Abstract
While epidemiologic studies suggest that soy intake early in life may reduce breast cancer risk, there are also concerns that exposure to soy isoflavones during childhood may alter pubertal development and hormonal profiles. Here, we assessed the effect of a high-soy diet on pubertal breast development, sex hormones, and growth in a nonhuman primate model. Pubertal female cynomolgus monkeys were randomized to receive a diet modeled on a typical North American diet with one of two protein sources for ~4.5 years: i) casein/lactalbumin (CL, n=12, as control) or ii) soy protein isolate with a human equivalent dose of 120 mg/day isoflavones (SOY, n=17), which is comparable to approximately four servings of soy foods. Pubertal exposure to the SOY diet did not alter onset of menarche, indicators of growth and pubertal progression, or circulating estradiol and progesterone concentrations. Greater endometrial area was seen in the SOY group on the first of 4 postmenarchal ultrasound measurements (P<0.05). There was a subtle effect of diet on breast differentiation whereby the SOY group showed higher numbers of differentiated large-sized lobular units and a lower proportion with immature ducts following menarche (P<0.05). Numbers of small lobules and terminal end buds and mammary epithelial cell proliferation did not differ by diet. Expression of progesterone receptor was lower in immature lobules of soy-fed animals (P<0.05). Our findings suggest that consumption of soy starting before menarche may result in modest effects consistent with a more differentiated breast phenotype in adulthood.
Keywords: puberty, breast cancer, soy isoflavones, estrogen, macaque
Introduction
Environmental exposures to hormonally active compounds during critical windows of development can influence breast cancer risk later in life (1). Soy protein contains a variety of bioactive compounds including isoflavones (IF), which are structurally similar to estrogen, bind to estrogen receptors (ERs), and elicit both estrogenic and anti-estrogenic responses depending on dose, tissue location, and estrogen context (2, 3). Soy intake has been widely studied as a potential dietary determinant of breast cancer risk, both as a natural chemopreventive approach as well as potential risk factor. Recent evidence suggests that timing of exposure may be critical to determine the magnitude and direction of soy effects. Several epidemiologic studies indicate that lower risk of breast cancer is observed when soy is consumed throughout life or before/during key periods of breast development (4, 5). These observations parallel those in rodents (6), supporting the idea that early soy exposure may alter breast phenotype later in life.
Puberty is a developmental process that involves a complex series of interactions between growth factors and sex hormones. Age at menarche, a key milestone of puberty, is a consistent predictor of later breast cancer risk in human observational studies, potentially due to hormonal and developmental factors (7, 8). In females, puberty is a key period for breast morphogenesis and differentiation. Ovarian hormones drive elongation and branching of rudimentary ducts and development of terminal end buds (TEBs) (9), which subsequently develop into lobuloalveolar structures. The lobules further undergo gradual maturation wherein the number of terminal ductular and alveolar units per lobule increases, resulting in a concomitantly larger size (10). The degree of lobular differentiation has been inversely related to cancer risk (11, 12), suggesting that modulation of breast developmental patterns may influence later life susceptibility to cancer. We hypothesized that pubertal exposure to soy would enhance mammary gland differentiation, potentially leading to a lower risk breast phenotype.
Previous studies have primarily used rodent models to assess environmental influences on breast development. While these models have contributed greatly to our understanding of molecular signaling in the breast, there are important developmental and physiologic differences between rodents and primates. Most notably, pubertal breast development in rodents is mainly composed of ductal growth with scant lobular differentiation prior to pregnancy (13). Macaque monkeys serve as a valuable animal model for women’s health due in part to their highly similar reproductive physiology, pubertal stages of development, and patterns of ductal and lobular morphogenesis in the breast (14, 15). Cynomolgus macaques also exhibit a nonseasonal 28-30 day menstrual cycle with ovarian hormone and tissue responses comparable to humans (16). The primary aim of the current study was to assess the effect of dietary soy exposure on breast development in cynomolgus macaques across the pubertal transition.
Materials and Methods
Animals and Diet Treatment
Thirty female cynomolgus macaques (Macaca fascicularis) were imported from the Institut Pertanian Bogor (Bogor, Indonesia) at approximately 1.5 years of age, as confirmed by dentition. Female macaques typically reach puberty at the age of 2-3 years. Animals were randomized to social groups of 4-5 on the basis of body weight to receive one of two diets for ~4.5 years: (i) a control diet with casein and lactalbumin as the protein source (CL, n=12) or (ii) a diet with isolated soy protein containing IF (provided by Solae, LLC) (SOY, n=18) with the human equivalent of 120 mg/day of IF (in aglycone equivalents), which is ~3-5 times higher than the typical consumption in Asian population (17) (Supplementary Table S1). Macronutrient composition of the diets approximated a typical North American diet with 35% calories from fat. Breast biopsies were taken every six months starting at one month into treatment, with a total of 9 biopsies per animal spanning the period of pubertal breast development. Other measures at the time of biopsy included serum sex hormones, uterine size by ultrasound, bone mineral measures by Dual Energy X-Ray Absorptiometry (DEXA) scans, nipple length, trunk length, and body weight. Animals were swabbed daily for vaginal bleeding throughout the study, and menarche was defined as the initiation of regular monthly vaginal bleeding (16, 18). Following menarche, menstrual cycle stage of the animals (i.e., follicular or luteal) was determined retrospectively based on their menstrual bleeding calendar. Two animals died during the study due to causes unrelated to the dietary treatment, one at the beginning of the study (SOY) and one approaching year 4 of the study (CL); this latter animal did not have data from the final biopsy.
All procedures involving animals were performed at the Wake Forest School of Medicine, which is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care (AAALAC). Procedures were conducted in compliance with state and federal laws and standards of the US Department of Health and Human Services and approved by the Wake Forest University Animal Care and Use Committee.
Serum Isoflavonoids
Serum concentrations of the main isoflavones (genistein, daidzein) and isoflavone metabolite (equol) were measured using liquid chromatography electrospray ionization mass spectrometry at the laboratory of Dr. Adrian Franke (University of Hawaii Cancer Center), as described elsewhere (19). The measurements were performed on 18-hour fasted serum samples collected at the time of biopsy.
Dual Energy X-Ray Absorptiometry Scans
Whole body DEXA scanning was performed every six months using a Norland XR-46 Bone Densitometer (Norland Corp, Fort Atkinson, WI). Utilizing Norland Host Software, we generated measurements for whole body bone mineral content (BMC, in grams) and lumbar spine (lumbar vertebrae 2-4) bone mineral density (BMD, in grams per cm2) (20). The coefficients of variation were 1.7% for BMC and 2.1% for BMD.
