Abstract
Objective
To extend findings that African American women report greater stress during pregnancy, have higher blood pressure (BP), and are twice as likely to have low birthweight infants relative to white women. This study examines a) racial differences in associations between stress and BP during pregnancy, and b) the combined effects of stress and BP on infant birthweight in a sample of 170 African American and white women.
Methods
A prospective, longitudinal study of pregnant women was conducted in which measures of BP, stress, and other relevant variables were collected. Multiple measures of systolic and diastolic BP were taken at each of three points during pregnancy (18–20, 24–26, and 30–32 weeks gestation).
Results
Both systolic blood pressure (SBP) and diastolic blood pressure (DBP) were positively associated with stress in pregnant African American women and not in pregnant white women. In analyses of birthweight, there were no main effects of BP or stress. However, a significant interaction demonstrated that, when stress was high, DBP was negatively associated with birthweight and a combination of high stress and high DBP predicted the lowest birthweight in the sample. Furthermore, African American women were twice as likely as white women to have a combination of high stress and high DBP.
Conclusions
Racial differences in relationships between stress and BP, and the interactive effect of stress and DBP on birthweight together suggest that a high stress-high BP profile may pose a risk for lower birthweight among African American women, in particular, and possibly for all pregnant women.
Keywords: pregnancy, birthweight, African American, blood pressure, stress
INTRODUCTION
African American women are twice as likely to give birth prematurely and to have low birthweight infants compared with white women (1). These racial differences constitute some of the most dramatic health disparities in the United States. To address this issue, research has generally focused on identifying characteristics of African American women that are less prevalent in a lower-risk group, such as white women. Research has also examined associations between these individual characteristics and birth outcomes identifying psychosocial and biological variables, such as high stress and increased blood pressure (BP) responses to stress as independent risk factors contributing to racial disparities in adverse birth outcomes (2). However, researchers have been unable to account for why African American women are at such high risk for adverse pregnancy outcomes (3,4). Therefore, we take a different approach and consider the combined effects of biological and psychosocial risk factors on birthweight to provide new insights into the persistent racial disparities in birth outcomes.
Blood Pressure: Biological Risk Factor
In the general population, African Americans have a greater incidence of clinical hypertension than whites (5). It has been estimated that twice as many African American women as white women enter pregnancy with preexisting hypertension (6). Hypertension (systolic BP (SBP) ≥140 mm Hg; diastolic BP (DBP) ≥90 mm Hg) during pregnancy is a serious risk factor for fetal growth restriction and preterm delivery, and can be fatal to the pregnant woman or fetus if this condition goes untreated (7,8).
Less well understood are the implications of subclinical levels of BP. Although research suggests that variations in subclinical BP are related to cardiovascular health in nonpregnant African Americans (9), subclinical BP during pregnancy is understudied. There are several changes in physiology during pregnancy, including systematic adjustments in maternal blood volume and BP (10,11) that make this an important area of independent study.
Stress: A Psychosocial Risk Factor
A number of theories have predicted associations between various conceptualizations of stress (e.g., stressful life events, stress appraisals) and health (12), at times suggesting distinct pathways by which different forms of stress affect health (13). As members of a racial minority group, African American women face a large range and notable combination of stressors (14). Research has shown that African American pregnant women tend to report more stressful life events (4) and greater psychosocial distress from life events compared with other racial groups (15).
There is a significant body of evidence linking psychosocial stress (stressful life events, stress responses, anxiety, appraisals of stress) to a variety of birth outcomes, including lower birthweight and shorter length of gestation (1,16,17). One approach to understanding stress and pregnancy outcomes in African Americans is the theory of allostatic load in which physiologic wear and tear resulting from responses to chronic and repeated acute stress may lead to dysregulation of the body’s stress response systems and contribute to negative health outcomes (14,18,19).
A lifetime of allostatic load may cause African American pregnancies to be particularly susceptible to the negative consequences of stress (14,19). Relevant studies of state anxiety (20) and stressful life events (21) have found associations with infant birthweight in African Americans, but reported no associations between stress and pregnancy outcomes in other racial groups including white women. Also, racism—a uniquely salient psychosocial stressor for people of color— has been linked to compromised birth outcomes in African Americans (22–24).
Blood Pressure and Stress
There is some evidence in the literature that associations between BP and psychosocial variables differ in African Americans and whites. Stress reactivity studies have shown that African American women exhibited greater DBP responses to a stressful speech task than white women (25). Also, BP reactions to acute stress (26,27) and 24-hour ambulatory BP (28) have been associated with defensiveness, expressiveness, and hostility in African Americans whereas no such relationships have been noted in whites. Although each of these studies suggests that there is a stronger association between psychosocial factors and cardiovascular functioning in African Americans, none of them involved pregnant women. It is difficult to generalize stress and BP findings with nonpregnant samples to pregnant samples. For instance, studies suggested that, compared with nonpregnant women, pregnant women’s BP responses to stress are dampened (29,30).
It has long been thought that interactions of stress and BP are related to physical health. Evidence suggests that excessive cardiovascular reactions to acute stress indicate a greater risk of developing cardiovascular disease (31–33). Few studies, however, have investigated associations among stress, subclinical resting BP levels, and health. We suspect that a positive relationship between resting BP and chronic stress may reflect a form of cardiovascular hypersensitivity to stress and psychophysiological dysfunction. Such hypersensitivity may be related to poorer pregnancy outcomes and, if more prevalent in African American women, may explain some of the racial disparities in pregnancy outcomes.
