data are not available as yet. Finally, sexual dysfunction adverse effects were minimal (1–2% over placebo rates) [Stahl, 2011].
Other clinical applications
Given that other agents with SSRI activity and 5HT1A receptor activity carry FDA approval for depression, generalized anxiety disorder, obsessive—compulsive disorder, social anxiety disorder, panic disorder, post-traumatic stress disorder (PTSD), eating disorders, and premenstrual disorders [Stahl, 2011, 2008], it would follow that vilazodone conceptually has the pharmacodynamic mechanisms necessary to alleviate symptoms attributed to these disorders as well. Interestingly, one animal model study conducted by Adamec and colleagues [Adamec et al. 2004] revealed that rodents treated with therapeutic levels of vilazodone had fewer poststress (predator-induced) clinical symptoms. Vilazodone appeared to lower the risk of animal model PTSD symptoms, in particular there was a reduction in post-trauma hypervigiliance, which is part of the triad of human PTSD symptoms (re-living, avoidance, hyperarousal) [APA, 2000].
The dose of vilazodone must be more fully explored. A clear ‘no effect’ dose has not been established and a 20 mg dose trial will be required as a condition of approval, as will studies in children and longer-term relapse prevention studies in depression. Also, because 40 mg only occupies an estimated 50% of SERT and 5HT1A receptors [Rabiner et al. 2000], it seems reasonable to test doses in the 50–80 mg/day range by slow upward titration, especially for treatment-resistant cases of depression and other related disorders.
Conclusions
Vilazodone has been approved for treatment of MDD. The usual treatment guidelines [APA, 2010] should be followed to make an accurate diagnosis, ruling out bipolarity, substance misuse, and personality disorders prior to its use. If an ADT is warranted, monotherapy with an approved agent with a good risk—benefit, or efficacy—tolerability profile should be chosen. Although vilazodone may be acceptable as a first-line agent, and its combined SPARI mechanism offers a unique initial antidepressant approach when compared with SSRIs and SNRIs, vilazodone will likely be used in patients who do not respond to an SSRI or an SNRI or do not tolerate these agents given their prevalence and ease of use. Vilazodone may be especially useful if the patient develops sexual dysfunction, weight gain or increased blood pressure on an SSRI or an SNRI. Vilazodone should strongly be considered secondarily if patients cannot tolerate or risk intervention with an atypical second-generation antipsychotic because of weight gain, sedation, extrapyramidal symptoms, or dyslipidemia.
Footnotes
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Thomas L. Schwartz, MD is an associate professor of psychiatry at the SUNY Upstate Medical University. Over the past 12 months (May 2010-May 2011) Dr Schwartz has served as a Consultant to PamLab. He has served on speakers bureaus for Pfizer Inc., Wyeth Pharmaceuticals, AstraZeneca, and Merck, and has received research and/or grant support from Cephalon, Cyberonics, and Forest.
Umar Siddiqui, MD is a research coordinator at the SUNY Upstate Medical University's Treatment Resistant Depression and Anxiety Disorders Program. He has no conflicts of interest to disclose.
Stephen M. Stahl, MD, PhD is an adjunct professor of psychiatry at the University of California, San Diego School of Medicine and an honorary visiting senior fellow at the University of Cambridge, UK. Over the past 12 months (January 2009-January 2010) Dr Stahl has served as a Consultant to Allergan, Astra Zeneca, BioMarin, BioVail, Boehringer Ingelheim, Bristol Myers-Squibb, Cenerex, Covance, Cypress Bioscience, Dianippon, Eisai, Eli Lilly, Forest, GlaxoSmith Kline, Labopharm, Lundbeck, Marinus, Meda Corp, Meiji, Merck, Novartis, Pfizer, Pfizer Canada, Pierre Fabre, PamLab, Prexa Pharmaceuticals, Propagate Pharma, Royalty Pharma, Sanofi, Schering Plough Corporation, Shire, SK Corporation, Soffinova, Solvay, Vanda, and Wyeth. He has served on speakers bureaus for Pfizer Inc., Wyeth Pharmaceuticals and Schering Plough Corporation and has received research and/or grant support from Astra Zeneca, Boehringer Ingelheim, Bristol Myers-Squibb, Cephalon, Dainippon, Eli Lilly, Forest, Lundbeck, Novartis, PamLabs, Pfizer, Pfizer Canada, Pharmasquire, Sanofi Aventis, Schering Plough, Shire, and Wyeth.
