Abstract
Cannabis is a complex plant, with major compounds such as delta-9-tetrahydrocannabinol and cannabidiol, which have opposing effects. The discovery of its compounds has led to the further discovery of an important neurotransmitter system called the endocannabinoid system. This system is widely distributed in the brain and in the body, and is considered to be responsible for numerous significant functions. There has been a recent and consistent worldwide increase in cannabis potency, with increasing associated health concerns. A number of epidemiological research projects have shown links between dose-related cannabis use and an increased risk of development of an enduring psychotic illness. However, it is also known that not everyone who uses cannabis is affected adversely in the same way. What makes someone more susceptible to its negative effects is not yet known, however there are some emerging vulnerability factors, ranging from certain genes to personality characteristics. In this article we first provide an overview of the biochemical basis of cannabis research by examining the different effects of the two main compounds of the plant and the endocannabinoid system, and then go on to review available information on the possible factors explaining variation of its effects upon different individuals.
Keywords: Cannabis, delta-9-tetrahydrocannabinol, cannabidiol, tetrahydrocannabivarin, endocannabinoids, individual sensitivity to cannabis
Introduction
Cannabis is a complex plant with over 400 chemical entities of which more than 60 of them are cannabinoid compounds, some of them with opposing effects. Cannabis is also the most widely used illicit drug in the world and its use has been associated with various mental health problems, particularly in the young [Hall and Degenhardt, 2007; Degenhardt et al. 2010]. Despite the links made between its use and the development of mental health problems, it is also known that not everyone who uses it is affected adversely in the same way. In this article we will provide an overview of the different effects of the two main compounds of the plant, as well as its effects upon different sections of the population. Before presenting the available evidence in the literature on the reasons for the varying effects of cannabis in different individuals, we will first review the present knowledge on the biochemistry of the cannabis plant and the endocannabinoid system.
Brief history of the biochemistry of the cannabis plant
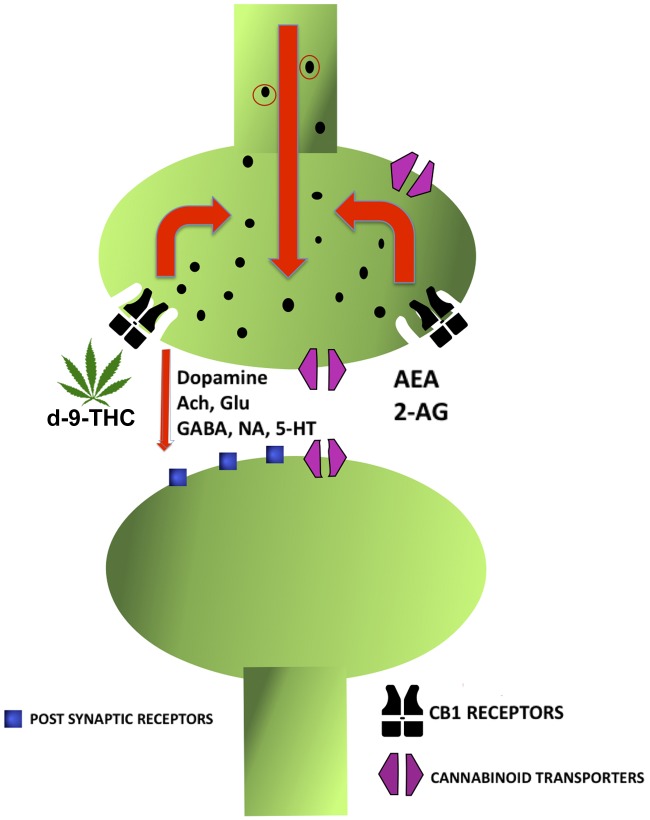
Even though cannabis has been used and cultivated by mankind for at least 6000 years [Li, 1973] our current knowledge on its pharmacological properties is based on studies which have taken place only since the end of the nineteenth century. The very first compound isolated in pure form from the plant was cannabinol [Wood, 1899]. It was initially wrongly assumed to be the main active compound of the plant responsible for its psychoactive effects [Mechoulam and Hanus, 2000]. The second compound found was cannabidiol (CBD) by Mechoulam and Shvo [Mechoulam and Shvo, 1963]. The following year in 1964, Gaoni and Mechoulam isolated the main active compound, delta-9-tetrahydrocannabinol (d-9-THC) (Figure 1) [Gaoni and Mechoulam, 1964].
Figure 1.
Chemical structures of delta-9-tetrahydrocannabinol and cannabidiol.
Cannabinoid receptor system
Another cornerstone in cannabinoid research was the identification of the specific binding sites of d-9-THC in the brain [Devane et al. 1988], which was followed by the cloning of cannabinoid 1 receptor (CB1R) [Matsuda et al. 1990]. This system was named the ‘cannabinoid receptor system’ due to the binding affinity of d-9-THC to these receptors as a partial agonist. Shortly after, a second receptor, CB2R, was discovered [Munro et al. 1993]. Around the same time, the existence of the endocannabinoid system was confirmed by Devane and colleagues following the extraction of a molecule, an ethanolamine of arachidonic acid (AEA), which bound to these receptors [Devane et al. 1992]. This endocannabinoid agonist was given the name ‘anandamide’, based on a Sanskrit word meaning ‘bliss’. Mechoulam and colleagues isolated the second endocannabinoid neurotransmitter, 2-arachidonylglycerol (2-AG), 3 years later [Mechoulam et al. 1995]. Research in more recent years has shown that d-9-THC, as a partial agonist, resembles anandamide in its CB1 affinity, albeit with less efficacy than anandamide, whilst displaying even lower efficacy at CB2Rs than at CB1Rs in vitro [Pertwee, 2008].
Cannabinoid 1 and 2 receptors
CB1Rs are mainly in the brain, particularly in the substantia nigra, the basal ganglia, limbic system, hippocampus and cerebellum, but are also expressed in the peripheral nervous system, liver, thyroid, uterus, bones and testicular tissue [Russo and Guy, 2006; Pagotto et al. 2006; Pertwee, 2006]. CB2Rs are mostly expressed in immune cells, spleen and the gastrointestinal system, and to some extent in the brain and peripheral nervous system [Izzo, 2004; Pertwee, 2006]. Interestingly, both CB1 and CB2Rs are also found in human placenta and have been shown to play a role in regulating serotonin transporter activity [Kenney et al. 1999]. Indeed further research has revealed that the endocannabinoid system also plays a significant role in various aspects of human reproduction [Taylor et al. 2010].
