Abstract
Introduction:
Radical surgery is the “gold standard” for treatment of invasive penile carcinoma but very poor aesthetic, functional and psychological outcomes have been reported. Our purpose was to assess the impact of organ potency-sparing surgery in locally confined carcinoma of the penis.
Materials and Methods:
We evaluated retrospectively 42 patients with early penile cancer (Ta,T1,T2), treated with glandulectomy and glanduloplasty with urethral mucosa and sparing of cavernosal apexes, or glandulectomy and limited apical resection in cases of Stage T2. Sexual function, ejaculation and libido were evaluated with an IIEF-15 questionnaire before the appearance of neoplasia (about three months before the surgery) and six months after surgery. Quality of life was evaluated by the Bigelow-Young questionnaire. The scores relating to two weeks prior to the surgery have been compared to those obtained six months after surgery. The statistical analysis was conducted using t-Student for repeated measures and analysis of variance.
Results:
Six months after surgery 73% of patients reported spontaneous rigid erections, 60% coital activity while 76% of the group treated with urethral glanduloplasty reported normal ejaculation and orgasm, regained an average of 35 days after surgery. The average IIEF-15 scores reported in the entire series in the domains of erection, libido and coital activity of the pre-cancer period were not statistically different than those recorded six months after surgery. In the group treated with glandular reconstruction, pre-and postoperative IIEF-15 mean scores related to ejaculation and orgasm domains were not significantly different. Mean scores of Bigelow-Young questionnaires related to sexual pleasure, familial, social and professional relationships showed significant improvement after surgery.
Conclusions:
Potency sparing-sparing surgical treatments have a positive impact on a wide spectrum of the patient's life including family relationships, and social and working conditions.
Keywords: Organ potency-sparing surgery, penile cancer, penile cancer treatment, penile carcinoma, sexual outcomes
INTRODUCTION
Radical surgery is the “gold standard” for the treatment of the primary lesion of penile carcinoma. The conventional surgery includes penectomy with a radical or partial amputation. These procedures allow an excellent local control of disease, with a 6% recurrence rate for partial penectomy. In the absence of lymph node metastasis, these procedures are associated with a five-year survival in 80% of cases.[1]
However, the conventional surgery has given poor aesthetic, anatomical and functional results, and this dramatically influences patients’ quality of life. The psychological complications may include anxiety, depression and poor acceptance of disability.[2,3,4]
The major surgical complications include: difficulties in urination whilst standing, impaired sexual function, and an appearance of distal urethral stenosis in 20% of cases, which require a second surgery in 8% of cases.[5]
Modern guidelines for early-stage tumors prescribe conservative “penile-sparing” techniques, which include the dissection of the glans from the cavernosal apexes with a full excision of small tumors localized on the glans or prepuce.[6,7] The length and shape of the penis are therefore maintained inducing less of an emotional impact than radical surgery, with the recovery of coital function in most cases.[8] The reconstruction of penile anatomy and function after demolitive surgery should therefore be mandatory. This, however, represents a yet unsolved challenge.
Most authors reported confusing results about techniques of glandectomy and penile-sparing surgery without glans reconstruction.[9,10,11,12]
Potency-sparing techniques include reconstructive glanduloplasty using split-thickness skin grafts, buccal mucosa or scrotal flaps which have been carried out to restore both the anatomic and aesthetic appearance of the penis.[13,14,15,16]
All of these procedures only partially solve aesthetic and psychological problems but, for the most part, the patient completely loses sensibility and consequently the ability to achieve ejaculation and orgasm. Furthermore, penile length and appearance are definitively compromised. With the original technique of urethral glanduloplasty, satisfactory functional and sexual outcomes such as the restoration of erection, sensibility in the area of the neoglans and ejaculation have been reported.[17] (Please check this retains your original meaning)
Many studies have been carried out on the global, clinical, and psychological outcomes of surgery in penile carcinoma[18] without any distinction between conservative and demolitive techniques. Furthermore, few papers have reported on sexual outcomes related to conservative and reconstructive surgical techniques.
The purpose of this study was to evaluate the psychological and sexual outcomes and the quality of life related to the original technique, consisting of organ potency-sparing surgery and glans reconstruction with distal urethra in patients affected by locally confined carcinoma of the penis.
