Abstract
Emergency department use contributes to high end-of-life costs and is potentially burdensome for patients and family members. We examined emergency department use in the last months of life for patients age sixty-five or older who died while enrolled in a longitudinal study of older adults in the period 1992–2006. We found that 51 percent of the 4,158 decedents visited the emergency department in the last month of life, and 75 percent in the last six months of life. Repeat visits were common. A total of 77 percent of the patients seen in the emergency department in the last month of life were admitted to the hospital, and 68 percent of those who were admitted died there. In contrast, patients who enrolled in hospice at least one month before death rarely visited the emergency department during that period. Policies that encourage the preparation of patients and families for death and early enrollment in hospice may prevent emergency department visits at the end of life.
Emergency departments are not designed to provide end-of-life care and in many ways are poorly suited to do so. Nonetheless, they are visited with surprising frequency by severely ill patients whose deaths are approaching.(1) The often overcrowded and seemingly chaotic nature of the emergency department may add to the stress that patients and their families feel.
Most people say they prefer to receive end-of-life care at home.(2, 3) But pain, worsening symptoms, or other urgent needs may force an emergency department visit. In such cases, patients often arrive in the emergency department acutely ill, with their care plan uncertain and their families deeply anxious at the approach of a dreaded event.(1, 3, 4)
Emergency department care is expensive, and it is a major component of escalating costs of care at the end of life.(5) Most patients who are hospitalized at that point are admitted through the emergency department, and it is there that care pathways are often determined, including the balance between palliative and life-sustaining treatments.(6, 7)
We used a nationally representative data set linked to Medicare claims data to study emergency department use by older adults at the end of life. The objective of this study was to use these data to describe the prevalence and frequency of, and factors associated with, emergency department use in the last months of life, as well as care following the visit, including hospitalization and death in the hospital.
Study Data And Methods
Setting And Participants
The Health and Retirement Study was designed to examine changes in health and wealth as people age.(8) It provided a data set that enabled us to assess patient characteristics and health status as well as family-level end-of-life concerns that can be linked to dying patients’ emergency department visits.
Health and Retirement Study participants are more than fifty years old and living in the community at the time of enrollment in the study, which began in 1992. Participants are interviewed every two years following enrollment. Additional participants are added every six years so that the study remains representative of the US population over fifty. Follow-up rates are very high (84–93 percent), and date of death is determined for 99 percent of participants using the National Death Index, a centralized record of death certificate information maintained by the National Center for Health Statistics.(9
The study’s interviews are conducted over the phone. For participants who are age eighty or older, are too sick to be interviewed by phone, or do not have access to a phone, interviews are conducted in person. If participants are too sick or cognitively unable to complete the interview, interviews are conducted with proxies. Interviews after death are conducted with participants’ next of kin. Details of the sampling frame and complex survey design are available elsewhere.(10
We linked Health and Retirement Study data to Medicare claims to ascertain emergency department use, using previously described methods.(11) Because the timing of death is often unpredictable, we examined the relationship between emergency department use and death in two directions.
For the first analysis, we included 8,338 participants age sixty-five or older who were continuously enrolled in Medicare fee-for-service Parts A and B from 1992 to 2006 and visited the emergency department. For these participants, we asked what percentage of older adults died within six months of visiting the emergency department.
For the second analysis, we focused on the subset of 4,585 participants who died, and for whom there were 4,158 next-of-kin interviews completed with the measures necessary for our analysis. For these participants, we asked what percentage of older adults who died had visited the emergency department in the last 6 months and last month before death.
Finally, we matched each decedent participant to a Health and Retirement Study subject who was alive at the time the participant died, categorized by age group (65–74, 75–84, and 85 or older) and sex. This allowed us to compare decedents’ and nondecedents’ rates of emergency department use.
This study was approved by the Institutional Review Board of the University of California, San Francisco.
Measures
We used Medicare claims to measure emergency department use, hospitalization, and intensive care unit use.(12) We examined factors that might be correlated with emergency department use in the last months of life, based on our clinical experience and review of the literature. Demographic factors included age, sex, race or ethnicity, and net worth.
Clinical factors were drawn from Health and Retirement Study interviews with next of kin conducted after the subject’s death. Next of kin were asked to describe the participant’s clinical condition during the last three months life. Factors included the presence or absence of four chronic conditions (cancer, lung disease, stroke, and heart condition), need for help in activities of daily living, cognitive impairment, and the presence of moderate or severe pain.
Health system factors included census region, urban versus rural residence, hospice use prior to the last month of life (hereafter referred to as “early hospice use”), nursing home residence, and year of death. We examined what we categorized as “anticipatory/preparatory” factors—for example, whether the subject’s next of kin reported that the death was expected or unexpected at the time it occurred and whether or not there was an advance directive.
Statistical Analysis
First, using the sample of 10,364 patients (both living and deceased), we calculated the percentage of emergency department visits by patients who died within six months of the visit.