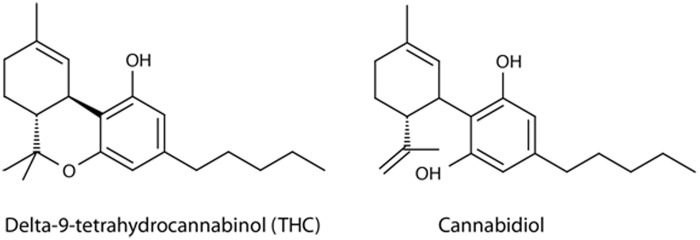
In the brain, CB1Rs are found at the terminals of central and peripheral neurons, where they mostly mediate inhibitory action on ongoing release of a number of excitatory and inhibitory dopaminergic, gamma-aminobutyric acid (GABA), glutamatergic, serotoninergic, noradrenalin and acetylcholine neurotransmitter systems (Figure 1). Because of the involvement of these systems they affect functions such as cognition, memory, motor movements and pain perception [Howlett et al. 2002]. The release of endocannabinoids, such as AEA and 2-AG, from the postsynaptic sites to the synaptic cleft occur in response to elevation of intracellular calcium and they then act as retrograde neurotransmitters on presynaptically located CB1Rs to maintain homeostasis and prevent the excessive neuronal activity [Howlett et al. 2002; Terry et al. 2009]. They are then rapidly removed from the extracellular space by cannabinoid transporters, often referred to as anandamide membrane transporters, which facilitate their breakdown by internalizing the molecule and allowing access to fatty acid amide hydrolase [Pertwee, 2010]. Despite its significance in the endocannabinoid system, little is known about the cannabinoid transporters.
When cannabis is used, d-9-THC as a partial agonist binds to CB1R and acts in a less selective manner in inhibiting the release of neurotransmitters normally modulated by endocannabinoids such as AEA and 2-AG. It has been putatively suggested that it may also increase the release of dopamine, glutamate and acetylcholine in certain brain regions, possibly by inhibiting the release of an inhibitory neurotransmitter like GABA onto dopamine, glutamate or acetylcholine-releasing neurons [Bhattacharyya et al. 2009a] (Figure 2).
Figure 2.
CB1 receptors - effects of endocannabinoids and d-9-THC Release of Anandamide (AEA) and 2- arachidonoylglycerol (2-AG) to inhibit glutamate (Glu), Gamma-aminobutyric acid (GABA), acetylcholine (Ach), dopamine, noradrenaline (NA) and serotonin (5-HT). Endocannabinoids are removed from the extracellular space by cannabinoid transporters.
However, the functionalities of the CB1Rs are not always straightforward due to complex interactions with the other neurotransmitter systems. These are related to CB1Rs and CB2Rs being members of the super family of G-protein-coupled receptors (GPCRs) [Pertwee et al. 2010]. GPCRs sense an external molecule outside the nerve cell and by contact with the molecule can signal transduction pathways, which ultimately lead to cellular responses. External ligands such as d-9-THC, various synthetic compounds and endocannabinoids such as anandamide can activate these receptors [Pertwee et al. 2010]. Interestingly some alkylamides from the Echinacea plant can also bind to the CB2Rs even more strongly than the endogenous cannabinoids [Raduner et al. 2006]. The mechanism of action for CBD is not yet clear, as this compound does not bind to CB1Rs or CB2Rs [Tsou et al. 1998; Hayakawa et al. 2008].
Normally GPCRs are linked together to form a receptor complex. However, the signalling effects can be complex due to CB1Rs forming heteromers, which can be defined as having different parts such as subunits, with two or more other GPCRs, particularly if they are densely expressed in the same neuron. For instance, a CB1R can form a heteromer with dopamine D2 receptor, or in another instance it can also form a heteromer with two other receptors such as dopamine D2 and adenosine A2A [Navarro et al. 2008]. Interestingly, as a result, ligand bindings can produce unexpected pharmacological effects. For instance, in a heteromer complex, not only the antagonist of CB1R but also the other receptor antagonist can block the inhibitory effect of CB1R agonist. This has been demonstrated by Marcellino and colleagues when the CB1R antagonist rimonabant and the specific A2AR antagonist MSX-3 blocked the inhibitory effect of CB1 agonist on D2-like receptor agonist induced hyperlocomotion in rats [Marcellino et al. 2008]. Receptor heteromers provide better understanding of how these different neurotransmitter systems interact with each other. Compelling evidence for the existence of CB1R heteromers in striatal dendritic spines of striatal GABAergic efferent neurons, particularly at a postsynaptic location, has also been reported [Ferré et al. 2009]. The authors propose that it is likely that functional CB1–A2A–D2 receptor heteromers can be found in the dendritic spines of GABAergic enkephalinergic neurons, where they are highly coexpressed, and their analysis provides new information on the role of endocannabinoids in striatal function, which can be considered as retrograde signals that inhibit neurotransmitter release. Further evidence for the existence of D2 and CB1Rs in ventral striatum is provided by electron microscopy analysis, which confirms the relevance to the rewarding and euphoric, as well as motor effects produced by cannabis, by enhancing dopamine levels particularly in the nucleus accumbens [Pickel et al. 2006]. CB1R expression in the striatum and their role in differential signalling between different developmental stages and sensorimotor and associative/limbic circuits have also been demonstrated in a recent study [van Waes et al. 2012].
Most recently it has been shown that CB2Rs form heteromers with CB1Rs in the brain and the agonist coactivation of CB1Rs and CB2Rs results in negative crosstalk in AKT1 phosphorylation and neurite outgrowth [Callén et al. 2012]. The authors point out that there is a bidirectional cross antagonism which involves the antagonists of either receptor to block the other. It is suggested that these data illuminate the mechanism by which CB2Rs can negatively modulate CB1R function.
In more recent years, three other novel receptor candidates, GPR18, GPR19 and GPR55, have been discovered, as well as non-CB1Rs and non-CB2Rs, but knowledge on these systems is incomplete and the discussion on whether or not they meet the criteria to qualify as receptors or channels is ongoing [Mackie and Stella, 2006; Pertwee et al. 2010; Pamplona and Takahashi, 2012]. It is generally established that some endocannabinoids, d-9-THC and several synthetic CB1R/CB2R agonists and antagonists can also interact with a number of non-CB1, non-CB2 GPCRs, ligand-gated ion channels and nuclear receptors (see the recent review by Pertwee and colleagues [Pertwee et al. 2010]). In conclusion, the biochemical mechanisms of this system are far more complex and the discussion on whether any known mammalian channel or non-CB1R/CB2R should be classified as a novel cannabinoid ‘CB3’ receptor or channel is ongoing.
The involvement of the particular neural regions and the neurotransmitter systems here is significant due to the fact that the very same brain areas and neurotransmitter systems are also implicated in psychoses, particularly in schizophrenia [van Os and Kapur, 2009; Smieskova et al. 2010; Stone, 2011].
