Abstract
The present investigation evaluated the factor structure of the Distress Tolerance Scale (DTS; Simons and Gaher 2005) among a sample of 173 (54.9% males) daily cigarette smokers (M=16.64 cigarettes per day, SD=7.83). Comparison of a single higher-order model and a hierarchical multidimensional model was conducted using confirmatory factor analyses (CFA). In addition, evaluation of the internal consistency and convergent and discriminant validity of the better-fitting model was completed. CFA of the DTS indicated a single second-order factor of distress tolerance, and four lower-order factors including Tolerance, Appraisal, Absorption, and Regulation; each factor demonstrated acceptable levels of internal consistency. In addition, the DTS displayed good convergent and discriminant validity with theoretically relevant smoking and affect variables. Results are discussed in terms of explicating the latent structure of distress tolerance, as measured by the DTS, within the context of smoking research.
Keywords: Distress tolerance, Distress intolerance, Emotion regulation, Cigarette smokers, Nicotine, Substance use, Confirmatory factor analysis
Distress tolerance reflects the perceived or actual ability to withstand negative affect or other aversive psychological and/or physical states (Brown et al. 2005; Leyro et al. 2010). Numerous conceptual models of psychopathology suggest distress (in)tolerance may play a central explanatory role in the production and maintenance of a variety of psychological disorders (Zvolensky et al. 2010).
Theory on distress tolerance and substance use behavior, in particular, has posited that persons with lower levels of distress tolerance may be sensitive and reactive to distressing states elicited by addiction processes and engage in use to regulate such states. Specifically, persons with low levels of distresss tolerance may be particularly prone to pursuit of negative reinforcement opportunities to escape/avoid or reduce distressing experiential states in the form of substance use (i.e. self-medication or coping oriented drug use; Leyro et al. 2010). Failure to inhibit such avoidance behavior may be a central process underlying substance use maintenance (Richards et al. 2010). For example, a low threshold for tolerating negative affect and other aversive internal states, which routinely occur during smoking deprivation (e.g., withdrawal symptoms, bodily sensations), may be associated with increased smoking behavior aimed at temporarily ameliorating—perceptually or objectively—such experiential discomfort (Baker et al. 2004; Hajek 1991; Parrott 1999; Zvolensky et al. 2003). Consistent with this perspective, Hajek and colleagues (Hajek 1991; Hajek et al. 1987; West et al. 1989) found that daily smokers with lower levels of distress tolerance for physical discomfort (bodily sensations) reported shorter durations of abstinence from smoking. Similarly, daily smokers who relapse faster than their counterparts also tend to demonstrate lower levels of distress tolerance on laboratory-based stress tasks (e.g., Brandon et al. 2003; Brown et al. 2002; Brown et al. 2008). Other work indicates that the perceived capacity to tolerate emotional distress is significantly and uniquely related to smoking motives aimed at mood and addiction management (Leyro et al. 2008). Overall, distress tolerance is a promising explanatory factor with regard to smoking cessation outcomes and motives, a position consistent with contemporary theoretical models of smoking behavior (e.g., Brown et al. 2005).
To index distress tolerance, Simons and Gaher (2005) developed a promising self-report measure entitled the Distress Tolerane Scale (DTS). The DTS is specifically aimed at measuring the perceived capacity to tolerate distress from a multidimensional framework. There are four components to the DTS model: an individual’s (1) ability to tolerate emotions (tolerance); (2) assessment of the emotional situation as acceptable (appraisal); (3) level of attention absorbed by the negative emotion and relevant interference with functioning (absorption); and (4) ability to regulate emotion (regulation). Items are rated on a 5-point Likert scale (5=Strongly disagree to 1=Strongly agree), with higher scores corresponding to greater levels of distress tolerance. (Please see Table 2 for full-text of items). To date, factor analytic work on the DTS has been conducted exclusively on college student samples (Simons and Gaher 2005). The initial factor analytic findings supported a single latent global distress tolerance factor; however, secondary factor analyses supported an alternative, and stronger, hierarchical multidimensional model with a single second-order factor, global distress tolerance, and four first-order factors (Simons and Gaher 2005).
Table 2.
Standardized factor loadings (and Standard Errors) for Single- and Four-Factor (Hierarchical Multidimensional) solutions of the DTS
| Item Number | Single-factor | Four-Factor (Hierarchical Multidimensional) |
|||
|---|---|---|---|---|---|
| DTS | Tolerance | Absorption | Appraisal | Regulation | |
| 1. Feeling distress or upset is unbearable to me. | 0.69 (0.08) | 0.75 (0.08) | |||
| 2. When I feel distressed or upset, all I can think about is how bad I feel. | 0.67 (0.10) | 0.75 (0.09) | |||
| 3. I can’t handle feeling distressed or upset. | 0.79 (0.08) | 0.86 (0.09) | |||
| 4. My feelings of distress are so intense that they completely take over. | 0.77 (0.09) | 0.80 (0.09) | |||
| 5. There’s nothing worse than feeling distressed or upset | 0.25 (0.15) | 0.29 (0.15) | |||
| 6. I can tolerate being distressed or upset as well as most people. (reverse scored) | 0.48 (0.14) | 0.49 (0.14) | |||
| 7. My feelings of distress or being upset are not acceptable. | 0.67 (0.10) | 0.70 (0.10) | |||
| 8. I’ll do anything to avoid feeling distressed or upset. | 0.54 (0.13) | 0.74 (0.12) | |||
| 9. Other people seem to be able to tolerate feeling distressed or upset better than I can. | 0.74 (0.11) | 0.77 (0.10) | |||
| 10. Being distressed or upset is always a major ordeal for me. | 0.78 (0.08) | 0.79 (0.08) | |||
| 11. I am ashamed of myself when I feel distressed or upset. | 0.69 (0.11) | 0.71 (0.11) | |||
| 12. My feelings of distress or being upset scare me. | 0.71 (0.09) | 0.74 (0.09) | |||
| 13. I’ll do anything to stop feeling distressed or upset. | 0.60 (0.13) | 0.83 (0.14) | |||
| 14. When I feel distressed or upset, I cannot help but concentrate on how bad the distress actually feels. | 0.72 (0.10) | 0.78 (0.09) | |||
| Higher Order DTS (from Four-Factor model) | 0.93 (0.05) | 0.92 (0.06) | 0.92 (0.05) | 0.70 (0.15) | |
DTS Distress Tolerance Scale (Simons and Gaher 2005)
Despite the theoretical and empirical importance of distress tolerance for smoking behavior (Brown et al. 2005; Richards et al. 2010), there has been no direct empirical exploration of Simons and Gaher’s (2005) perceived affective distress tolerance construct, as indexed by the DTS, among smokers. To address this gap in the existing literature, the aim of the current investigation was to examine the factor structure, internal consistency, and convergent/discriminant validity of the DTS and factor analytically derived DTS subscale scores among daily cigarette smokers. Based on previous factor analytic work by Simons and Gaher (2005), as well as its intended multidimensional framework, it was hypothesized that a hierarchical multidimensional model of the DTS, comprised of a global second-order distress tolerance factor predicting four first-order factors, would be supported over a single higher-order model. It was additionally important to examine the single and multidimensional models given the mixed findings by Simons and Gaher (2005) yielding moderate support for both.
