Abstract
Purpose
There is a clear link between dietary behavior and a range of chronic diseases, and overweight and obesity constitute an indirect risk in relation to these diseases. The worksite is a central venue for influencing dietary behavior. The purpose of this paper is to provide an overview of workplace influences on worker dietary patterns.
Design/methodology/approach
The paper reviews the evidence of the effectiveness of dietary health promotion, and provides a brief overview of appropriate theoretical frameworks to guide intervention design and evaluation. The findings are illustrated through research examples.
Findings
Through case studies and published research, it is found that workplace dietary interventions are generally effective, especially fruit and vegetable interventions. There is less consistent evidence on the long term effectiveness of workplace weight management interventions, underscoring the need for further research in this area. This paper also reports evidence that changes in the work environment, including through health and safety programs, may contribute to enhancing the effectiveness of workplace health promotion, including dietary interventions. Organizational factors such as work schedule may also influence dietary patterns. The social ecological model, the social contextual model and political process approach are presented as exemplar conceptual models that may be useful when designing or assessing the effects of workplace health promotion.
Originality/value
Using the worksite as setting for influencing health by influencing dietary patterns holds considerable promise and may be instrumental in reducing workers’ risk of chronic diseases.
Keywords: Workplace, nutrition, obesity, health promotion, occupational safety and health
1. Introduction
There is clear evidence that an unhealthy diet is related to increased risk for a range of chronic diseases, including heart disease, diabetes, and cancer (American Institute for Cancer Research, 2007). Diet plays a direct role in increasing risk of these chronic diseases, and additionally contributes to increased risk indirectly through overweight and obesity (American Institute for Cancer Research, 2007). Dietary recommendations to reduce chronic disease risk include lowering saturated fat, trans-fat, and red meat consumption, and increasing fruit and vegetable intake (American Institute for Cancer Research, 2007, National Institutes of Health, 2002).
Worksites represent an important venue for influencing dietary patterns. Given the considerable time workers spend on their jobs, worksites offer an important venue to reach large numbers of workers in order to provide on-going education as well as healthy food options. In addition, through worksites it may be possible to support behavior changes long-term through co-worker support, changes in the foods available at work, and consideration of other work-related factors associated with workers’ dietary patterns (Sorensen et al., 2004b, Sparling, 2010, Story et al., 2008, Egerter et al., 2008). There is a growing body of evidence supporting the efficacy of these worksite approaches in promoting healthy diets (Glanz et al., 1996, Hennrikus and Jeffery, 1996, Benedict and Arterburn, 2008, Matson-Koffman et al., 2005, Janer et al., 2002, Engbers et al., 2005, Pelletier, 2009).
The purpose of this paper is to provide an overview of workplace influences on worker dietary patterns. We review the evidence for the efficacy and effectiveness of workplace efforts to improve dietary behaviors, overweight/obesity, and the food environment. While some studies have focused on demonstrating efficacy, that is quantifying the magnitude of intervention effect under highly controlled study designs with homogenous populations that maximize internal validity, others have aimed to demonstrate effectiveness, that is study designs that seek to balance internal and external validity by implementing the intervention with more ‘real world’ settings and representative participants (Flay, 1986). We further examine other workplace influences on workers’ dietary habits, including the efforts to prevent work-related illness and injury, reduce work-related stress, and expand work-related benefits and resources. In addition, recognizing the importance of the application of appropriate theoretical frameworks to guide intervention design and evaluation, we provide a brief overview of several models that may be applied to workplace efforts to promote a healthy diet. Although this manuscript is not meant to provide an exhaustive review of the literature, throughout these sections we provide research examples to exemplify the research findings for dietary behaviors.
2. Evidence for efficacy and effectiveness: Influencing dietary behaviors through the worksite
There is a growing body of literature on the effectiveness of workplace programs in improving workers’ dietary habits. Workplace initiatives have targeted a number of dietary behaviors, including fruits and vegetables, fat, red meat intake, and fiber. A review of nutrition and cholesterol worksite programs from 1980 to 1995 reported that approximately half of 26 reviewed studies demonstrated a significant effect on one or more dietary behaviors (Glanz et al., 1996). A more recent review of workplace efforts to improve fruit and vegetable intake identified factors employed by successful programs, including organizational support, targeting multiple levels of influence and participants’ social context (see section 4.1 and 4.2), encouraging worker participation, and addressing multiple health behaviors (Sorensen et al., 2004b).
Much of the worksite research on dietary interventions has focused on fruit and vegetable intake. In the U.S., nine studies were conducted in the 1990s under the National Cancer Institute’s ‘5-a-day for Better Health’ program to increase fruit and vegetable intake; three were implemented in workplaces (Sorensen et al., 1999, Buller et al., 1999, Beresford et al., 2001). Each intervention focused on more than one level of influence including individual workers, their social networks, and changes in the food environment. These studies resulted in significant improvements in fruit and vegetable consumption, with an average effect size of 0.3-0.5 servings of fruits and vegetables per day. Subsequent analyses of the 5-a-day studies conducted among adults demonstrated that improvements in knowledge and self-efficacy were significant mediators of the observed increases in fruit and vegetable intake (Campbell et al., 2008). Similar research has also been conducted in Europe. For example, in Denmark, the ‘6-a-day’ worksite study implemented changes over an 8 month period among canteen staff of five workplaces, focusing on improving the taste and preparation of fruit and vegetables (Lassen et al., 2004). One year post-baseline, this pre-test/post-test study resulted in an average increase of approximately 1 serving of fruits and vegetables per day per participant.