The remainder of our analysis focused on the 4,158 decedents. We began by determining the proportion of these older people who visited the emergency department in the last six months and in the last month of life.
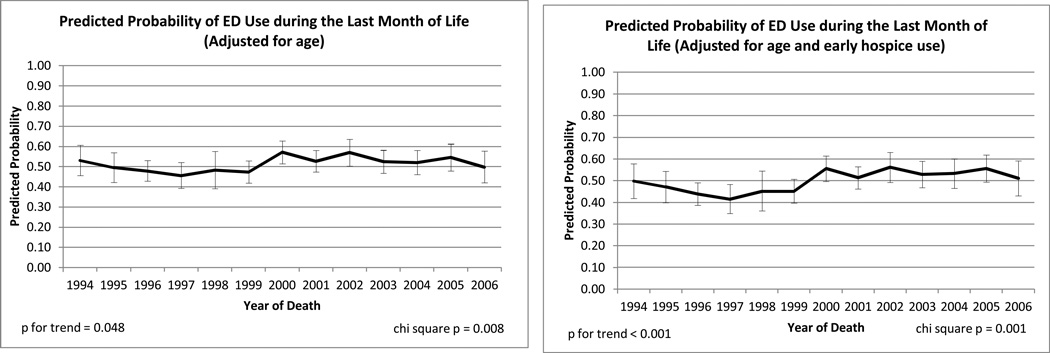
To understand which factors were independently associated with emergency department use by participants in the last month of life, we created a multivariable model adjusted for the demographic and clinical factors described above. The results of the multivariable logistic regression are presented as probabilities of emergency department use across different levels for each predictor of interest adjusted for age, sex, race or ethnicity, net worth, chronic conditions, physical dependency, cognitive impairment, and pain. We present time trends in emergency department use in the last month of life adjusted for variations in age of the Health and Retirement Study decedent sample across years and increasing rates of early hospice use (Appendix Exhibit 1).(11
Appendix 1.
Time trends in emergency department (ED) use in the last month of life 1994 to 2006 are displayed. Sample sizes of decedents were too small in 1992 and 1993 to generate reliable estimates. Panel A: Time trends in ED use adjusted for age at death. Panel B: time trends adjusted for age at death and rising rates of early hospice use (hospice use before the last month of life) over the examined time period (1994, 5%; 2006, 15%).
We examined care patterns following emergency department visits in the last month of life. Specifically, we examined hospitalization following the emergency department visit, intensive care unit use, and location of death.
The Health and Retirement Study purposely oversamples certain key subpopulations and also carefully tracks nonresponse rates by subpopulation. To produce nationally representative statistical estimates and to attach correct standard errors to these estimates, we performed a survey-weighted analysis using weights provided by the Health and Retirement Study.(13, 14) The statistical analyses were performed using the statistical software Stata, version 10.1, and the statistical analysis software SAS, version 9.2.
Limitations
We were unable to discern the specific reason for emergency department visits. A diagnostic code for congestive heart failure, for example, is not particularly informative as to the reason for the emergency department visit, such as shortness of breath, or the reasons that led to that condition, such as difficulty contacting an outpatient provider, lack of access to medications for symptom relief, or a family that was unprepared to manage end-of-life symptoms. Similarly, we could not definitively state that certain emergency department visits were avoidable. Finally, although our findings suggest that changes over time have been modest, the latest available Medicare claims data files are from 2006, and practice may have changed since that time.
Study Results
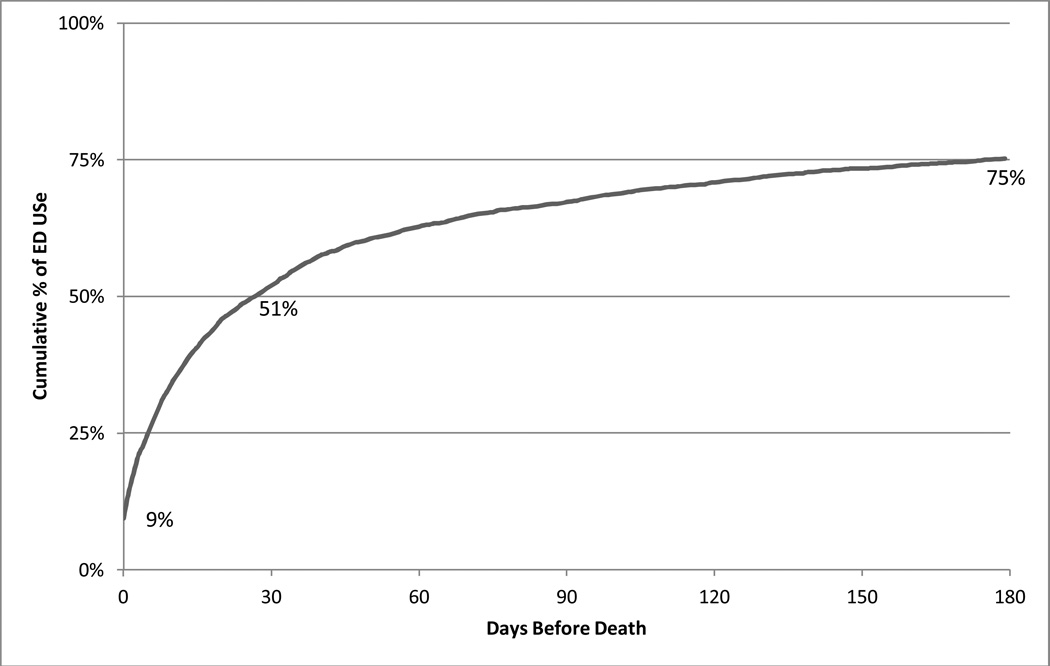
In this nationally representative study of older adults, 8,338 living and dead participants visited the emergency department. Of the total, 15 percent, or about one out of every seven emergency department visits, were made by a patient who died in the six months after that visit. Among the oldest participants (those over age eighty-four), the proportion was 24 percent, or about one out of four. Among the 4,158 participants who died, seventy-five percent transited through the emergency department in the last six months of life (Exhibit 2); half did so in the last month of life.