Somatometry
Trunk length, nipple length, endometrial thickness, and uterine and endometrial area were measured as indicators of growth and reproductive maturation. Trunk length was measured from the suprasternal notch to symphysis pubis using a Vernier Caliper (Fischer Scientific, Pittsburgh, PA). Nipple length was also measured by caliper. Ultrasound of the uterus was performed utilizing portable ultrasound devices equipped with 5.0-13 MHz linear transducers (SonoSite, Bothell, WA). Measurements of uterine area, endometrial area, and endometrial thickness were manually performed on the digitized images using NIH ImageJ (version 1.45q, available at rsbweb.nih.gov/ij/). Post-menarche analysis was adjusted for normal cyclical variation in endometrial thickness across the menstrual cycle, using menstrual cycle days 1-9 as the period of anticipated thinnest endometrium, with day 1 counted as the first day of menstrual bleeding (21).
Hormone Assays
Serum concentrations of estradiol (E2) and progesterone (P4) were measured by radioimmunoassay (RIA) using commercially available kits and protocols from Siemens Healthcare Diagnostics (Los Angeles, CA). Prior to menarche, serum hormone concentrations were measured in blood samples that were collected at the time of breast biopsy. One year after menarche, blood was collected at three consecutive menstrual cycles, twice during each menstrual cycle (at day 9-13 for E2 and day 18-25 for P4). The RIAs were performed at the Biomarkers Core Laboratory of the Yerkes National Primate Research Center of Emory University (Atlanta, GA) using standard procedures. The normal assay ranges were 2.85-546.00 pg/ml for E2 and 0.10-40.00 ng/ml for P4.
Breast Biopsy Collection
Serial breast biopsies were collected using methods described previously (22). The biopsy samples were wedge-shaped, ~200 mg in weight, 2-3 cm x 1 cm from nipple to the edge of the gland. Each sample was divided; one half was frozen for biomolecular work, and the other half was placed on a fiberglass screen to prevent distortion, fixed at 4°C in 4% paraformaldehyde for 24 hours, and then transferred to 70% ethanol. Fixed tissues were then processed for whole mount staining, histology, and immunohistochemical staining. Hematoxylin and eosin (H&E)-stained slides were evaluated for developmental morphology and pathologic lesions blinded to experimental treatment by a pathologist (CJW) in consultation with a board-certified veterinary pathologist (JMC).
Whole Mount Mammary Gland Staining
Whole mounts were stained using 0.27% Toluidine Blue as previously described (15, 23). Whole mounts were photographed in toto, and the digital images were used for morphologic measures.
Mammary Gland Morphometry
For measurement of mammary gland epithelial area, H&E-stained slides were digitized (Infinity 3 digital camera, Lumenera, Ottawa, Canada; Adobe Photoshop version 6.0, San Jose, CA) and measured with methods described previously (23) and modified as follows for developmental structures. Breast epithelium was subdivided into lobuloalveolar and ductal compartments. Lobules were categorized as immature (type 1) or mature (type 2 and 3) (10). Ducts were categorized as either immature (multiple luminal cell layers, columnar cell morphology, rounded myoepithelial cells, with/without a small lumen), transitional (multiple luminal cell layers with less stratification, more elongated morphology, increased lumen size, flattened myoepithelial cell borders), or mature (single luminal cell layer, cuboidal morphology, flattened myoepithelial cells). We did not histologically differentiate between TEBs and immature ducts on H&E images due to their overlapping features (15). Total epithelial area of the biopsy section and area of each lobule and ductal type were determined by manually tracing the structures using a computer-assisted technique with Image Pro-Plus Software (Media Cybernetics Inc., Bethesda, MD). Epithelial area was expressed as a percentage of the total area examined.
For whole mounts, mammary glandular structures were categorized as TEBs (tear drop-shaped, >100 μm in width), small-sized lobules (area <100,000 μm2), or large-sized lobules (area >100,000 μm2), and quantified across the entire tissue using NIH ImageJ. Structural counts were expressed as number of TEBs or lobules per cm2.
Quantitative Gene Expression
Expression of mRNA for markers of mammary gland differentiation (casein alpha s1, CSN1S1; mucin-1, MUC1; E74-like factor 5, ELF5; signal transducer and activator of transcription factor 5A and 5B, STAT5A and STAT5B), proliferation (MKI67), and ER activity (progesterone receptor, PGR) was measured using quantitative real-time reverse-transcriptase PCR (qRT-PCR) based on standard methods described elsewhere (24). Amplification was performed using the ABI PRISM® 7500 Fast Sequence Detection System (Applied Biosystems, Foster City, CA). Human or macaque-specific Taqman primer-probe assays were used to quantify target transcripts (Supplementary Table S2) with normalization to cynomolgus macaque-specific primer-probe sets of housekeeping genes GAPDH and ACTB. Relative gene expression was determined using the ΔCt method calculated by ABI Relative Quantification 7500 Software v2.0.1 (Applied Biosystems, Foster City, CA). Stock mammary tissues and tumor samples were run in triplicate on each plate as external calibrators.
Immunohistochemistry
We used immunohistochemistry to assess protein expression and localization of markers for proliferation (Ki67) and estrogen activity (PGR) in mammary epithelial cells as previously described (22). Monoclonal antibodies used were anti-Ki67 (Ki67/MIB1; Dako, Carpinteria, CA) and anti-PGR (NCL-PGR; Novocastra Labs, Newcastle-upon-Tyne, UK), both with 1:100 dilution. Cell staining was quantified by a computer-assisted technique with grid filter where positively stained cells were scored based on staining intensity (+1, +2, or +3) to obtain a semi-quantitative measurement of staining intensity and distribution by H-score calculation (22).
Data Analyses
Data that were not normally distributed were transformed by logarithmic or square-root conversions to improve normality of the residuals. Data were back transformed to original scale for presentation of results; values are presented as least square means (LSM) + standard error of the mean (SEM) or LSM (LSM-SEM, LSM+SEM) when standard errors were asymmetric. We used JMP (version 10.0.0, SAS Institute; Cary, NC) to fit a mixed model ANOVA with a random animal effect to model diet and time effects adjusted for body weight and menstrual cycle stage (post-menarche) to estimate and compare differences in serum isoflavonoid levels, hormone levels, somatometric measures, mammary gland differentiation, mammary epithelial cell proliferation, and ER activity markers in the breast, between SOY and CL groups over time. We also used SAS (version 9.2, SAS Institute; Cary, NC) to fit a mixed effects logistic regression with a random animal effect to model if a particular duct or lobule type was found at a given time point, and if there were differences by diet group, adjusted for body weight and menstrual cycle stage (post-menarche) (25). Menarche data were analyzed using a survival model and logistic regression to model whether onset occurred by 12 months of treatment adjusted for body weight. All outcomes were compared between monkeys of similar development stage across the pubertal transition, and the analyses were done separately for pre- and post-menarche. We also compared pre-vs. post-menarche. Multiple pairwise comparisons were done with Tukey Honestly Significant Difference (HSD) Test. Correlation between differentiation marker expression and large-sized lobule count was analyzed using a pairwise test for the significance of the Pearson Product-moment correlation coefficient.
