Abstract
Objective
To evaluate the effect of Medicaid bed-hold policies on hospitalization of long-stay nursing home residents.
Data Sources
A nationwide random sample of long-stay nursing home residents with data elements from Medicare claims and enrollment files, the Minimum Data Set, the Online Survey Certification and Reporting System, and Area Resource File. The sample consisted of 22,200,089 person-quarters from 754,592 individuals who became long-stay residents in 17,149 nursing homes over the period beginning January 1, 2000 through December 31, 2005.
Study Design
Linear regression models using a pre/post design adjusted for resident, nursing home, market, and state characteristics. Nursing home and year-quarter fixed effects were included to control for time-invariant facility influences and temporal trends associated with hospitalization of long-stay residents.
Principal Findings
Adoption of a Medicaid bed-hold policy was associated with an absolute increase of 0.493 percentage points (95% CI: 0.039–0.946) in hospitalizations of long-stay nursing home residents, representing a 3.883 percent relative increase over the baseline mean.
Conclusions
Medicaid bed-hold policies may increase the likelihood of hospitalization of long-stay nursing home residents and increase costs for the federal Medicare program.
Keywords: Medicaid, Medicare, bed-hold policies, hospitalization
Many states have enacted bed-hold programs with the intent of providing continuity of care for Medicaid beneficiaries residing in nursing homes.1 These states pay nursing homes to reserve beds so that the Medicaid residents may return to their facility of occupancy following an acute hospitalization. The policies appear to be effective in achieving that goal (Intrator et al. 2009). However, reimbursements made to nursing homes for days that residents are hospitalized may influence facilities' propensity to hospitalize occupants. The goal of this article is to examine the effect of state Medicaid bed-hold policies on hospitalizations of long-stay nursing home residents. Understanding the influence Medicaid bed-hold policies have on the cost and quality of care will inform policy makers as they consider the benefits of these programs in the context of competing budget priorities. Our study addresses the magnitude of the impact of bed-hold policies on hospitalizations and also provides information on the costs they impose on the federal Medicare program.
Background
Prior studies have examined the relationship between state Medicaid bed-hold policies and hospitalization of nursing home residents, but they differ in their methods and populations studied. Freiman and Murtaugh (1993) used data from the 1987 National Medical Expenditures Survey and did not find a statistically significant association between states' bed-hold policies and hospitalizations. Intrator et al. (2007) used cross-sectional data consisting of assessments from the Minimum Data Set and Medicare inpatient claims from 2000 to estimate the impact of bed-hold policies on hospitalizations among nursing home residents. This study found a highly significant association between the presence of bed-hold policies and hospitalization of long-stay nursing home residents, but it suggested that nursing homes were unable to target particular types of hospitalizations. However, the study's finding may have resulted from its inability to assess policy changes over time, leading to estimates reflecting heterogeneity in nursing home hospitalization rates that may have existed in the absence of bed-hold policies. A more recent examination of nursing home residents found an increased likelihood of hospitalization after residents became eligible for a state's bed-hold policy (Cai et al. 2011). The study was limited to residents in a single state and was not able to assess bed-hold policy changes over time. Bed-hold policies have also been associated with hospitalizations of short-stay nursing home residents covered by Medicare through hypothesized spillover effects (Grabowski et al. 2010).
Hospitalization of nursing home residents often leads to functional and cognitive decline and exposes individuals to iatrogenic disease (Ouslander, Weinberg, and Phillips 2000; Boockvar et al. 2004; Coleman et al. 2004). In addition, hospitalization of nursing home residents is frequent and costly (Grabowski, O'Malley, and Barhydt 2007). As noted by Grabowski (2008), these issues have led to increased interest in hospitalizations of nursing home residents among policy makers. To our knowledge, this study is the first longitudinal investigation of the effects of state Medicaid bed-hold policies on the hospitalization of long-stay nursing home residents using a nationally representative sample.
Conceptual Framework
Given the narrow financial margins that many nursing homes operate under, payment changes created by new or modified state and federal policies have been hypothesized to necessitate adaptive responses by nursing homes in the context of local market forces to avoid performance failure (Zinn et al. 2009). Organizational response to increase profit margins may affect the case mix of residents, staffing levels, among other aspects of care that impact its quality (Intrator, Castle, and Mor 1999; Intrator, Zinn, and Mor 2004; Feng et al. 2006; Intrator et al. 2007; Gruneir et al. 2008). Our conceptual framework posits a relationship between Medicaid bed-hold reimbursements to nursing homes and hospitalization of residents. States with bed-hold policies provide payments to nursing homes as an incentive to reserve beds for residents during acute hospitalizations. These policies differ between states in terms of the amount of daily reimbursements and the number of qualifying days, in addition to some states requiring sufficient occupancy rates to receive payments. However, these policies create an incentive to hospitalize Medicaid nursing home residents when the marginal profit associated with bed-hold payment surpasses the marginal profit associated with caring for an individual in the nursing home. Grabowski et al. (2010) also hypothesized this relationship and conjectured that spillover effects arising from Medicaid bed-hold policies increased rehospitalization of Medicare patients receiving skilled nursing care in nursing homes. The results of their study were consistent with the stated hypothesis.