Exhibit 2.
Cumulative Incidence of emergency department (ED) visits during the last 6 months of life, noting the incidence on the last day of life (9%), and the cumulative incidence at 30 days before death (51%) and 180 days before death (75%).
The rate of emergency department use in the last month of life was much higher than the rate among participants matched by age and sex to the subject who were alive at the time the subject died. In the matched group, only 4 percent visited the emergency department in a one-month time period.
Focusing on decedents, we found that the mean age of the 4,158 participants who had died was eighty-three (standard deviation eight), and 47 percent were women (Exhibit 1). Among the decedents, the burden of chronic conditions, functional dependency, and cognitive impairment was high: The mean number of chronic diseases was 1.4 (out of 4); 77 percent of patients were dependent in at least one activity of daily living, and 67 percent were in three or more (data not shown). In addition, over one-third were cognitively impaired, experienced moderate or severe pain, and resided in a nursing home (Exhibit 1). The top three primary diagnoses for emergency department visits in the last six months of life were congestive heart failure (8.0 percent of visits), pneumonia (6.6 percent), and acute stroke (4.9 percent) (see Appendix Exhibit 2 for the rest of the top ten primary diagnoses).(15
Exhibit 1.
Characteristics Of Decedents In The Health and Retirement Study, 1992–2006
| Characteristic | Median/Percent |
|---|---|
| Net worth a | $79,000 |
| Female | 47% |
| Age | |
| 65–74 | 19% |
| 75–84 | 40 |
| ≥85 | 41 |
| Race/ethinicity | |
| White | 87% |
| African American | 9 |
| Latino | 3 |
| Other | 1 |
| Chronic conditions | |
| Cancer | 31% |
| Lung disease | 25 |
| Heart condition | 57 |
| Stroke | 31 |
| Status, last three months of life | |
| ≥3 ADL dependenciesb | 67% |
| Cognitive impairment | 43 |
| Moderate or severe pain | 46 |
| Health system factors | |
| Early hospice usec | 9% |
| Nursing home residence | 36 |
| Communication factors | |
| Death expected | 61% |
| Advanced care plan | 45 |
SOURCE Authors’ analysis of the Health and Retirement Study data linked to Medicare claims. NOTES N = 4,158. Percentages are weighted to reflect national estimates.
Net worth includes housing and non-housing assets. Interquartile range is $10,000–$214,000.
ADL is activities of daily living, such as getting into and out of bed, walking across the room, eating, dressing, bathing, and toileting.
Hospice use at least one month before death.
Appendix 2.
Leading Primary Diagnoses for the 6,824 Emergency Department Visits that Occurred During the Last Six Months of Life for the 4,158 Decedents*
| Count | % | Diagnosis |
|---|---|---|
| 532 | 8.0% | Congestive heart failure; nonhypertensive |
| 435 | 6.6% | Pneumonia (except caused by tuberculosis or sexually transmitted disease) |
| 326 | 4.9% | Acute cerebrovascular disease |
| 277 | 4.2% | Septicemia (except in labor) |
| 248 | 3.7% | Acute myocardial infarction |
| 215 | 3.3% | Cardiac arrest and ventricular fibrillation |
| 213 | 3.2% | Fluid and electrolyte disorders |
| 206 | 3.1% | Chronic obstructive pulmonary disease and bronchiectasis |
| 198 | 3.0% | Urinary tract infections |
| 171 | 2.6% | Aspiration pneumonitis; food/vomitus |
The diagnostic group assigned by the Clinical Classification Software using the primary ICD-9-CM diagnosis code for the emergency department (ED) visit. Percentages were weighted to reflect national estimates.
Routine visits were common. In fact, 41 percent of the 4,158 participants who died had made more than one visit in that time period, and 12 percent had gone to the emergency department more than once in the last month of life (data not shown).