Results
Serum Isoflavonoid Concentrations
Total serum isoflavonoid concentrations were significantly higher in SOY group compared to CL (P<0.0001). The mean concentration in SOY was 119 nmol/L (107.9, 131.2nmol/L) after overnight fasting, compared to 22 nmol/L (19.8, 25.2 nmol/L) in CL. Equol was the predominant circulating isoflavonoid, accounting for 70% of total isoflavonoids. This finding was similar to our previous work (22).
Pubertal Development
Body weight, trunk length, BMC, and BMD increased across the treatment period (time effect P<0.0001) but did not differ between diet groups. Mean body weights were 1.76 + 0.08 kg and 1.70 + 0.07 kg prior to dietary treatment and 3.51 + 0.17 kg and 3.79 + 0.15 kg at the end of the study in the CL and SOY groups, respectively. Trunk length, BMC and BMD were associated with body weight (P<0.0001). While trunk length increased across both menarchal stages (data not shown), BMC and BMD only significantly increased after menarche (Supplementary Figure S3).
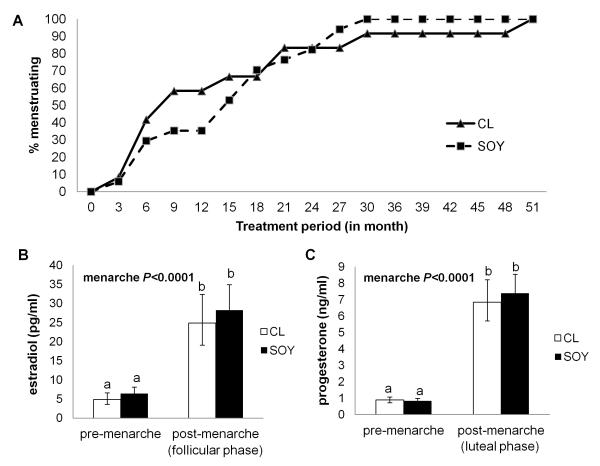
Timing of menarche varied widely across individuals with no effect of diet (Figure 1A). By month 12 of treatment, CL showed a nonsignificantly higher proportion of menstruating animals than SOY, and the onset was marginally associated with body weight (P=0.07). By month 18, ~70% of animals in each diet group had begun cycling.
Figure 1.
Onset of menarche and circulating reproductive hormones in cynomolgus macaques fed a high-soy (SOY) or casein-lactalbumin (CL)-based diet. A: The proportion of post-menarchal monkeys across the study period did not differ by diet. B,C: Serum concentrations of estradiol (B) and progesterone (C) were higher after menarche, with no dietary effect. Values are LSM for n=11-17 monkeys/group (error bars=SEM). The significant main effect is indicated in each panel. a,b Labeled means without a common letter differ (P<0.0005) by LSM Tukey’s HSD test. Body weight was included in the model as a covariate.
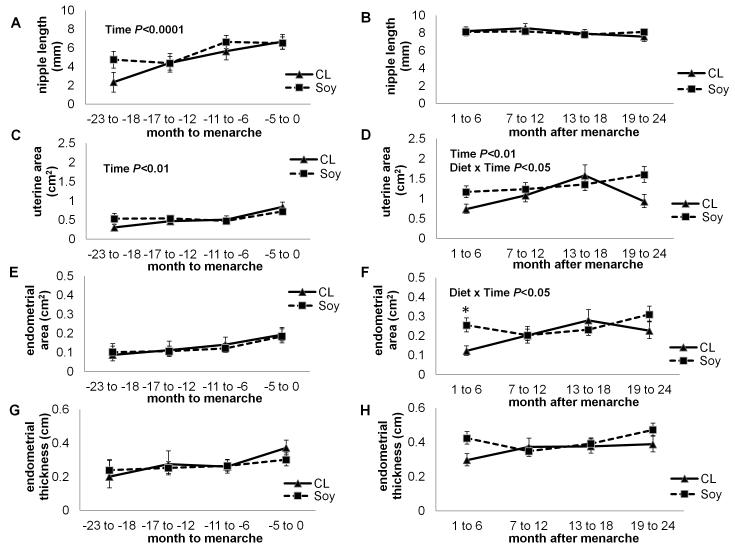
Hormone status (Figure 1B,C) and markers for pubertal progression (Figure 2) were evaluated. Nipple length increased up to menarche (P<0.0001), which was partially driven by the change in body weight (P<0.0001). Uterine area also increased across pre-menarche (P<0.01) and was associated with body weight (P<0.01), whereas endometrial area (P=0.07) and thickness (P=0.1) did not significantly change. Importantly, there was no diet effect observed for any of these markers before menarche. Serum hormone concentrations were elevated after menarche (P<0.0001 in both diet groups) but remained unaffected by diet. Uterine area increased across post-menarche (P<0.01) with a significant diet x time interaction (P<0.05), and showed an association with body weight (P<0.05). Endometrial area and thickness were primarily determined by menstrual cycle day (P<0.01 and P=0.05, respectively). There was no diet effect observed on endometrial outcomes when covaried with menstrual cycle day. We found a significant diet x time interaction on endometrial area (P<0.05), with greater area in the SOY group during 1-6 months after menarche (P<0.05).
Figure 2.
Measurement of puberty markers before (A,C,E,G) and after (B,D,F,H) menarche in cynomolgus macaques fed a soy (SOY) or casein-lactalbumin (CL) diet. A-B: Nipple length showed a significant increase prior to menarche independent of diet. C-D: Uterine area increased over time with no main effect of diet. E-H: Endometrial area (E,F) and thickness (G,H) did not significantly change over time albeit an increasing pattern. Values are LSM for n=4-12 (CL) or 5-17 (SOY), error bars=SEM. The significant main effect and interaction are indicated in each panel. Asterisk (*) indicates P<0.05 with LSM Tukey’s HSD test for SOY compared to CL. Body weight was included in the model as a covariate except in nipple length analysis. Post-menarchal analysis also included menstrual cycle day (i.e. day 1-9 or after) in the model as a covariate.