MATERIALS AND METHODS
Patients
Forty-two patients (mean age 56 years) with penile cancer clinically confined (Ta, T1, T2) were prospectively evaluated. All patients were white Caucasians, with no serious concurrent psychological or physical illnesses. Thirty-eight out of 42 patients (90.4%) enrolled in the study had a high-school degree or higher education and belong to the middle or upper class [Table 1].
Table 1.
Demographics
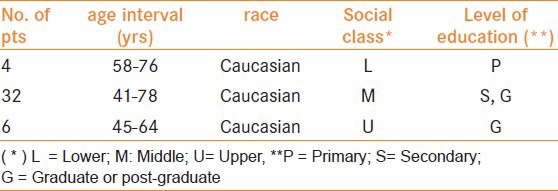
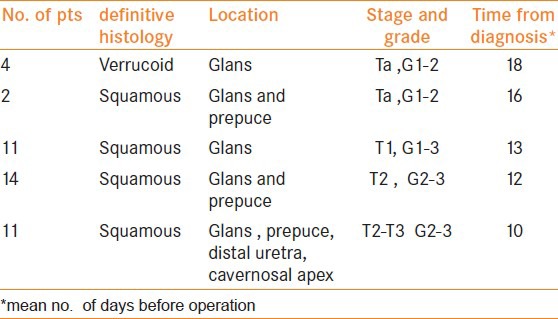
Treatment strategies included diathermocoagulation in six cases with superficial lesions, glandulectomy and glanduloplasty with urethral mucosa and the sparing of cavernosal apexes in 25 cases, and glandulectomy and limited apical resection in 11 cases of Stage T2. Oncological issues of this series have been summarized in Table 2.
Table 2.
Tumor characteristics
Inguinal lymphadenectomy according to Catalona's technique was carried out in all the patients staged T2-T2 or G3, either during demolitive surgery or as a second delayed operation after assessment of definitive histology.
Surgical technique of glans reconstruction
Glans has been carefully dissected from cavernosal apexes and from distal urethra and removed “en-bloque” with the neuro-vascular bundle. Saving cavernosal apexes allowed the physician to perform a potency-sparing technique, thanks to the preservation of adequate penile length for coital function. Histological margins of cavernosal apexes and distal urethra have been intraoperatively checked.
Glandular reconstructive urethroplasty included a full dissection and mobilization of the whole penile urethra from the ventral corpora cavernosa from the apexes as far as the base of the penile shaft, in order to obtain a uretrhal stump at least 3 cm longer than the cavernous bodies. Subsequently, the ventral part of the urethra was longitudinally sectioned for 3 cm and shaped to cover the cavernosal apexes, tying the mucosa over the dorsal side of penile albuginea [Figure 1]. Urethral margins were fixed to the corpora cavernosa apexes by 3/0 absorbable sutures and the penile skin was sutured to the corpora cavernosa at a distance of 1 cm from the margin of the neoglans. This was a decision to widen the area of the neoglans by the growth and migration of urethral epithelium that would have occurred completely, 30 days after the operation. Finally, the urethral neomeatus was sutured to the penile skin ventrally and a bladder catheter was left for five days.
Figure 1.

The neoglans is created by positioning distal urethra in the distal part of the cavernosal apexes
Data Collection
Potential participants received invitation letters, detailed information sheets and consent forms. Patients participated only if they so desired; informed consent was obtained one to two days before the surgery. Participants were interviewed individually within the Urology Department.
Sexual functions, such as erection, ejaculation and libido were evaluated with an IIEF-15 questionnaire relating to: before the appearance of the neoplasia (about three months before the surgery), two weeks before surgery and six months after surgery. Quality of life was evaluated through Bigelow's questionnaire[19] in the same clinical periods.
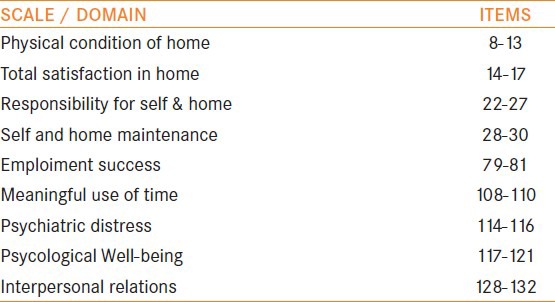
This is a clinical tool [Table 3] which has been widely tested, has good face validity and is clinically informative for use with mentally ill patients. It is sensitive enough to discriminate between mental health and non-mental health community residents and has been used in several treatment evaluation studies. The questionnaire included questions relating to unpleasant feelings, familial and social relationships, and quality of work. The scores relating to two weeks before the surgery have been compared to those obtained six months after surgery.