Present Study
In the present study, we examined relationships between race, stress, and BP, and the additive and interactive effects of these variables on infant birthweight in African American and white pregnant women, a majority of whom were normotensive. Consistent with previous epidemiological studies, we anticipated that African American women would give birth to lower birthweight infants. We also hypothesized that African American women would have higher resting BP values, report greater stress, and show a stronger positive association between BP and stress compared with whites. Because one normative physiological adaptation during pregnancy is a gradual rise in BP beginning between 24 and 32 weeks gestation (11), relatively high subclinical BP at this time during pregnancy may not be a risk factor for adverse birth outcomes. However, in combination with high stress, subclinical high BP is hypothesized to pose a risk for lower birthweight. Thus, we expected an interaction of stress and BP effects on birthweight.
It is possible that a high stress by high BP interaction contributes to racial disparities in birthweight for two reasons. First, a combination of high stress and high BP is likely to be more prevalent in African American women compared with white women. Second, it is possible that the effects of a profile of high stress and high BP is more potent in African American compared with white women; that is, African American women may be more susceptible to the adverse effects of this combination (2). To examine these possibilities, we utilized a dataset with extensive measures of stress and BP at various times in pregnancy.
METHODS
Study Design
The Multi-Site Behavior in Pregnancy Study was a prospective, longitudinal study of stress during pregnancy that took place from 1997 to 2003. A total of 498 pregnant women provided psychosocial and medical data at multiple time points during their pregnancies (including 18–20, 24–26, and 32–34 weeks gestation). Data were collected at an urban major medical center in Los Angeles County. The Institutional Review Boards of the participating institutions approved this study.
Participants
Participants were at least 18 years of age and ≤18 weeks into a singleton, intrauterine pregnancy on study entry. Pregnant women were not eligible if they had current or prior medical conditions (e.g., systemic maternal disease, history of clinical hypertension) or risky prenatal health behaviors (e.g., use of cigarettes or controlled substances) that affected cardiovascular, neuroendocrine, hepatic, or renal functioning.
For the purposes of the present study, we included only women who self-identified as US-born “ non-Hispanic white” or “black/African American.” Given that we were interested in racial, rather than ethnic differences, women who indicated they were “black, not American,” Hispanic-American, or multi-ethnic were not included in the subsample. Because >90% of the African American participants took part in the study at one of two study centers, we restricted our subsample to women who were recruited at that location. Of the 170 participants who fit these criteria, 35 women were missing data at one or more time points due to a missed appointment or early withdrawal from the study. These women were compared with women who had complete data and were not statistically different on any study variables (p > .05) except they had lower per capita household income (p < .05). Because of this one difference, we could not assume that these women were missing completely at random and used multiple imputation methods to impute missing data (34,35). The Expectation-Maximization algorithm converged in k = 18 iterations. Therefore, results of m = 4 imputations were generated every k = 50 iterations and combined using the NORM software package (36). The results of multiple imputation analyses were similar to the results of analyses involving only women with complete data. Coefficients and p values reported here are the results of the multiple imputation analyses (n = 170). Descriptive statistics were averaged across imputed datasets.
Procedure
The three time points of data collection were 18 to 20, 24 to 26, and 32 to 34 weeks gestation. Research nurses collected medical data, such as weight and BP measurements, from women directly. Trained interviewers administered in-depth, semistructured interviews and questionnaires to assess sociodemographic factors and psychosocial stress. Medical charts were reviewed to obtain birthweight, gestational age (best obstetric estimate), and other medical data. Participants were compensated with $15 per visit. At the final study session, participants were given a $50 gift certificate to a popular children’s store.
Sociodemographic and Medical/Health Background Factors
Data were collected on sociodemographic and medical/health background factors that might confound relationships between the primary variables of interest. Educational attainment was rated on a 4-point ordinal scale (1 = high school or less to 4 = graduate/professional degree). Per capita income was calculated by dividing annual household income by household size. Body mass index (BMI) on study entry was calculated from height and weight. Parity, the number of times the participant had previously given birth, was dichotomized into 0 = nulliparous or 1 = multiparous.
Blood Pressure
A Critikon Dinamap Vital Sign Monitor 2100 (GE Healthcare, Milwaukee, WI) was used to measure BP at each time point with the participant seated. The amount of time a participant was seated before measurements were taken varied. Two BP readings separated by a 2-minute rest period were collected and averages of the DBP and SBP values were calculated to ensure the accuracy of the measurement. Repeated-measures analyses demonstrated there was no significant difference in SBP over time (means (Ms): 18–20 weeks = 115.06 mm Hg, 24–26 weeks = 114.57 mm Hg, and 32–34 weeks = 116.72 mm Hg), F = 1.97, p > .09. There was a significant difference in DBP levels over time (Ms: 18–20 weeks = 63.01 mm Hg, 24–26 weeks = 62.99 mm Hg, and 32–34 weeks = 65.04 mm Hg), F = 3.44, p < .01). To examine overall “dosage” effects of SBP and DBP on outcome and in relationship to a composite psychosocial stress index, values were combined to create average SBP and DBP indices.1
Psychosocial Stress
Chronic Socioenvironmental Stress
At 24 to 26 weeks gestation, patients were asked ten questions rated on a scale from 1 (never) to 5 (very often) about how often they had experienced specific financial and environmental difficulties over the last 6 months. This brief measure was developed for a similar study involving stress and pregnancy based on a variety of sources and included questions such as, “Did you have trouble meeting monthly bills?” and “Did you worry about crime in your neighborhood?” (37). Cronbach’s α revealed acceptable reliability among the items (α = 0.77). Mean chronic stress scores were calculated for each subject with greater values indicating more chronic stress.