Functions of the endocannabinoid receptor system
Available evidence indicates that we do not yet have a complete understanding of the varied functions of the endocannabinoid system, which is widely distributed both in the brain and in the peripheral system and most glands and organs in the body. However, there has been a dramatic increase in research exploring this system during the last decade and it is considered to be one of the fastest growing fields in psychopharmacology, whilst the number of ‘classic’ neurotransmitter’ studies have either declined or remained the same [Pamplona and Takahashi, 2012]. Even though our knowledge on the role of the endocannabinoid system is still evolving, the available evidence indicates that this system has multiple regulatory roles in neuronal, vascular, metabolic, immune and reproductory systems. As mentioned previously, the on-demand regulatory role on other neurotransmitter systems clearly affect functions such as cognition, memory, motor movements and pain perception [Howlett et al. 2002].
Cannabis plant
The cannabis plant has two main subspecies, Cannabis indica and Cannabis sativa, and they can be differentiated by their different physical characteristics. Indica-dominant strains are short plants with broad, dark green leaves and have higher cannabidiol content than the sativa plants in which THC content is higher. Sativa-dominant strains are usually taller and have thin leaves with a pale green colour. Due to its higher THC content, C. sativa is the preferred choice by users. It is a complex plant with about 426 chemical entities, of which more than 60 are cannabinoid compounds [Dewey, 1986]. The four major compounds are d-9-THC, CBD, d-8-THC and cannabinol, which have been most researched [Pertwee, 1997, 2008; Pamplona and Takahashi, 2012].
In the plant, cannabinoids are synthesized and accumulated as cannabinoid acids, but when the herbal product is dried, stored and heated, the acids decarboxylize gradually into their proper forms, such as CBD or d-9-THC [De Meijer et al. 2003]. Originally it was thought that CBD was the metabolic parent to d-9-THC, but it was later found that its biosynthesis occurs according to a genetically determined ratio [Russo and Guy, 2006]. Even though the chemical structures of all four compounds are similar, their pharmacological effects can be very different. The most researched compounds of the plant are d-9-THC and CBD and therefore we will mainly focus on these two compounds and their differences.
Delta-9-tetrahydrocannabinol and cannabidiol
Natural compounds of the cannabis plant are also referred to as phytocannabinoids of which d-9-THC is the main psychoactive ingredient and has been widely researched both in animals and humans. It characteristically produces, in a dose-dependent manner, hypoactivity, hypothermia, spatial and verbal short-term memory impairment [Hayakawa et al. 2007]. However, the second major compound, CBD, does not affect locomotor activity, body temperature or memory on its own. However, higher doses of CBD can potentiate the lower doses of d-9-THC by enhancing the level of CB1R expression in the hippocampus and hypothalamus. The authors suggest that CBD potentiates the pharmacological effects of d-9-THC via a CB1R-dependent mechanism [Hayakawa et al. 2007].
The available research indicates that the main two compounds, d-9-THC and CBD, whilst having similar effects in certain domains, also have almost opposite effects to one another in other aspects [Carlini et al. 1974; Borgwardt et al. 2008; Fusar-Poli et al. 2009; Morrison et al. 2009; Bhattacharyya et al. 2009b; Winton-Brown et al. 2011]. Table 1 summarizes the varying effects of these two compounds.
Table 1.
Effects of tetrahydrocannabinol and cannabidiol, adapted and updated from Russo and Guy [2006].
CBD, cannabidiol; CNS, central nervous system; GI, gastrointestinal; THC, tetrahydrocannabinol.
In fact the different and opposing effects of the main two compounds of the plant were noticed in some early studies. In a double-blind study with 40 healthy volunteers, Karniol and colleagues orally administered d-9-THC and CBD and the mixtures of the two together, whilst pulse rate, time production tasks and psychological reactions were measured [Karniol et al. 1974]. Whilst d-9-THC alone increased pulse rate, disturbed time tasks and induced strong psychological reactions in the subjects, CBD alone provoked no such effects. However, CBD was efficient in blocking most of the effects of d-9-THC when both drugs were given together. CBD also decreased the anxiety component of d-9-THC effects in such a way that the subjects reported more pleasurable effects.
Most recently there have been a number of drug challenge studies with sound methodologies examining the effects of both of these compounds. Our group carried out a number of double-blind, pseudo-randomized studies on healthy volunteers who had previous minimal exposure to cannabis. All participants were administered 10 mg of d-9-THC, 600 mg of CBD and placebo (flour) in three different functional magnetic resonance imaging sessions while performing a response inhibition task, a verbal memory task, an emotional task (viewing fearful faces) and an auditory and visual sensory processing task. The overall concluding results showed that d-9-THC and CBD had different behavioural effects and also, at times, opposing brain activation in various regions [Borgwardt et al. 2008; Fusar-Poli et al. 2009; Bhattacharyya et al. 2009b; Winton-Brown et al. 2011]. D-9-THC caused transient psychotic symptoms and increased the levels of anxiety, intoxication and sedation, whilst CBD had no significant effect on behaviour or these parameters.
In relation to the imaging data, during the response inhibition task, relative to placebo, d-9-THC attenuated the engagement of brain regions that normally mediate response inhibition, whilst CBD modulated activity in regions not implicated with this task [Borgwardt et al. 2008]. During the verbal learning and retrieval of word pair tasks, d-9-THC modulated activity in mediotemporal and ventrostriatal regions, whilst CBD had no such effect [Bhattacharyya et al. 2009b]. During an emotional processing task d-9-THC and CBD had clearly distinct effects on the neural, electrodermal and symptomatic response to fearful faces [Fusar-Poli et al. 2009]. Our results suggest that the effects of CBD on activation in limbic and paralimbic regions may contribute to its ability to reduce autonomic arousal and subjective anxiety, whereas the anxiogenic effects of d-9-THC may be related to effects in other brain regions. During the auditory task, again these two compounds had opposite effects in the superior temporal cortex when subjects listened to speech and in the occipital cortex during visual processing [Winton-Brown et al. 2011].
Our group also assessed whether pretreatment with CBD could prevent the acute psychotic symptoms induced by d-9-THC when six healthy volunteers were administered d-9-THC intravenously on two occasions, after placebo or CBD pretreatment [Bhattacharyya et al. 2010]. We found that pretreatment with CBD prevented the transient psychotic symptoms induced by d-9-THC.
Both animal and human studies indicate that CBD has anxiolytic properties. In fact in a recent double-blind study carried out on patients with generalized social anxiety disorder, it was found that relative to placebo, CBD significantly reduced subjective anxiety and its effect was related to its activity on limbic and paralimbic areas as shown by single photon emission computed tomography [Crippa et al. 2011].
CBD has also been proposed to have antipsychotic effects and is considered a potential antipsychotic medicine, particularly due its relatively low side-effect profile [Zuardi et al. 1995]. Furthermore, it is also being developed as a possible ‘medicine’ for various other conditions, such as inflammation, diabetes, cancer and neurodegenerative diseases [Izzo et al. 2009].