Table 3.
Bigelow's questionnaire
Statistical analysis
Statistical analysis was conducted using t-Student for repeated measures for continuous variables and analysis of variance for logical variables. P value < 0.05 has been considered as significant.
RESULTS
Six months after surgery 31/42 patients (73%) reported spontaneous rigid erections, 25/42 (60%) reported coital activity while 19/25 (76%) of the group treated with glans reconstruction (urethral glanduloplasty) reported normal ejaculation and orgasm, regained an average of 35 days after surgery [Table 4, right column]. Thirty out of 42 patients (71%) reported scores related to libido comparable to those before disease.
Table 4.
IIEF-15 score assessed before penile cancer disease and six months after surgical treatment

The average scores in the entire study were as follows: before the appearance of neoplasia (about three months before the surgery), the IIEF-15 scores for erection, ejaculation, orgasm and libido were 20, 5, 11, and 9 respectively. These were not significantly different (i.e. P > 0.05) to those recorded two weeks before the surgery, which were: 21, 5, 13, and 8 respectively [Table 5].
Table 5.
Quality of life questionnaire scores evaluated before and during disease and six months after surgery. (*p<0.05)
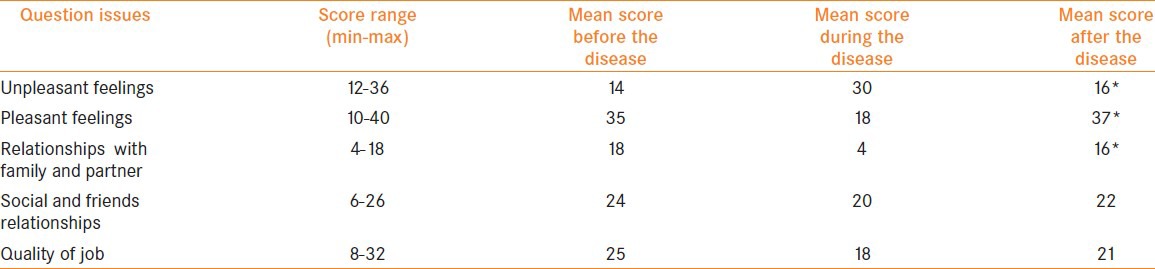
Mean scores on Bigelow's quality of life questionnaire (relating to sexual pleasure, familial, social and professional relationships) showed a significant improvement at 6 months after surgery from those at 2 weeks before surgery (P<0.01). In particular, scores relating to unpleasant feelings decreased from 30 to 16 (P < 0.01), sexual pleasure scores increased from 18 to 37 (P < 0.01), familial and partner relations also improved (4 to 16) (P < 0.01). No significant difference was recorded in the domains relating to friend relationships and professional quality whose scores increased from 20 to 22 (P < 0.05) and 18 to 21 (P > 0.05).
DISCUSSION
Penile cancer and its treatment can affect sexual function, psychological well-being, quality of life, and may also result in post-traumatic stress disorder.
One of the major handicaps in evaluating sexual outcomes after penile surgery is the lack of standardization of clinical data. The majority of studies used retrospective data collection from a small number of patients in single units, using different measuring tools. In addition, the study tools differed by administration, interview and semi-structured interview.
An early systematic review of the quality of life (psychosexual and psychosocial) literature in penile cancer has considered 6 of 437 studies on this issue.[18] Authors have reported an overall impact on patients’ wealth in up to 40% and psychological symptoms in approximately 50%, with signs of post-traumatic stress disorder in almost the same proportion.
Specifically, in 6 studies reviewed by authors, 13 different quantitative tools were used to assess psychological wealth. The Hospital Anxiety and Depression Score (HADS) demonstrated pathological anxiety in up to 31% of patients.[18] Ficarra[20] used the Diagnostic and Statistical Manual of Mental Disorders of psychiatric illness (DSM III-R) pointing out a rate of mental illness in 53%, avoidance behavior in 25% and impaired wealth in 40%.
The IIEF-15 was the most common tool used to assess sexual function. The results varied from 36% with no sexual function in one study, to 67% in another reporting reduced sexual satisfaction, to 78% reporting high confidence with erections in yet another.[18]
The glans-sparing technique has been documented in 12 patients:[21] for all of whom sexual desire was “high/very high”. The cosmetic results were “satisfying/very satisfying” in 83% patients.