In addition, extant research on distress tolerance among smokers suggests potentially important relations between the global perceived distress tolerance construct and smoking cessation as well as expectancies and motives related to smoking. However, because such research has focused upon global distress tolerance, it is unclear whether or how specific facets of distress tolerance, as delineated by Simon and Gaher’s (2005) multidimensional model, may operate within this context. Exploration of the latent nature of distress tolerance via examination of single and multidimensional models will thereby help clarify whether these extant associations may be better-explained by a specific lower-order facet(s) of perceived distress tolerance or a single global distress tolerance construct.
Finally, the DTS also was expected to demonstrate internally consistent factors (Cronbach’s alpha ≥ .70; Nunnally and Bernstein 1994) as well as convergent and discriminant validity with regard to its associations to a range of theoretically-relevant smoking, affect, and demographic variables. We chose to examine a specfic set of theoretically-relevant smoking and affect variables based on extant findings indicating that distress tolerance among smokers is related to cessation duration and relapse as well as expectancies and motives related to smoking (e.g. Brown et al. 2002, 2008; Hajek 1991, Hajek et al. 1987; West et al. 1989; Leyro et al. 2008; Richards et al. 2010).
Method
Participants and Procedure
Participants recruited from the greater Burlington, Vermont community via advertisements placed throughout various community settings and university-based bulletin boards and classrooms. Please see the Results Section for a comprehensive presentation of the participant characteristics. During the study, participants (1) provided verbal and written informed consent; (2) underwent a diagnostic interview (SCID-NP), conducted by a trained doctoral-level student, in order to determine presence of study exclusion criteria (please see below); (3) provided CO analysis of breath samples to biochemically verify smoking status; and (4) completed a battery of self-report measures to assess both affective variables and smoking history characteristics. Exclusionary criteria included: (1) limited mental competancy or the inability to provide informed, written consent; (2) current suicidal or homicidal ideation; and (3) current or past history of psychotic symptoms.
Measures
The Structured Clinical Interview for DSM-IV Axis I Disorders- Non-Patient Edition (SCID-NP)
The SCID-NP (First et al. 1994) is a well-established diagnostic interview for psychiatric problems.
Smoking History Questionnaire (SHQ; Brown et al. 2002)
The SHQ is a continuous self-report questionnaire used to assess smoking history and pattern. The SHQ includes 20 items pertaining to smoking rate, age of onset of smoking initiation, and years of being a daily smoker. The SHQ has been successfully used in previous studies as a measure of smoking history (e.g., Zvolensky et al. 2004).
Fagerström Tolerance Questionnaire (FTQ; Fagerström 1978)
The FTQ was used as a continuous self-report measure of nicotine dependence and cigarettes smoked per day. Specifically, the FTQ was administered, and it was scored as the Fagerström test for Nicotine Dependence (FTND; Heatherton et al. 1991). The FTND has shown good internal consistency, positive relations with smoking variables (e.g., saliva cotinine; Heatherton et al. 1991; Payne et al. 1994), and high degrees of test-retest reliability (Pomerleau et al. 1994).
Carbon Monoxide Analysis
Biochemical verification of smoking history was completed by CO analysis of breath samples (10 ppm cutoff; Cocores 1993). Expired air CO levels were assessed using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.). CO analysis of breath samples were used to verify smoking status at the baseline appointment, where data for the current investigation was obtained.
Alcohol Use Disorders Identification Test (AUDIT; Babor et al. 1992)
The AUDIT is a 10-item self-report screening measure developed by the World Health Organization to assess frequency of alcohol consumption and to identify individuals with alcohol problems (Babor et al. 1992). Frequency and quantity items of the AUDIT were used to index weekly alcohol consumption (an average weekly-based frequency by quantity per occasion composite score), and the AUDIT total score was utilized to identify current difficulties with alcohol use (Babor et al. 1992). There is a large body of literature documenting the psychometric properties of the AUDIT (Saunders et al. 1993).
Distress Tolerance Scale (DTS; Simons and Gaher 2005)
The 14-item DTS was utilized for the current investigation. The original 14-item, rather than the current 15-item, version of the DTS was used as a function of the time period during which these data were collected. The item not included in this version (i.e., “When I feel distressed or upset, I must do something about it immediately”) is not part of the DTS total score, but it is one of three regulation subscale items. A detailed description of the DTS was provided in the Introduction section of this paper, and thus, is not repeated here.
Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991)
The SCQ (Brandon and Baker 1991) is a 50-item self-report measure that assesses smoking expectancies on a 0–9 scale for likelihood of occurrence, ranging from 0= “completely unlikely” to 9= “completely likely.” The entire measure and its constituent factors have demonstrated sound psychometric properties (Buckley et al. 2005; Brandon and Baker 1991; Downey and Kilbey 1995). The subscales demonstrated strong internal consistency (SCQ-Negative Personal Consequences, α=.91; SCQ-Positive Reinforcement, α=.92; SCQ-Negative Reinforcement, α=.92; and SCQ-Appetite, α=.91) among the current sample.
Positive Affect Negative Affect Scale (PANAS; Watson et al. 1988)
The PANAS is a 20-item measure on which respondents indicate, on a 5-point Likert-type scale (1 =very slightly or not at all to 5=extremely), the extent to which they generally feel different feelings and emotions (e.g., “Hostile”). The PANAS is a well-established mood measure commonly used in psychopathology research (Watson et al. 1988). Factor analysis indicates that it assesses two global dimensions of affect: negative affect (PANAS-NA) and positive affect (PANAS-PA). A large body of literature supports the psychometric properties of the PANAS (see Watson 2000). The subscales demonstrated strong internal consistency (PANAS-NA, α=.90; PANAS-PA, α=.87) among the current sample.
Data Analytic Strategy
The data analytic plan had three components. First, the sample variance-covariance matrix of the 14-item DTS (Simons and Gaher 2005) was analyzed using a linear structural relations program and a maximum-likelihood minimization function (LISREL 8.80; Jöreskog and Sörbom 2006) to test both the single-factor and four-factor models previously identified by Simons and Gaher (2005). Each item was constrained to load onto one factor in accordance with the original model proposed by Simons and Gaher (2005).
With regard to the multidimensional model (i.e., involving more than one latent exogenous variable), the factors were permitted to correlate although measurement errors were forced to be independent. This approach was chosen because it was believed that latent factors were related and explained by a higher order factor, while each indicator was believed to measure one overarching latent construct.
In addition to examination of the overall model χ2 (e.g., Bollen 1989), Goodness-of-fit was evaluated using a comprehensive set of fit indices including: χ2 (e.g. Bollen 1989), Standardized Root Mean Square Residual (SRMR; Hu and Bentler 1995), Root Mean Square Error of Approximation (RMSEA; Browne and Cudeck 1993), p value for test of close fit (RMSEA<.05; CFit; Brown 2006), the Comparative Fit Index (CFI; Bentler 1990), and the Tucker-Lewis Index (TLI; Bentler and Bonett 1980). Multiple indices were selected to provide comprehensive data regarding model fit (i.e., absolute fit, fit adjusting for model parsimony, fit relative to a null model); evaluated together, these indices provide a conservative and reliable evaluation of the tested models (Jaccard and Wan 1996). Because the competing single-factor and four-factor (hierarchical multidimensional) models were nested (e.g. the single-factor model was comprised of a subset of the free parameters of the four-factor model), comparative fit was evaluated using the χ2 difference test.
Second, Cronbach’s alpha was used to document internal consistency of the better-fitting model. Finally, zero-order correlations were computed between the DTS total and subscale factor scores in relation to the smoking, affect, and demographic variables to evaluate convergent and discriminant validity.
Results
Participants
Participants were 173 (54.9% males) adult smokers (Mage=27.68 years, SDage=11.79). The racial distribution of the sample was consistent with that of the State of Vermont (State of Vermont Department of Health 2007)— 94.8% of participants identified as White/Caucasian, 2.3% African American/Black, 1.2% Hispanic, and 1.7% “other”. On average, participants smoked 16.64 cigarettes per day (SD=7.83) and reported smoking daily for approximately 11.04 years (SD=11.45; range=1–48). The mean score on the Fagerström Test for Nicotine Dependence (FTND: Heatherton et al. 1991) was 3.37, indicating relatively low levels of nicotine dependence. The mean value for carbon monoxide (CO) verification of smoking status readings was 17.37 parts per million (SD=11.67) (Cocores 1993), consistent with levels of a regular daily smoker (parts per million>8). With respect to alcohol consumption, as measured by the Alcohol Use Disorders Identification Test (AUDIT; Babor et al. 1992), approximately 17.5% of the sample reported not currently consuming alcohol, 15.7% reported drinking monthly or less, 18.7% reported drinking 2 to 4 times per month, 30.7% reported drinking 2 to 3 times per week, and 17.5% reported drinking 4 or more times per week. Participants, on average, reported consuming 3 to 4 alcoholic drinks per occasion, and scored a mean of 10.78 (SD=7.72) on the AUDIT, indicating moderate alcohol use problems (Babor et al. 1992).
Confirmatory Factor Analysis
Single-factor model
First, Simon and Gaher’s (2005) single-factor model was fit to the data, yielding a χ² (77, n=173)=223.67, p<.05. However, because the χ² is restricted in a variety of ways including sensitivity to sample size and the assumption of multivariate normality, there is a likelihood of an indication of poor fit even when the model is properly specified (e.g. Bentler and Bonett 1980; McIntosh 2006). Therefore, goodness-of-fit was further evaluated. Overall, the fit was mixed: GFI=.84; AGFI=.78; SRMR=.062; RMSEA=.11 (95% CI: .09–.12); CFI=.95, TLI=.94. Although the GFI value fell just within the liberal cutoff range1, the AGFI value fell just outside the recommended range. In addition, the SRMR, RMSEA, CFI, and TLI values fell just within the more liberal cutoff range for acceptable fit (Table 1).
Table 1.