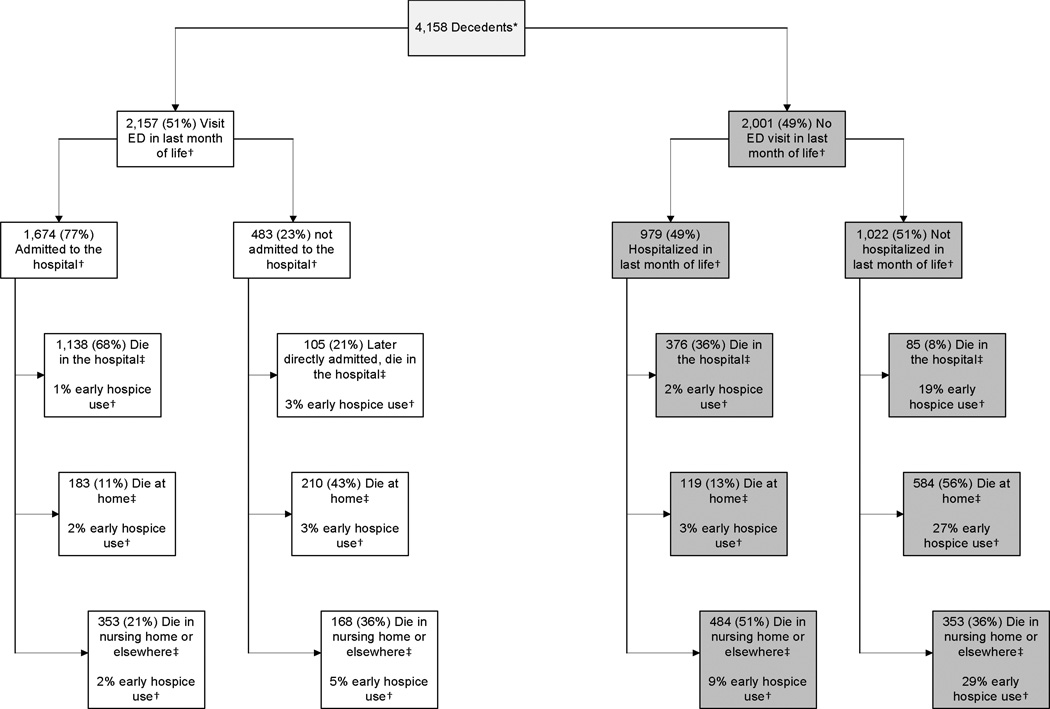
Hospitalization also was common following an emergency department visit toward the end of life. Among the 2,157 participants who visited the emergency department in the last month of life, 77 percent were subsequently hospitalized. Of those who were hospitalized, 39 percent were admitted to an intensive care unit, and 68 percent died in the hospital (Appendix Exhibit 3).(15)
Exhibit 3.
Flow diagram outlining emergency department, hospitalization, and location of death among the 4,58 patients in the Health and Retirement Study (HRS) who died between 1992 and 2006. Early hospice use indicates hospice use prior to the last month of life. Discrepancies between hospitalization and location of death may be explained by direct admissions to the hospital and differential sources of information for these factors. Sources of data are: * HRS and National Death Index mortality files; † Medicare claims data; ‡ HRS interviews with next-of-kin following subject’s death. Abbreviation: ED – emergency department.
Early hospice use and death in the home, nursing home, or other setting outside the hospital was more common among participants who did not visit the emergency department in the last month of life (Appendix Exhibit 3).(15
Exhibit 3 shows emergency department use in the last month of life by various characteristics, after adjustment for demographic and clinical factors. For example, patients who were African American or Latino were more likely to visit the emergency department than white patients. (for a complete list of factors, see Appendix Exhibit 4).(15) After adjustment, patients who experienced moderate or severe pain were 4 percent more likely to visit the emergency department in the last month of life than patients who had less pain. Having an advance directive had little effect after adjustment. These differences were modest in comparison to those between patients who did and did not enroll in hospice early.
Exhibit 3.