Perceived Stress
A shortened version of the Perceived Stress Scale (PSS) (38) was administered at 18 to 20 weeks and 30 to 32 weeks gestation. This measure was a modified 12-item version of the PSS assessing how often the participant felt stressed or lacking in control during the past week.2 Participants provided ratings from 1 (never) to 5 (very often). These items have been used in other studies of pregnant women (39,40) and had good reliability in the present study (Cronbach’s α = 0.80 at 18–20 weeks and 0.84 at 32–34 weeks). Ratings were summed such that higher values indicated greater perceived stress. Results of a repeated-measures analysis of variance (ANOVA) indicated that there was no significant difference between time points (Ms = 26.80 and 26.64; p > .10), and scores were averaged to create a mean PSS score for the pregnancy.
State Anxiety
Participants completed the brief 10-item state version of the State-Trait Anxiety Inventory (STAI) (41) at each of the three time points regarding anxiety in the last few days on a scale from 1 (not at all) to 4 (very much). This scale was reliable at each time point (Cronbach’s α ranged from 0.84 to 0.90). Responses were averaged within each time point. Again, a repeated-measures ANOVA indicated no significant difference over time in this sample (Ms = 1.94, 1.91, and 1.90; p > .10), so scores were averaged to create a mean STAI score for the pregnancy.
Pregnancy Anxiety
Ten items assessing anxiety associated with pregnancy (42) were administered at each of the three time points during pregnancy. Participants made ratings on a scale from 1 (not at all) to 4 (very much) with higher scores indicating greater pregnancy anxiety. Reliability was acceptable at each time point (Cronbach’s α ranged from 0.75 to 0.85). A repeated-measures ANOVA revealed a significant effect with higher pregnancy anxiety earlier in pregnancy (18–20 weeks M = 1.84; both 24–26 and 32–34 weeks Ms = 1.73), F = 10.38, p < .001. Therefore, the pregnancy anxiety scores at Times 2 and 3 were averaged and the Time 1 score was treated as an independent stress measure before being included in the composite stress index.
Composite Stress Index
Previous studies that have used multiple measures of stress in combination have found the strongest evidence that high stress is associated with adverse birth outcomes (42,43). Therefore, we employed a composite stress index designed to capture the multidimensional nature of stress in a single score. The composite included chronic socioenvironmental stress, subjective appraisals of stress (PSS), and two forms of anxious mood previously found to be relevant to pregnancy outcomes, namely, general state anxiety (STAI) and anxiety about the pregnancy itself (pregnancy anxiety) (42,44). Correlations among the measures ranged from r =.40 to .94. Most of the measures of stress did not change over the course of pregnancy and they were therefore averaged into mean scores and then standardized (all standardizations were z scores). The exception to this was that pregnancy anxiety changed over time with Time 1 differing from Times 2 and 3. Therefore, Time 1 pregnancy anxiety was standardized independently of the average of Times 2 and 3. The standardized measures of chronic socioenvironmental stress, PSS, STAI, Time 1 pregnancy anxiety, and Times 2 to 3 pregnancy anxiety were then combined into an average composite stress index representing all forms of stress throughout pregnancy.
RESULTS
Overview
First, bivariate associations among study variables were examined. Then, t tests, χ2 tests, and regression analyses were used to compare African American and white women on the study variables. Sociodemographic and medical/health variables that differed by race were controlled for in separate regression analyses, comparing stress and BP associations across racial groups and testing effects of stress, BP, and race on birthweight.
Bivariate Associations
Correlation coefficients are shown in Table 1.
TABLE 1.
Intercorrelations Among Demographic, Medical, and Stress Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | |||||||||
| 2. BMI | 0.060 | ||||||||
| 3. Nulliparity (0 = nulliparous) | 0.030 | 0.237** | |||||||
| 4. Adjusted household income | 0.260** | −0.294** | −0.561** | ||||||
| 5. Highest level of education | 0.425** | −0.252** | −0.267** | 0.574** | |||||
| 6. SBP | 0.041 | 0.425** | 0.078 | −0.194* | −0.219** | ||||
| 7. DBP | −0.035 | 0.274** | −0.062 | −0.042 | −0.126 | 0.586** | |||
| 8. Gestational age at delivery | −0.118 | 0.004 | −0.211** | 0.049 | 0.042 | −0.063 | −0.084 | ||
| 9. Birthweight | −0.044 | 0.031 | −0.155* | 0.069 | 0.014 | −0.013 | 0.001 | 0.646** | |
| 10. Composite stress | −0.086 | 0.060 | −0.127 | −0.223** | −0.164* | 0.127 | 0.090 | 0.114 | −0.015 |
BMI = body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure.
p < .05;
p < .01.
Blood Pressure
As expected, women with greater BMI had higher SBP and DBP. Also, higher SBP was correlated with lower adjusted income and lower educational attainment (Table 1).
Birth Outcomes
The relationship between birthweight and gestational age was significant with shorter length of gestation associated with lower birthweight (Table 1). Gestational age was significantly related to nulliparity such that women who had not given birth previously tended to have longer gestations.
Stress
Women lower on per capita income and educational level reported greater overall stress on the composite stress measure (Table 1). Correlations between stress and BP and between stress and birth outcome were not significant.
Racial Differences
Demographic and Background Variables
Demographic and background characteristics of the sample are presented in Table 2. African American participants were younger (mean ± standard deviation (SD) = 29.89 ± 4.79 years) than white participants (32.23 ± 4.09 years), t = 3.21, p < .01, Cohen’s d = 0.53. Also, African American participants tended to report significantly lower education than white participants with the modal responses being “some college” versus “bachelor’s degree,” respectively (χ2 = 38.45, p < .001). Per capita household income was also significantly less for African American women ($16,475 ± 14,008) than white women ($37,039 ± 15,448), t = 8.25,p < .001, Cohen’s d = 1.39. On average, the African American sample had significantly greater BMI (27.02 ± 6.86 kg/m2) than the white sample (22.98 ± 4.29 kg/m2), t = 4.68, p < .001, Cohen’s d = 0.71, and the African American women were more likely to have previously given birth (67% versus 25%), χ2 = 27.16, p < .001.