Mammary Gland Differentiation
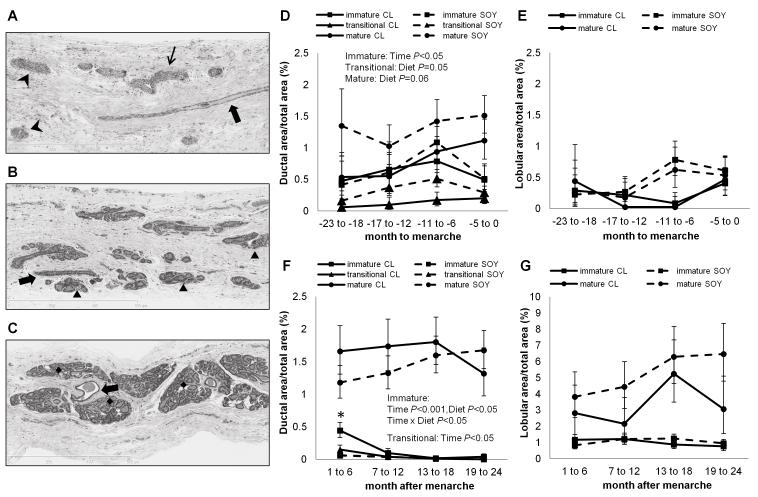
Histological assessment revealed no significant abnormalities in mammary gland morphology throughout the study. Two animals (SOY) had a minimal lymphocytic perilobular infiltrate at one biopsy timepoint. A lobule in one animal (CL) contained abundant globular hypereosinophilic secretory material (eosinophilic secretory change), which was found only on the last biopsy.
Mammary epithelial features showed normal patterns of pubertal breast development (Figure 3A-C). Pre-menarchal breast contained predominantly ductal structures, with marginally greater areas of transitional and mature ducts in SOY relative to CL (P=0.05 and P=0.06, respectively) (Figure 3D). Following menarche, the relative area of immature and transitional ducts decreased (P<0.001), whereas that of lobules increased compared to pre-menarche (P<0.0001). After menarche (Figure 3F), there was a main effect of diet on immature ducts (P<0.05) with a significant diet x time interaction (P<0.05) whereby the area was greater in CL compared to SOY at 1-6 months post-menarche (P<0.01). In mixed model logistic regression, the proportion of post-menarchal monkeys that had immature ducts present in the breast was higher in CL relative to SOY (diet effect P<0.05). There was no diet effect on lobular area across the pubertal transition (Figure 3E, G). Histologically, total epithelial area reached 6% (4.8%, 8.0%) in CL and 10% (8.5%, 11.9%) in SOY by two years post-menarche. Similar to other pubertal measures, body weight was associated with the areas of immature ducts, transitional ducts, immature lobules, and mature lobules (P<0.05 for all).
Figure 3.
Pubertal mammary gland development of cynomolgus macaque fed a high-soy (SOY) or casein-lactalbumin (CL)-based diet. A-C: Pre-menarchal breast (A) composed of mostly ductal structures (immature, transitional, and mature types indicated as arrowheads, thin arrows, and thick arrows, respectively). Immature lobules (▲) were abundant approaching menarche (B) while mature lobules (◆) predominated post-menarche (C) (H&E staining, 10X magnification). D: Immature ducts were the only structures that showed a significant rise prior to menarche. E: There was no significant change in lobular area across pre-menarche. F: The proportion of immature and transitional ducts significantly decreased following menarche. G: The post-menarche breast contained primarily mature lobules. Values are LSM for n=4-12 (CL) or 5-17 (SOY), error bars=SEM. The significant main effects and interactions are indicated in each panel. Asterisk (*) indicates s difference between SOY and CL (P<0.01) by LSM Tukey’s HSD test. Body weight and menstrual cycle stage (post-menarche) were included in the model as covariates.
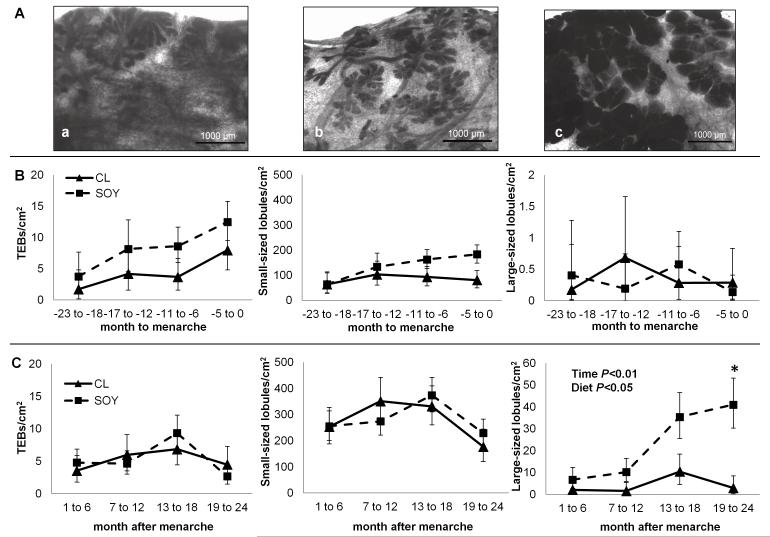
There was no diet effect on the numbers of TEBs and small-sized lobules at either pre- or post-menarche (Figure 4). Regardless of diet, the number of small-sized lobules after menarche was higher than that before menarche (P<0.0001), and there was an increasing pattern over time with a slight decrease by 1.5-2.0 years after menarche. The number of large-sized lobules significantly increased after menarche (time effect P<0.01), and there was an overall diet effect whereby the number was greater in SOY at this stage (diet effect P<0.05). This effect was mainly driven by whether or not animals had any large lobules present in the breast (diet effect P<0.01). Further, the difference was most evident at 1.5-2.0 years after menarche when the SOY group showed about 5-fold higher number of large-sized lobules compared to CL (P<0.05).
Figure 4.
Quantification of TEBs and lobular structures in the breast of cynomolgus macaques fed a high-soy (SOY) or casein-lactalbumin (CL) diet across the pubertal transition. A: Whole mount images of the breast (toluidine blue staining) predominated by TEBs (a), small-sized lobule (b), and large-sized lobule (c). B: Before menarche, the lobular number did not differ between diet groups. C: After menarche, the amount of large-sized lobules significantly increased and was higher in the SOY group. Values are LSM for n=4-12 (CL) or 5-17 (SOY), error bars=SEM. The significant main effects are indicated in each panel. Asterisk (*) indicates a difference between SOY and CL (P<0.05) by LSM Tukey’s HSD test. Body weight and menstrual cycle stage (post-menarche) were included in the model as covariates.
We did not find a diet effect on gene expression of differentiation markers before or after menarche (Table 1). There was a significant time effect on mRNA expression for CSN1S1 (P<0.0001), ELF5 (P<0.0001), MUC1 (P<0.01), STAT5A (P<0.0001), and STAT5B (P<0.001). Post-menarchal increases in CSN1S1 and ELF5 were seen in both SOY (P<0.001) and CL (P<0.01), while STAT5A and STAT5B increased only in SOY (P<0.01). The mRNA expression of all markers was positively correlated with the number of large-sized lobules (r=0.35, P<0.0001 for CSN1S1; r=0.37, P<0.0001 for ELF5; r=0.25, P<0.01 for MUC1; r=0.34, P<0.0001 for STAT5A; r=0.27, P<0.001 for STAT5B). When stratified by dietary groups, correlations of CSN1S1 and ELF5 with large-sized lobule number were stronger in the SOY group, and correlations of MUC1, STAT5A and STAT5B with number of large-sized lobule were only significant in the SOY group. While body weight was significantly associated with lobule count (P<0.0005 for all lobule types), it was not associated with mRNA expression of differentiation markers.