Characteristics Associated With Emergency Department (ED) Use During The Last Month Of Life, 1992–2006
| Characteristic | Visited ED last month of life (%), unadjusted |
95% CI, unadjusted |
p value |
Visited ED last month of life (%), adjusteda |
95% CI, adjusteda |
p value |
|---|---|---|---|---|---|---|
| Net worth | ||||||
| >$79,000 | 51 | 48, 53 | __b | 51 | 49, 54 | __b |
| ≤$79,000 | 52 | 49, 55 | 0.345 | 52 | 49, 55 | 0.775 |
| Sex | ||||||
| Male | 53 | 51, 55 | __b | 52 | 49, 55 | __b |
| Female | 50 | 47, 53 | 0.066 | 51 | 49, 53 | 0.438 |
| Age | ||||||
| 65–74 | 56 | 52, 60 | __b | 56 | 52, 60 | __b |
| 75–84 | 54 | 50, 57 | 0.365 | 53 | 50, 56 | 0.305 |
| 85 | 47 | 44, 50 | 0.003 | 48 | 44, 52 | 0.011 |
| Race/ethnicity | ||||||
| White | 50 | 48, 53 | __b | 51 | 49, 53 | __b |
| African American | 56 | 52, 61 | 0.008 | 56 | 52, 60 | 0.038 |
| Latino | 62 | 55, 69 | 0.003 | 61 | 53, 68 | 0.02 |
| Chronic conditions | ||||||
| No cancer | 54 | 51, 57 | __b | 54 | 52, 57 | __b |
| Cancer | 46 | 43, 49 | < 0.001 | 46 | 43, 49 | < 0.001 |
| No lung disease | 51 | 48, 53 | __b | 51 | 49, 54 | __b |
| Lung disease | 53 | 50, 57 | 0.302 | 52 | 48, 56 | 0.721 |
| No heart condition | 48 | 46, 51 | __b | 49 | 46, 51 | __b |
| Heart condition | 54 | 51, 56 | 0.001 | 54 | 51, 57 | 0.001 |
| No stroke | 51 | 49, 53 | __b | 51 | 49, 53 | __b |
| Stroke | 52 | 49, 55 | 0.507 | 53 | 50, 57 | 0.219 |
| ADL dependency, last 3 months of life c | ||||||
| 0 | 63 | 59, 67 | __b | 62 | 58, 66 | __b |
| 1–2 | 71 | 67, 75 | 0.012 | 70 | 66, 74 | 0.008 |
| ≥3 | 44 | 42, 47 | < 0.001 | 45 | 42, 48 | < 0.001 |
| Cognitive impairment, last 3 months of life | ||||||
| No | 56 | 53, 58 | __b | 54 | 51, 57 | __b |
| Yes | 46 | 43, 49 | <0.001 | 49 | 46, 52 | 0.018 |
| Moderate or severe pain, last 3 months of life | ||||||
| No | 51 | 48, 53 | __b | 50 | 47, 53 | __b |
| Yes | 52 | 50, 55 | 0.31 | 54 | 51, 57 | 0.038 |
| Health system factors | ||||||
| Census region | ||||||
| Northeast | 53 | 50, 55 | 0.487 | 53 | 50, 56 | 0.672 |
| Midwest | 49 | 44, 54 | 0.123 | 50 | 45, 54 | 0.144 |
| South | 54 | 50, 58 | __b | 54 | 50, 58 | __b |
| West | 45 | 42, 49 | 0.001 | 46 | 40, 51 | 0.012 |
| Urban/rural | ||||||
| Urban | 50 | 48, 51 | __b | 50 | 48, 52 | __b |
| Rural | 54 | 49, 59 | 0.082 | 55 | 50, 60 | 0.05 |
| Early hospice use d | ||||||
| No | 56 | 53, 58 | __b | 55 | 53, 58 | __b |
| Yes | 10 | 6, 13 | <0.001 | 11 | 8, 15 | <0.001 |
| Nursing home residence | ||||||
| No | 55 | 53, 57 | __b | 53 | 50, 55 | __b |
| Yes | 45 | 41,9 | <0.001 | 50 | 46 53 | 0.172 |
| Communication factors | ||||||
| Death expected | ||||||
| No | 60 | 57 ,62 | __b | 56 | 53, 59 | __b |
| Yes | 46 | 43, 49 | <0.001 | 49 | 46, 52 | 0.006 |
| Advanced care plan | ||||||
| No | 55 | 52, 58 | __b | 55 | 52, 58 | __b |
| Yes | 49 | 45, 52 | 0.001 | 52 | 49, 55 | 0.081 |
SOURCE Authors’ analysis of the Health and Retirement Study data linked to Medicare claims. NOTES N = 4,158. For a complete list of factors associated with ED use, see Appendix Exhibit 4 (see Note 15 in text). CI is confidence interval. aNetworth includes housing and non-housing assets. Interquartile range is $10,000-$214,000.
< 5% missing for all variables except history of an advance care plan (19.2% missing). The question about presence of an advance care plan w as not in asked in interviews after death in the 1998 wave of the Health and Retirement Study; therefore, the analyses of advance care plans included only the 3,494 participants who responded to this question. Percentages were weighted to reflect national estimates.
reference.
ADL is activities of daily living, such as getting into and out of bed, walking across the room, eating, dressing, bathing, and toileting.
Hospice use at least one month before death.
The rise in emergency department use between 1994 and 2006 was marginally significant in analyses adjusted for age (p for trend = 0.048) (Appendix Exhibit 1).(15) However, when adjusting for early utilization of hospice, there was a modest increase in emergency department use over time (p for trend < 0.001), suggesting that a rise in early utilization of hospice (5 percent in 1994; 15 percent in 2006) may have blunted what would have otherwise been a greater increase in emergency department use over time (Appendix Exhibit 1).(15)
Discussion
High Rates Of Emergency Department Use
As noted above, seventy-five percent of the decedents in our study transited through the emergency department in the last six months of life, and half in the last month of life. Yet we also found substantial variation in emergency department use in the last month of life by age, race or ethnicity, illness burden, functional dependency, cognitive impairment, pain, region, year of death, and whether or not death was expected. Early enrollment in hospice was by far the strongest predictor of emergency department use or lack thereof. Specifically, emergency department use was relatively rare among people enrolled in hospice at least one month before death.