Long-stay residents should be in stable health, similar to community dwelling older adults (Intrator, Zinn, and Mor 2004). Therefore, hospitalizations of long-stay nursing home residents are a marker of the quality of care received, controlling for patients' underlying health and severity of illness. Due to the potentially endogenous relationship between rehospitalization and complications arising from the preceding hospitalization, residents with short stays were excluded from our study (Intrator, Castle, and Mor 1999; Intrator, Zinn, and Mor 2004; Mor et al. 2010).
Methods
Sources of Data/Study Population
Our data source was a longitudinal file composed of the Minimum Data Set Resident Assessment Instrument (MDS), Medicare inpatient claims, the On-line Survey of Certification and Reporting (OSCAR), and the Area Resource File (ARF) for the period beginning January 1, 2000 through December 31, 2005. The most recent MDS assessment prior to the beginning of the quarter was used for each resident. The MDS includes data on over 400 items and imparted details on case mix acuity, diagnoses and health conditions, cognitive and physical functioning, among other factors. Many of these items have been previously validated (Mor et al. 2011). Medicare inpatient claims provided information on hospital discharges, including primary and secondary diagnosis fields. OSCAR supplied nursing homes characteristics, such as occupancy rates, staffing, case mix, size, proprietary status, hospital affiliation, in addition to other traits. Characteristics of counties, which we used as a proxy for markets, were obtained from the ARF. These included, but were not limited to, the Herfindahl index, demographic characteristics, and supply of hospital beds. Data on state policies, collected through a comprehensive survey conducted by the Center for Gerontology and Health Care Research at Brown University, were incorporated.
The primary analytic file consisted of a 25 percent random sample of long-stay residents (N = 754,592), defined as individuals residing in nursing homes for 90 days or more. In a secondary analysis, three samples, one for each case state (Illinois, Massachusetts, and Michigan), were created. For each of these samples, every nursing home in the case state was matched to a control facility among the pool of nursing homes in states that did not experience a bed-hold policy change. The samples created more similar groups for comparison as the broader sample in our primary analysis may have included some nursing homes in control states that had characteristics much different from those in case states. Nursing homes were matched on for-profit status, the proportion of registered nurses among a facility's licensed practical nurses and registered nurses, the average total hours per day registered nurses spent with each resident, in addition to the presence of a medical doctor and/or a physician extender, such as a nurse practitioner (Bergstralh and Kosanke 2011). All long-stay residents from the matched nursing homes that met the criteria specified for our study population below were used in the analyses. In all samples, many residents were observed more than once with a different number at risk of hospitalization in each quarter.
Our study population was restricted to long-stay residents at least 65 years old as nonelderly residents have conditions that differ from the broader nursing home population (Lair 1992; Buchanan et al. 2001, 2003; Buchanan, Wang, and Huang 2002; Aschbrenner et al. 2011). In addition, nursing home residents participating in Medicare managed care were not included as we lacked access to claims data for these individuals. Due to unique geographic and political features, individuals residing in facilities in Alaska, Hawaii, and the District of Columbia were excluded.
Two additional national samples were created for sensitivity analyses. The first was limited to individuals in nursing homes where 85 percent or more of the residents were covered by states' Medicaid programs. Bed-hold programs only reimburse nursing homes for residents who are Medicaid beneficiaries, and a more concentrated effect of the policy should be seen among this population. The second sensitivity analysis excluded residents who died, but were not hospitalized, in the same quarter. This was done to assess the effect of mortality on hospitalization rates. If bed-hold policies were associated with mortality, estimates of the likelihood of hospitalization may be biased (Gorodeski, Starling, and Blackstone 2010).
Variables
An active state Medicaid bed-hold policy was the determinant of interest for hospitalizations of long-stay nursing home residents. The variable was coded to indicate the presence of a bed-hold policy if one was in effect at any time during a given quarter in the state in which a nursing home was located. Four states implemented or repealed bed-hold policies over the 6-year study period. In 2001, Michigan implemented a new bed-hold policy, which it maintained through the remaining years of the study period. Illinois terminated a bed-hold policy in July 2003 and reinstated it in August 2004, but with a required minimum occupancy rate for Medicaid residents of 90 percent. In July 2004, Massachusetts repealed its policy only to reinstate it 6 months later with retroactive payments for the termination period. Tennessee both repealed and reinstated the state's bed-hold policy within a 2-month period in 2005. As the policy was discontinued and reinstated in the same quarter, the structure of our data file precluded us from evaluating it for this state.