CBD is not the only compound which shows different effects to its main ingredient d-9-THC, a partial CB1R agonist. Another interesting compound of the plant, d-9-tetrahydrocannabivarin (d-9-THCV), a novel CB1R antagonist, also exerts potentially useful actions in the treatment of epilepsy and obesity [Pertwee, 2008; Izzo et al. 2009]. A review of this compound, along with d-9-THC and CBD by Pertwee suggests that plant extractions of d-9-THCV produces its antiobesity effects more by increasing energy expenditure than by reducing food intake [Pertwee, 2008]. The author also points out that a medicine such as d-9-THCV, by simultaneously blocking CB1Rs and activating CB2Rs, may have potential for the management of disorders such as chronic liver disease and obesity, particularly when these are associated with inflammation.
Different strengths of street cannabis
As d-9-THC is the main ingredient which causes the desired ‘stoned’ effect, users prefer the strains of the plant with higher THC content. Particularly over the past 15 years, such variants of the plant have been more widely available on the street ‘market’, which are usually referred to as ‘skunk’ or ‘sinsemilla’. In a study carried out by Potter and colleagues, when the potency of cannabis seized by police in England between the years of 1996/8 and 2004/5 were compared, the median content of d-9-THC was found to be 13.9% in more recent years, significantly higher than recorded 10 years previously [Potter et al. 2008]. However, the CBD content was found to be extremely low in more recent times. The authors also found that in herbal or resin forms of the drug, the average CBD content exceeded that of THC. More recently, a meta-analysis to assess the potency of cannabis from 1970 to 2009 was carried out. From 21 case series covering a number of countries, a recent and consistent worldwide increase in cannabis potency was reported [Cascini et al. 2011].
These findings suggest that current trends for preferring higher THC content variants carry significant health risks, particularly to those who are susceptible to its harmful effects. Indeed, Morgan and colleagues carried out a study on 120 current users, which included 66 daily and 54 recreational users, whose hair analyses revealed their THC and CBD amounts. The study found that higher THC levels in hair in daily users were associated with increased depression and anxiety, as well as poorer prose recall and source memory [Morgan et al. 2011]. However, higher CBD in hair was associated with lower psychosis-like symptoms and better recognition memory. In relation to people with psychosis, health risks are even higher with stronger variants of the plant. In a recent study of people with a first episode of psychosis, it was found that patients used higher-potency cannabis for longer durations and greater frequency compared with a healthy control group [Di Forti et al. 2009].
As the stronger variants have been taking over the street market, there has been a surge of interest in studying the links between cannabis use and mental health problems. The first to draw attention to such a link was a number of epidemiological studies and reviews, which pointed towards an association between the use of cannabis and the increased risk of developing a psychotic illness, in a dose-dependent manner [Zammit et al. 2002; Arseneault et al. 2002; Moore et al 2007]. A psychotic outcome is not the only diagnostic category which has been associated with cannabis use. Symptoms of depression and anxiety commonly coexist with cannabis use and lead to diagnostic dilemmas [Nunes et al. 2006; Dakwar et al. 2011]. Cannabis use can induce such symptoms, as well as be used secondary to a primary depressive illness [Dakwar et al. 2011; Fairman and Anthony, 2012]. As the majority of the studies have had psychotic illness as an outcome, in this section we will mainly be focusing on this diagnostic category.
Intersubject variation in response to the psychotogenic effects of cannabis
About 18.5% of people in the UK use cannabis regularly [Atha, 2005]. This is important as the strong THC variants of cannabis use have been increasing steeply, as have concerns on cannabis-related health risks, particularly for young people [Hall and Degenhardt, 2007; Potter et al. 2008; EMCDDA, 2011]. Recent epidemiological studies point towards a link between the use of cannabis and the development of a psychotic illness [Zammit et al. 2002; van Os et al. 2002; Arseneault et al. 2002; Henquet et al. 2005]. Further evidence comes from a systematic review of longitudinal and population-based studies which show that cannabis use significantly increases the risk of development of a psychotic illness in a dose-dependent manner [Moore et al. 2007].
However, only a small minority develop a full-blown psychotic illness in the form of schizophrenia or bipolar disorder, whilst a larger group, ranging from 15% to 50%, experience transient psychotic symptoms of brief duration, from a couple of hours to up to a week, and usually recover without requiring any intervention [Thomas, 1996; Green et al. 2003; D’Souza et al. 2004, 2009; Morrison et al. 2009]. Indeed drug challenge studies with d-9-THC on healthy volunteers have shown a broad range of transient symptoms, behaviours and cognitive deficits ranging from anxiety to psychosis to transient memory disturbance [D’Souza et al. 2004; Curran et al. 2002; Morrison et al. 2009]. The clinical picture of transient psychosis can be indistinguishable from a frank acute psychosis with delusions and hallucinations, except for its short duration.
Evidently there is considerable variation in the effects of cannabis on individuals. The biological basis of this variable sensitivity is yet unclear. There have been a number of studies exploring which groups are more vulnerable to developing a psychotic outcome as a result of cannabis use [van Os et al. 2002; Henquet et al. 2004]. Findings so far indicate that the effect of cannabis use is much stronger in those with any predisposition for psychosis at baseline than in those without [Henquet et al. 2005]. Indeed, individuals with a predisposition to psychosis indicated by a positive family history of psychosis have been found to be particularly sensitive to the effects of cannabis [McGuire et al. 1995]. Another indicator for a higher psychosis risk is the presence of subclinical psychotic features and again such individuals have been affected by a higher risk of developing a psychotic illness [Henquet et al. 2004]. Furthermore those who are at ultra high risk for psychosis have been reported to be more sensitive to the psychotogenic effects of cannabis compared with users in the general population [Peters et al. 2009].
Because of the reported links between the schizotypal personality and schizophrenia, this type of personality disorder has come under scrutiny in examining the role of cannabis in producing psychotic symptoms. Indeed, it has been shown that people scoring high in schizotypy who use cannabis are more likely to have psychosis-like experiences at the time of use, together with unpleasant side effects [Barkus et al. 2006]. This study has been replicated and it has been confirmed that those with schizotypal personality disorder carry a higher risk of experiencing psychotic symptoms with cannabis use [Stirling et al. 2008]. Most recently, another study has provided further support for a strong association between early cannabis use and the development of schizophrenia spectrum disorder symptoms [Anglin et al. 2012].
The reported vulnerability factors mentioned here imply a strong genetic predisposition and there have been a number of studies looking particularly to specific genes which have been implicated in psychoses. The first such study was carried out by Caspi and colleagues [Caspi et al. 2005]. In this longitudinal study, a specific susceptibility gene which has been linked to schizophrenia and bipolar disorder, catechol-O-methyltransferase (COMT), was examined in a representative birth cohort followed to adulthood. The study found that carriers of the COMT valine158 allele were most likely to exhibit psychotic symptoms and to develop schizophreniform disorder if they used cannabis before the age of 15. However, the number of people carrying this allele was small in this study. Using a case-only design of 493 people with schizophrenia, Zammit and colleagues re-examined this association but their findings did not support the different effects of cannabis use on schizophrenia according to variation in COMT [Zammit et al. 2007]. Zammit’s group also looked for evidence of an interaction between cannabis use and COMT genotype by restricting the analysis to participants who claimed to have first used cannabis by the same cutoff period as the Caspi group, but failed to find evidence supporting the link.