TABLE 2.
Demographics and Medical Variables
| African Americans |
Non- Hispanic Whites |
|||
|---|---|---|---|---|
| % | na | % | na | |
| Age, years | ||||
| 20–25 | 23.1 | 13 | 4.8 | 6 |
| 26–29 | 19.5 | 11 | 16.3 | 19 |
| 30–34 | 38.2 | 21 | 54.6 | 63 |
| ≥35 | 19.1 | 11 | 24.3 | 28 |
| Education | ||||
| High school or less | 32.7 | 16 | 8.7 | 10 |
| Some college | 43.6 | 15 | 18.3 | 21 |
| Bachelor’s degree | 16.4 | 8 | 40.9 | 47 |
| Graduate degree | 7.3 | 1 | 32.2 | 37 |
| Income per household capita | ||||
| ≤$7,999 | 36.4 | 15 | 1.7 | 2 |
| $8,000–14,999 | 20.0 | 9 | 3.9 | 5 |
| $15,000–39,999 | 37.7 | 13 | 50.2 | 58 |
| ≥$40,000 | 5.9 | 2 | 44.1 | 51 |
| Body mass index (kg/m2) | ||||
| < 18.5 (underweight) | 1.8 | 1 | 6.3 | 7 |
| 18.5–24.9 (normal) | 44.1 | 17 | 72.2 | 83 |
| 25–29.9 (overweight) | 26.8 | 9 | 16.1 | 19 |
| ≥30 (obese) | 27.3 | 11 | 5.4 | 6 |
| Previous live birth | ||||
| Yes | 67.3 | 26 | 25.2 | 29 |
| No | 32.7 | 14 | 74.8 | 86 |
In the case of missing data, frequencies reflect average numbers (n) across imputed datasets rounded to the nearest whole number.
To rule out the possibility that results of the following BP and birth outcome analyses could be accounted for by racial differences in demographic and background variables, we included age, BMI, nulliparity, adjusted income, and education as controls.
Stress and Blood Pressure
Table 3 shows t test and effect size results of racial comparisons of stress and BP. Although African American women seemed to have higher composite stress, SBP, and DBP than white women, these differences were not significant. When control variables (age, BMI, nulliparity, education, and adjusted income) were included in regression analyses of SBP and DBP, the racial differences remained nonsignificant (p > .30, Cohen’s d < .20).
TABLE 3.
Comparison of African American and white Women on Stress, Blood Pressure, and Birth Outcome
| African Americans (n = 40), Mean ± SD |
Whites (n = 97), Mean ± SD |
t | p | Cohen’s d | |
|---|---|---|---|---|---|
| Composite stress | 0.10 ± 0.83 | −0.05 ± 0.81 | 1.10 | .27 | 0.18 |
| SBP (mm Hg) | 116.92 ± 8.66 | 114.75 ± 8.88 | 1.49 | .14 | 0.25 |
| DBP (mm Hg) | 64.68 ± 6.14 | 63.20 ± 7.32 | 1.27 | .20 | 0.22 |
| Gestational age at delivery (weeks) | 38.52 ± 2.69 | 39.22 ± 1.62 | 2.02 | .04 | 0.31 |
| Birthweight (g) | 3161.55 ± 609.89 | 3536.88 ± 566.61 | 3.73 | <.001 | 0.64 |
Composite stress = an average of five standardized stress variables; SBP = systolic blood pressure; DBP = diastolic blood pressure.
Six (15%) African American women and two (2%) white women were diagnosed with pregnancy-induced hypertension or preeclampsia. A χ2 test of independence demonstrated that this racial difference was statistically significant (p < .01, Fisher’s exact test). One of the African American women diagnosed with preeclampsia had her labor induced. To be sure that our results involving BP and birthweight as outcomes were not dependent on clinical hypertension or an early induction of labor, predictive models were run with and without these women. As results did not differ, only those for the overall sample are reported.
Birthweight
A hierarchical regression was conducted to examine racial differences in birthweight controlling for age, socioeconomic status (SES), BMI, and nulliparity. Nulliparity accounted for a marginally significant amount of variance, b = −100.74, t = − 1.73,p < .09, and the racial difference in birthweight was significant such that African American women gave birth to lower birthweight babies than white women, b = −265.984, t = −4.04, p < .001, Cohen’s d = 0.62. Also, there was a racial difference in length of gestation such that African American women had shorter gestations than white women (Table 3). Models predicting birthweight were examined with and without length of gestation as a control variable.
Associations of Stress and Blood Pressure
Although stress and BP were not associated in the overall sample (Table 1) hierarchical linear regression models were run separately for SBP and DBP to determine whether associations between stress and BP differed by race. Age, BMI, nulliparity, adjusted income, and educational attainment were entered in the first step, race and the composite stress index in the second step, and a race × composite stress interaction variable in the third step (Table 4). In step 1 of both models, BMI was the only control variable associated with the BP. In step 2 of both models, neither the composite stress variable nor race was significantly associated with BP. In step 3 of the models, significant race × stress results indicated that the stress-BP association differed by racial group with average ΔR2 = 0.03 for the final step of the SBP analysis and average ΔR2 = 0.09 for the final step of the DBP analysis (Table 4). Follow-up simple slope analyses (45) revealed that for African American women, the associations between composite stress and SBP (b = 3.31, t = 2.39, p < .02) and composite stress and DBP (b = 4.04, t = 3.57, p < .001) were positive and significantly different from zero. In contrast, for white women, the association between composite stress and BP did not differ from zero for SBP (b = −0.47, t = − 0.49, p > .62) or DBP (b = −1.28, t = −1.62, p > .10).
TABLE 4.