Our primary outcome measure was any hospitalization in the quarter with admission directly from a nursing home. This was a binary indicator that did not differentiate between the number, or length, of hospitalizations. Thus, our estimates indicate the likelihood of a resident experiencing at least one hospitalization during the quarter. Death occurring within the quarter (yes/no) was assessed as a separate outcome to evaluate the association between bed-hold policies and the likelihood of mortality. Control variables at the patient level were derived from residents' most recent MDS assessments. On average, these were completed about 51 days prior to the beginning of the quarter. These measures consisted of basic demographic characteristics, including gender, race, and age. Variables from the MDS reflecting health and mobility were used to signify clinical risk of hospitalization. These included chronic diagnoses, symptoms predictive of hospitalization, cognitive impairment, and other signs of poor health. Specific variables predicting these outcomes and conditions included indicators for a diagnosis of diabetes, cancer, emphysema, or chronic obstructive pulmonary disease to account for chronic conditions associated with hospitalization (Castle and Mor 1996); binary measures of fever and weight loss, as these are symptoms that may be linked to higher likelihood of hospitalization (Intrator et al. 2007); Cognitive Performance Scale above 3 (Morris et al. 1994); high body mass index (>30); low body mass index (<19); required assistance for activities of daily living; current use of nine or more prescription drugs (Intrator et al. 2007); receipt of antipsychotics or hypnotics; use of restraints; or any hospice utilization. Advance directives reduce the chances of hospitalization with documented restrictions on treatment and also potentially through undocumented limitations on care (Zweig et al. 2004; Gozalo and Miller 2007). As such, an indicator for the presence of a do-not-resuscitate order was also used as a control. Variables for each level of the Changes in Health, End-Stage Disease and Symptoms and Signs (CHESS) scale, which is predictive of declining health, were also included (Hirdes, Frijters, and Teare 2003). Previous research has suggested that bed-hold policies are unable to target specific types of hospitalization (Intrator et al. 2007). Therefore, interactions between the CHESS variables and policy indicator were used to assess whether residents were disproportionately affected based on severity of illness. For example, bed-hold policies may have lowered the threshold for hospitalization, which would have had a disproportionate effect on those with a lower CHESS score.
We also controlled for nursing home characteristics. These independent variables included quarterly occupancy rates, percent of black residents, the proportions of Medicare and Medicaid residents, total registered nurse hours/day per resident, and the mean value of Resource Utilization Groups across residents in each facility.
Medicaid per diem rates paid by states to nursing homes (adjusted for the Consumer Price Index) and the use of case mix adjustment for reimbursements have been shown to independently influence hospitalization (Intrator and Mor 2004; Feng et al. 2006). Measures of each were used in our analysis. Competitive nursing home markets have also been previously associated with hospitalizations. This warranted inclusion of an indicator for a Herfindahl index less than 0.10 (Intrator et al. 2007).
Statistical Analyses
The following model specification was used with the person-quarter as the unit of analysis:
| (1) |
Residents, states, and quarters were indexed by i, j, and t, respectively. HOSP is an indicator for any hospitalization of a long-stay resident admitted directly from a nursing home during the quarter. POLICY is a measure for the presence of a state bed-hold policy; X is a set of patient, nursing home, and market characteristics; and ηi and μt represent nursing home and year-quarter fixed effects, respectively. These absorbed unobserved time-invariant characteristics of facilities and controlled for seasonal trends or other shocks occurring within specific time periods. Thus, our model identified the impact of bed-hold policies on hospitalizations through the implementation and termination of states' programs over time.
Equation (1) was treated as a linear probability model. This overlooks the dichotomous nature of the outcome, but it should yield consistent estimates given the extremely large number of observations in our analytic file and the broad array of independent variables used in the model. The standard errors were adjusted for clustering at the level of the state-quarter. All analyses were carried out using SAS version 9.2 (SAS Institute, Cary, NC) and Stata SE version 11 (StataCorp, College Station, TX).
Results
Hospitalization rates rose over the study period for each of our case states but appeared to experience abrupt increases when bed-hold policies were implemented (Figure 1). Compared with residents in non-bed-hold states, those in states with active policies tended to be older, were less likely to be racial minorities, and differed in the prevalence of some comorbidities (Table 1). Nursing homes in bed-hold states tended to have lower proportions of Medicare patients, higher occupancy rates, housed residents of slightly higher acuity, and were more likely to be located in competitive markets. States with bed-hold policies had higher Medicaid reimbursements to nursing homes but fewer adjusted payments for patient case mix.
Figure 1.