Confirmatory factor analyses of the Distress Tolerance Scale: overall model fit
| χ2 | df | p | GFI | AGFI | SRMR | RMSEA | (90% CI) | CFI | TLI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Single-Factor | 223.67** | 77 | < .001 | 0.84 | 0.78 | 0.062 | 0.11 | (0.09–0.12) | 0.95 | 0.94 |
| Four-Factor | 153.82** | 73 | < .001 | 0.89 | 0.84 | 0.049 | 0.078 | (0.060–0.096) | 0.97 | 0.97 |
| Chi-Square Difference Test | 69.85** | 4 | 0.00 | – | – | – | – | – | – | – |
p<.01
χ2 (e.g., Bollen 1989); GFI goodness-of-fit index (Jöreskog and Sörbom 1981); AGFI adjusted goodness-of-fit index (Jöreskog and Sörbom 1981); SRMR standardized root mean square residual (Hu and Bentler 1995); CFI comparative fit index (Bentler 1990); RMSEA root mean square error of approximation (Browne and Cudeck 1993); TLI Tucker-Lewis index (Bentler and Bonett 1980)
Inspection of the standardized residuals (absolute values≥ 1.96) and TD modification indices (absolute values≥3.84) indicated potential areas of strain and shared error variances; specifically, several indicator variables may share error variances and non-discriminantly tap similar facets of the construct. Item-factor loadings (range=.25–.79; p’s<.05) and standard errors (range=.08 to .15) are detailed in Table 2.
Hierarchical Multidimensional Model
Next, the hierarchical multidimensional model was fit to the data, resulting in a χ² (73, n=173)=153.82, p<0.05, indicative of poor fit. However, model fit was further inspected due to limitations of the χ² test. Overall, the fit was mixed: GFI=.89; AGFI=.84; SRMR=.049; RMSEA=.078 (95% CI: .060; .096); CFI=.97, TLI=.97. Both the GFI and AGFI fell just within the liberal cutoff ranges. In addition, the RMSEA fell just within the more liberal cutoff range of acceptable fit, whereas the SRMR, CFI, and TLI values fell within the conservative cutoff range (Table 1).
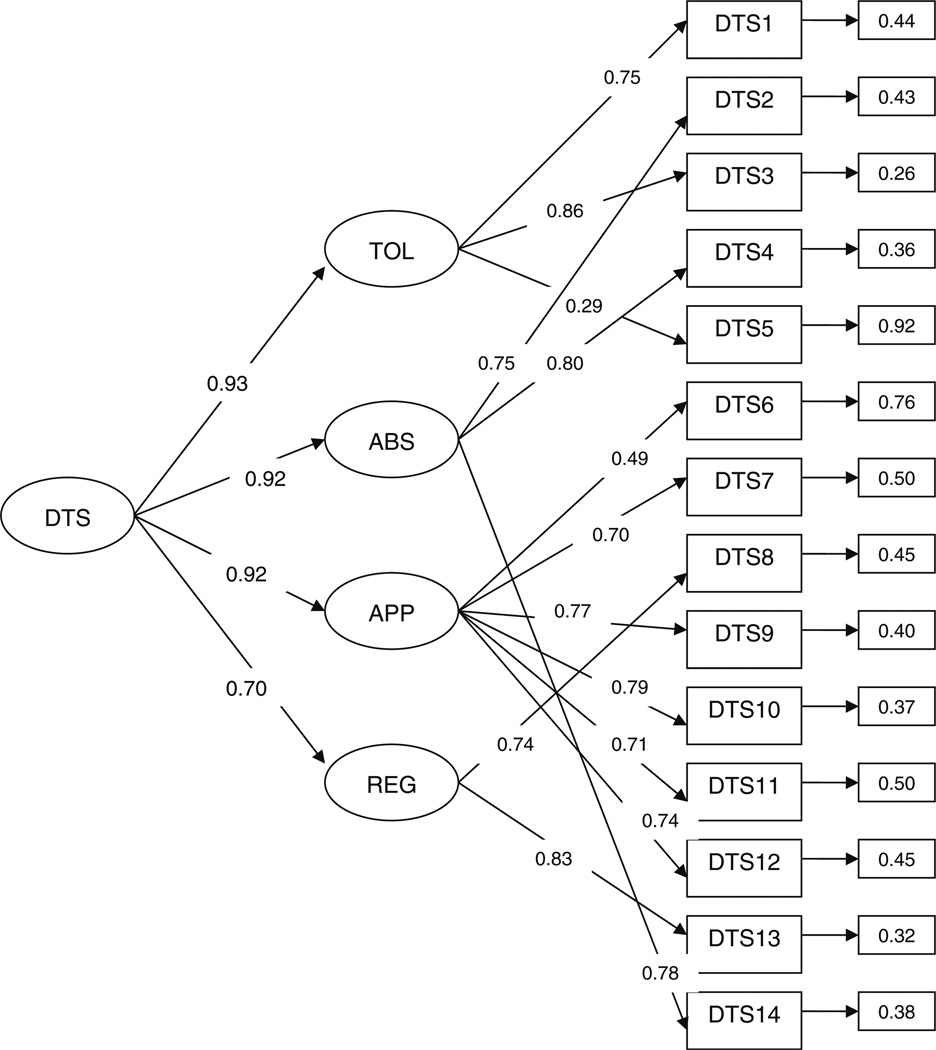
Standardized residuals (absolute values≥1.96) and LY, PSI, and TE modification indices were examined and indicated several areas of possible model strain; and the potential cross-loading of several indicator variables (items) on multiple latent factors, shared variance between first-order factors. Item-factor loadings (range=.29 to .86), subscale-factor loadings (range=.70 to .93), and standard errors (range=.05 to .15) are detailed in Fig. 1 and Table 2. Of note, error variances spanned a broad range (.26 to .92), indicating that some indicators of the putative DT factors are better than others (Fig. 1).
Fig. 1.