Several studies have focused on providing tailored interventions to promote dietary changes for individual workers. For example, in the U.S., the Tools for Health study was conducted among construction laborers, and included tailored and targeted print materials as well as motivational-interviewing based telephone calls. This intervention resulted in a significant 1.5 serving increase in the intervention group, compared to a slight decrease (-0.09) in the control group. (Sorensen et al., 2007a). As another example, the U.S.-based “Alive” [A Lifestyle Intervention Via Email] was an automated program that promoted changes in multiple dietary behaviors among non-medical employees of a large healthcare organization using a series of emails tailored to individual and family factors (e.g., having children in the home) (Sternfeld et al., 2009). Over a 4-month follow-up, participants made several significant changes relative to the control group, including a 0.35 serving increase of fruits and vegetables, 0.75g decrease in saturated fat, and 0.29g decrease in trans-fat.
Other research has explored the role of worksite environmental changes to promote dietary changes by increasing access to healthy foods. While some studies have reported increased intake of fruit and vegetables, reduction in self-reported intake of fat and increased sales of healthy foods as a result of labeling or increased access to healthy foods, others have shown no dietary changes in relation to such environmental modifications (Matson-Koffman et al., 2005, Engbers et al., 2005). Reducing food prices may also contribute to dietary improvements. In two studies, French and colleagues found that reducing prices on healthful snacks in vending machines can increase sales of these snacks (French et al., 2001). For example, in the latter of these two studies, the effect of lowering the price and increasing the availability of healthy foods was tested in vending machines used by workers at four bus garages in the U.S (French et al., 2010). Using input from the employee advisory group, more healthful beverages, snacks, and entrees were increased to reach a benchmark of 50% of offerings in the healthy category. These targeted foods were priced 10% lower than their normal price. Compared to the no-intervention control group, garages in the intervention group increased sales of healthy items including snacks.
A growing literature is also exploring the efficacy of workplace interventions to support weight management or weight reduction for overweight or obese workers (Hennrikus and Jeffery, 1996); (Benedict and Arterburn, 2008). In a review of 11 randomized trials from 1995-2006, modest weight loss of -0.2 to -6.4kg was noted in intervention groups compared to control groups over a range of 2 – 18 month follow-up across studies ((Benedict and Arterburn, 2008). We briefly review three U.S. studies that have been conducted since this review. First, a study targeted to the physical and social environment of metropolitan transit workers, found a non-significant mean BMI change of -0.14, 18-months post baseline compared to workers in the garages in the control group (French et al., 2010). The authors concluded that worksite environmental interventions may be less effective when workers, such as bus drivers, mainly spend their workdays away from the worksite (French et al., 2010). Second, a pre-test/post-test trial with truck drivers included several components: team weight loss competitions, behavioral computer-based training, self-monitoring, and telephone coaching using motivational interviewing. The intervention resulted in a significant decrease in body weight of 7.8 lbs 6-months post baseline (Olson et al., 2009). Finally, an intervention for employees was conducted at six hospitals using strategies targeting the social and physical environment such as displaying print materials, working with the food service staff to increase offerings of healthful foods, and nutrition labeling at the cafeteria (Lemon et al., 2010). Results indicated no significant effects on BMI in intent-to-treat analyses, however, those who participated in more intervention events achieved a decrease in BMI (0.012 units) with each unit increase in participation (scale 0-100) after 2 years. Overall, these studies demonstrate the potential of worksite weight management interventions as well as the challenges, particularly in promoting a sufficient level of participation and exposure to intervention components. Clearly, further work is needed pertaining to long-term follow-up in randomized controlled trials (Benedict and Arterburn, 2008).
This diverse group of studies representing a range of workers and workplace settings point to several key intervention components, including providing ongoing maintenance and support for targeted changes, responding to workers’ day-to-day work experiences, addressing the social and physical workplace environment, and tailoring to individual factors using principles of behavioral theory (e.g. stage of change) (Prochaska et al., 1997). These factors are explored further in section 4.
3. Healthy eating in the context of the work environment
Workers’ dietary patterns are also likely to be influenced by other factors in the work environment. As illustrated in Figure 1, other workplace initiatives contributing to worker health may also spill over to influence workers’ dietary patterns. In addition to educational programming and policies to improve worker health behaviors such as diet, worksites may be engaged in efforts to prevent work-related illness and injury, reduce work-related stress, and expand work-related resources (Egerter et al., 2008).
Figure 1.