Table 1.
Gene expression of differentiation markers in the mammary gland of female cynomolgus macaques fed a high- soy (SOY) or casein/lactalbumin (CL)-based diet, as measured by qRT-PCRa.
| Gene | Stage Effect | Diet Effect |
Diet | Pubertal Stage |
Correlation with lobular maturation |
|
|---|---|---|---|---|---|---|
| Pre-menarche | Post-menarche | |||||
| CSN1S1 | P<0.0001 | P=0.73 | CL | 1.00 (0.65, 1.53) | 5.23 (3.92, 6.99)(b) | r=0.36, P=0.004 |
| SOY | 1.11 (0.77, 1.59) | 6.07 (4.75, 7.76)(c) | r=0.35, P=0.0003 | |||
| ELF5 | P<0.0001 | P=0.22 | CL | 1.00 (0.74, 1.34) | 2.89 (2.39, 3.49)(b) | r=0.36, P=0.004 |
| SOY | 1.16 (0.90, 1.49) | 4.51 (3.84, 5.31)(c) | r=0.37, P=0.0001 | |||
| MUC1 | P=0.01 | P=0.63 | CL | 1.00 (0.60, 1.67) | 2.12 (1.40, 3.21) | r=0.23, P=0.07 |
| SOY | 0.75 (0.49, 1.15) | 1.66 (1.17, 2.36) | r=0.29, P=0.004 | |||
| STAT5A | P=0.002 | P=0.61 | CL | 1.00 (0.80, 1.24) | 1.44 (1.26, 1.66) | r=0.19, P=0.13 |
| SOY | 0.92 (0.77, 1.11) | 1.87 (1.66, 2.10)(b) | r=0.39, P=<0.0001 | |||
| STAT5B | P=0.0003 | P=0.48 | CL | 1.00 (0.84, 1.19) | 1.44 (1.29, 1.60) | r=0.14, P=0.27 |
| SOY | 0.96 (0.83, 1.11) | 1.81 (1.65, 1.99)(b) | r=0.30, P=0.002 | |||
Values are presented as fold-change of LSM (LSM-SEM, LSM+SEM) from pre-menarchal CL group;n=3-11 (CL) and 4- 17 (SOY). Letter superscripts indicate difference from pre-menarchal relative expression with P<0.01
or P<0.001
by LSM Tukey’s HSD test.
Epithelial cell proliferation was not affected by soy treatment
Post-menarche MKI67 mRNA expression was 1.7 fold higher than pre-menarche levels (P<0.05) but there was no effect of diet (Supplementary Figure S4). Ki67 protein expression in the ductal and lobular structures of the mammary gland also did not differ by diet, with or without menstrual cycle stage in the model. Before menarche, proliferation of the epithelial cells in the mature lobule compartment marginally increased over time (P=0.06). After menarche, the proliferation in the immature lobule compartment showed a non-significant decreasing pattern with time (P=0.07). We found a significant association of body weight and Ki67 expression in mature ducts (P<0.05), immature lobules (P<0.005), and mature lobules (P<0.005). This effect was interpreted to reflect the onset of ovarian activity at puberty.
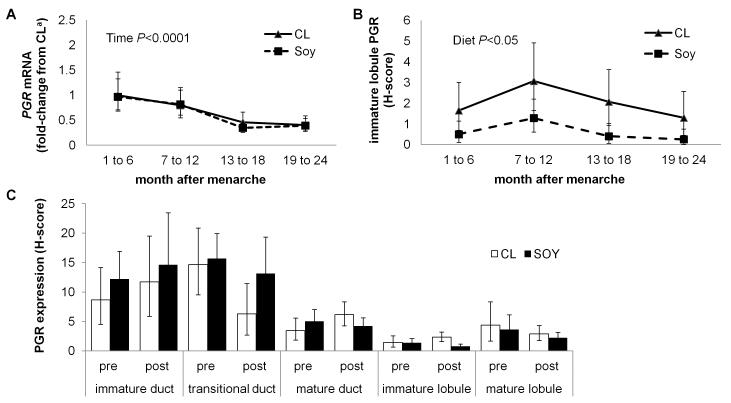
Estrogen activity in the breast decreased following menarche
There was a significant time effect on PGR expression across the pubertal transition (P<0.05). Regardless of diet group, PGR mRNA expression decreased after menarche (P<0.0001) (Figure 5A). While there was no diet effect on PGR mRNA, PGR protein expression in immature lobules post-menarche was lower in the SOY group (diet effect P<0.05) (Figure 5B). The effect was mainly driven by a higher proportion of monkeys in CL (vs. SOY) that showed positively stained cells in the immature lobule (diet effect P<0.05). Localized PGR protein expression did not differ by menarche status (Figure 5C). Body weight was inversely associated with PGR expression in mature ducts (P<0.05), immature lobules (P<0.01), and mature lobules (P<0.05).
Figure 5.
Progesterone receptor (PGR) expression as a marker for estrogen activity in the mammary tissue of cynomolgus macaques fed a high-soy (SOY) or casein-lactalbumin (CL) diet across the pubertal transition. A: mRNA expression of PGR decreased after menarche. B: Protein expression of PGR in the immature lobules of the breast was lower in the SOY group after menarche. C: Immunolocalization of PGR in the breast was similar before (pre) and after (post) menarche and not affected by diet. Values are presented as LSM and error bars=SEM. a Fold-change from CL at 1-6 months after menarche. The significant main effect is indicated in each panel. Body weight and cycle stage were included in the model as covariates.
Discussion
In this study, we showed that pubertal soy intake did not alter onset of menarche, pubertal progression, circulating reproductive hormones, or mammary epithelial cell proliferation. Soy had a modest effect on post-menarchal breast differentiation as indicated by a higher number of large-sized lobules and fewer immature ducts. The numbers of TEB and small-sized lobules, and differentiation markers, however, did not differ significantly by diet. There was lower expression of PGR in immature lobules of the soy-fed animals after menarche, possibly indicating altered estrogen response.