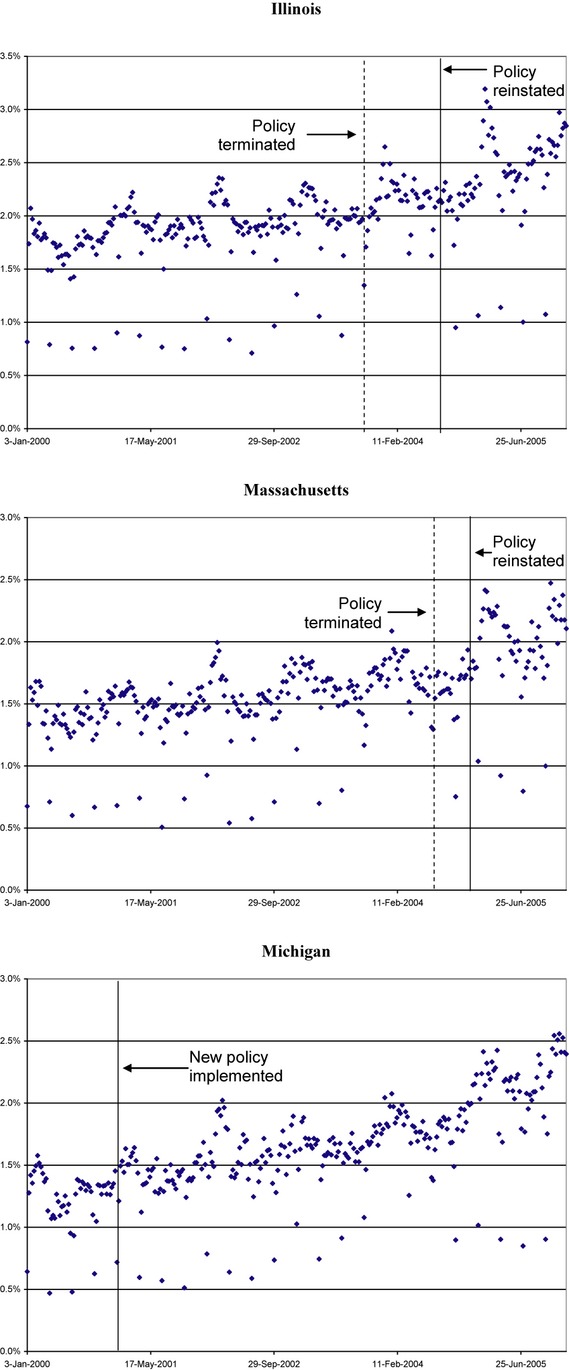
Unadjusted Weekly Hospitalization Rates of Nursing Home Residents
Table 1.
| No Bed-Hold | Bed-Hold | p-Value | |
|---|---|---|---|
| Residents | (n = 140,285) | (n = 614,307) | |
| Age | 82.87 | 83.26 | <0.001 |
| Male (%) | 27.96 | 27.71 | 0.0625 |
| Black (%) | 10.47 | 9.13 | <0.001 |
| Other race (%) | 5.97 | 3.74 | <0.001 |
| Do-not-resuscitate order (%) | 52.50 | 52.25 | 0.0991 |
| CHESS1 (%) | 31.80 | 32.13 | 0.0164 |
| CHESS2 (%) | 22.42 | 23.91 | <0.001 |
| CHESS3 (%) | 9.88 | 10.96 | <0.001 |
| CHESS4 (%) | 3.26 | 3.50 | <0.001 |
| CHESS5 (%) | 0.34 | 0.33 | 0.5388 |
| Complete ADL impairment (%) | 8.71 | 7.91 | <0.001 |
| Cognitive Performance Scale >3 (%) | 57.88 | 56.77 | <0.001 |
| Weight loss (%) | 13.37 | 13.09 | 0.005 |
| Unstable status (%) | 38.61 | 37.16 | <0.001 |
| Fever (%) | 1.79 | 1.72 | 0.0786 |
| Diabetes mellitus (%) | 24.64 | 24.65 | 0.9716 |
| Congestive heart failure (%) | 14.88 | 17.74 | <0.001 |
| Emphysema/COPD (%) | 9.96 | 12.10 | <0.001 |
| Cancer (%) | 4.14 | 5.33 | <0.001 |
| 9 + medications in last 7 days (%) | 40.88 | 40.69 | 0.1929 |
| Any antipsychotics/hypnotics use (%) | 28.02 | 27.03 | <0.001 |
| Restraint use (%) | 5.62 | 4.42 | <0.001 |
| Hospice care (%) | 2.45 | 1.96 | <0.001 |
| Nursing homes | (n = 3,510) | (n = 13,639) | |
| Percent Medicaid ≥85% | 16.50 | 16.81 | 0.6544 |
| Percent Medicare ≥15% | 19.49 | 17.35 | 0.0031 |
| Percent black | 8.73 | 8.19 | 0.0698 |
| Occupancy rate ≥95% | 23.13 | 29.10 | <0.001 |
| Total direct care hours/day/resident | 3.46 | 3.41 | 0.2102 |
| Mean RUGS across nursing home | 0.79 | 0.80 | 0.0112 |
| Percent in a competitive market | 38.83 | 48.02 | <0.001 |
| States | |||
| Medicaid daily rate (CPI adj.) | 112.64 | 120.24 | <0.001 |
| Case mix reimbursement (%) | 73.91 | 64.77 | |
| Bed-hold policy (%) | 20.47 | 79.53 | |
Note that the first observation of each resident and nursing home was used.