Patients need therefore to be supported externally (via partners, family and friends) and internally (via life experiences). Wives, ex-wives and girlfriends should be involved in such a rehabilitation program in order to give emotional and practical support.
Currently, no sufficient help is offered in terms of screening for depression or anxiety in penile cancer patients. Support from professionals is extremely important. Positive responses included gratitude for the rapidity of surgery, removal of unpleasant symptoms and relief of initial anxiety. Frequent follow-up appointments were appreciated as they provided reassurance of swift intervention in any recurrence.
The modern approach to penile carcinoma should be a compromise between oncological safety and functional preservation. In our experience (experiment), glans reconstructive urethroplasty has shown clear long-term anatomical and functional advantages if compared to standard therapies for penile carcinoma: postoperative IIEF scores have demonstrated recovery of sexual function to that of before the onset of disease, including rigid erection, libido and ejaculation, with operative time not significantly longer than the simple amputation (mean: 35 min). The quality of life of patients after the operation in terms of quality of job, familial and partner relationships, and sexual pleasure was satisfactory.
It was surprising that the ejaculatory reflex was restored in the majority of our patients. The new arising concept is that thermal and tactile vibratory stimulation of the urethral mucosa of the neoglans can activate ejaculatory and orgasmic pathways during sexual activity and some investigational reports seem to support this hypothesis.[22,23,24] Thus far, no published surgical technique for penile carcinoma has exhibited a full recovery of sexual functions.
CONCLUSIONS
Our study indicates that sexual-sparing surgical treatments have a positive impact in a multitude of ways on a patient's life including familial relationships, and social and working conditions. These treatments allow the patient to obtain both cancer eradication and anatomical-psychological integrity, to preserve body image and to restore complex mechanisms such as erection and ejaculation.
A rehabilitation program incorporating psycho-sexual counseling is also needed. The role of women and the centrality of wives in supporting men's health in general, and in penile cancer in particular, is also very important.
Furthermore it is necessary to identify adequate tools to measure and identify psychological and sexual dysfunction in this group of patients.
Well designed multicentre studies are therefore needed to improve the global management of patients with penile cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McDougal WS, Kirchner FK, Jr, Edwards RH, Killion LT. Treatment of carcinoma of the penis: The case for primary lymphadenectomy. J Urol. 1986;136:38–41. doi: 10.1016/s0022-5347(17)44718-5. [DOI] [PubMed] [Google Scholar]
- 2.Ficarra V, Mofferdin A, D’Amico G. Comparison of the quality of life of patients treated by surgery or radiotherapy in epidermoid cancer of the penis. Prog Urol. 1999;9:715–20. [PubMed] [Google Scholar]
- 3.D’Ancona CA, Botega NJ, Moraes C, Lavoura NS, Jr, Santos JK, Rodrigues Netto N, Jr, et al. The quality of life after penectomy for penile carcinoma. Urology. 1998;50:593–6. doi: 10.1016/s0090-4295(97)00309-9. [DOI] [PubMed] [Google Scholar]
- 4.Opjordsmoen S, Waehre H, Aass N, Fossa SD. Sexuality in patients treated for penile cancer: Patients’ experience and doctors’ judgement. Br J Urol. 1994;73:554. doi: 10.1111/j.1464-410x.1994.tb07643.x. [DOI] [PubMed] [Google Scholar]
- 5.Blandly JP. Operative urology. 2 ed. Oxford: Blackwell Scientific hbI; 1986. [Google Scholar]
- 6.Bissada NK, Yakout HH, Fahmy WE, Gayed MS, Touijer AK, Greene GF, et al. Multi-institutional long-term experience with conservative surgery for invasive penile carcinoma. J Urol. 2003;169:500–2. doi: 10.1097/01.ju.0000043808.58188.52. [DOI] [PubMed] [Google Scholar]