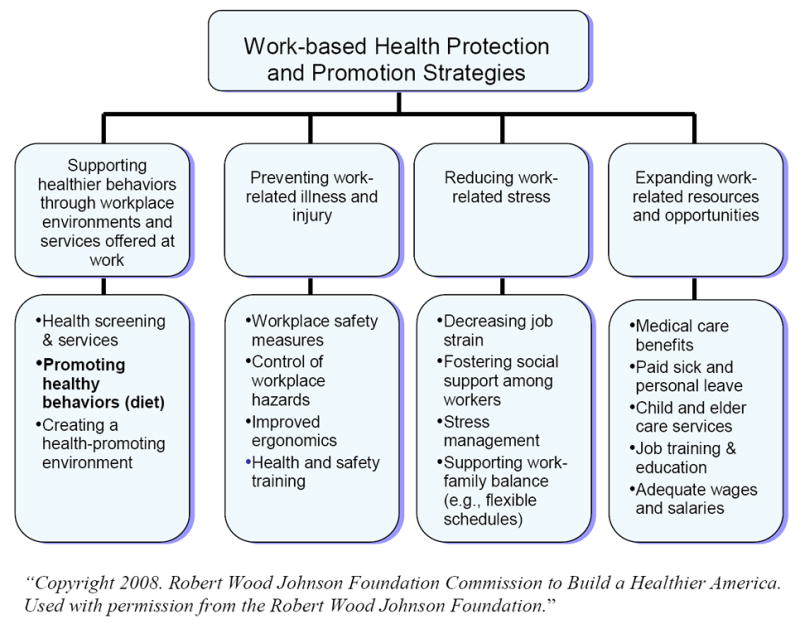
Framework of Strategies to Improve Healthy Eating through the Workplace
3.1 Preventing work-related injuries and illness
Although they focus on different pathways to worker health, occupational health and safety and worksite health promotion share the common aim of promoting worker health, with complementary functions in protecting and enhancing the health of workers. There is growing evidence that an integrated or coordinated approach across these parallel paths may contribute to enhanced effectiveness in promoting health behaviors as well as influencing the work environment (Sorensen and Barbeau, 2004, Institute of Medicine et al., 2005, Sorensen et al., 2002). This principle of integrating worksite health promotion and occupational health and safety is the underpinning of the WorkLife Initiative of the US National Institute of Occupational Safety and Health [I], and was recently endorsed by the US American Heart Association for cardiovascular health promotion (Carnethon et al., 2009).
The evidence for the effectiveness of this approach in improving diet and related outcomes is only beginning to emerge. One study testing an integrated approach to worker health within small manufacturing businesses found a significant effect on increasing fruit and vegetable consumption (Sorensen et al., 2005). In another study testing an integrated safety and health intervention for truck drivers, a reduction in body weight and significant improvements in safe driving were found (Olson et al., 2009). Two recent reviews have provided frameworks for this coordinating occupational safety and health interventions with those targeting obesity and nutrition behaviors. First, Schulte and colleagues provided a rationale for this focus in relation to obesity, concluding that there may be an association between obesity and workplace risks such as hazardous exposures on the job. For example, there is evidence to indicate that obesity may increase the risk of some occupational diseases, including musculoskeletal disorders, cardiovascular disease, and asthma. At the same time, these authors observed that workplace efforts to address both occupational hazards and obesity must take care that efforts do not result in blaming individual workers for their obesity (Schulte et al., 2007). Second, Reavley and colleagues described a systematic approach for bringing together key stakeholders (e.g., health educators, representatives from government, occupational health and safety officers) to develop a detailed logic model for the Australian WorkHealth Program. The model integrates the promotion of health behaviors, including nutrition and obesity, with safe work environments and ongoing quality improvement for the prevention and management of osteoarthritis (Reavley et al., 2010).
3.2 Addressing work-related stress and other organizational factors
Organizational factors in the work environment, such as work-related stress and work schedules, can also affect food choices and risk of obesity. In a large three-country analysis of the association between job strain and working overtime with food behaviors and obesity, although no significant relationships were found with the fully adjusted models for food behavior, working overtime was associated with obesity among women in London (Lallukka et al., 2008). Others have similarly reported the relationship of work schedule factors and psychosocial stressors to obesity, as well as other unhealthy behaviors such as heavy alcohol use and lack of exercise (Kivimaki et al., 2002, Siegrist and Rodel, 2006, Kouvonen et al., 2006). Work scheduling may influence dietary patterns through the pathway of sleep. For example, recent findings from a workplace study of mobile workers in the U.S. found that although low job strain, higher perceived job satisfaction and supervisor support were associated with more healthful sugary drink and/or snack intake, these effects were mediated by levels of adequate sleep, indicating the important role of sleep habits especially among workers with rotating schedules or shift work (Devine et al., 2003, Buxton et al., 2009). Additionally, qualitative evidence has underscored the relationship of work flexibility and the ability to manage work and family responsibilities to healthy eating strategies such as planning meals ahead of time and bringing fruit from home to work (Devine et al., 2003).
A strategy to address work conditions and limited time to prepare healthful meals is being evaluated in an ongoing Danish research project [II]. Canteen Takeaway is a program that assists worksites in establishing a service of making ready-to-heat meals available to employees for purchase at the worksite, for taking home as an evening meal. This study is investigating the potential impact of this program on the dietary patterns of employees and their families, as well as improvements in the healthiness of meals, the potential financial benefits for the employer, and the characteristics of workers who participate. For the worksite, this service may contribute to improving employees’ work-life balance, because it might reduce time needed for shopping, preparing, and cooking the meal and cleaning afterwards. A small study at a white collar worksite compared dietary intake on days in which canteen takeaway was and was not offered using four, 24-hour dietary recalls (Hansen et al., 2009). Initial data showed that intake of fruits and vegetables was higher (up to 220g, approximately 1-2 servings) on days in which canteen takeaway was offered for both men and women, but was only statistically significant for women.