State information was from 2005.
Regression estimates using our nationwide 25 percent random sample indicated a higher likelihood of hospitalization associated with bed-hold policies (Table 2 (i)). Presence of an active policy was associated with a statistically significant absolute increase of 0.493 percentage points in the likelihood of any hospitalization, representing a 3.883 percent relative increase over the unadjusted baseline mean (12.698 percent) for all states during the study period. As would be expected, an increased risk of hospitalization was associated with a higher score on the CHESS scale. However, regression estimates for interactions between CHESS levels and the policy indicator did not reveal a consistent pattern indicating an increased risk based on acuity. Higher Medicaid daily rates paid to nursing homes did not appear to influence hospitalizations. Conversely, use of case mix reimbursement by states significantly lowered the likelihood of hospitalization.
Table 2.
Regression Estimates†
| (i) | (ii) | (iii) | (iv) | |
|---|---|---|---|---|
| Variables | National 25% Sample | IL & Matched Controls | MA & Matched Controls | MI & Matched Controls |
| Policy | 0.00493** (0.000393–0.00946) | 0.00535**(0.000283–0.0104) | −0.00143 (−0.00695–0.00410) | 0.00315* (−0.000318–0.00662) |
| CHESS 1 | 0.0285*** (0.0260–0.0311) | 0.0326*** (0.0290–0.0361) | 0.0204*** (0.0167–0.0240) | 0.0240*** (0.0217–0.0264) |
| CHESS 2 | 0.0629*** (0.0588–0.0671) | 0.0757*** (0.0684–0.0831) | 0.0444*** (0.0386–0.0501) | 0.0546*** (0.0512–0.0580) |
| CHESS 3 | 0.112*** (0.106–0.118) | 0.150***(0.121–0.178) | 0.0894*** (0.0825–0.0962) | 0.0929*** (0.0870–0.0987) |
| CHESS 4 | 0.123*** (0.114–0.131) | 0.163*** (0.135–0.191) | 0.0907*** (0.0784–0.103) | 0.100*** (0.0883–0.112) |
| CHESS 5 | 0.122***(0.103–0.141) | 0.177*** (0.144–0.210) | 0.100*** (0.0611–0.139) | 0.118*** (0.0915–0.145) |
| Policy*CHESS1 | −0.00304** (−0.00578–−0.000287) | −0.00320* (−0.00696–0.000549) | 0.00542*** (0.00153–0.00931) | 0.00111 (−0.00156–0.00378) |
| Policy*CHESS2 | 0.000131 (−0.00424–0.00450) | −0.00558 (−0.0124–0.00119) | 0.0184*** (0.0122–0.0247) | 0.00629*** (0.00236–0.0102) |
| Policy*CHESS3 | 0.00126 (−0.00550–0.00802) | −0.0229* (−0.0502–0.00438) | 0.0178***(0.00959–0.0260) | 0.0108*** (0.00379–0.0178) |
| Policy*CHESS4 | 0.00592 (−0.00318–0.0150) | −0.0122 (−0.0391–0.0148) | 0.0276*** (0.0136–0.0416) | 0.0157** (0.00152–0.0299) |
| Policy*CHESS5 | 0.000640 (−0.0201–0.0213) | −0.0309* (−0.0649–0.00305) | 0.0294 (−0.0129–0.0716) | −0.00474 (−0.0342–0.0247) |
| N | 5,541,274 | 2,101,621 | 1,350,541 | 1,339,097 |
Note. Robust confidence intervals (95%) in parentheses adjusted for clustering at the level of the state-quarter.
All models include nursing home and year/quarter fixed effects.
***p < .01; **p < .05; *p < .1.
We found heterogeneous effects associated with bed-hold policies in our secondary analysis that examined residents in nursing homes from each case state that were matched with facilities in states that did not experience a policy change. An increase of 3.790 percent (an absolute increase of 0.535 percent) in the likelihood of hospitalization relative to the state's unadjusted baseline mean for the study period was associated with Illinois's bed-hold policy (Table 2 (ii)). The effect of the state's policy did not vary significantly by resident acuity. Massachusetts's bed-hold policy was not associated with higher overall rates of hospitalization among long-stay nursing home residents (Table 2 (iii)). The estimated effect of Michigan's bed-hold program just missed statistical significance at the 5 percent level, but it indicated a modest absolute increase of 0.315 percentage points in the likelihood of hospitalization, representing a relative increase of 0.028 percent compared with the state's unadjusted mean hospitalization rate (Table 2 (iv)).