Puberty is the major period for mammary gland morphogenesis in females. In humans, hormonal and growth factor signals induce the rudimentary ductal tree to elongate, branch, and form lobuloalveolar structures (9). In rodents, pubertal breast development is mainly a process of rapid ductal growth; and prominent lobuloalveolar growth only occurs during pregnancy (13, 26). Here we document for the first time the pattern of mammary gland development across the pubertal transition in the macaque model, showing a high degree of interindividual variation and morphologic similarities to humans. The human TEB is the leading edge of mammary gland growth that gives rise to new branches and alveolar buds that further cluster around a terminal duct, forming nascent lobules (10). Similarly, pre-menarchal macaque breast consists mainly of TEBs, ductal structures, and immature lobules. After menarche, fewer TEBs are present and the majority of the epithelial compartment is in the form of large ducts and lobuloalveolar structures. A large increase in macaque mammary lobular differentiation occurs around the time of menarche and more markedly around one year after menarche, similar to that reported in humans (10). Lobules type 1 and 2 become the predominating unit of the adolescent macaque breast, which is consistent with our prior findings in the adult nulliparous macaque (27). Large-sized lobules, composed of more mature type 2 and type 3 lobules, also become more abundant and cover the majority of the epithelial compartment. The adult macaque breast is comprised of 80% or more stroma, similar to that in nonlactating women (9).
Mammary differentiation is a determinant of breast cancer risk. Less differentiated progenitor-type cells in the terminal ducts are likely founder cells for the majority of ductal carcinomas, the most common type of human breast cancer (12, 26). Mammary stem and progenitor cells are present throughout life and they are targets for transformation. The fate of these cells is mainly regulated during key developmental events such as puberty and pregnancy (28). In human epidemiologic studies, nulliparity is associated with higher breast cancer risk, potentially due to less differentiation of susceptible progenitor cell populations (29, 30, 31). Experimentally, in vitro and rodent studies indicate that less differentiated mammary cells and lobules are more proliferative, susceptible targets of carcinogens, and prone to neoplastic transformation (12, 32). Recent evidence also points to epigenetic changes during development that may lead to carry-over effects on cancer risk (33, 34).
Several observational studies have reported that adolescent soy intake may reduce breast cancer risk (35, 36, 37). Mechanisms for this effect are unclear, and these studies are generally limited by recall and “healthy person” biases. A prominent hypothesis is that early soy exposure may enhance breast differentiation, potentially through ER agonist effects. Parenteral administration of purified genistein resulted in fewer terminal ducts and increased numbers of alveolar buds in a carcinogen-treated mouse model (38). In rats, early life exposure to dietary soy protein (39) or high dose genistein (40) reduced the number of TEBs. Our studyextends these findings by evaluating developmental effects on the primate breast using soy/IF doses relevant to high dietary human exposures. Our findings suggest that soy intake before menarche may modestly enhance breast differentiation leading to a greater content of mature lobular structures following menarche. The markers CSN1S1, ELF5, STAT5, and MUC1 have important roles in lobular epithelial differentiation (33, 41, 42), and we previously reported that these genes were highly expressed in the mammary gland of pregnant and lactating cynomolgus macaques (43). Here we confirmed their use as differentiation markers in the macaque breast. The positive correlations between the expression of these markers and lobular differentiation were generally stronger in the soy-fed animals, further supporting the idea that soy may have a mild promotional effect on breast differentiation.
Soy IF share structural similarities to endogenous estrogens, bind to and transactivate ERs, and modulate proliferation of ER-responsive cells in vitro. This evidence has led to the idea that soy may alter ER-mediated activity in the developing breast through agonistic, antagonistic, or other hormone-disrupting effects. Here we found no evidence of strong ER agonist effects of a high-soy diet on systemic markers such as BMD or mammary gland markers such as epithelial cell proliferation. Interestingly, PGR immunolabeling in immature lobules was lower in soy-fed animals after menarche, suggesting that soy exposure may in some way diminish ER responsiveness in the type 1 lobule of adolescent breast. This was a modest effect specific to a single compartment, however, and it is unclear how such an alteration in ER activity may relate to differentiation patterns.
Although epidemiologic evidence generally suggests that soy intake may be beneficial for chemoprevention in some populations of women (4, 5), other rodent and cell culture studies have identified soy IF as potential endocrine-disrupting compounds due to ER or hormone modulating actions. Accordingly, there are concerns that exposure to soy during early life or critical stages of development may be potentially harmful for reproductive development (44). Our study showed that pubertal exposure to relatively high dietary levels of soy IF did not alter reproductive hormone concentrations or time to menarche in the macaque model. The IF dose used in the current study was ~60 times greater than those consumed by young girls in Germany (45) and the US (46); they found delayed breast development with higher daidzein intake (45) or urinary excretion (46). The total amount of circulating IF in our study doubled that in a study on Korean girls which reported an association of high soy IF with accelerated breast development (47). Equol was not assessed in those human studies. Here we also found no soy effect on nipple length or the prepubertal uterus. We did observe a transiently higher endometrial area in the SOY group at one time point, but no difference in uterine area or endometrial thickness; in the absence of a histologic assessment this finding is difficult to interpret. However, we have in several studies shown a lack of uterotrophic effects of dietary IF at up to 500 mg/woman/day equivalent in adult female macaques (24).
Other than the species differences, several factors may explain the neutral or less-profound effect of IF in our study compared to the previous findings in rodents (44). One factor could be the difference in timing of exposure; in-utero/neo-natal may be a more sensitive period for modulation such as via epigenetic modification (48). Another is the delivery method, wherein prior rodent studies often used parenteral administration as opposed to dietary dosing strategy that mimics soy consumption in humans. Many studies also utilized genistein as purified aglycone which may elicit a different effect than the genistein, daidzein, and glycitein mixture of soy IF consumed within a protein matrix. In addition, equol was the predominating isoflavonoid found in our study. Equol is a natural product of daidzein metabolism by gut flora with distinct biological properties from genistein and daidzein (49). Notably, only ~30% of adult non-Asian and non-vegetarian populations have the ability to produce this metabolite (50), and human equol production, when present, is generally less robust than in rodents and macaques. This phenotype could potentially account for the differences between our findings and other studies.
Our results suggest that exposure to a soy diet beginning at puberty does not have overt effects on pubertal growth and development. If anything, pubertal soy exposure may have a subtle effect in enhancing mammary gland differentiation following menarche. Future studies are needed to determine whether such a phenotype may influence breast cancer risk later in life.
Supplementary Material
Acknowledgments
The authors thank Jean Gardin, Hermina Borgerink, Lisa O’Donnell, Joseph Finley, Russell O’Donnell, and Matt Dwyer for their technical contributions.
Grant Support This work was supported by the NIH grant R01 AT00639 (NCCAM) (to JMC), P30 CA71789 (to AAF), and T32 OD010957 (to JMC/CJW).
Footnotes
Authors’ disclosure: The authors have no conflicts of interest to declare. Soy protein isolate was donated by Solae, LLC (St. Louis, MO).