Improving The Quality Of Outpatient Care
These high rates of emergency department use in the last months of life suggest opportunities for improvement in the outpatient setting. As was the case in our sample, the last months of life for older adults are often characterized not by sudden death, but by chronic illness, pain, functional decline, and cognitive impairment.(16, 17) Many health problems and symptoms in late life are predictable, and some visits to the emergency department could potentially be avoided with access to high-quality outpatient care.(18, 19)
Most people prefer to die at home, and rates of end-of-life hospitalization are unlikely to decrease without reducing rates of emergency department use. The emergency department is seldom the best place for discussions about the goals of care.
Primary providers can plan for the eventuality of death by preparing patients and families for end-of-life symptoms, engaging in discussions about goals of care, arranging treatment that matches the patient’s wishes, and documenting preferences in ways that will be accessible to emergency department providers.(20–24) To this end, recent policy initiatives, such as those passed in 2008 in California(25) and 2010 in New York(26) that require physician disclosure of prognosis, may reduce costly and potentially burdensome use of the emergency department at the end of life.
Federal Initiatives
At the federal level, legislation that would have provided reimbursement under Medicare for physicians to address end-of-life planning was stripped from national health reform amid a furor over so-called death panels. In our study, advance directives were not associated with emergency department visits after adjustment.
Advance care planning is much more than the advance directive document, however. It also includes the discussion of and planning and preparation for future events by patients, caregivers, and physicians. There is some evidence to suggest that such discussions have an effect on high-cost, high-intensity health services.(27
The Medicare hospice benefit was recently criticized for spending increases primarily caused by increases in lengths-of-stay over the past decade.(28, 29) However, these critiques do not account for the avoidance of costly acute care services by early enrollees in hospice.(29) In our study, early enrollment was associated with 80 percent less use of the emergency department in the last month of life, and dramatically reduced rates of hospitalization and of death in the hospital, compared to the rates for patients who did not enroll early. Although hospice use at the end of life has increased over the past decade, most patients enroll in hospice late, less than a month before death.(30)
Many analysts have viewed this delayed entry into hospice as a problem in the quality of end-of-life care.(30, 31) In fact, the type of care that patients receive in hospice—such as symptom control, family support, and discussion of preferences—are of benefit long before the final days of life.
The Medicare hospice benefit is available to all adults age sixty-five or older, and rising rates of early hospice use are encouraging. Yet we found that only 9 percent of the older adults in our study who died had enrolled in hospice before the last month of life. Policy initiatives should be directed toward increasing early hospice enrollment among elderly patients. Strong consideration should be given to removing from the Medicare hospice benefit the requirement of a prognosis of six months or less to live, basing eligibility and reimbursement instead on need for hospice services.(32
The Role Of Palliative Care
Part of the Affordable Care Act directs support to chronically ill elderly people in the outpatient setting, avoiding high-cost repeat emergency department visits and hospital readmissions. Potential avenues for supporting chronically ill elderly people on an outpatient basis include promoting early hospice use and mandating that inpatient and outpatient palliative care services are incorporated into accountable care organizations.(33, 34)
Palliative care is focused on improving quality of life for patients with serious illness. Its major areas of expertise include pain and symptom management and communication about goals of care. Palliative care is ideally initiated at the time of diagnosis of advanced heart disease, dementia, cancer, or other serious condisions, and can be delivered concurrently with life-prolonging care. Specialized palliative care is delivered by interdisciplinary palliative care teams.
Early enrollment in outpatient palliative care services has shown great promise in improving the quality of life for patients with serious illness, but access to these services remains limited.(19, 20, 35)Prognosis is inherently challenging, and even when prognosis is limited, some patients may elect not to enroll in hospice early. Our research suggests that many of these patients will transit through the emergency department at the end of life, and palliative care needs to be integrated into emergency services.
The majority of palliative care in emergency departments, however, is delivered not by palliative care specialists but by emergency department doctors, nurses, and social workers.(21) Hospice, in contrast, is a specific palliative service and Medicare benefit for patients with a prognosis of six months or less.
Emergency departments should be supported in their growing efforts to improve palliative care for patients, such as the well-respected Education on Palliative and End-of-Life Care Project curriculum, newly developed for training emergency medicine professionals.(36) The American Board of Emergency Medicine is one of 11 specialty boards that cosponsorspalliative medicine as a recognized subspecialty.(37)
In qualitative research, emergency providers and terminally ill patients and their caregivers suggested a change in emergency care, recognizing that the goals of patients near the end of life often do not fit well within the traditional emergency department model.(1, 3, 38, 39) Some providers suggested that emergency protocols could be modified by creating an explicit triage category of supportive care focused on symptom stabilization.