Racial Comparison of Stress-Blood Pressure Association Regression Results
| B | t | p | |
|---|---|---|---|
| Systolic blood pressure | |||
| Step 1 | |||
| Age | 0.92 | 1.14 | .26 |
| BMI | 3.37 | 4.29 | <.001 |
| Nulliparity | −0.88 | −1.13 | .26 |
| Adjusted income | −0.71 | −0.75 | .45 |
| Education | −1.31 | −1.60 | .11 |
| Step 2 | |||
| Race | −0.90 | −1.02 | .31 |
| Composite stress index | 0.74 | 0.89 | .37 |
| Step 3 | |||
| Race × composite stress | 1.89 | 2.33 | .02 |
| Diastolic Blood Pressure | |||
| Step 1 | |||
| Age | −0.02 | −0.22 | .83 |
| BMI | 0.27 | 2.81 | .006 |
| Nulliparity | −0.13 | −1.10 | .27 |
| Adjusted income | −0.07 | −0.52 | .61 |
| Education | −0.01 | −0.12 | .91 |
| Step 2 | |||
| Race | 0.01 | 0.08 | .94 |
| Composite stress index | −0.04 | −0.39 | .70 |
| Step 3 | |||
| Race × composite stress | 0.32 | 3.12 | .002 |
Race is coded as − 1 = white, 1 = African American; BMI = body mass index.
Stress, Blood Pressure, and Birthweight
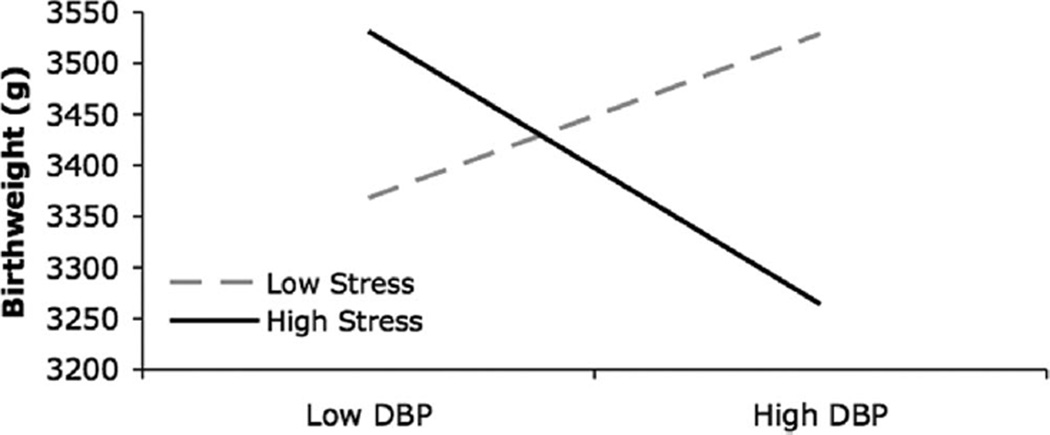
Regression analyses examining relationships between stress, BP, and birthweight controlled for age, nulliparity, BMI, education, and adjusted income in step 1; composite stress and BP were entered independently in step 2; and a composite stress × BP interaction variable was entered in the final step. In the model involving SBP, SBP was not statistically related to birthweight (p > .30). In a separate model, DBP and composite stress did not independently predict birthweight (b = −20.27 and −35.96, respectively, p > .50); however, the composite stress × DBP interaction was significant (b = −107.04, t = −2.06, average ΔR2 = 0.03, p < .04), indicating that the relationship between DBP and birthweight differs at high and low levels of stress. The interaction is depicted in Figure 1.
Figure 1.
Predicted stress by blood pressure interaction on birthweight values plotted using Aiken and West’s (48) procedure for graphing interactions between continuous variables. DBP =diastolic blood pressure.
To further examine the hypothesis that, under conditions of high stress, there would be a negative association between DBP and birthweight, regions of significance analyses (46) revealed that there was a negative association between DBP and birthweight that was statistically significant (b = –211.96, p = .05) when composite stress was ≥2.08 SD above the mean. When stress was low, regions of significance analyses indicated that the positive association between DBP and birthweight depicted in Figure 1 was not reliable (i.e., no region of significance was indicated). Therefore, these analyses show that, in the current sample, there is not a reliable relationship between DBP and birthweight when stress is low, but there is a negative association between DBP and birthweight when stress is high.
In a final model, length of gestation was added to the first step of the regression to determine if the results are due to timing of delivery. The birthweight variable proxies fetal growth when length of gestation is controlled. Length of gestation was the only significant predictor of birthweight in the first step (b = 191.79, t = 10.26, p < .01). Stress and DBP continued to be unrelated to birthweight independently and the stress × DBP interaction remained significant (b = –77.48, t = –1.94, average ΔR2 = 0.01, p = .05).
Racial Differences in Prevalence and Susceptibility
To examine if the prevalence of high DBP and high stress differed by race, the number of individuals in each racial group falling above the sample mean on both variables was compared. In the four imputed datasets, 38.63% of the African American women fell above both the composite stress index mean (0.00) and the DBP mean (63.68 mm Hg), whereas 19.78% of the white women did. A χ2 test of independence revealed this was a significant difference in frequency (χ2 = 7.07, p < .01). To examine if the effect of a stress by DBP interaction on birthweight differed by racial group, a three-way, composite stress × DBP × race interaction variable was added to a regression analysis of birthweight. This interaction was not significant (p > .20). Thus, it seems that in this study there is no support for a model in which African American women were more susceptible than white women to the effects of high stress combined with high DBP, but there was support for a model in which African American women had a significantly greater prevalence of high stress combined with high DBP.