Sensitivity Analyses
Bed-hold programs only reimburse nursing homes for days associated with the hospitalization of residents participating in states' Medicaid programs. If nursing homes are more likely to hospitalize residents to generate additional revenue from bed-hold reimbursements, a stronger effect should be seen among residents with Medicaid as their primary source of payment. Our data source did not include payment information for individuals, but we were able to identify nursing homes with a high percentage of Medicaid residents (≥85 percent) in our national sample. Using the sample of residents in high-Medicaid facilities, the estimated effect of bed-hold policies on the likelihood of hospitalization derived from model (1) increased substantially compared with our primary analysis. Presence of a bed-hold policy was associated with a 5.446 percent increase relative to the baseline mean (14.138 percent) among residents in these nursing homes.
The potential effect of mortality on the likelihood of hospitalization was ignored in our primary analysis using hospitalization as the outcome. Death is a competing outcome and its influence on the estimated effect of bed-hold policies on hospitalization needs to be considered (Intrator et al. 2007; Gorodeski, Starling, and Blackstone 2010; Grabowski et al. 2010). We addressed this issue in two ways. First, we repeated our primary analysis using death in the quarter (yes/no) as the outcome for model (1). The results indicated that bed-hold policies were not significantly associated with a higher likelihood of mortality. Second, we created a national sample that excluded patients who died but were not hospitalized during the same quarter. If bed-hold policies increased mortality, and patients who died were at higher risk of hospitalization but died prior to hospitalization, our primary analysis may have been biased. Estimating parameters with this sample using model (1) allowed us to compare them with the results from our main analysis to determine whether this was the case. The parameter estimate associated with the presence of a bed-hold policy obtained with the new sample was consistent with our initial result (data are not shown but are available from the authors).
Discussion
Medicaid bed-hold policies appear to be effective at increasing the likelihood of residents returning to the nursing homes they occupied prior to hospitalization (Intrator et al. 2009). Although we were unable to determine the cost to states, as our data source precluded us from determining the exact number of hospitalizations for residents and the number of days nursing homes were reimbursed by Medicare for skilled nursing care as opposed to Medicaid payments for long-term care, it is clear that these policies place a significant financial burden on states. Given the budgetary stress that many states are experiencing in the current financial climate, some have considered eliminating their policies (Lazar 2011). Policy makers should consider whether the benefit of continuity of care outweighs the expense of these policies, keeping their impact on the quality of care in mind.
The increases in hospitalization of long-stay nursing home residents associated with bed-hold policies not only reflects a serious concern for the quality of care but also imposes costs on the federal Medicare program that may be ignored by state policy makers. We identified 752,061 long-stay nursing home residents in states with an active bed-hold policy in the last quarter of 2005. Our estimated 0.493 percentage point increase in the hospitalization of long-stay nursing home residents associated with states' bed-hold policies translates to 14,830 additional acute hospital stays annually for this population. Assuming an average cost of $8,300 per hospitalization, a simple calculation to approximate the additional expense to Medicare yields an estimate of $123M yearly (Jencks, Williams, and Coleman 2009; Grabowski et al. 2010). This is a conservative figure given that the outcome used in our primary analysis only measured whether residents had any hospitalization in a quarter and did not account for individuals having multiple hospital stays in the same period. Moreover, the estimated expense to Medicare did not include costs associated with higher payments for skilled nursing care when residents returned to nursing homes. Payments for hospitalizations of residents with nursing home stays of less than 90 days were also not incorporated into the estimate. Previously demonstrated spillover effects of bed-hold policies affecting hospitalization of patients receiving skilled nursing care would be included in this group (Grabowski et al. 2010). If these expenditures were added in, the overall estimated cost to Medicare would be substantially higher.
The effect of bed-hold policies on hospitalizations underscores the consequences of failing to align financial incentives between state and federal payers. Although bed-hold policies may be effective at increasing the continuity of care for nursing home residents, there is no incentive for states to consider the cost of hospitalizations borne by the federal Medicare program. States could make investments in Medicaid services that would reduce the likelihood of hospitalization for nursing home residents, but the savings would go to Medicare providing little incentive to initiate them (Grabowski 2007). Similarly, as states seek to minimize expenditures, reductions in Medicaid services may adversely impact Medicare spending. Bed-hold programs exemplify the negative impact of fragmentation in services for individuals participating in both Medicaid and Medicare.
Our study has limitations that warrant discussion. We were unable to evaluate the influence of changes in specific components of states' bed-hold policies: the proportion of the average Medicaid daily rate paid to nursing homes, the number of qualifying days, and minimum required occupancy rate. Among our case states, only Illinois changed its requirements for bed-hold payments. When the state's policy was reinstated in 2004, it required a minimum occupancy rate of 90 percent for Medicaid residents. Despite the new Medicaid occupancy requirement, our estimates indicated that the state's bed-hold policy led to increased hospitalization rates for long-stay nursing home residents. Grabowski et al. (2010) previously noted that little monitoring and enforcement of occupancy rates occurs, indicating that they may have little effect on the behavior of nursing homes. In addition, we controlled for unobserved time-invariant factors affecting hospitalizations of nursing home residents as well as a variety of influences that may have changed over time. However, we cannot rule out the possibility of bias arising from unobserved time-varying factors (Besley and Case 1994). For example, nursing homes may alter their behavior and work to reduce hospitalizations if state officials threaten to repeal a bed-hold program, which would bias estimates toward the null.