3.3 Expanding work-related resources and benefits
In considering the impact of work on employee health and health behaviors, it is important to consider as well the role of the broad range of resources and benefits provided through employers. Workplace efforts in ensure adequate pay, provide training opportunities to increase opportunities for promotions, and expand job-related benefits, particularly for those from disadvantaged backgrounds, may bolster workplace health promotion efforts, including efforts to promote healthy eating. (Egerter et al., 2008). Efforts to reduce disparities in availability of the range of work-related resources may also include access to employee assistance programs (providing counseling referrals for substance abuse, financial, and legal difficulties) and workplace health promotion programs, which are is lower among workers who are blue-collar, lower paid, and part-time (Stoltzfus, 2006).
A variety of resources are increasingly available to address these disparities and improve workers’ access to these benefits. Examples of initiatives for increasing access to higher-ranking work can be drawn from federally-funded programs, such as the U.S. Jobs Corp [III] or non-profit organizations, such as the U.S. Year Up program [IV]. Year Up seeks to provide paid training opportunities with their corporate partners to young urban youth across 5 U.S. cities while also providing college credit. Finally, other organizations address issues related to work benefits and resources including improving workplace flexibility, helping family caregivers, and improving financial standing of workers. The non-profit research organization Families and Work Institute [V] is an example of a group that seeks to collect information about the interactions between work and family life and provide recommendations to act upon their findings.
4. Conceptual models to guide interventions and evaluations
A conceptual model based on established social and behavioral theories can provide a useful structure to guide the design, delivery and evaluation of workplace health promotion programs. We provide three examples of conceptual frameworks that inform intervention design at multiple levels.
4.1 Social Ecological Model
Social ecological models have a long-standing background, drawing from both public health and psychology fields. Social ecological models serve as a comprehensive framework to guide health behavior interventions and describe how health behaviors may be influenced by multiple levels, usually including individual factors (e.g. demographics, behaviors, cognitions), social environment (e.g. family, co-workers, friends), physical and organizational environment settings (e.g. worksites), and macro-level environments (e.g. societal values, food marketing) (Story et al., 2008). One of the early models of the interaction of multiple levels of change and individual behavior was described by Bronfenbrenner in 1979, in which interactions between social groups (e.g. family), various settings (e.g. school, work), and larger social systems (e.g. cultural beliefs) were described (Bronfenbrenner, 1979); later versions of this model emphasize the influence of multiple levels over the lifecourse and in successive generations (Bronfenbrenner, 2000). As noted in section 2.3, changes to the work environment can have a beneficial impact on healthy eating behaviors, including through food availability on-site (cafeteria, vending machines), nutrition labeling of these offerings, and visibility of promotional material (Story et al., 2008). In addition to articulating the multiple levels of influence on health behaviors, social ecological models also rely on additional core principals, including the assumptions that there are interactions among these levels of influence, that interventions across multiple levels are likely to be more effective, and that interventions should focus on specific behaviors (Sallis et al., 2008).
The Treatwell 5-a-Day study provides one example of an intervention relying on a social ecological model (Sorensen et al., 1999). In this study, 22 worksites were randomly assigned to one of three conditions: a minimal intervention control group; a worksite intervention group, which included a worksite-based intervention that promoted increased fruit and vegetable consumption through worker engagement, educational programming, and increased access to fruits and vegetables in the work setting; and a worksite-plus-family intervention group, which included the worksite-based intervention plus outreach efforts to workers’ families. This intervention illustrates the potential impact of multiple levels of influence, including educational efforts to build individual knowledge and attitudes, worksite environmental changes, and promotion of changes within the family. This study found significant between-group differences, with the worksite-plus-family intervention having the greatest impact on improvements in fruit and vegetable consumption corresponding to a 0.5 serving increase compared to the control group (Sorensen et al., 1999)
4.2 Social Contextual Model
The social contextual model was designed to guide intervention planning and evaluation by identifying social contextual factors that are amenable to change through interventions, and additional characteristics of the social context that may be important in informing intervention design. Specifically, the model delineates pathways through which population characteristics, such as income or occupation, influence health behaviors such as diet. By illuminating these pathways that reflect the realities of people’s day-to-day life experiences, the intention of the model is to improve the design of interventions by increasing their relevance to their intended audiences. This framework distinguishes between modifying conditions, that is, factors that independently impact on outcomes but which are not influenced by the intervention, and mediating mechanisms, which can be modified by the intervention. Social context, including life experiences, social relationships, organizational structures and societal influences, may function as either modifying conditions or mediating mechanisms, depending on their location within or outside the causal pathway between the intervention and the outcomes (Sorensen et al., 2003). Designing (Sorensen et al., 2004a, Stoddard et al., (in review), Sorensen et al., 2005) interventions that are responsive to both mediating and modifying conditions has been shown to promote beneficial changes in eating behaviors and to address disparities by race/ethnicity (Emmons et al., 2005) and occupation (Sorensen et al., 2005).