Standardized factor loadings and error variances for the hierarchical multidimensional model (N=173)
Observed correlations between first-order factors of tolerance, appraisal, absorption, and regulation [ETA and KSI] were high (range=.65 to .86). Here, potentially problematic large correlations (r>.80) were observed—between Tolerance and Absorption (r=.86), Tolerance and Appraisal (r=.85) and between Absorption and Appraisal (r=.85).
The nested chi-square difference test indicated that the four-factor hierarchical multidimensional model improved the model significantly relative to the single-factor model, χ² (4)=69.85, p<.001 (Table 1). Additionally, the four-factor hierarchical multidimensional model produced a lower Akaike’s Information Criterion (AIC) value than the single-factor solution (AICs=287.81 and 212.86 respectively).
Internal Consistency
Cronbach’s alpha was computed for the single second-order factor and each of the four first-order factors. The observed alpha values were as follows: DTS total score=.91, Tolerance subscale=0.66, Absorption subscale=0.83, Appraisal subscale=0.85, and Regulation subscale=0.77.
Convergent and Discrimininant Validity
Please see Table 3 for a summary of zero-order correlations. Here, we found that: (1) DTS total as well as DTS-Tolerance and DTS-Appraisal subscales were significantly negatively related to number of years as a regular (daily) smoker; (2) the DTS-Regulation subscale was significantly negatively related to number of cigarettes smoked daily; and (3) DTS total as well as Appraisal and Regulation subscales were significantly negatively related to nicotine dependence. With regard to smoking consequences, DTS total and subscale scores exhibited a variety of significant relationships to beliefs that smoking will lead to negative personal consequences (SCQ-NC), dampen negative affect (SCQ-NR), provide the smoker with positive experiences (SCQ-PR), and also help manage appetite control (SCQ-AP). With regard to positive and negative affect, only the Tolerance subscale score was significantly associated with positive affect (r=.27, p<.01) whereas the DTS total and all subscale scores were significantly negatively associated with negative affect (range r’s: −.17 to −.40, p<.05). There was no signifcant association between sex and distress tolerance (see Table 3).
Table 3.
Descriptive data and zero-order correlations among theoretically-relevant variables
| Variable Name | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | M (SD) | Range |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. DTS-Totala | – | .80* | .85** | .92** | .71 ** | −.14 | −.16* | −.13 | −.22** | −.23** | −.13 | −.27** | −.30** | .04 | −.39** | 3.43 (.87) | 1.21–5.00 |
| 2.DTS-Tolb | – | – | .66** | .63** | .47** | −.07 | −.15* | −.02 | 0.15 | −.17* | −.11 | −.19* | −.30** | .27** | −.17* | 3.37 (.94) | 1.00–5.00 |
| 3. DTS-Absc | – | – | – | .69** | .49** | −.12 | −.04 | −.06 | −.10 | −.21** | −.13 | −.24** | −.30** | .05 | −.36** | 3.33 (1.12) | 1.00–5.00 |
| 4. DTS-Appd | – | – | – | – | .57** | −.13 | −.19* | −.16 | −.26** | −.23** | −.11 | −.22** | −.26** | −.03 | −.40** | 3.59 (.99) | 1.00–5. 00 |
| 5. DTS-Rege | – | – | – | – | – | −.08 | −.09 | −.17* | −.19* | −.11 | −.13 | −.31** | −.14 | −.07 | −.30** | 3.21 (1.16) | 1. 00–5. 00 |
| 6.Sexf | – | – | – | – | – | – | −.09 | −.16* | −.23** | .14 | .02 | .06 | .24** | .01 | .09 | ______ | |
| 7. Years Smokeg | – | – | – | – | – | – | – | .36** | .44** | .02 | −.10 | −.01 | −.10 | −.02 | .05 | 11.04 (11.45) | 1. 00–48.00 |
| 8. Cig/dayh | – | – | – | – | – | – | – | – | .65** | .16* | .14 | .16* | −.02 | .14 | .20* | 16.64 (7.83) | 2.00–50.00 |
| 9. FTNDi | – | – | – | – | – | – | – | – | – | .15 | .15 | .16* | .12 | −.02 | .15 | 3.37 (1.95) | 0.00–9.00 |
| 10. SCQ-NCJ | – | – | – | – | – | – | – | – | – | – | .58** | .56** | .41** | .12 | 28** | 5.79 (1.61) | 0.00–8.94 |
| 11. SCQ-PRk | – | – | – | – | – | – | – | – | – | – | – | .78** | .32** | .17* | .33** | 5.67 (1.86) | 0.00–9.00 |
| 12. SCQ-NR1 | – | – | – | – | – | – | – | – | – | – | – | – | .36** | .12 | .39** | 5.51 (2.06) | 0.00–9.00 |
| 13. SCQ-APm | – | – | – | – | – | – | – | – | – | – | – | – | – | −.14 | .11 | 3.09 (2.38) | 0.00–9.00 |
| 14. Positive Affectivityn | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 44** | 24.14 (9.39) | 4.00–49.00 |
| 15. Negative Affectivityo | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 16.21 (9.07) | 2.00–48.00 |
N=173.