In conclusion, Medicaid bed-hold polices may have important budgetary consequences for both state and federal programs in addition to implications for the quality of care received by nursing home residents. Given these concerns, states with bed-hold policies may wish to reconsider their value as budget priorities compete for sparse resources. In a broader context, bed-hold policies highlight the inefficiencies created by fragmentation of health care services for nursing home residents participating in both Medicaid and Medicare. Reconsideration of bed-hold policies should be part of larger reforms aimed at coordination of care.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: National Institute on Aging (grant 1P01AG027296) “Shaping Long-Term Care in America”; the Robert Wood Johnson Foundation Program: Changes in Health Care Financing and Organization (grant 64435); Health Assessment Lab: Alvin R. Tarlov and John E. Ware Jr. Doctoral Dissertation Award to Dr. Unruh.
Disclosures: Dr. Vincent Mor is a co-founder of PointRight (formerly LTCQ, Inc.) and currently serves as a member of its Board of Directors. During the previous 36 months, Dr. Mor has also been a member of the boards of HCRManorCare, NaviHealth, Tufts Health Plan Foundation, and Hospice Care of Rhode Island. He has also been a consultant for Abt Associates, Research Triangle Institute, Welsh Carson Investment Co., and Alliance for Long Term Care Quality. An abstract based on this project was presented at the AcademyHealth Annual Research Meeting in June 2012 in Orlando, Florida.
Disclaimers: None.
Footnotes
States with active bed-hold policies in 2005 (Q4): AL, AR, AZ, CA, CT, DE, FL, GA, IA, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MS, MT, ND, NE, NJ, NM, NY, OH, OK, PA, SC, SD, TN, VT, WI, WV, and WY.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Aschbrenner K, Grabowski D, Cai S, Bartels S, Mor V. “Nursing Home Admissions and Long-Stay Conversions among Persons with and without Serious Mental Illness”. Journal of Aging & Social Policy. 2011;23(3):286. doi: 10.1080/08959420.2011.579511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergstralh E, Kosanke J. “GMATCH SAS Macro”. 2011. Available at http://mayoresearch. mayo. edu/mayo/research/biostat/sasmacros. cfm. Accessed April 28.
- Besley T, Case A. “Unnatural Experiments? Estimating the Incidence of Endogenous Policies”. National Bureau of Economic Research. 1994 w. 4956. [Google Scholar]
- Boockvar K, Fishman E, Kyriacou CK, Monias A, Gavi S, Cortes T. “Adverse Events Due to Discontinuations in Drug Use and Dose Changes in Patients Transferred between Acute and Long-Term Care Facilities”. Archives of Internal Medicine. 2004;164(5):545. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- Buchanan RJ, Wang S, Huang C. “Profiles of Nursing Home Residents with HIV”. Journal of Health Care for the Poor and Underserved. 2002;13(3):379–91. doi: 10.1353/hpu.2010.0698. [DOI] [PubMed] [Google Scholar]
- Buchanan RJ, Wang S, Huang C, Graber D. “Profiles of Nursing Home Residents with Multiple Sclerosis Using the Minimum Data Set”. Multiple Sclerosis. 2001;7(3):189. doi: 10.1177/135245850100700310. [DOI] [PubMed] [Google Scholar]
- Buchanan RJ, Gorman DM, Wang S, Huang C. “Co-morbidity and Treatment Needs among Nursing Home Residents Receiving Alcohol and Drug Treatment”. Journal of Addictive Diseases. 2003;22(2):31–47. doi: 10.1300/J069v22n02_03. [DOI] [PubMed] [Google Scholar]
- Cai S, Mukamel DB, Veazie P, Katz P, Temkin-Greener H. “Hospitalizations in Nursing Homes: Does Payer Source Matter? Evidence from New York State”. Medical Care Research and Review. 2011;68(5):559–78. doi: 10.1177/1077558711399581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle NG, Mor V. “Hospitalization of Nursing Home Residents: A Review of the Literature, 1980–1995”. Medical Care Research and Review. 1996;53(2):123. doi: 10.1177/107755879605300201. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Min S, Chomiak A, Kramer AM. “Posthospital Care Transitions: Patterns, Complications, and Risk Identification”. Health Services Research. 2004;39(5):1449–66. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, Grabowski DC, Intrator O, Mor V. “The Effect of State Medicaid Case-Mix Payment on Nursing Home Resident Acuity”. Health Services Research. 2006;41(4p1):1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freiman MP, Murtaugh CM. “The Determinants of the Hospitalization of Nursing Home Residents”. Journal of Health Economics. 1993;12(3):349–59. doi: 10.1016/0167-6296(93)90017-9. [DOI] [PubMed] [Google Scholar]