The Healthy Directions-Small Business study used the Social Contextual Model to design an intervention targeting dietary patterns and physical activity among low-income, multi-ethnic workers in 26 manufacturing industries (Sorensen et al., 2005). For example, recognizing that workers may live in a neighborhood with limited access to supermarkets selling affordable fruits and vegetables, intervention programming was responsive to this condition by working with management to establish policies for offering healthy food options at the workplace. Stratifying the analyses by occupational class, findings revealed a significant improvement in fruit and vegetable consumption among workers, although not among managers. Further analyses explored the role of the social context on changes in fruit and vegetable consumption, and found that key social contextual factors at the individual and interpersonal levels were significantly associated with increased fruit and vegetable intake, including being born outside the U.S., more social ties, and supportive social norms (Sorensen et al., 2007b).
4.3 Political Process Approach
The Political Process Approach, also integrates organizational context and has been applied to workplace health promotion, including efforts to increase the consumption of fruits and vegetables at worksites (Thorsen et al., 2005). According to this approach, worksite health promotion can also be seen as a worksite change process. Where the Social Contextual Model highlights social-contextual factors at the organizational level among other levels, the Political Process Approach emphasizes the political processes that occur in the workplace organization. When planning or assessing the effects of worksite health promotion, it is important to be aware of the political processes that shape worksite norms, values, and patterns of conflict and consensus. Existing social compromises may develop over time, resulting in social norms and values, also termed ‘stiffened politics,’ implying that these norms and values are no longer questioned in the daily practice of the worksite (Kamp, 2000). The underlying principles behind these norms and values are called the “social constitution” of the worksite (Hildebrandt and Selz, 1989). This term was developed by the German industrial sociologists Hildebrandt and Seltz, in 1989 to challenge the technical and economic models predominant at the time. Political processes occur when the social constitution is put under pressure. For example, resistance to planned health promotion programs may occur when they are viewed as exerting control over what has been seen as private health behaviors such as weight, smoking habits, or freedom to choose unhealthy food in the canteen (Olsen, 1994). When planning such programs, it is important to be aware of these worksite-specific norms and values and related social practices, and recognize the need for addressing these norms and values as part of the planning, for example through involving employee representatives (Thorsen et al., 2005).
5. Discussion
As this paper describes, the workplace offers considerable promise in playing a part in promoting worker health through improvements in dietary patterns and weight management. Worksite health promotion approaches have also been recommended internationally. For example, the World Health Organization 2004 report, “Global Strategy on Diet, Physical Activity and Health,” endorsed workplaces as “important settings for health promotion and disease prevention. People need to be given the opportunity to make healthy choices in the workplace in order to reduce their exposure to risk…Workplaces should make possible healthy food choices…” (World Health Organization, 2004). The European Network for Workplace Health Promotion has issued a number of statements of common goals and recommendations for workplace health promotion, including the Luxemburg Declaration on Workplace Health Promotion in the European Union, the Lisbon Statement on Workplace Health in Small and Medium-Sized Enterprises, and the Barcelona Declaration on Developing Good Workplace Health Practice in Europe [VI].
5.1. Implications for best practice
Sets of ‘best practices’ have been proposed by several organizations; assessing research studies according to a standard list of best practices for workplace health promotion provides a more complete understanding of different study components and offers a point of comparison between studies. For example, the U.S. National Institute of Occupational Safety and Health has established a set of essential elements to guide programs and policies for workplace health promotion [VII]. These essential elements are divided into four sections: 1) organizational culture and leadership, which includes linking program and business objectives and obtaining management support; 2) program design, which includes building integrated systems, using effective communication, promoting worker participatory strategies, tailoring to the needs of the specific workplace, using incentives/rewards, and planning for sustainability; 3) program resources, including implementing incremental start-up plans, providing adequate staffing, budget, and resources, and being accountable for program and outcomes; and 4) program evaluation, which includes checking for and carrying out corrective action using feedback loops. The conceptual models we reviewed in Section 4 also provide guidance for implementing programs across levels, including programs for individual workers (such as targeting across the stages of change, using goal setting, and building self-efficacy for change) and programs that seek to change or recognize the social environment, work conditions, and the physical environment. While the use of best practices such as these are available to guide workplace health promotion efforts, further work is needed to identify barriers and facilitators to using best practices so that effective programs can be more broadly disseminated.
5.2 Implications for future research
The research examples provided throughout this paper illustrate effective approaches that have been undertaken to address healthy eating in the workplace and establish evidence for intervention efficacy. Further research is needed to explore the linkages between health promotion efforts for individual workers and efforts to improve the organizational, physical and social environments at work. Strengthening these linkages could serve to maximize the impact of change within a multi-level program. Furthermore, in light of documented disparities in dietary patterns by socio-demographic characteristics such as racial/ethnic groups and occupational classes (U.S. Department of Health and Human Services, 2000, Thompson et al., 2009, Kant et al., 2007, Thane et al., 2007), continued research is needed to identify and understand relevant social contextual variables in order to improve strategies to encourage healthy eating behaviors in the workplace. In addition, research is needed to identify best processes for sustaining and disseminating effective programs, in order to assure the ongoing impact of these efforts.