More recently, van Winkel and colleagues looked at the effects of recent cannabis use whilst examining 152 single nucleotide polymorphisms in 42 candidate genes in 801 patients with psychosis and their 740 unaffected siblings [van Winkel et al. 2011]. The authors found that genetic variation in serine-threonine protein kinase (AKT1) may mediate both short- and long-term effects on psychosis expression associated with cannabis use. The authors suggest that the likely mechanism could be cannabinoid-regulated AKT1/glycogen synthase kinase 3 signalling downstream of the dopamine D2 receptor. Indeed, CB1R agonists have been shown to induce AKT1 phosphorylation, whilst the antagonists of this receptor have inhibited AKT1 signalling pathways [Molina-Holgado et al. 2002]. Further support for the possible involvement of the AKT1 gene comes from our study with healthy volunteers. This study found that, during the encoding and recall conditions of the verbal memory task, the induction of psychotic symptoms by d-9-THC was correlated with the attenuated striatal and midbrain activation only in those who were G homozygotes of AKT1 and carriers of the 9-repeat allele dopamine transporter (DAT1) [Bhattacharyya et al. 2012] (Table 2).
Table 2.
Proposed factors determining sensitivity to psychosis in cannabis users.*
| Sensitivity to psychosis as determined by: | Possible sensitivity factors | Study group |
|---|---|---|
| Predisposition to psychosis | Family history of psychotic illness | McGuire et al. [1995] |
| Presence of subclinical psychotic symptoms | Henquet et al. [2004] | |
| Ultra high risk groups | Peters et al. [2009] | |
| Personality | Schizotypal personality disorder | Barkus et al. [2006]; Stirling et al. [2008]; Anglin et al. [2012] |
| Psychosis susceptibility genes | COMT | Caspi et al. [2005] |
| AKT1 | van Winkel et al. [2011] | |
| AKT1 and DAT1 | Bhattacharyya et al. [2012] |
Please note that except for the schizotypal personality disorder, the other studies need to be replicated.
AKT1, serine-threonine protein kinase; COMT, catechol-O-methyltransferase; DAT1, dopamine transporter gene.
Apart from schizotypal personality, the vulnerability factors to the psychotogenic effects of cannabis require replication. It is clear that further work needs to be carried out to explore the biological mechanisms which determine the vulnerability towards a psychotic outcome.
Conclusion
During the last decade, endocannabinoid research has been one of the fastest growing fields in psychopharmacology, opening ways to discover new medicines for a wide variety of health problems, ranging from metabolic disorders, to glaucoma and schizophrenia.
The distribution of the endocannabinoid system in the brain is interesting as the very same brain areas are also implicated in psychoses, particularly in schizophrenia. Furthermore, complex and intricate involvement of this system with other neurotransmitters such as dopamine, GABA and glutamatergic systems may have implications for the development of a psychotic illness.
Naturally, due to the recent and constant increase in the availability of higher THC content variants of cannabis around the world, there have been increasing concerns about the health risks, particularly for young people. However, cannabis affects people differently and therefore it is important to understand what makes someone more at risk and how they differ compared with those who do not develop psychotic illness. Here we have provided an overview of the available information on the risk factors which may make an individual more at risk, such as predisposition to psychosis, schizotypal personality and certain susceptibility genes.
Finding groups who are vulnerable is particularly important so that they can be targeted for early preventative and therapeutic interventions. Such a search would also lead to the discovery of the biochemical mechanisms involved in cannabis and endocannabinoid research and ultimately to a better understanding of how the brain and the body functions.
Acknowledgments
Thanks to Ethan Russo and Geoffrey W. Guy for providing the inspiration for Table 1. Also thanks to Dr Sanem Atakan for her help with the editing of the first draft.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The author declare no conflicts of interest in preparing this article.
References
- Anderson B., Rizzo M., Block R., Pearlson G., O’Leary D. (2010) Sex, drugs and cognition: effects of marijuana. J Psychoactive Drugs 42: 413–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglin D., Corcoran C., Brown A., Chen H., Lighty Q., Brook J., et al. (2012) Early cannabis use and schizotypal personality disorder symptoms from adolescence to middle adulthood. Schizophr Res 137: 45–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L., Cannon M., Murray R., Poulton R., Caspi A., Moffitt T. (2002) Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 325: 1212–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atha M. (2005) Independent Drug Monitoring Unit (IDMU) Cannabis use in Britain. Available at: http://www.idmu.co.uk/
- Athanasiou A., Clarke A., Turner A., Kumaran N., Vakilpour S., Smith P., et al. (2007) Cannabinoid receptor agonists are mitochondrial inhibitors: a unified hypothesis of how cannabinoids modulate mitochondrial function and induce cell death. Biochem Biophys Res Commun 364: 131–137 [DOI] [PubMed] [Google Scholar]
- Barkus E., Stirling J., Hopkins R., Lewis S. (2006) Cannabis-induced psychosis-like experiences are associated with high schizotypy. Psychopathology 39: 175–178 [DOI] [PubMed] [Google Scholar]
- Batkai S., Pacher P., Osei-Hyiaman D., Radaeva S., Liu J., Harvey-White J., et al. (2004) Endocannabinoids acting at cannabinoid-1 receptors regulate cardiovascular function in hypertension. Circulation 110: 1996–2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N., Jones R. (1981) Cardiovascular and metabolic considerations in prolonged cannabinoid administration in man. J Clin Pharmacol 21: 214S–223S [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S., Atakan Z., Martin-Santos R., Crippa J., Kambeitz J., Prata D., et al. (2012) Preliminary report of biological basis of sensitivity to the effects of cannabis on psychosis: AKT1 and DAT1 genotype modulates the effects of delta-9-tetrahydrocannabinol on midbrain and striatal function. Mol Psychiatry 31 January (epub ahead of print). [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S., Crippa J., Martin-Santos R., Winton-Brown T., Fusar-Poli P. (2009a) Imaging the neural effects of cannabinoids: current status and future opportunities for psychopharmacology. Curr Pharm Des 15: 2603–2614 [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S., Fusar-Poli P., Borgwardt S., Martin-Santos R., Nosarti C., O’Carroll C., et al. (2009b) Modulation of mediotemporal and ventrostriatal function in humans by delta-9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry 66: 442–451 [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S., Morrison P., Fusar-Poli P., Martin-Santos R., Borgwardt S., Winton-Brown T., et al. (2010) Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 35: 764–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgwardt S., Allen P., Bhattacharyya S., Fusar-Poli P., Crippa J., Seal M., et al. (2008) Neural basis of Δ-9-tetrahydrocannabinol and cannabidiol: effects during response inhibition. Biol Psychiatry 64: 966–973 [DOI] [PubMed] [Google Scholar]