References
- Adamec R., Bartoszyk G., Burton P. (2004) Effects of systemic injections of vilazodone, a selective serotonin reuptake inhibitor and serotonin 1A receptor agonist, on anxiety induced by predator stress in rats. Eur J Pharmacol 504: 65–77 [DOI] [PubMed] [Google Scholar]
- APA. (2000) American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 4th edn text revision, American Psychiatric Publishing: Washington, DC [Google Scholar]
- APA. (2010) American Psychiatric Association practice guideline for major depressive disorder in adults. Am J Psychiatry 150: 1–26 [DOI] [PubMed] [Google Scholar]
- Barowsky J., Schwartz T.L. (2006) An evidence based approach to augmentation and combination strategies for treatment resistant depression. Psychiatry (Edgmont) 3: 42–61 [PMC free article] [PubMed] [Google Scholar]
- Bartoszyk G.D., Hegenbart R., Ziegler H. (1997) EMD 68843, a serotonin reuptake inhibitor with selective presynaptic 5-HT1A receptor agonistic properties. Eur J Pharmacol 322: 147–153 [DOI] [PubMed] [Google Scholar]
- Blier P., Ward H.E., Tremblay P., Laberge L., Hébert C., Bergeron R. (2010) Combination of antidepressant medications from treatment initiation for major depressive disorder: A double-blind randomized study. Am J Psychiatry 167: 281–288 [DOI] [PubMed] [Google Scholar]
- Corya S.A., Perlis R.H., Keck P.E., Jr, Lin D.Y., Case M.G., Williamson D.J., et al. (2006) A 24-week open-label extension study of olanzapine-fluoxetine combination and olanzapine monotherapy in the treatment of bipolar depression. J Clin Psychiatry 67: 798–806 [DOI] [PubMed] [Google Scholar]
- Dawson L.A., Watson J.M. (2009) Vilazodone: A 5-HT1A receptor agonist/serotonin transporter inhibitor for the treatment of affective disorders. CNS Neurosci Thera 15: 107–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duxon M.S., Starr K.R., Upton N. (2000) Latency to paroxetine-induced anxiolysis in the rat is reduced by co-administration of the 5-HT1A receptor antagonist WAY100635. Br J Pharmacol 130: 1713–1719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forest Pharmaceuticals (2011) Vilazodone FDA Package Insert, New York, USA.
- Heinrich T., Bottcher H., Gericke R., Bartoszyk G.D., Anzali S., Seyfried C.A., et al. (2004) Synthesis and structure—activity relationship in a class of indolebutylpiperazines as dual 5-HT(1A) receptor agonists and serotonin reuptake inhibitors. J Med Chem 47: 4684–4692 [DOI] [PubMed] [Google Scholar]
- Hogg S., Dalvi A. (2004) Acceleration of onset of action in schedule-induced polydipsia: Combinations of SSRI and 5-HT1A and 5-HT 1B receptor antagonists. Pharmacol Biochem Behav 77: 69–75 [DOI] [PubMed] [Google Scholar]
- Hudziak J., Waterman C.S. (2005) Buspirone, In Kaplan and Sadock's comprehensive textbook of psychiatry (8th edn) (Sadock B.J., Sadock V.A., Eds.), Lipincott Williams & Wilkins: Philadelphia, New York [Google Scholar]
- Hughes Z.A., Starr K.R., Langmead C.J., Hill M., Bartoszyk G.D., Hagan J.J., et al. (2005) Neurochemical evaluation of the novel 5-HT1A receptor partial agonist/serotonin reuptake inhibitor, vilazodone. Eur J Pharmacol 510: 49–57 [DOI] [PubMed] [Google Scholar]
- Khan A., Cutler A.J., Kajdasz D.K., Gallipoli S, Athanasiou M, Robinson D.S., et al. (2011) A Randomized, Double-Blind, Placebo-Controlled, 8-Week Study of Vilazodone, a Serotonergic Agent for the Treatment of Major Depressive Disorder. J Clin Psychiatry 72: 441–447 [DOI] [PubMed] [Google Scholar]
- Murck H., Frieboes R.M., Antonijevic I.A., Steiger A. (2001) Distinct temporal pattern of the effects of the combined serotonin-re-uptake inhibitor and 5-HT1A agonist EMD 68843. Psychopharmacology 155: 187–192 [DOI] [PubMed] [Google Scholar]
- Othmer E., Othmer S.C. (1987) Effect of buspirone on sexual dysfunction in patients with generalized anxiety disorder. J Clin Psychiatry 48: 201–203 [PubMed] [Google Scholar]