p<.05
p<.01
Distress Tolerance Scale—Total score (DTS; Simons and Gaher 2005);
Tolerance Subscale, Distress Tolerance Scale (DTS; Simons and Gaher 2005);
Absorption subscale, Distress Tolerance Scale (DTS; Simons and Gaher 2005);
Appraisal subscale, Distress Tolerance Scale (Simons and Gaher 2005);
Regulation subscale, Distress Tolerance Scale (DTS; Simons and Gaher 2005);
Sex (l=male; 2=female);
Number of years regular smoker, Smoking History Questionnaire (SHQ; Brown et al. 2002);
Cigarettes Smoked/Day,
Nicotine Dependence, Fagerström Test for Nicotine Dependence (FTND; Heatherton et al. 1991);
Negative Personal Consequences subscale, Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991);
Positive Reinforcement subscale, Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991);
Negative Reinforcement subscale, Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991);
Appetite Control subscale, Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991);
Positive Affect subscale, Positive Affect Negative Affect Scale (PANAS: Watson et al. 1988);
Negative Affect subscale, Positive Affect Negative Affect Scale (PANAS: Watson et al. 1988)
Discussion
The primary aim of the current investigation was to comparatively evaluate the latent structures of the DTS among a sample of cigarette smokers and previously observed findings among a sample of college students (Simons and Gaher 2005). Specifically, CFA demonstrated that a hierarchical, multidimensional model provided a better fit for the observed DTS data among a sample of adult smokers than a single factor model. The single factor model also fit the DTS data, but demonstrated inferior fit relative to the hierarchical, multidimensional solution. Specifically, CFA documented a single second-order factor of distress tolerance, and four lower-order factors including Tolerance, Appraisal, Absorption, and Regulation consistent with the secondary EFA and CFA examinations conducted by Simons and Gaher (2005). Theoretically, while the hierarchical, multidimensional model may be less parsimonious than the single factor model of the DTS, it does provide greater conceptual specificity of the structure and potential key elements underlying distress tolerance (Bernstein et al. 2010).
Although CFAs in the present study provided support for the hierarchical, multidimensional (four-factor) model of the DTS, a number of important caveats are noteworthy and may inform ongoing study of the DTS and related perceived distress tolerance constructs. Most importantly, the observed factor analytic model demonstrated acceptable fit indices and better fit relative to the single-factor model, but it was also characterized by several areas of potential model strain as reflected by elevated standardized residuals (absolute values≥1.96) and LY, PSI, and TE modification indices (absolute values≥3.84). A potentially greater concern regarding the validity and utility of the multidimensional model involves the high observed correlations (range=.65 to .86) between first-order factors of Tolerance, Appraisal, Absorption, and Regulation [ETA and KSI]. Specifically, potentially problematic correlations (r>.80) were observed between Tolerance and Absorption (r=.86), Tolerance and Appraisal (r=.85), and Absorption and Appraisal (r=.85). These correlations may be interpreted to mean that these first-order factors covary so strongly with one another that our conceptualization of these putatively distinct, albeit related, facets of distress tolerance is questionable (Simons and Gaher 2005). In addition, observed modification indices and standardized residuals provided further evidence of the limitedness of the multidimensional factor solution. Specifically, elevated modification indices indicated that several indicators (items) may load onto multiple lower-order factors. Elevated standardized residuals indicated shared variance between lower-order factors, and shared error variance between indicator variables. Thus, in contrast to the reported comparative model fit results, it may be advisable to consider conceptualizing perceived distress tolerance, as measured by the DTS, as a global, unidimensional construct for research and clinical purposes. Important areas for future study of the DTS may therefore involve (1) developing and testing of multiple hierarchical, multidimensional models, with potential consideration of omission or replacement of “problematic” items that may not distinguish putatively distinct lower-order factors of distress tolerance; and (2) ongoing evaluation of the differential convergent, discriminant, and predictive validity of these potentially novel multidimensional factors for understanding behavioral outcomes of interest (e.g., forms of psychopathology, smoking cessation outcome).
In terms of internal consistency, the DTS total score and Absorption, Appraisal, and Regulation subscale scores possessed good internal consistency (Cronbach’s alpha ≥ .70; Nunnally and Bernstein 1994). The only notable exception to this pattern of findings involved the relatively lower internal consistency observed for the Tolerance subscale; notably, in the present sample of smokers, we observed a slightly lower alpha score for the Tolerance subscale than that reported by Simons and Gaher (2005). Overall, the present reliability findings are highly similar to those reported by Simons and Gaher (2005), lending further empirical support to the internal consistency of the DTS among a smoking population.
The DTS displayed relatively good convergent and discriminant validity across a range of theoretically-relevant smoking and affect variables. In terms of the association between the DTS and smoking-related variables, lower levels of global distress tolerance were related to greater number of years as a regular smoker as well as greater levels of nicotine dependence but not daily smoking rate. In terms of the DTS subscales, the tendency to assess an emotional situation as acceptable was associated with fewer years of being a smoker and lower levels of nicotine dependence. Furthermore, a greater ability to regulate distressing emotions appropriately was associated with decreased levels of nicotine dependence and smoking rate. The findings parallel previous examination of the DTS and its subscales suggesting a significant association between ability to regulate emotions and alcohol use problems (Simons and Gaher 2005). Furthemore, consistent with theoretical models (e.g., Brown et al. 2005), lower levels of distress tolerance were associated with greater expectations of negative consequences and negative reinforcement due to smoking. Interestingly, there also were significant associations with the expectation of appetite control. These findings suggest that greater difficulties tolerating and regulating emotions may be uniquely related to smoking as a self-regulation strategy for negatively evaluated emotions as well as other physical functions (e.g., appetite).
Furthermore, as expected, the total score as well as all subscale scores were significantly (inversely) associated with negative affect, such that lower levels of distress tolerance were associated with higher levels of negative affectivity. The Tolerance subscale also was significantly associated with positive affect; specifically, a greater ability to tolerate emotions was associated with higher levels of positive affect. These relations to negative and positive affectivity also are consistent with those observed by Simons and Gaher (2005).
Finally, whereas Simons and Gaher (2005) observed a significant sex-difference with respect to DTS scores in their initial investigation, suggesting that men report greater levels of perceived distress tolerance after controlling for negative affectivity, no significant zero-order associations were observed between sex and DTS or its subscales in the current investigation (see Table 3).