- 7.Davis JW, Schellammer PF, Schlossberg SM. Conservative surgical therapy for penile and urethral carcinoma. Urology. 1999;53:386–92. doi: 10.1016/s0090-4295(98)00483-x. [DOI] [PubMed] [Google Scholar]
- 8.Gotsadze D, Matveev B, Zak B, Mamaladze V. Is organ-sparing treatment of penile carcinoma justified? Eur Urol. 2000;38:306–12. doi: 10.1159/000020298. [DOI] [PubMed] [Google Scholar]
- 9.Da Fonseca AG, Rabelo GN, Vidal KS, De Sousa FJ. Glandectomy with preservation of corpora cavernosa in the treatment of penile carcinoma. Int Braz J Urol. 2003;29:437–40. doi: 10.1590/s1677-55382003000500010. [DOI] [PubMed] [Google Scholar]
- 10.Greenberger ML, Lowe BA. Penile stump advancement as an alternative to perineal urethrostomy after penile amputation. J Urol. 1999;161:893–4. [PubMed] [Google Scholar]
- 11.Santanelli F, Paolini G. Glans, urethra, and corporeal body reconstruction by free osteocutaneous forearm flap transfer. Ann Plast Surg. 2003;50:545–9. doi: 10.1097/01.SAP.0000038149.45356.12. [DOI] [PubMed] [Google Scholar]
- 12.Jordan GH. Penile reconstruction, phallic construction and urethral reconstruction. Urol Clin North Am. 1999;26:1–13. doi: 10.1016/s0094-0143(99)80003-2. [DOI] [PubMed] [Google Scholar]
- 13.Smith Y, Hadway P, Biedrzycki O, Perry MJ, Corbishley C, Watkin NA. Reconstructive surgery for invasive squamous carcinoma of the glans penis. Eur Urol. 2007;52:1179–85. doi: 10.1016/j.eururo.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 14.Palminteri E, Berdondini E, Lazzeri M, Mirri F, Barbagli G. Resurfacing and reconstruction of the glans penis. Eur Urol. 2007;52:893–8. doi: 10.1016/j.eururo.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 15.Mazza ON, Cheliz GM. Glanduloplasty with scrotal flap for partial penectomy. J Urol. 2001;166:887–9. [PubMed] [Google Scholar]
- 16.Cook A, Khoury AE, Bagli DJ, Farhat WA, Pippi Salle JL. Use of buccal mucosa to simulate the coronal sulcus after traumatic penile amputation. Urology. 2005;66:1109. doi: 10.1016/j.urology.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Gulino G, Sasso F, Falabella R, Bassi PF. Distal urethral reconstruction of the glans for penile carcinoma: Results of a novel technique at 1-year of follow-up. J Urol. 2007;178(3 Pt 1):941–4. doi: 10.1016/j.juro.2007.05.059. [DOI] [PubMed] [Google Scholar]
- 18.Maddineni SB, Lau MM, Sangar VK. Identifying the needs of penile cancer sufferers: A systematic review of the quality of life, psychosexual and psychosocial literature in penile cancer. BMC Urol. 2009;9:8. doi: 10.1186/1471-2490-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bigelow DA, Young DJ. Effectiveness of a case management program. Validation and application of the Quality of life questionnaire. Respondent self-report version. Community Ment Health J. 1991;27:115–23. doi: 10.1007/BF00752814. [DOI] [PubMed] [Google Scholar]
- 20.Ficarra V, Righetti R, D’Amico A, Pilloni S, Balzarro M, Schiavone D, et al. General state of health and psychological well-being in patients after surgery for urological malignant neoplasms. Urol Int. 2000;65:130–4. doi: 10.1159/000064857. [DOI] [PubMed] [Google Scholar]
- 21.Li P, Song N, Yin C, Zhang W, Li J, Hua L, et al. Glans preserving surgery for penile superficial cancer. J Androl. 2011 doi: 10.2164/jandrol.111.013896. 10.2164/jandrol.111.013896. [DOI] [PubMed] [Google Scholar]
- 22.Bullen K, Matthews S, Edwards S, Marke V. Exploring men's experiences of penile cancer surgery to improve rehabilitation. Nurs Times. 2009;105:20–4. [PubMed] [Google Scholar]
- 23.Duran ID, Rojas-Piloni JG, Cueva-Rolon R. Facilitation and inhibition of the urethrogenital reflex in spinal cord-transected rats. Brain Res. 1997;14:1–10. doi: 10.1016/s0006-8993(97)00897-4. [DOI] [PubMed] [Google Scholar]
- 24.Carro-Juarez M, Rodriguez-Manzo G. Role of genital sensory information in the control of the functioning of the spinal generator for ejaculation. Int J Impot Res. 2005;17:114–20. doi: 10.1038/sj.ijir.3901277. [DOI] [PubMed] [Google Scholar]