- Page M.E., Cryan J.F., Sullivan A., Dalvi A., Saucy B., Manning D.R., et al. (2002) Behavioral and neurochemical effects of 5-{4-[4-(5-Cyano-3-indolyl)-butyl)-butyl]-1-piperaziny}-benzofuran-2-carboxamide (EMD 68843): A combined selective inhibitor of serotonin reuptake and 5-hydroxytryptamine 1A receptor partial agonist. J Pharmacol Exp Ther 302: 1–8 [DOI] [PubMed] [Google Scholar]
- Pellow S., Chopin P., File S.E., Briley M. (1985) Validation of open: Closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Method 14: 149–167 [DOI] [PubMed] [Google Scholar]
- Pies R. (1998) Handbook of Essential Psychopharmacology, American Psychiatric Press Inc.: Washington, DC [Google Scholar]
- Rabiner E.A., Gunn R.N., Wilkins M.R., Sargent P.A., Mocaer E., Sedman E., et al. (2000) Drug action at the 5-HT(1A) receptor in vivo: Autoreceptor and postsynaptic receptor occupancy examined with PET and [carbonyl-(11)C]WAY-100635. Nucl Med Biol 27: 509–513 [DOI] [PubMed] [Google Scholar]
- Rickels K., Athanasiou M., Robinson D.S., Gibertini M., Whalen H., Reed C.R. (2009) Evidence for efficacy and tolerability of vilazodone in the treatment of major depressive disorder: A randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 70: 326–333 [DOI] [PubMed] [Google Scholar]
- Roberts C., Hagan J.J., Bartoszyk G.D., Kew J.N. (2005) Effect of vilazodone on 5-HT efflux and re-uptake in the guinea-pig dorsal raphe nucleus. Eur J Pharmacol 517: 59–63 [DOI] [PubMed] [Google Scholar]
- Rush A. (2010) Combining antidepressant medications: A good idea?. Am J Psychiatry 167: 241–243 [DOI] [PubMed] [Google Scholar]
- Rush A.J., Trivedi M.H., Wisniewski S.R., Nierenberg A.A., Stewart J.W., Warden D., et al. (2006) Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiatry 163: 1905–1917 [DOI] [PubMed] [Google Scholar]
- Schwartz T.L., Rashid A. (2007) Augmentation and Combination Pharmacotherapy trends in major depressive disorder: Results of a brief survey of psychiatrists. P&T 32: 28–31 [Google Scholar]
- Schwartz T.L., Stah S.M. (2010) Optimizing Antidepressant Management of Depression: current Status and Future Perspectives, Vol. 27, 9th edn, Karger: Basel, pp. 254–267 [Google Scholar]
- Sorbera L.A., Rabasseda X., Silvestre J., Castaner J. (2001) Vilazodone hydrochloride—antide-pressant—5-HT1A partial agonist—5-HT reuptake inhibitor. Drugs Future 26: 247–252 [Google Scholar]
- Stahl S. (2008) Stahl's Essential Psychopharmacology: Neuroscientific Basis and Practical Applications, 3rd edn, Cambridge University Press: Cambridge [Google Scholar]
- Stahl S. (2009) Combining antidepressant therapies from the initiation of treatment: A paradigm shift for major depression. J Clin Psychiatry 70: 1493–1494 [DOI] [PubMed] [Google Scholar]
- Stahl S. (2010) Enhancing outcomes from major depression: Using antidepressant combination therapies with multifunctional pharmacologic mechanisms from the initiation of treatment. CNS Spectrums 15: 79–94 [DOI] [PubMed] [Google Scholar]
- Stahl S. (2011) Essential Psychopharmacology: the Prescriber's Guide, 4th edn, Cambridge University Press: Cambridge [Google Scholar]
- Treit D. (1990) A comparison of anxiolytic and nonanxiolytic agents in the shock-probe burying test for anxiolytics. Pharmacol Biochem Behav 36: 203–205 [DOI] [PubMed] [Google Scholar]
- Treit D., Menard J., Royan C. (1993) Anxiogenic stimuli in the elevated plus-maze. Pharmacol Biochem Behav 44: 463–469 [DOI] [PubMed] [Google Scholar]
- Trivedi M.H., Fava M., Wisniewski S.R., Thase M.E., Quitkin F., Warden D., et al. for the STAR*D Study Team (2006) Medication augmentation after the failure of SSRIs for depression. N Engl J Med 354: 1243–1252 [DOI] [PubMed] [Google Scholar]
- Weisler R., Joyce M., McGill L., Lazarus A., Szamosi J. Eriksson, H. Moonstone Study Group. (2009) Extended release quetiapine fumarate monotherapy for major depressive disorder: Results of a double-blind, randomized, placebo-controlled study. CNS Spectr 14: 299–313 [DOI] [PubMed] [Google Scholar]