One overarching conclusion based on the observed pattern of associations between the DTS total and subscale scores and smoking and affective variables is of a discriminant matrix of relations. Such findings are largely consistent with theorizing underlying the observed hierarchical and multidimensional model of the DTS and perceived tolerance of affective distress (Simons and Gaher 2005). Specifically, DTS total scores were not associated universally with all smoking and affective variables; rather, specific DTS subscale scores were associated with specific dependent variables. One notable exception to this discriminant pattern of convergent and discriminant associations was observed with respect to negative affectivity. Unlike the other studied smoking variables and positive affectivity, DTS total and all subscale scores were uniformly related to negative affectivity; though the Tolerance subscale scores were relatively less strongly associated with negative affectivity scores relative to the DTS total and other subscale scores. Future study of the unique pattern of association(s) between distress tolerance and its putative facets, as indxed by the DTS, and negative affectivity may be key to better understanding the role(s) of distress tolerance in smoking cessation processes.
The present study has a number of limitations and related future directions that warrant comment. First, the studied participants were not a representative sample of cigarette smokers. Moreover, though the sample size was sufficient (Hutcheson and Sofroniou 1999), it is somewhat small for factor analytic work. Future research could address these concerns by evaluating a larger representative sample of smokers and thereby evaluating the replicability and stability of the observed factor analytic findings. Second, the present study utilized a cross-sectional design. Thus, directionality of observed associations between DTS scores and criterion variables as well as the longitudinal stability of distress tolerance as indexed by the DTS, among smokers were not evaluated. Third, it is possible that distress tolerance is affected by certain demographic factors such as sex and age. The current sample was too limited in overall size to permit a formal and comprehensive test of such issues. Future work may usefully explore whether demographic factors affect the structure of distress tolerance, as measured by the DTS or whether the DTS demonstrates factorial homogeneity across these subgroups of smokers.
Footnotes
The current investigation represents novel information and has not been previously presented. The authors declare that they have no competing interests for this research project.
Suggested cutoff values for fit indices have varied throughout the years in the interpretation of structural equation model fit. Many fit indices have shown sensitivity to aspects of data including sample size and model parsimony (Hooper et al. 2008). In addition, interpretation of model fit is sometimes hindered by stringent criteria cutoff values (Hooper et al. 2008). To aid in the interpretation of the currently proposed goodness-of-fit was evaluated using both conservative (Brown 2006; Hooper et al. 2008; Hu and Bentler 1999; Kline 2005) and liberal (Anderson and Gerbing 1984; Bentler 1992; Hu and Bentler 1999; MacCallum et al. 1996; Marsh et al. 1988; Wheaton et al. 1977) index cutoffs to better facilitate interpretation of model fit in the event values fall outside the conservative range. Goodness-of-fit was specifically evaluated using the following indices: χ2 (p > .05) (Hu and Bentler 1999), Normed χ2 (NC; Wheaton et al. 1977) of 2.0 (Tabachnick and Fidell 2007) to 5.0 (Wheaton et al. 1977), Goodness-of-Fit Index (GFI; Jöreskog and Sörbom 1981) > .95 (Miles and Shevlin 1998) to .85 (Anderson and Gerbing 1984), Adjusted Goodness-of-Fit Index > .95 (Miles and Shevlin 1998) to .8 (Marsh et al. 1988) (AGFI; Jöreskog and Sörbom 1981); Standardized Root Mean Square Residual (Hu and Bentler 1995) < .05 (Byrne 1998) to .1 (Marsh et al. 1988), Root Mean Square Error of Approximation (RMSEA; Steiger 1990) < .06 (Hu and Bentler 1999) to .08 (MaCallum et al. 1996), the Comparative Fit Index (CFI; Bentler 1990) > .95 (Hu and Bentler 1999) to 90 (Bentler 1992), and the Tucker-Lewis Index (TLI; Bentler and Bonett 1980) > .95 (Hu and Bentler 1999) to .90 (Bentler and Bonett 1980).
Contributor Information
Teresa M. Leyro, Department of Psychology, University of Vermont, John Dewey Hall, 2 Colchester Avenue, Burlington VT 05405-0134, USA, teresa.leyro@uvm.edu
Amit Bernstein, Department of Psychology, University of Haifa, Mount Carmel, Haifa, Israel 31905, abernstein@psy.haifa.ac.il.
Anka A. Vujanovic, National Center for PTSD, Behavioral Science Division, VA Boston Healthcare System, Boston, MA, USA, anka.vujanovic@gmail.com Division of Psychiatry, Boston University School of Medicine, 150 South Huntington Avenue (116B-2), Boston, MA 02130, USA.