- Callén L., Moreno E., Barraso-Chinea P., Moreno-Delgado D., Cortes A., Mallol J., et al. (2012) Cannabinoid receptors CB1 and CB2 form functional heteromers in the brain. J Biol Chem 287: 20851-20865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlini E., Karniol I., Renault P., Schuster C. (1974) Effects of marihuana in laboratory animals and in man. Br J Pharmacol 50: 299–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascini F., Aiello C., Di Tanna G. (2011) Increasing delta-9-tetrahydrocannabinol (Δ-9-THC) content in herbal cannabis over time: systematic review and meta-analysis. Curr Drug Abuse Rev 5: 32-40 [DOI] [PubMed] [Google Scholar]
- Caspi A., Moffitt T., Cannon M., McClay J., Murray R., Harrington H., et al. (2005) Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry 57: 1117–1127 [DOI] [PubMed] [Google Scholar]
- Costa B., Trovato A., Comellii F., Giagnoni G., Colleoni M. (2007) The non-psychoactive cannabis constituent cannabidiol is an orally effective therapeutic agent in rat chronic inflammatory and neuropathic pain. Eur J Pharmacol 556: 75–83 [DOI] [PubMed] [Google Scholar]
- Crippa J., Derenusson G., Ferrari T., Wichert-Ana L., Duran F., Martin-Santos R., et al. (2011) Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: apreliminary report. J Psychopharmacol 25: 121–130 [DOI] [PubMed] [Google Scholar]
- Crippa J., Zuardi A., Martin-Santos R., Bhattacharyya S., Atakan Z., McGuire P., et al. (2009) Cannabis and anxiety: a critical review of the evidence. Hum Psychopharmacol 7: 515–523 [DOI] [PubMed] [Google Scholar]
- Curran H., Brignell C., Fletcher S., Middleton P., Henry J. (2002) Cognitive subjective dose–response effects of acute oral delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users. Psychopharmacology 164: 61–70 [DOI] [PubMed] [Google Scholar]
- Dakwar E., Nunes E., Bisaga A., Carpenter K., Mariani J., Sullivan M., et al. (2011) A comparison of independent depression and substance-induced depression in cannabis-, cocaine-, and opioid-dependent treatment seekers. Am J Addict 20: 441–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Coffey C., Carlin J., Swift W., Moore E., Patton G. (2010) Outcomes of occasional cannabis use in adolescence: 10-year follow-up study in Victoria, Australia. Br J Psychiatry 196: 290–295 [DOI] [PubMed] [Google Scholar]
- De Meijer E., Bagatta M., Carboni A., Crucitti P., Moliterni V., Ranalli P., et al. (2003) The inheritance of chemical phenotype in Cannabis sativa L. Genetics 63: 335–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devane W., Dysarz F., Johnson M., Melvin L., Howlett A. (1988) Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol 34: 605–613 [PubMed] [Google Scholar]
- Devane W., Hanus L., Breuer A., Pertwee R., Stevenson L., Griffin G., et al. (1992) Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258: 1946–1949 [DOI] [PubMed] [Google Scholar]
- Dewey W. (1986) Cannabinoid pharmacology. Pharmacol Rev 38: 151–178 [PubMed] [Google Scholar]
- Di Forti M., Morgan C., Dazzan P., Pariente C., Mondelli V., Marques T., et al. (2009) High-potency cannabis and the risk of psychosis. Br J Psychiatry 195: 488–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Marzo V., Piscitelli F. (2011) Gut feelings about the endocannabinoid system. Neurogastroenterol Motil 23: 391–398 [DOI] [PubMed] [Google Scholar]
- Di Marzo V., Piscitelli F., Mechoulam R. (2011) Cannabinoids and endocannabinoids in metabolic disorders with focus on diabetes. Handb Exp Pharmacol 203: 75–104 [DOI] [PubMed] [Google Scholar]
- D’Souza D., Perry E., MacDougall L., Ammerman Y., Cooper T., Wu Y., et al. (2004) The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29: 1558–1572 [DOI] [PubMed] [Google Scholar]
- D’Souza D., Sewell R., Ranganathan M. (2009) Cannabis and psychosis/schizophrenia: human studies. Eur Arch Psychiatry Clin Neurosci 259: 413–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2011) Annual Report 2011: The State of the Drug Problems in Europe. Lisbon: EMCDDA [Google Scholar]
- Fairman B., Anthony J. (2012) Are early-onset cannabis smokers at an increased risk of depression spells? J Affect Disord 138: 54–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferré S., Goldberg S., Lluis C., Franco R. (2009) Looking for the role of cannabinoid receptor heteromers in striatal function. Neuropharmacology 56(Suppl. 1): 226–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., Crippa J., Bhattacharyya S., Borgwardt S., Allen P., Martin-Santos R., et al. (2009) Distinct effects of delta-9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch Gen Psychiatry 66: 95–105 [DOI] [PubMed] [Google Scholar]
- Gaoni Y., Mechoulam R. (1964) Isolation, structure and partial synthesis of an active constituent of hashish. J Am Chem Soc 86: 1646–1647 [Google Scholar]
- Gorelick D., Heishman S. (2006) Methods for clinical research involving cannabis administration. Methods Mol Med 123: 235–253 [DOI] [PubMed] [Google Scholar]
- Green B., Kavanagh D., Young R. (2003) Being stoned: a review of self-reported cannabis effects. Drug Alcohol Rev 22: 453–460 [DOI] [PubMed] [Google Scholar]
- Green K. (1998) Marijuana smoking vs cannabinoids for glaucoma therapy. Arch Ophthalmol 116: 1433–1437 [DOI] [PubMed] [Google Scholar]
- Hall W., Degenhardt L. (2007) Prevalence and correlates of cannabis use in developed and developing countries. Curr Opin Psychiatry 20: 393–397 [DOI] [PubMed] [Google Scholar]
- Hayakawa K., Mishima K., Hazekawa M., Sano K., Orito K., et al. (2008) Cannabidiol potentiates pharmacological effects of delta(9)-tetrahydrocannabinol via CB(1) receptor-dependent mechanism. Brain Res 1888: 157–164 [DOI] [PubMed] [Google Scholar]