Acknowledgments
Our thinking on this topic has been greatly informed by our collaborators, among them, Elizabeth Barbeau, Karen Emmons, Elizabeth Harden, Mary Kay Hunt, Anthony LaMontagne, Deborah McLellan, Anne Stoddard, Lorraine Wallace, and Gregory Wagner, and by the worksites and labor unions collaborating on our research. We additionally appreciate the support of a grant from Liberty Mutual, Inc, and funding from the National Cancer Institute (1K05 CA108663).
Biographies
Lisa Quintiliani, Ph.D., R.D., is a post-doctoral fellow in the Medical Informatics program at Boston University Medical Center in Boston, MA, USA. She has a background in public health and dietetics, completing a Cancer Prevention Fellowship Program at the Harvard School of Public Health and the Dana-Farber Cancer Institute, Boston MA. Dr. Quintiliani earned a Ph.D. in Nutrition from the University of North Carolina at Chapel Hill, NC, USA.
Signe Poulsen, M.Sc. in management engineering, is a Ph.D.-student at the Technical University of Denmark. As part of her Ph.D.-program she is visiting the Dana-Farber Cancer Institute for 4 months (spring 2010).
Dr. Glorian Sorensen is Professor of Society, Human Development, and Health in the Harvard School of Public Health and Director of the Dana-Farber’s Center for Community-Based Research. Her research has tested the efficacy of worksite interventions across a range of settings.
Footnotes
Contributor Information
Lisa Quintiliani, Boston University Medical Center, General Internal Medicine, Boston MA USA, lmquinti@bu.edu, Phone: 01-617-638-2740.
Signe Poulsen, Technical University of Denmark, Department of Management Engineering, Section for Innovation and Sustainability, sipo@man.dtu.dk, Phone: 45-4525-6070; 01-617-582-7461.
Dr. Glorian Sorensen, Harvard School of Public Health, Department of Society, Human Development and Health and Dana-Farber Cancer Institute, Center for Community-Based Research, Boston MA USA, Glorian_sorensen@dfci.harvard.edu, Phone: 01-617-632-2183
References
- American Institute for Cancer Research. Food, nutrition and the prevention of cancer: A global perspective. Washington, DC: World Cancer Research Fund, American Institute for Cancer Research; 2007. [DOI] [PubMed] [Google Scholar]
- Benedict MA, Arterburn D. Worksite-based weight loss programs: a systematic review of recent literature. American Journal of Health Promotion. 2008;22:408–16. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- Beresford SAA, Thompson B, Feng Z, Christianson A, Mclerran D, Patrick DL. Seattle 5-A-Day worksite program to increase fruit and vegetable consumption. Preventive Medicine. 2001;32:230–238. doi: 10.1006/pmed.2000.0806. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Bronfenbrenner U. In: Encyclopedia of Psychology. Kazdin AE, editor. Washington DC: American Psychological Association; 2000. [Google Scholar]
- Buller DB, Morrill C, Taren D, Aickin M, Sennott-Miller L, Buller MK, Larkey L, Alatorre C, Wentzel TM. Randomized trial testing: The effect of peer education at increasing fruit and vegetable intake. Journal of the National Cancer Institute. 1999;91:1491–1500. doi: 10.1093/jnci/91.17.1491. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Quintiliani LM, Yang MH, Ebbeling CB, Stoddard AM, Pereira LK, Sorensen G. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. American Journal of Public Health. 2009;99(Suppl 3):S636–43. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, Mclerran D, Turner-Mcgrievy G, Feng Z, Havas S, Sorensen G, Buller D, Beresford SA, Nebeling L. Mediation of adult fruit and vegetable consumption in the National 5 A Day for Better Health community studies. Annals of Behavioral Medicine. 2008;35:49–60. doi: 10.1007/s12160-007-9002-y. [DOI] [PubMed] [Google Scholar]
- Carnethon M, Whitsel LP, Franklin BA, Kris-Etherton P, Milani R, Pratt CA, Wagner GR. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120:1725–41. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- Devine CM, Connors MM, Sobal J, Bisogni CA. Sandwiching it in: Spillover of work onto food choices and family roles in low- and moderate-income urban households. Social Science Medicine. 2003;56:617–630. doi: 10.1016/s0277-9536(02)00058-8. [DOI] [PubMed] [Google Scholar]
- Egerter S, Dekker M, An J, Grossman-Kahn R, Braveman P. Work Matters for Health. Robert Wood Johnson Foundation Commission to Build a Healthier America. 2008;(Brief 4: Worker Health) [Google Scholar]
- Emmons KM, Stoddard AM, Fletcher R, Gutheil C, Suarez EG, Lobb R, Weeks JC, Bigby JA. Cancer prevention among working-class, multi-ethnic adults: Results of the Healthy Directions Health Centers Study. American Journal of Public Health. 2005;95:1200–1205. doi: 10.2105/AJPH.2004.038695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engbers LH, Van Poppel MN, Chin APMJ, Van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. American Journal of Preventive Medicine. 2005;29:61–70. doi: 10.1016/j.amepre.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Flay BR. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Preventive Medicine. 1986;15:451–474. doi: 10.1016/0091-7435(86)90024-1. [DOI] [PubMed] [Google Scholar]