Alison C. McLeish, Department of Psychology, University of Cincinnati, 5130A Edwards I, P.O. Box 2120376, Cincinnati, OH 45221-0376, USA, alison.mcleish@uc.edu
Michael J. Zvolensky, Anxiety and Health Research Laboratory, Department of Psychology, University of Vermont, John Dewey Hall, 2 Colchester Avenue, Burlington, VT 05405-0134, USA, michael.zvolensky@uvm.edu
References
- Anderson JC, Gerbing DW. The effect of sampling error on convergence, improper solutions, and goodness-of-fit indices for maximum likelihood confirmatory factor analysis. Psychometrika. 1984;49:155–173. [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT- Alcohol Use Disorders Identification test: Guidelines for use in primary health care. Geneva: World Health Organization; 1992. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Bentler PM. EQS structural equations program manual. Los Angelas, CA: BMDP Statistical Software; 1992. [Google Scholar]
- Bernstein A, Vujanovic AA, Leyro TM, Zvolensky MJ. Distress tolerance: Research synthesis and future directions. In: Bernstein A, Zvolensky MJ, Vujanovic AA, editors. Distress tolerance. New York: Guilford; 2010. [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Brandon TH, Baker TB. The smoking consequences questionnaire: the subjective expected utility of smoking in college students. Psychological Assessment. 1991;3:484–491. [Google Scholar]
- Brandon TH, Herzog TA, Juliano LM, Irvin JE, Lazev AB, Simmons VN. Pretreatment task persistence predicts smoking cessation outcome. Journal of Abnormal Psychology. 2003;112:448–456. doi: 10.1037/0021-843x.112.3.448. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford; 2006. [Google Scholar]
- Brown R, Lejuez C, Kahler C, Strong D. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, Zvolensky MJ. Distress tolerance and early smoking lapse (theory and clinical implications) Clinical Psychology Review. 2005;25:713–733. doi: 10.1016/j.cpr.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Palm KM, Strong DR, Lejuez CW, Kahler CW, Zvolensky MJ, et al. Distress tolerance treatment for early-lapse smokers: rationale, program description, and preliminary findings. Behavior Modification. 2008;32:302–332. doi: 10.1177/0145445507309024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Beverly Hills: Sage; 1993. [Google Scholar]
- Buckley TC, Kamholz BW, Mozley SL, Gulliver SB, Holohan DR, Helstrom AW, et al. A psychometric evaluation of the Smoking Consequences Questionnaire-Adult in smokers with psychiatric conditions. Nicotine & Tobacco Research. 2005;7:739–745. doi: 10.1080/14622200500259788. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modelling with LISREL, PRELIS and SIMPLIS: Basic concepts, applications and programming. Mahwah: Erlbaum; 1998. [Google Scholar]
- Cocores J. Nicotine dependence: diagnosis and treatment. The Psychiatric Clinics of North America. 1993;16:49–60. PMid:8456047. [PubMed] [Google Scholar]
- Downey KK, Kilbey MM. Relationship between nicotine and alcohol expectancies and substance dependence. Experimental and Clinical Psychopharmacology. 1995;3:174–182. [Google Scholar]
- Fagerstrom KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3:235–241. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV patient edition (SCID-N/ P, Version 2.0) New York: Biometrics Research Department; 1994. [Google Scholar]
- Hajek P. Individual differences in difficulty quitting smoking. British Journal of Addiction. 1991;86:555–558. doi: 10.1111/j.1360-0443.1991.tb01807.x. [DOI] [PubMed] [Google Scholar]
- Hajek P, Belcher M, Stapleton J. Breath-holding endurance as a predictor of success in smoking cessation. Addictive Behaviors. 1987;12:285–288. doi: 10.1016/0306-4603(87)90041-4. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hooper D, Coughlan J, Mullen M. Structural equation modeling: guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6:53–60. http://www.ejbrm.com/ vol6/v6-i1/Hooperetal.pdf. [Google Scholar]
- Hu L-T, Bentler P. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling. Concepts, issues, and applications. London: Sage; 1995. pp. 76–99. [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indices in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hutcheson G, Sofroniou N. The multivariate social scientist: Introductory statistics using generalized linear models. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Thousand Oaks: Sage; 1996. [Google Scholar]
- Jöreskog KG, Sörbom D. Lisrel user’s guide. Version V. Chicago: International Educational Services; 1981. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8.80 for Windows [Computer Software] Lincolnwood, IL: Scientific Software International, Inc; 2006. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford; 2005. [Google Scholar]
- Leyro TM, Zvolensky MJ, Vujanovic AA, Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: replication and extension. Nicotine & Tobacco Research. 2008;10:985–994. doi: 10.1080/14622200802097555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010 doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- Marsh HW, Balla JR, McDonald RP. Goodness of fit indexes in confirmatory factor analysis: the effect of sample size. Psychological Bulletin. 1988;103:391–410. [Google Scholar]
- McIntosh C. Rethinking fit assessment in structural equation modelling: a commentary and elaboration on Barrett (2007) Personality and Individual Differences. 2006;42:859–867. [Google Scholar]
- Miles J, Shevlin M. Effects of sample size, model specification and factor loadings on the GFI in confirmatory factor analysis. Personality and Individual Differences. 1998;25:85–90. [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- Parrott AC. Does cigarette smoking cause stress? The American Psychologist. 1999;54:817–820. doi: 10.1037//0003-066x.54.10.817. [DOI] [PubMed] [Google Scholar]
- Payne TJ, Smith PO, McCracken LM, McSherry WC, Antony MM. Assessing nicotine dependence: a comparison of the Fagerstrom Tolerance Questionnaire (FTQ) with the Fagerstrom Test for Nicotine Dependence (FTND) in a clinical sample. Addictive Behaviors. 1994;19:307–317. doi: 10.1016/0306-4603(94)90032-9. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 1994;19:33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Richards JM, Daughters SB, Bornovalova MA, Brown RA, Lejuez CW. Substance use disorders. In: Zvolensky M, Bernstien A, Vujanovic A, editors. Distress tolerance. New York: Guilford; 2010. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Simons J, Gaher R. The Distress Tolerance Scale: development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- State of Vermont Department of Health. 2007 Vermont population estimates. 2007 Retrieved December 17, 2009, from http://healthvermont.gov/research/2007pop/documents/RACE-NOTE07.PDF.
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. New York: Allyn and Bacon; 2007. [Google Scholar]
- Watson D. Mood and temperament. New York: Guilford; 2000. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- West RJ, Hajek P, Belcher M. Severity of withdrawal symptoms as a predictor of outcome of an attempt to quit smoking. Psychological Medicine. 1989;19:981–985. doi: 10.1017/s0033291700005705. [DOI] [PubMed] [Google Scholar]
- Wheaton B, Muthen B, Alwin DF, Summers GF. Assessing Reliability and Stability in Panel Models. In: Heise DR, editor. Sociological methodology. San Francisco: Jossey-Bass; 1977. pp. 84–136. [Google Scholar]
- Zvolensky MJ, Schmidt NB, Stewart SH. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;10:29–51. [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: an initial examination. Addictive Behaviors. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Vujanovic AA. Distress tolerance. New York: Guilford; 2010. [Google Scholar]