Authors’ Contributions Conception and design: JMC, CEW, TCR
Development of methodology: JMC, CEW, CJL, TCR, FND
Data acquisition: FND, CJL, AAF
Histopathology: CJW, JMC
Analysis and interpretation of data: FND, JAT, JMC
References
- 1.Wolff MS, Collman GW, Barrett JC, Huff J. Breast cancer and environmental risk factors: epidemiological and experimental findings. Annu Rev Pharmacol Toxicol. 1996;36:573–96. doi: 10.1146/annurev.pa.36.040196.003041. [DOI] [PubMed] [Google Scholar]
- 2.Cline JM, Wood CE. Estrogen/isoflavone interactions in cynomolgus macaques (Macaca fascicularis) Am J Primatol. 2009;71:722–31. doi: 10.1002/ajp.20680. [DOI] [PubMed] [Google Scholar]
- 3.Kuiper GG, Carlsson B, Grandien K, Enmark E, Haggblad J, Nilsson S, et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. Endocrinology. 1997;138:863–70. doi: 10.1210/endo.138.3.4979. [DOI] [PubMed] [Google Scholar]
- 4.Trock BJ, Hilakivi-Clarke L, Clarke R. Meta-analysis of soy intake and breast cancer risk. J Natl Cancer Inst. 2006;98:459–71. doi: 10.1093/jnci/djj102. [DOI] [PubMed] [Google Scholar]
- 5.Wu AH, Yu MC, Tseng CC, Pike MC. Epidemiology of soy exposures and breast cancer risk. Br J Cancer. 2008;98:9–14. doi: 10.1038/sj.bjc.6604145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warri A, Saarinen NM, Makela S, Hilakivi-Clarke L. The role of early life genistein exposures in modifying breast cancer risk. Br J Cancer. 2008;98:1485–93. doi: 10.1038/sj.bjc.6604321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahlgren M, Melbye M, Wohlfahrt J, Sorensen TIA. Growth patterns and the risk of breast cancer in women. New Engl J Med. 2004;351:1619–26. doi: 10.1056/NEJMoa040576. [DOI] [PubMed] [Google Scholar]
- 8.Apter D. Hormonal events during female puberty in relation to breast cancer risk. Eur J Cancer Prev. 1996;5:476–82. [PubMed] [Google Scholar]
- 9.Howard BA, Gusterson BA. Human breast development. J Mammary Gland Biol Neoplasia. 2000;5:119–37. doi: 10.1023/a:1026487120779. [DOI] [PubMed] [Google Scholar]
- 10.Russo J, Russo IH. Development of the human breast. Maturitas. 2004;49:2–15. doi: 10.1016/j.maturitas.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Baer HJ, Collins LC, Connolly JL, Colditz GA, Schnitt SJ, Tamimi RM. Lobule type and subsequent breast cancer risk: results from the Nurses’ Health Studies. Cancer. 2009;115:1404–11. doi: 10.1002/cncr.24167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russo J, Mailo D, Hu YF, Balogh G, Sheriff F, Russo IH. Breast differentiation and its implication in cancer prevention. Clin Cancer Res. 2005;11:931s–6s. [PubMed] [Google Scholar]
- 13.Richert MM, Schwertfeger KL, Ryder JW, Anderson SM. An atlas of mouse mammary gland development. J Mammary Gland Biol Neoplasia. 2000;5:227–41. doi: 10.1023/a:1026499523505. [DOI] [PubMed] [Google Scholar]
- 14.Cline JM, Wood CE. The Mammary Glands of Macaques. Toxicol Pathol. 2008;36:134s–41s. doi: 10.1177/0192623308327411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wood CE, Hester JM, Cline JM. Mammary gland development in early pubertal female macaques. Toxicol Pathol. 2007;35:795–805. doi: 10.1080/01926230701584213. [DOI] [PubMed] [Google Scholar]
- 16.Weinbauer GF, Niehoff M, Niehaus M, Srivastav S, Fuchs A, Van Esch E, et al. Physiology and Endocrinology of the Ovarian Cycle in Macaques. Toxicol Pathol. 2008;36:7S–23S. doi: 10.1177/0192623308327412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Messina M, Nagata C, Wu AH. Estimated Asian adult soy protein and isoflavone intakes. Nutr Cancer. 2006;55:1–12. doi: 10.1207/s15327914nc5501_1. [DOI] [PubMed] [Google Scholar]
- 18.Stute P, Wood CE, Kaplan JR, Cline JM. Cyclic changes in the mammary gland of cynomolgus macaques. Fertil Steril. 2004;82(Suppl 3):1160–70. doi: 10.1016/j.fertnstert.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 19.Franke AA, Halm BM, Kakazu K, Li X, Custer LJ. Phytoestrogenic isoflavonoids in epidemiologic and clinical research. Drug Test Anal. 2009;1:14–21. doi: 10.1002/dta.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lees CJ, Kaplan JR, Chen H, Jerome CP, Register TC, Franke AA. Bone mass and soy isoflavones in socially housed, premenopausal macaques. Am J Clin Nutr. 2007;86:245–50. doi: 10.1093/ajcn/86.1.245. [DOI] [PubMed] [Google Scholar]
- 21.Morgan PM, Hutz RJ, Kraus EM, Bavister BD. Ultrasonographic assessment of the endometrium in rhesus monkeys during the normal menstrual cycle. Biol Reprod. 1987;36:463–9. doi: 10.1095/biolreprod36.2.463. [DOI] [PubMed] [Google Scholar]
- 22.Wood CE, Register TC, Franke AA, Anthony MS, Cline JM. Dietary soy isoflavones inhibit estrogen effects in the postmenopausal breast. Cancer Res. 2006;66:1241–9. doi: 10.1158/0008-5472.CAN-05-2067. [DOI] [PubMed] [Google Scholar]
- 23.Cline JM. Assessing the mammary gland of nonhuman primates: effects of endogenous hormones and exogenous hormonal agents and growth factors. Birth Defects Res B Dev Reprod Toxicol. 2007;80:126–46. doi: 10.1002/bdrb.20112. [DOI] [PubMed] [Google Scholar]
- 24.Wood CE, Appt SE, Clarkson TB, Franke AA, Lees CJ, Doerge DR, et al. Effects of high-dose soy isoflavones and equol on reproductive tissues in female cynomolgus monkeys. Biol Reprod. 2006;75:477–86. doi: 10.1095/biolreprod.106.052142. [DOI] [PubMed] [Google Scholar]
- 25.Tooze JA, Grunwald GK, Jones RH. Analysis of repeated measures data with clumping at zero. Stat Methods Med Res. 2002;11:341–55. doi: 10.1191/0962280202sm291ra. [DOI] [PubMed] [Google Scholar]
- 26.Hennighausen L, Robinson GW. Information networks in the mammary gland. Nat Rev Mol Cell Biol. 2005;6:715–25. doi: 10.1038/nrm1714. [DOI] [PubMed] [Google Scholar]