DISCUSSION
Several hypotheses regarding racial differences in stress, BP, and infant birthweight were tested with support obtained for some. We hypothesized that there would be racial differences in associations between stress and resting BP during pregnancy, and this was confirmed. Stress was significantly and positively associated with SBP and DBP in African Americans but not in whites, and this result was not an artifact of racial differences in stress or BP. Contrary to our hypotheses, there was no racial difference in the composite stress index or BP. As expected, African American women had lower birthweight infants than white women. The hypothesis concerning the joint effects of high stress and high BP on birthweight was confirmed for DBP, but not for SBP. That is, although there were no main effects of DBP or stress on birthweight, there was a significant interaction between the composite stress index and DBP such that women with both high stress and high DBP gave birth to the smallest infants whereas women who had only one risk factor (high DBP or high stress) gave birth to babies with the highest birthweights in the sample.
When we controlled for length of gestation in a regression analysis of birthweight, the stress by DBP interaction remained significant, suggesting that shortened gestation is not the primary pathway through which stress and DBP profiles are affecting birthweight. The stress by DBP effect on fetal growth may involve pathways such as constricted blood flow to the uterus or related physiological processes including well-documented changes in neuroendocrine levels, such as increases in corticotropin releasing hormone (47) or changes in immune system functioning, e.g., shifts from Th1 to Th2 (48). Future research should consider these and other physiological pathways.
Whether racial disparities in health reflect greater prevalence of risk factors in African Americans, greater susceptibility to the effects of risk factors, or some combination of prevalence and susceptibility is central to our understanding of racial disparities in birth outcomes (2). A regression involving a three-way stress by DBP by race interaction did not reveal evidence that African American infant birthweights were more sensitive than white infant birthweights to the effects of high stress and high DBP. The presence of this combination had similar effects on birthweight for both racial groups, which suggests a valuable general risk profile. However, African American women were twice as likely as white women to have high stress and high DBP. This pattern of prevalence is consistent with national statistics of birthweight and race; African American women are about two times more likely to give birth to low birthweight infants (1). Thus, screening for this profile is useful in all pregnant women but especially in African American women.
Our results must be seen in light of the fact that we conducted a number of tests involving a small sample of African American women. Post hoc power analyses indicated that our interaction analyses had moderate statistical power (~0.60). This indicates that Type II error may have occurred and some relationships between race, stress, BP, and birthweight may not have been detected (49). It is also important to consider that the stress by DBP interaction explained 3% of the variance in birthweight after controlling first for the effects of more traditional factors (e.g., SES, BP, and stress). Regions of significance analyses indicated that women with high stress (2 SD above the mean) had infants that were 211 g lower in birthweight for every 7 mm Hg (1 SD) increase in maternal DBP. Overall, given this study’s moderate power and the meaningful amount of variance in birth outcome explained, we believe, that this initial finding of a stress by DBP interaction effect on birthweight provides a worthy basis for replication and extension.
This sample of pregnant women was recruited in prenatal clinics and the offices of private physicians, thereby excluding women without access to healthcare who may have fewer socioeconomic resources, higher levels of stress, and poorer overall health status than the participants in this study. Thus, this sample provided a unique opportunity to examine biological and psychosocial characteristics of an African American population at disproportionate risk for an array of adverse pregnancy outcomes at the same time controlling for many of the variables already known to adversely influence health (e.g., lack of access to quality healthcare). Our sample also had low incidence of hypertension. However, a sample of hypertensive women would have been more likely to be receiving treatment, and the use of a continuous BP variable, instead of a categorical one (i.e., hypertensive versus normotensive) allowed us to identify factors associated with at-risk status rather than those associated with post diagnoses status and treatment (9). Relationships among stress, BP, and birthweight would be expected to be even stronger in a higher risk sample of very poor pregnant women with higher stress and higher BP. The stress-BP association evident in the African American women in this study suggests that, even in a lower-risk subgroup, the tendency to have a combination of high stress and high resting DBP may hold important implications for the growth and development of the fetus and pregnancy outcomes.
We used allostatic load as a theoretical framework for our study, suggesting that racial differences in lifetime stress may contribute to racial differences in physiological functioning and racial health disparities (50). However, because the composite stress measure did not reveal racial differences in stress, it is not clear that allostatic load can explain racial differences in stress and BP associations in the current sample. Also, without direct evidence of chronic wear and tear to stress response systems and because of the physiological adaptations of pregnancy not considered by allostatic load theory, we must be cautious in interpreting allostatic load as the root cause of the patterns uncovered here. It is possible that genetic differences in racial groups predispose African Americans to have higher BP (51–53) or exaggerated reactions to environmental stress (27). In addition, experiences of racism and discrimination may have important effects on African American women’s stress accumulation, physiology, and birth outcomes (2,14,23). We did not consider racism stressors in the current study and an allostatic load perspective may not account for potentially unique physiological effects of stressors like these (54,55). Our understanding of the health-related consequences of stress in African Americans will benefit from consideration of alternative models of stress, the inclusion of racism- and discrimination-associated stress measures, and their interactions with physiological parameters in future research (37).
Our results suggest that particular attention needs to be directed to pregnant women who have both high stress and high DBP. Because of adaptive physiological (11) and psychological (56,57) changes that occur during pregnancy, relatively high DBP or high stress may not independently confer risk. However, if high DBP and high stress are both present, women may be at significantly greater risk of a poor birth outcome and warrant extra intervention during pregnancy. In addition, because African American women are at greater risk of the combination of these risk factors than white women, these results are relevant to try to reduce racial disparities in low birthweight.
In summary, both stress and BP have individually been implicated as relevant to racial disparities in adverse birth outcomes. Our findings are the first, however, to suggest that a) the combined effect of stress and DBP is interactive and that b) women who are facing high stress are susceptible to the potentially negative impact of higher DBP on their infant’s birthweight. Furthermore, our findings suggest that the combined impact of stress and DBP may contribute to a racial disparity in infant birthweight. Unlike white women, the levels of chronic stress and high DBP in African American women are interrelated during pregnancy and there is a significantly greater prevalence of African American women with this profile. The combined impact of multiple risk factors is a promising avenue to add to the ongoing search for an understanding and eradication of persistent racial disparities in pregnancy outcomes and health.