Structural barriers to change need to be overcome, including a pervading fear of litigation among emergency physicians, logistical hurdles to emergency providers rapidly coordinating home or hospice services with outpatient clinicians, and a general lack of access to palliative medicine consultation services in the emergency department, particularly at night and on weekends.(3, 39, 40)
Conclusion
Emergency department visits are common at the end of life, and a substantial minority of all visits to the emergency department by older adults are made by patients who will die within six months of the visit. For patients whose terminal trajectories are clear, we can do better in the outpatient setting.(22–24) Outpatient providers can help prepare families for the eventuality of death, including by giving them early referrals to hospice and, where available, outpatient palliative care services. Policies that require physicians to disclose a terminal prognosis and that provide reimbursement for advance care planning should be encouraged.
For other older adults, serious illness is unexpected and emergency department visits are unavoidable.(41) Therefore, emergency departments should be supported in their efforts to incorporate palliative and end-of-life care principles into their practices. Ultimately clinicians and policy makers need to work together to ensure high-quality care experiences for patients and families seen in the emergency department during a vulnerable time.
Acknowledgments
Acknowledgment/Disclosure
Alexander Smith was supported by career development grants from the National Palliative Care Research Center and the National Center for Research Resources UCSF-CTSI (UL1 RR024131). Kenneth Covinsky was supported by a K-24 grant from the National Institute on Aging (K24AG029812).
Footnotes
Early versions of this article were presented in oral abstract form at the annual meetings of the Society of General Internal Medicine in Minneapolis, Minnesota, April 29 2010, and the American Geriatrics Society in Orlando, Florida, May 13 2010.
NOTES
- 1.Smith AK, Schonberg MA, Fisher J, Pallin DJ, Block SD, Forrow L, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010 Jun;39(6):972–981. doi: 10.1016/j.jpainsymman.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000 Fall;3(3):287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 3.Smith AK, Fisher J, Schonberg MA, Pallin DJ, Block SD, Forrow L, et al. Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med. 2009 Jul;54(1):86–93. e1. doi: 10.1016/j.annemergmed.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Christakis N. Death Foretold: Prophecy and Prognosis in Medical Care. Chicago, IL: University of Chicago Press; 1999. [Google Scholar]
- 5.Hospital-Based Emergency Care: At the Breaking Point (Future of Emergency Care) Washington: The National Academies Press; 2007. Committee on the Future of Emergency Care in the United States Health System. [Google Scholar]
- 6.Beemath A, Zalenski RJ. Palliative emergency medicine: resuscitating comfort care? Ann Emerg Med. 2009 Jul;54(1):103–105. doi: 10.1016/j.annemergmed.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Chan GK. End-of-life and palliative care in the emergency department: a call for research, education, policy and improved practice in this frontier area. J Emerg Nurs. 2006 Feb;32(1):101–103. doi: 10.1016/j.jen.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Juster FT, Suzman R. An Overview of the Health and Retirement Study. J Hum Resour. 1995;30(suppl):S7–S56. [Google Scholar]
- 9.National Center for Health Statistics: National Death Index. 2012 May 9; Available from: http://www.cdc.gov/nchs/data_access/ndi/about_ndi.htm.
- 10.Walter LC, Lewis CL, Barton MB. Screening for colorectal, breast, and cervical cancer in the elderly: a review of the evidence. Am J Med. 2005 Oct;118(10):1078–1086. doi: 10.1016/j.amjmed.2005.01.063. [DOI] [PubMed] [Google Scholar]
- 11.Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008 Aug 10;26(23):3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knaus WA, Harrell FE, Jr, Lynn J, Goldman L, Phillips RS, Connors AF, Jr, et al. The SUPPORT prognostic model. Objective estimates of survival for seriously ill hospitalized adults. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med. 1995 Feb 1;122(3):191–203. doi: 10.7326/0003-4819-122-3-199502010-00007. [DOI] [PubMed] [Google Scholar]
- 13.Health and Retirement Study Sample Evolution: 1992–1998. Ann Arbor, MI: The University of Michigan; 2008. [2/20/2012]; Available from: http://hrsonline.isr.umich.edu/sitedocs/surveydesign.pdf. [Google Scholar]
- 14.Rhee SH, Corley RP, Friedman NP, Hewitt JK, Hink LK, Johnson DP, et al. The etiology of observed negative emotionality from 14 to 24 months. Front Genet. 2012;3:9. doi: 10.3389/fgene.2012.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.To access the Appendix click on the Appendix link in the box to the right of the article online [Google Scholar]