- Gorodeski EZ, Starling RC, Blackstone EH. “Are All Readmissions Bad Readmissions?”. New England Journal of Medicine. 2010;363(3):297–8. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- Gozalo PL, Miller SC. “Hospice Enrollment and Evaluation of Its Causal Effect on Hospitalization of Dying Nursing Home Patients”. Health services research. 2007;42(2):587–610. doi: 10.1111/j.1475-6773.2006.00623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC. “Medicare and Medicaid: Conflicting Incentives for Long-Term Care”. Milbank Quarterly. 2007;85(4):579–610. doi: 10.1111/j.1468-0009.2007.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC. “Medicaid Nursing Home Payment and the Role of Provider Taxes”. Medical Care Research and Review. 2008;65(4):514. doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, O'Malley AJ, Barhydt NR. “The Costs and Potential Savings Associated with Nursing Home Hospitalizations”. Health Affairs. 2007;26(6):1753. doi: 10.1377/hlthaff.26.6.1753. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Feng Z, Intrator O, Mor V. “Medicaid Bed-Hold Policy and Medicare Skilled Nursing Facility Rehospitalizations”. Health Services Research. 2010;45(6p2):1963–80. doi: 10.1111/j.1475-6773.2010.01104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruneir A, Miller SC, Feng Z, Intrator O, Mor V. “Relationship Between State Medicaid Policies, Nursing Home Racial Composition, and the Risk of Hospitalization for Black and White Residents”. Health services research. 2008;43(3):869–81. doi: 10.1111/j.1475-6773.2007.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirdes JP, Frijters DH, Teare GF. “The MDS CHESS Scale: A New Measure to Predict Mortality in Institutionalized Older People”. Journal of the American Geriatrics Society. 2003;51(1):96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Castle NG, Mor V. “Facility Characteristics Associated with Hospitalization of Nursing Home Residents: Results of a National Study”. Medical care. 1999;37(3):228. doi: 10.1097/00005650-199903000-00003. [DOI] [PubMed] [Google Scholar]
- Intrator O, Mor V. “Effect of State Medicaid Reimbursement Rates on Hospitalizations from Nursing Homes”. Journal of the American Geriatrics Society. 2004;52(3):393–8. doi: 10.1111/j.1532-5415.2004.52111.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Zinn J, Mor V. “Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long Stay Residents”. Journal of the American Geriatrics Society. 2004;52(10):1730–6. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Grabowski DC, Zinn J, Schleinitz M, Feng Z, Miller S, Mor V. “Hospitalization of Nursing Home Residents: The Effects of States' Medicaid Payment and Bed-Hold Policies”. Health services research. 2007;42(4):1651. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O, Schleinitz M, Grabowski DC, Zinn J, Mor V. “Maintaining Continuity of Care for Nursing Home Residents: Effect of States' Medicaid Bed-Hold Policies and Reimbursement Rates”. Health Services Research. 2009;44(1):33–55. doi: 10.1111/j.1475-6773.2008.00898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. “Rehospitalizations among Patients in the Medicare Fee-for-Service Program”. New England Journal of Medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Lair TJ. A Profile of 1987 Nursing Home Users Under 65. National Medical Expenditure Survey Research Findings 13. Rockville, MD: Agency for Health Care Policy and Research; 1992. [Google Scholar]
- Lazar K. Boston.com. Boston, MA: Boston Globe; 2011. “Lawmakers defy governor, restore nursing home program”. [Google Scholar]
- Mor V, Intrator O, Feng Z, Grabowski DC. “The Revolving Door of Rehospitalization from Skilled Nursing Facilities”. Health Affairs. 2010;29(1):57. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, Unruh M, Cai S. “Temporal and Geographic Variation in the Validity and Internal Consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0”. BMC Health Services Research. 2011;11(1):78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, Lipsitz LA. “MDS Cognitive Performance Scale©”. Journal of Gerontology. 1994;49(4):M174. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Weinberg AD, Phillips V. “Inappropriate Hospitalization of Nursing Facility Residents: A Symptom of a Sick System of Care for Frail Older People”. Journal of the American Geriatrics Society. 2000;48(2):230. doi: 10.1111/j.1532-5415.2000.tb03919.x. [DOI] [PubMed] [Google Scholar]
- Zinn J, Mor V, Feng Z, Intrator O. “Determinants of Performance Failure in the Nursing Home Industry”. Social Science & Medicine. 2009;68(5):933–40. doi: 10.1016/j.socscimed.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweig SC, Kruse RL, Binder EF, Szafara KL, Mehr DR. “Effect of Do Not Resuscitate Orders on Hospitalization of Nursing Home Residents Evaluated for Lower Respiratory Infections”. Journal of the American Geriatrics Society. 2004;52(1):51–8. doi: 10.1111/j.1532-5415.2004.52010.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