- 27.Cline JM, Wood CE. The Mammary Glands of Macaques. Toxicologic Pathology. 2008;36:130S–41S. doi: 10.1177/0192623308327411. 36: , 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eden JA. Breast cancer, stem cells and sex hormones. Part 2: the impact of the reproductive years and pregnancy. Maturitas. 2010;67:215–8. doi: 10.1016/j.maturitas.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 29.Morimoto Y, Killeen J, Hernandez BY, Mark Cline J, Maskarinec G. Parity and expression of epithelial histopathologic markers in breast tissue. Eur J Cancer Prev. 2012 doi: 10.1097/CEJ.0b013e32835c7fc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faupel-Badger JM, Arcaro KF, Balkam JJ, Eliassen AH, Hassiotou F, Lebrilla CB, et al. Postpartum remodeling, lactation, and breast cancer risk: summary of a National Cancer Institute-sponsored workshop. J Natl Cancer Inst. 2013;105:166–74. doi: 10.1093/jnci/djs505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tiede B, Kang Y. From milk to malignancy: the role of mammary stem cells in development, pregnancy and breast cancer. Cell Res. 2011;21:245–57. doi: 10.1038/cr.2011.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lamartiniere CA. Timing of exposure and mammary cancer risk. J Mammary Gland Biol Neoplasia. 2002;7:67–76. doi: 10.1023/a:1015722507237. [DOI] [PubMed] [Google Scholar]
- 33.Rijnkels M, Kabotyanski E, Montazer-Torbati MB, Hue Beauvais C, Vassetzky Y, Rosen JM, et al. The epigenetic landscape of mammary gland development and functional differentiation. J Mammary Gland Biol Neoplasia. 2010;15:85–100. doi: 10.1007/s10911-010-9170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hochberg Z, Feil R, Constancia M, Fraga M, Junien C, Carel JC, et al. Child health, developmental plasticity, and epigenetic programming. Endocr Rev. 2011;32:159–224. doi: 10.1210/er.2009-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Korde LA, Wu AH, Fears T, Nomura AM, West DW, Kolonel LN, et al. Childhood soy intake and breast cancer risk in Asian American women. Cancer Epidemiol Biomarkers Prev. 2009;18:1050–9. doi: 10.1158/1055-9965.EPI-08-0405. [DOI] [PubMed] [Google Scholar]
- 36.Shu XO, Jin F, Dai Q, Wen W, Potter JD, Kushi LH, et al. Soyfood intake during adolescence and subsequent risk of breast cancer among Chinese women. Cancer Epidemiol Biomarkers Prev. 2001;10:483–8. [PubMed] [Google Scholar]
- 37.Thanos J, Cotterchio M, Boucher BA, Kreiger N, Thompson LU. Adolescent dietary phytoestrogen intake and breast cancer risk (Canada) Cancer Causes Control. 2006;17:1253–61. doi: 10.1007/s10552-006-0062-2. [DOI] [PubMed] [Google Scholar]
- 38.Hilakivi-Clarke L, Onojafe I, Raygada M, Cho E, Skaar T, Russo I, et al. Prepubertal exposure to zearalenone or genistein reduces mammary tumorigenesis. Br J Cancer. 1999;80:1682–8. doi: 10.1038/sj.bjc.6690584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Badger TM, Ronis MJ, Simmen RC, Simmen FA. Soy protein isolate and protection against cancer. J Am Coll Nutr. 2005;24:146S–9S. doi: 10.1080/07315724.2005.10719456. [DOI] [PubMed] [Google Scholar]
- 40.Fritz WA, Coward L, Wang J, Lamartiniere CA. Dietary genistein: perinatal mammary cancer prevention, bioavailability and toxicity testing in the rat. Carcinogenesis. 1998;19:2151–8. doi: 10.1093/carcin/19.12.2151. [DOI] [PubMed] [Google Scholar]
- 41.Choi YS, Chakrabarti R, Escamilla-Hernandez R, Sinha S. Elf5 conditional knockout mice reveal its role as a master regulator in mammary alveolar development: failure of Stat5 activation and functional differentiation in the absence of Elf5. Dev Biol. 2009;329:227–41. doi: 10.1016/j.ydbio.2009.02.032. [DOI] [PubMed] [Google Scholar]
- 42.Rahn JJ, Dabbagh L, Pasdar M, Hugh JC. The importance of MUC1 cellular localization in patients with breast carcinoma: an immunohistologic study of 71 patients and review of the literature. Cancer. 2001;91:1973–82. doi: 10.1002/1097-0142(20010601)91:11<1973::aid-cncr1222>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 43.Stute P, Sielker S, Wood CE, Register TC, Lees CJ, Dewi FN, et al. Life stage differences in mammary gland gene expression profile in non-human primates. Breast Cancer Res Treat. 2012;133:617–34. doi: 10.1007/s10549-011-1811-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jefferson WN, Patisaul HB, Williams CJ. Reproductive consequences of developmental phytoestrogen exposure. Reproduction. 2012;143:247–60. doi: 10.1530/REP-11-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng G, Remer T, Prinz-Langenohl R, Blaszkewicz M, Degen GH, Buyken AE. Relation of isoflavones and fiber intake in childhood to the timing of puberty. Am J Clin Nutr. 2010;92:556–64. doi: 10.3945/ajcn.2010.29394. [DOI] [PubMed] [Google Scholar]
- 46.Wolff MS, Britton JA, Boguski L, Hochman S, Maloney N, Serra N, et al. Environmental exposures and puberty in inner-city girls. Environ Res. 2008;107:393–400. doi: 10.1016/j.envres.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim J, Kim S, Huh K, Kim Y, Joung H, Park M. High serum isoflavone concentrations are associated with the risk of precocious puberty in Korean girls. Clin Endocrinol (Oxf) 2011;75:831–5. doi: 10.1111/j.1365-2265.2011.04127.x. [DOI] [PubMed] [Google Scholar]
- 48.De Assis S, Hilakivi-Clarke L. Timing of dietary estrogenic exposures and breast cancer risk. Ann N Y Acad Sci. 2006;1089:14–35. doi: 10.1196/annals.1386.039. [DOI] [PubMed] [Google Scholar]
- 49.Setchell KD, Clerici C. Equol: pharmacokinetics and biological actions. J Nutr. 2010;140:1363S–8S. doi: 10.3945/jn.109.119784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cassidy A, Brown JE, Hawdon A, Faughnan MS, King LJ, Millward J, et al. Factors affecting the bioavailability of soy isoflavones in humans after ingestion of physiologically relevant levels from different soy foods. J Nutr. 2006;136:45–51. doi: 10.1093/jn/136.1.45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.