- Henquet C., Krabbendam L., Spauwen J., Kaplan C., Lieb R., Wittchen H., et al. (2004) Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330: 11–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henquet C., Krabbendam L., Spauwen J., Kaplan C., Lieb R., Wittchen H., et al. (2005) Prospective cohort study of cannabis use, predisposition for psychosis and psychotic symptoms in young people. BMJ 330: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlett A., Barth F., Bonner T., Cabral G., Casellas P., Devane W., et al. (2002) International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev 54: 161–202 [DOI] [PubMed] [Google Scholar]
- Iwamura H., Suzuki H., Ueda Y., Kaya T., Inaba T. (2001) In vitro and in vivo pharmacological characterization of JTE-907, a novel selective ligand for cannabinoid CB2 receptor. J Pharmacol Exp Ther 296: 420–425 [PubMed] [Google Scholar]
- Izzo A. (2004) Cannabinoids and intestinal motility: welcome to CB2 receptors. Br J Pharmacol 142: 1201–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juknat A., Rimmerman N., Levy R., Vogel Z., Kozela E. (2011) Cannabidiol affects the expression of genes involved in zinc homeostasis in BV-2 microglial cells. Neurochem Int 9 December (epub ahead of print). [DOI] [PubMed] [Google Scholar]
- Karniol I., Carlini E. (1973) Comparative studies in man and in laboratory animals on 8- and 9-trans-tetrahydrocannabinol. Pharmacology 9: 115–126 [DOI] [PubMed] [Google Scholar]
- Karniol I., Shirikawa I., Kasinski N., Pfefermen A., Carlini E. (1974) Cannabidiol interferes with the effects of delta-9-tetrahydrocannabinol in man. Eur J Pharmacol 28: 172–77 [DOI] [PubMed] [Google Scholar]
- Kenney S., Kekuda R., Prasad P., Leibach F., Devoe L., Ganapathy V. (1999) Cannabinoid receptors and their role in the regulation of the serotonin transporter in human placenta. Am J Obstet Gynecol 181: 491–497 [DOI] [PubMed] [Google Scholar]
- Lakhan S., Rowland M. (2009) Whole plant cannabis extracts in the treatment of spasticity in multiple sclerosis: a systematic review. BMC Neurol 9: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H. (1973) An archaeological and historical account of cannabis in China. Economic Botany 28: 437–448 [Google Scholar]
- Mackie K., Stella N. (2006) Cannabinoid receptors and endocannabinoids: evidence for new players. AAPS J 8: E298–E306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcellino D., Carriba P., Filip M., Borgkvist A., Frankowska M., Bellido I., et al. (2008) Antagonistic cannabinoid CB1/dopamine D2 receptor interactions in striatal CB1/D2 heteromers. A combined neurochemical and behavioral analysis. Neuropharmacology 54: 815–823 [DOI] [PubMed] [Google Scholar]
- Matsuda L., Lolait S., Brownstein M., Young A., Bonner T. (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346: 561–564 [DOI] [PubMed] [Google Scholar]
- McGuire P., Jones P., Harvey I., Williams M., McGuffin P., Murray R. (1995) Morbid risk of schizophrenia for relatives of patients with cannabis-associated psychosis. Schizophr Res 15: 277–281 [DOI] [PubMed] [Google Scholar]
- Mechoulam R., Ben-Shabat S., Hanuš L., Ligumsky M., Kaminski N., Schatz A., et al. (1995) Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol 50: 83–90 [DOI] [PubMed] [Google Scholar]
- Mechoulam R., Hanus L. (2000) A historical overview of chemical research on cannabinoids. Chems Phys Lipids 108: 1–13 [DOI] [PubMed] [Google Scholar]
- Mechoulam R., Shvo Y. (1963) Hashish. I. The structure of cannabidiol. Tetrahedron 19: 2073–2078 [DOI] [PubMed] [Google Scholar]
- Molina-Holgado E., Vela J., Arévalo-Martin A., Almazán G., Molina-Holgado F., Borrell J., et al. (2002) Cannabinoids promote oligodendrocyte progenitor survival: involvement of cannabinoid receptors and phosphatidylinositol-3 kinase/Akt signalling. J Neurosci 22: 9742–9753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T., Zammit S., Lingford-Hughes A., Barnes T., Jones P., Burke M., et al. (2007) Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 370: 319–328 [DOI] [PubMed] [Google Scholar]
- Moreira F., Guimaraes F. (2005) Cannabidiol inhibits the hyperlocomotion induced by psychotomimetic drugs in mice. Eur J Pharmacol 512: 199–205 [DOI] [PubMed] [Google Scholar]
- Morgan C., Gardener C., Schafer G., Swan S., Demarchi C., Freeman T., et al. (2011) Sub-chronic impact of cannabinoids in street cannabis on cognition, psychotic-like symptoms and psychological well-being. Psychol Med 29: 1–10 [DOI] [PubMed] [Google Scholar]
- Morgan C., Schafer G., Freeman T., Curran H. (2010) Impact of cannabidiol on the acute memory and psychotomimetic effects of smoked cannabis: naturalistic study. Br J Psychiatry 197: 285–290 [DOI] [PubMed] [Google Scholar]
- Morrison P., Zois V., McKeown D., Lee T., Holt D., Powell J., et al. (2009) The acute effects of synthetic intravenous delta9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol Med 39: 1607–1616 [DOI] [PubMed] [Google Scholar]
- Munro S., Thomas K., Abu-Shaar M. (1993) Molecular characterization of a peripheral receptor for cannabinoids. Nature 365: 61–65 [DOI] [PubMed] [Google Scholar]
- Navarro G., Carriba P., Gandia J., Ciruela F., Casadó V., Cortés A., et al. (2008) Detection of heteromers formed by cannabinoid CB2, dopamine D2, and adenosine A2A G-protein-coupled receptors by combining bimolecular fluorescence complementation and bioluminescence energy transfer. ScientificWorldJournal 8: 1088–1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson A., Turner C., Stone B., Robson P. (2004) Effect of delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults. J Clin Psychopharmacol 24:305–313 [DOI] [PubMed] [Google Scholar]
- Nunes E., Liu X., Samet S., Matseoane K., Hasin D. (2006) Independent versus substance-induced major depressive disorder in substance-dependent patients: observational study of course during follow-up. J Clin Psychiatry 67: 1561–1567 [DOI] [PubMed] [Google Scholar]
- Pagotto U., Marsicano G., Cota D., Lutz B., Pasquali R. (2006) The emerging role of the endocannabinoid system in endocrine regulation and energy balance. Endocr Rev 27: 73–100 [DOI] [PubMed] [Google Scholar]
- Pamplona F., Takahashi R. (2012) Psychopharmacology of the endocannabinoids: far beyond anandamide. J Psychopharmacol 26: 7–22 [DOI] [PubMed] [Google Scholar]
- Parker L., Rock E., Limebeer C. (2011) Regulation of nausea and vomiting by cannabinoids. Br J Pharmacol 163: 1411–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee R. (1997) Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther 74: 129– 180 [DOI] [PubMed] [Google Scholar]
- Pertwee R. (2006) The pharmacology of cannabinoid receptors and their ligands: an overview. Int J Obes (Lond) 30: S13–S18 [DOI] [PubMed] [Google Scholar]