- 16.Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med. 2009 Oct 15;361(16):1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010 Apr 1;362(13):1173–1180. doi: 10.1056/NEJMoa0909087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care. 2003 Aug;41(8):992–1001. doi: 10.1097/00005650-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010 Aug 19;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 20.Morrison RS, Meier DE. Clinical practice. Palliative care. N Engl J Med. 2004 Jul 17;350(25):2582–2590. doi: 10.1056/NEJMcp035232. [DOI] [PubMed] [Google Scholar]
- 21.von Gunten CF. Secondary and tertiary palliative care in US hospitals. JAMA. 2002 Feb 20;287(7):875–881. doi: 10.1001/jama.287.7.875. [DOI] [PubMed] [Google Scholar]
- 22.Ahalt C, Walter LC, Yourman L, Eng C, Perez-Stable EJ, Smith AK. "Knowing is Better": Preferences of Diverse Older Adults for Discussing Prognosis. J Gen Intern Med. 2011 Nov 30; doi: 10.1007/s11606-011-1933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith AK, Williams BA, Lo B. Discussing overall prognosis with the very elderly. N Engl J Med. 2011 Dec 8;365(23):2149–2151. doi: 10.1056/NEJMp1109990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012 Jan 11;307(2):182–192. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drame M, Novella JL, Lang PO, Somme D, Jovenin N, Laniece I, et al. Derivation and validation of a mortality-risk index from a cohort of frail elderly patients hospitalised in medical wards via emergencies: the SAFES study. Eur J Epidemiol. 2008;23(12):783–791. doi: 10.1007/s10654-008-9290-y. [DOI] [PubMed] [Google Scholar]
- 26.Fischer SM, Gozansky WS, Sauaia A, Min SJ, Kutner JS, Kramer A. A practical tool to identify patients who may benefit from a palliative approach: the CARING criteria. J Pain Symptom Manage. 2006;31(4):285–292. doi: 10.1016/j.jpainsymman.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 27.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008 Oct 8;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iglehart JK. A new era of for-profit hospice care--the Medicare benefit. N Engl J Med. 2009 Jun 25;360(26):2701–2703. doi: 10.1056/NEJMp0902437. [DOI] [PubMed] [Google Scholar]
- 29.Hackbarth GM. Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission; 2009. [cited 2011 April 18, 2011]; Available from: http://www.medpac.gov/documents/Mar09_March%20report%20testimony_WM%20FINAL.pdf. [Google Scholar]
- 30.Christakis NA, Escarce JJ. Survival of Medicare patients after enrollment in hospice programs. N Engl J Med. 1996 Jul 18;335(3):172–178. doi: 10.1056/NEJM199607183350306. [DOI] [PubMed] [Google Scholar]
- 31.McCarthy EP, Burns RB, Ngo-Metzger Q, Davis RB, Phillips RS. Hospice use among Medicare managed care and fee-for-service patients dying with cancer. JAMA. 2003 May 7;289(17):2238–2245. doi: 10.1001/jama.289.17.2238. [DOI] [PubMed] [Google Scholar]
- 32.Groninger H. A gravely ill patient faces the grim results of outliving her eligibility for hospice benefits. Health Aff (Millwood) 2012 Feb;31(2):452–455. doi: 10.1377/hlthaff.2011.0473. [DOI] [PubMed] [Google Scholar]
- 33.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010 Apr 1;362(13):1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Widera E. Palliative Care and Accountable Care Organizations. GeriPal: A Geriatrics and Palliative Care Blog. 2010 [updated November 26, 2010March 11, 2011]; Available from: http://www.geripal.org/2010/11/palliative-care-and-accountable-care.html.
- 35.Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004 Jan 12;164(1):83–91. doi: 10.1001/archinte.164.1.83. [DOI] [PubMed] [Google Scholar]
- 36.Emanuel LL, Ferris FD, von Gunten CF. EPEC. Education for Physicians on End-of-Life Care. Am J Hosp Palliat Care. 2002 Jan-Feb;19(1):17. doi: 10.1177/104990910201900105. discussion-8. [DOI] [PubMed] [Google Scholar]
- 37.Quest TE, Marco CA, Derse AR. Hospice and palliative medicine: new subspecialty, new opportunities. Ann Emerg Med. 2009 Jul;54(1):94–102. doi: 10.1016/j.annemergmed.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 38.Lamba S, Quest TE. Hospice care and the emergency department: rules, regulations, and referrals. Ann Emerg Med. 2011 Mar;57(3):282–290. doi: 10.1016/j.annemergmed.2010.06.569. [DOI] [PubMed] [Google Scholar]
- 39.Grudzen CR, Richardson LD, Hopper SS, Ortiz JM, Whang C, Morrison RS. Does palliative care have a future in the emergency department? Discussions with attending emergency physicians. J Pain Symptom Manage. 2012 Jan;43(1):1–9. doi: 10.1016/j.jpainsymman.2011.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meier DE, Beresford L. Fast response is key to partnering with the emergency department. J Palliat Med. 2007 Jun;10(3):641–645. doi: 10.1089/jpm.2007.9959. [DOI] [PubMed] [Google Scholar]
- 41.Becker G, Murphy K, Philipson T. The Value of Life Near Its End and Terminal Care. 2007 Available from: http://www.nber.org/papers/w13333.pdf.