Acknowledgments
We would like to acknowledge the contributions of Christine Rini, PhD, Sarah Roper Coleman, MA, Susan Jackman, RN, and Joan Herberg, who were members of the research team, as well as members of the Dunkel Schetter Lab at UCLA. We also thank Wendy Troop-Gordon, PhD, for assistance with the data analysis.
This research was supported by Grant R01-HD28413 and T32-MH15750 fellowships from the National Institute for Child Health and Human Development (C.J.H., C.A.).
Glossary
- BP
blood pressure
- DBP
diastolic blood pressure
- SBP
systolic blood pressure
- BMI
body mass index
- Ms
means
Footnotes
Differences in stress, blood pressure, and pregnancy outcome relationships over time are presented elsewhere (C.J.H, C.D.S, C.J.H., L.G., C.S., unpublished data 2006).
This 12-item version included the published 10-item version and the following two questions derived from the original 14-item PSS (38): “How often have you dealt successfully with day-to-day problems and hassles?” and “How often have you felt that you were coping well or effectively handling the important changes that were occurring in your life?” This version correlated r =.99 with the 10-item version at both time points.
REFERENCES
- 1.Institute of Medicine. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 2.Giscombe´ CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: the impact of stress, racism, and related factors in pregnancy. Psychol Bull. 2005;131:662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, Johnson MJ. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175:1317–1324. doi: 10.1016/s0002-9378(96)70048-0. [DOI] [PubMed] [Google Scholar]
- 4.Lu MC, Chen B. Racial and ethnic disparities in preterm birth: the role of stressful life events. Am J Obstet Gynecol. 2004;191:691–699. doi: 10.1016/j.ajog.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 5.American Heart Association. Heart Disease and Stroke Statistics — 2005 Update. Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 6.Geronimus AT, Andersen HF, Bound J. Differences in hypertension prevalence among U.S. black and white women of childbearing age. Public Health Rep. 1991;106:393–399. [PMC free article] [PubMed] [Google Scholar]
- 7.Cunningham G, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstron KD. William’s Obstetrics. 21st ed. New York: McGraw Hill; 2001. [Google Scholar]
- 8.Goldenberg RL, Cliver SP, Cutter GR, Davis RO, Hoffman HJ, Wen SW. Blood pressure, growth retardation, and preterm delivery. Int J Technol Assess Health Care. 1992;8(Suppl 1):82–90. doi: 10.1017/s0266462300012952. [DOI] [PubMed] [Google Scholar]
- 9.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- 10.MacGillivray I, Rose G, Rowe B. Blood pressure survey during pregnancy. Clin Sci. 1969;37:395. [PubMed] [Google Scholar]
- 11.Torgersen KL, Curran CA. A systematic approach to the physiologic adaptations of pregnancy. Crit Care Nurs Q. 2006;29:2–19. doi: 10.1097/00002727-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Hobfoll SE, Schwarzer R, Chon KK. Disintangling the stress labyrinth: interpreting the meaning of the term stress as it is studied in health context. Anxiety Stress Coping. 1998;11:181–212. [Google Scholar]
- 13.Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. J Pers Soc Psychol. 1993;64:131–140. doi: 10.1037//0022-3514.64.1.131. [DOI] [PubMed] [Google Scholar]
- 14.Geronimus AT. The weathering hypothesis and the health of African American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–221. [PubMed] [Google Scholar]
- 15.Zambrana RE, Dunkel-Schetter C, Collins NL, Scrimshaw SC. Mediators of ethnic-associated differences in infant birth weight. J Urban Health. 1999;76:102–116. doi: 10.1007/BF02344465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoffman S, Hatch MC. Stress, social support and pregnancy outcome: a reassessment based on recent research. Paediatr Perinat Epidemiol. 1996;10:380–405. doi: 10.1111/j.1365-3016.1996.tb00063.x. [DOI] [PubMed] [Google Scholar]
- 17.Stanton AL, Lobel M, Sears S, DeLuca RS. Psychosocial aspects of selected issues in women’s reproductive health: current status and future directions. J Consult Clin Psychol. 2002;70:751–70. doi: 10.1037//0022-006x.70.3.751. [DOI] [PubMed] [Google Scholar]
- 18.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–2101. [PubMed] [Google Scholar]
- 19.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- 20.Norbeck JS, Anderson NJ. Psychosocial predictors of pregnancy outcomes in low-income black, Hispanic, and white women. Nurs Res. 1989;38:204–209. [PubMed] [Google Scholar]
- 21.Orr ST, James SA, Miller CA, Barakat B, Daikoku N, Pupkin M, Engstrom K, Huggins G. Psychosocial stressors and low birthweight in an urban population. Am J Prev Med. 1996;12:459–466. [PubMed] [Google Scholar]
- 22.Collins JW, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94:2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parker Dominguez T, Dunkel Schetter C, Glynn L, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychology. doi: 10.1037/0278-6133.27.2.194. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13:646–652. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20:315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- 26.Chen E, Matthews KA, Salomon K, Ewart CK. Cardiovascular reactivity during social and nonsocial stressors: do children’s personal goals and expressive skills matter? Health Psychol. 2002;21:16–24. [PubMed] [Google Scholar]