- Pertwee R. (2008) The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol 153: 199–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee R. (2009) Emerging strategies for exploiting cannabinoid receptor agonists as medicines. Br J Pharmacol 156: 397–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee R. (2010) Receptors and channels targeted by synthetic cannabinoid receptor agonists and antagonists. Curr Med Chem 17: 1360–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee R., Howlett A., Abood M., Alexander S., Di Marzo V., Elphick M. (2010) International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol Rev 62: 588–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters B., de Koning P., Dingemans P., Becker H., Linszen D., de Haan L. (2009) Subjective effects of cannabis before the first psychotic episode. Aust N Z J Psychiatry 43: 1155–1162 [DOI] [PubMed] [Google Scholar]
- Pickel V., Chan J., Kearn C., Mackie K. (2006) Targeting dopamine D2 and cannabinoid-1 (CB1) receptors in rat nucleus accumbens. J Comp Neurol 495: 299–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter D., Clark P., Brown M. (2008) Potency of delta 9-THC and other cannabinoids in cannabis in England in 2005: implications for psychoactivity and pharmacology. J Forensic Sci 53: 90–94 [DOI] [PubMed] [Google Scholar]
- Raduner S., Majewska A., Chen J., Xie X., Hamon J., Faller B., et al. (2006) Alkylamides from Echinacea are a new class of cannabinomimetics. Cannabinoid type 2 receptor-dependent and -independent immunomodulatory effects. J Biol Chem 281: 14192–14206 [DOI] [PubMed] [Google Scholar]
- Ramer R., Bublitz K., Freimuth N., Merkord J., Rohde H., Haustein M., et al. (2012) Cannabidiol inhibits lung cancer cell invasion and metastasis via intercellular adhesion molecule-1. FASEB J 26: 1535-1548 [DOI] [PubMed] [Google Scholar]
- Rhee M., Vogel Z., Barg J., Bayewitch M., Levy R., Hanus L., et al. (1997) Cannabinol derivatives: binding to cannabinoid receptors and inhibition of adenylylcyclase. J Med Chem 40: 3228–3233 [DOI] [PubMed] [Google Scholar]
- Russo E. B. (2001) Handbook of psychotropic herbs: a scientific analysis of herbal remedies for psychiatric conditions. Binghamton, NY: Haworth Press [Google Scholar]
- Russo E., Guy G. (2006) A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol andcannabidiol. Med Hypotheses 66: 234–246 [DOI] [PubMed] [Google Scholar]
- Russo E., Guy G., Robson P. (2007) Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex, a cannabis-based medicine. Chem Biodivers 4: 1729–1743 [DOI] [PubMed] [Google Scholar]
- Showalter V., Compton D., Martin B., Abood M. (1996) Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): identification of cannabinoid receptor subtype selective ligands. J Pharmacol Exp Ther 278: 989–999 [PubMed] [Google Scholar]
- Smieskova R., Fusar-Poli P., Allen P., Bendfeldt K., Stieglitz R., Drewe J., et al. (2010) Neuroimaging predictors of transition to psychosis – a systematic review and meta-analysis. Neurosci Biobehav Rev 34: 1207–1222 [DOI] [PubMed] [Google Scholar]
- Stirling J., Barkus E., Nabosi L., Irshad S., Roemer G., Schreudergoidheijt B., et al. (2008) Cannabis-induced psychotic-like experiences are predicted by high schizotypy. Confirmation of preliminary results in a large cohort. Psychopathology 41: 371–378 [DOI] [PubMed] [Google Scholar]
- Stone J. (2011) Glutamatergic antipsychotic drugs: a new dawn in the treatment of schizophrenia? Ther Adv Psychopharmacol 1: 5–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A., Amoako A., Bambang K., Karasu T., Gebeh A., Lam P., et al. (2010) Endocannabinoids and pregnancy. Clin Chim Acta 411: 921–930 [DOI] [PubMed] [Google Scholar]
- Terry G., Liow J., Zoghbi S., Hirvonen J., Farris A., Lerner A. (2009) Quantitation of cannabinoid CB1 receptors in healthy human brain using positron emission tomography and an inverse agonist radioligand. Neuroimage 48: 362–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas H. (1996) A community survey of adverse effects of cannabis use, Drug Alcohol Depend 42: 201–207 [DOI] [PubMed] [Google Scholar]
- Torres S., Lorente M., Rodriguez-Fornés F., Hernandez-Tiedra S., Salazar M., Garcia-Taboada E., et al. (2011) A combined preclinical therapy of cannabinoids and temozolomide against glioma. Mol Cancer Ther 10: 90–103 [DOI] [PubMed] [Google Scholar]
- Tsou K., Brown S., Sanudo-Pena M., Mackie K., Walker J. (1998) Immunohistochemical distribution of cannabinoid CB1 receptors in the rat central nervous system. Neuroscience 83: 393–411 [DOI] [PubMed] [Google Scholar]
- van Os J., Bak M., Bijl R., De Graaf R., Verdoux H. (2002) Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol 156: 319–327 [DOI] [PubMed] [Google Scholar]
- van Os J., Kapur S. (2009) Schizophrenia. Lancet 374: 635–645 [DOI] [PubMed] [Google Scholar]
- van Waes V., Beverley J., Siman H., Tseng K., Steiner H. (2012) CB1 cannabinoid receptor expression in the striatum: association with corticostriatal circuits and developmental regulation. Front Pharmacol 3: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Winkel R., Genetic Risk and Outcome of Psychosis (GROUP) Investigators (2011) Family-based analysis of genetic variation underlying psychosis-inducing effects of cannabis: sibling analysis and proband follow-up. Arch Gen Psychiatry 68: 148–157 [DOI] [PubMed] [Google Scholar]
- Wallace M., Wiley J., Martin B., DeLorenzo R. (2001) Assessment of the role of CB1 receptors in cannabinoid anticonvulsant effects. Eur J Pharmacol 428: 51–57 [DOI] [PubMed] [Google Scholar]
- Winton-Brown T., Allen P., Bhattacharrya S., Borgwardt S., Fusar-Poli P., Crippa J., et al. (2011) Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an fMRI study. Neuropsychopharmacology 36: 1340–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood T. (1899) Cannabinol, part I. J Chem Soc 75: 20–36 [Google Scholar]
- Zammit S., Allebeck P., Andreasson S., Lundberg I., Lewis G. (2002) Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ 325: 1199–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit S., Spurlock G., Williams H., Norton N., Williams N., O’Donovan M., et al. (2007) Genotype effects of CHRNA7, CNR1 and COMT in schizophrenia: interactions with tobacco and cannabis use Br J Psychiatry 191: 402–407 [DOI] [PubMed] [Google Scholar]
- Zuardi A., Guimaraes F. (1997) Cannabidiol as an anxiolytic and antipsychotic. In: Mathre M. (ed), Cannabis in Medical Practice: A Legal, Historical and Pharmacological Overview of the Therapeutic Use of Marijuana. Jefferson, NC: McFarland, p. 133–141 [Google Scholar]
- Zuardi A., Morais S., Guimaraes F., Mechoulam R. (1995) Antipsychotic effect of cannabidiol [letter]. J Clin Psychiatry 56: 485–486 [PubMed] [Google Scholar]