- French SA, Hannan PJ, Harnack LJ, Mitchell NR, Toomey TL, Gerlach A. Pricing and availability intervention in vending machines at four bus garages. Journal of Occupational and Environmental Medicine. 2010;52(Suppl 1):S29–33. doi: 10.1097/JOM.0b013e3181c5c476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Jeffery RW, Story M, Breitlow KK, Baxter JS, Hannan P, Snyder MP. Pricing and promotion effects on low-fat vending snack purchases: the CHIPS Study. American Journal of Public Health. 2001;91:112–7. doi: 10.2105/ajph.91.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sorensen G, Farmer A. The health impact of worksite nutrition and cholesterol intervention programs. American Journal of Health Promotion. 1996;10:453–470. doi: 10.4278/0890-1171-10.6.453. [DOI] [PubMed] [Google Scholar]
- Hansen G, Lassen AD, Ernst L, Poulsen S. Proceedings for Better Food at Work - the Nordic and Baltic Experience. Aalborg University; 2009. New possibilities in influencing eating patterns through healthier canteen take away. [Google Scholar]
- Hennrikus DJ, Jeffery RW. Worksite intervention for weight control: A review of the literature. American Journal of Health Promotion. 1996;10:471–498. doi: 10.4278/0890-1171-10.6.471. [DOI] [PubMed] [Google Scholar]
- Hildebrandt E, Selz R. Wandel betrieblicher Sozialverfassung durch systemische Kontrolle? Die Einführung computergestützter Produktionsplanungs- und Steurungssysteme im bundesdeutschen Maschinenbau. In English: Transformation of the ‘social constitution’ of firms by systemic control? The introduction of computerized production planning and control systems in the West German machine building industry. Berlin: 1989. [Google Scholar]
- Institute of Medicine, Committee to Assess Worksite Preventive Health Program Needs for Nasa Employees & Food and Nutrition Board. Integrating employee health: A model program for NASA. Washington, DC: Institute of Medicine, National Academies Press; 2005. [Google Scholar]
- Janer G, Sala M, Kogevinas M. Health promotion trials at worksites and risk factors for cancer. Scandinavian Journal of Work Environment and Health. 2002;28:141–157. doi: 10.5271/sjweh.658. [DOI] [PubMed] [Google Scholar]
- Kamp A. Breaking up old marriages: The political process of change and continuity at work. Technology Analysis & Strategic Management. 2000;12:75–90. [Google Scholar]
- Kant AK, Graubard BI, Kumanyika SK. Trends in black-white differentials in dietary intakes of U.S. adults, 1971-2002. American Journal of Preventive Medicine. 2007;32:264–272. doi: 10.1016/j.amepre.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimaki M, Leino-Arjas P, Luukkonen R, Riihimaki H, Vahtera J, Kirjonen J. Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. British Medical Journal. 2002;325:857. doi: 10.1136/bmj.325.7369.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouvonen A, Kivimaki M, Virtanen M, Heponiemi T, Elovainio M, Pentti J, Linna A, Vahtera J. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. doi: 10.1186/1471-2458-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lallukka T, Lahelma E, Rahkonen O, Roos E, Laaksonen E, Martikainen P, Head J, Brunner E, Mosdol A, Marmot M, Sekine M, Nasermoaddeli A, Kagamimori S. Associations of job strain and working overtime with adverse health behaviors and obesity: evidence from the Whitehall II Study, Helsinki Health Study, and the Japanese Civil Servants Study. Social Science and Medicine. 2008;66:1681–98. doi: 10.1016/j.socscimed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- Lassen A, Thorsen AV, Trolle E, Elsig M, Ovesen L. Successful strategies to increase the consumption of fruits and vegetables: results from the Danish ‘6 a day’ Work-site Canteen Model Study. Public Health Nutrition. 2004;7:263–70. doi: 10.1079/PHN2003532. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, Andersen V, Borg A, Hale J. Step ahead a worksite obesity prevention trial among hospital employees. American Journal of Preventive Medicine. 2010;38:27–38. doi: 10.1016/j.amepre.2009.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson-Koffman DM, Brownstein JN, Neiner JA, Greaney ML. A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: What works? American Journal of Health Promotion. 2005;19:167–193. doi: 10.4278/0890-1171-19.3.167. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Final Report. 2002 [PubMed] [Google Scholar]
- Olsen P. Inerti og bevægelse nye perspektiver på arbejde og politik i den industrielle virksomhed. Lyngby: Institut for Arbejdsmiljø, DTH. Peter Olsen og Chr. Clausen; UAb950501. English: Inertia and Movement - New perspectives on work and politics in the industrialized enterprise 1994 [Google Scholar]
- Olson R, Anger WK, Elliot DL, Wipfli B, Gray M. A new health promotion model for lone workers: results of the Safety & Health Involvement For Truckers (SHIFT) pilot study. Journal of Occupational and Environmental Medicine. 2009;51:1233–46. doi: 10.1097/JOM.0b013e3181c1dc7a. [DOI] [PubMed] [Google Scholar]
- Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: update VII 2004-2008. Journal of Occupational and Environmental Medicine. 2009;51:822–37. doi: 10.1097/JOM.0b013e3181a7de5a. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding C, Evers K. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- Reavley N, Livingston J, Buchbinder R, Bennell K, Stecki C, Osborne RH. A systematic grounded approach to the development of complex interventions: the Australian WorkHealth Program--arthritis as a case study. Social Science and Medicine. 2010;70:342–50. doi: 10.1016/j.socscimed.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. Jossey-Bass; 2008. [Google Scholar]
- Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM, Luster M, Munson AE, O’callaghan JP, Parks CG, Simeonova PP, Miller DB. Work, obesity, and occupational safety and health. American Journal of Public Health. 2007;97:428–36. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J, Rodel A. Work stress and health risk behavior. Scandinavian Journal of Work, Environment and Health. 2006;32:473–81. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E. Steps to a healthier US workforce: Integrating occupational health and safety and worksite health promotion: State of the science. Steps to a Healthier US Workforce Symposium; Washington, DC. National Institute for Occupational Safety and Health; 2004. [Google Scholar]
- Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: A social contextual model for reducing tobacco use among blue-collar workers. American Journal of Public Health. 2004a;94:230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Goldman R, Smith A, Brennan AA. Tools for Health: The efficacy of a tailored intervention targeted for construction laborers. Cancer Causes & Control. 2007a;18:51–59. doi: 10.1007/s10552-006-0076-9. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau EM, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working class, multi-ethnic workers: Results of the Healthy Directions - Small Business Study. American Journal of Public Health. 2005;95:1389–95. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Emmons K, Hunt MK, Barbeau E, Goldman R, Peterson K, Kuntz K, Stoddard A, Berkman L. Model for incorporating social context in health behavior interventions: applications for cancer prevention for working-class, multiethnic populations. Preventive Medicine. 2003;37:188–97. doi: 10.1016/s0091-7435(03)00111-7. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Linnan L, Hunt MK. Worksite-based research and initiatives to increase fruit and vegetable consumption. Preventive Medicine. 2004b;39:S94–S100. doi: 10.1016/j.ypmed.2003.12.020. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, Dubowitz T, Barbeau EM, Berkman LF, Peterson KE. The influence of social context on changes in fruit and vegetable consumption: Results of the Healthy Directions Studies. American Journal of Public Health. 2007b;97:1216–1227. doi: 10.2105/AJPH.2006.088120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, La Montagne A, Emmons K, Hunt MK, Youngstrom R, Mclellan D, Christiani DC. A comprehensive worksite cancer prevention intervention: behavior change results from a randomized controlled trial (United States) Cancer Causes & Control. 2002;13:493–502. doi: 10.1023/a:1016385001695. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, Peterson K, Cohen N, Hunt MK, Stein E, Palombo R, Lederman R. Increasing fruit and vegetable consumption through worksites and families in the treatwell 5-a-day study. American Journal of Public Health. 1999;89:54–60. doi: 10.2105/ajph.89.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparling P. Worksite health promotion: principles, resources, and challenges. Preventing Chronic Disease. 2010;7:A25. [PMC free article] [PubMed] [Google Scholar]
- Sternfeld B, Block C, Quesenberry CP, Jr, Block TJ, Husson G, Norris JC, Nelson M, Block G. Improving diet and physical activity with ALIVE: a worksite randomized trial. American Journal of Preventive Medicine. 2009;36:475–83. doi: 10.1016/j.amepre.2009.01.036. [DOI] [PubMed] [Google Scholar]
- Stoddard AM, Krieger N, Barbeau EM, Bennett G, Fay ME, Sorensen G, Emmons K. Recruiting a multi-ethnic working-class study samples: Baseline characteristics of Healthy Directions Study participants. in review. [Google Scholar]
- Stoltzfus E. Emerging benefits: Access to health promotion benefits in the United States, private industry, 1999 and 2005. Washington, DC: US Department of Labor, Bureau of Labor Statistics; 2006. [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annual Reviews of Public Health. 2008;29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Thane CW, Jones AR, Stephen AM, Seal CJ, Jebb SA. Comparative whole-grain intake of British adults in 1986-7 and 2000-1. British Journal of Nutrition. 2007;97:987–92. doi: 10.1017/S0007114507659078. [DOI] [PubMed] [Google Scholar]
- Thompson FE, Mcneel TS, Dowling EC, Midthune D, Morrissette M, Zeruto CA. Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in adults in the United States: National Health Interview Survey, 2005. Journal of the American Dietetic Association. 2009;109:1376–83. doi: 10.1016/j.jada.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsen AV, Jorgensen MS, Lassen A, Mikkelsen BE. Strategies to promote healthier eating at worksites - analysis of experiences from a social shaping perspective. Proceedings from the Fifth International Conference on Culinary Art and Sciences, Global and National Perspectives; Bournemouth University. 2005. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010: Understanding and improving health and objectives for health. 2. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. 2004 Http://Www.Who.Int/Dietphysicalactivity/Strategy/Eb11344/En/Index.Html.