- 27.Gump BB, Matthews KA, Raikkonen K. Modeling relationships among socioeconomic status, hostility, cardiovascular reactivity, and left ventricular mass in African American and white children. Health Psychol. 1999;18:140–150. doi: 10.1037//0278-6133.18.2.140. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro D, Goldstein IB, Jamner LD. Effects of cynical hostility, anger out, anxiety, and defensiveness on ambulatory blood pressure in black and white college students. Psychosom Med. 1996;58:354–364. doi: 10.1097/00006842-199607000-00008. [DOI] [PubMed] [Google Scholar]
- 29.de Weerth C, Buitelaar JK. Physiological stress reactivity in human pregnancy—a review. Neurosci Biobehav Rev. 2005;29:295–312. doi: 10.1016/j.neubiorev.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Matthews KA, Rodin J. Pregnancy alters blood pressure responses to psychological and physical challenge. Psychophysiology. 1992;29:232–240. doi: 10.1111/j.1469-8986.1992.tb01691.x. [DOI] [PubMed] [Google Scholar]
- 31.Manuck SB, Kaplan JR, Adams MR, Clarkson TB. Effects of stress and the sympathetic nervous system on coronary artery atherosclerosis in the cynomolgus macaque. Am Heart J. 1988;116:328–333. doi: 10.1016/0002-8703(88)90110-x. [DOI] [PubMed] [Google Scholar]
- 32.Lovallo WR, Gerin W. Psychophysiological reactivity: mechanisms and pathways to cardiovascular disease. Psychosom Med. 2003;65:36–45. doi: 10.1097/01.psy.0000033128.44101.c1. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosschot JF, Thayer JF, Christenfeld N, Linden W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 2003;65:22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- 34.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 1987. [Google Scholar]
- 35.Schafer JL, Olsen MK. Multiple imputation for multivariate missing-data problems: a data analyst’s perspective. Multivariate Behavioral Research. 1998;33:545–571. doi: 10.1207/s15327906mbr3304_5. [DOI] [PubMed] [Google Scholar]
- 36.Schafer JL. NORM: multiple imputation of incomplete multivariate data under a normal model, version 2. Software for Windows 95/98/NT. 1999 Available at http://www.stat.psu.edu/~jls/misoftwa.html.
- 37.Parker Dominguez T, Dunkel Schetter C, Mancuso R, Rini CM, Hobel C. Stress in African American pregnancies: testing the roles of various stress concepts in prediction of birth outcomes. Ann Behav Med. 2005;29:12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- 38.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 39.Lobel M, Dunkel-Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: a prospective study of socioeconomically disadvantaged women. Health Psychol. 1992;11:32–40. doi: 10.1037//0278-6133.11.1.32. [DOI] [PubMed] [Google Scholar]
- 40.Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Garite TJ. The association between prenatal stress and infant birth weight and gestational age at birth: a prospective investigation. Am J Obstet Gynecol. 1993;169:858–865. doi: 10.1016/0002-9378(93)90016-c. [DOI] [PubMed] [Google Scholar]
- 41.Spielberger CD. Assessment of state and trait anxiety: conceptual and methodological issues. Southern Psychologist. 1985;2:6–16. [Google Scholar]
- 42.Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18:333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- 43.Lobel M. Conceptualizations, measurement, and effects of prenatal maternal stress on birth outcomes. J Behav Med. 1994;17:225–272. doi: 10.1007/BF01857952. [DOI] [PubMed] [Google Scholar]
- 44.Roesch SC, Schetter CD, Woo G, Hobel CJ. Modeling the types and timing of stress in pregnancy. Anxiety Stress Coping. 2004;17:87–102. [Google Scholar]
- 45.Aiken LS, West SG. Multiple regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- 46.Bauer DJ, Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- 47.de Weerth C, Buitelaar JK. Physiological stress reactivity in human pregnancy—a review. Neurosci Biobehav Rev. 2005;29:295–312. doi: 10.1016/j.neubiorev.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 48.Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14:353–356. doi: 10.1016/0167-5699(93)90235-D. [DOI] [PubMed] [Google Scholar]
- 49.Cohen J, Cohen P, Aiken LS, West SG. Applied Multiple Regression/ Correlation Analyses for the Behavioral Sciences. New Jersey: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- 50.Rich-Edwards JW, Krieger N, Majzoub J, Zierler S, Lieberman E, Gillman M. Maternal experiences of racism and violence as predictors of preterm birth: rationale and study design. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):124–135. doi: 10.1046/j.1365-3016.2001.00013.x. [DOI] [PubMed] [Google Scholar]
- 51.Dimsdale JE. Stalked by the past: the influence of ethnicity on health. Psychosom Med. 2000;62:161–170. doi: 10.1097/00006842-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 52.Gleiberman L. Salt, hypertension, evolution. Psychosom Med. 2001;63:325–327. doi: 10.1097/00006842-200103000-00021. [DOI] [PubMed] [Google Scholar]
- 53.Kaufman JS. No more “slavery hypothesis” yarns. Psychosom Med. 2001;63:324–325. doi: 10.1097/00006842-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 54.Dallman MF. Stress by any other name…? Horm Behav. 2003;43:18–20. doi: 10.1016/s0018-506x(02)00034-x. discussion 8–30. [DOI] [PubMed] [Google Scholar]
- 55.Day TA. Defining stress as a prelude to mapping its neurocircuitry: no help from allostasis. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:1195–1200. doi: 10.1016/j.pnpbp.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 56.Glynn LM, Dunkel Schetter C, Wadhwa PD, Sandman CA. Pregnancy affects appraisal of negative life events. J Psychosom Res. 2004;56:47–52. doi: 10.1016/S0022-3999(03)00133-8. [DOI] [PubMed] [Google Scholar]
- 57.Glynn LM, Wadhwa PD, Dunkel-Schetter C, Chicz-Demet A, Sandman CA. When stress happens matters: effects of earthquake timing on stress responsivity in pregnancy. Am J Obstet Gynecol. 2001;184:637–642. doi: 10.1067/mob.2001.111066. [DOI] [PubMed] [Google Scholar]